Abstract
Purpose
Transversus abdominis plane (TAP) block is a newly developed and effective peripheral block involving the nerves of the anterior abdominal wall for lower abdominal surgery. We evaluated the postoperative analgesic efficacy of ultrasound-guided TAP block using 20 mL of 0.5% levobupivacaine in patients undergoing open appendectomy.
Methods
Forty-four patients undergoing appendectomy were assigned either to undergo a right sided-TAP block (group I, n = 22), or to receive standard care (group II, n = 22). All patients received standard anesthetics, and the TAP block group received ultrasound-guided right side TAP block using 20 mL of 0.5% levobupivacaine after induction of anesthesia. All patients received acetaminophen, and nonsteroidal anti-inflammatory drug as required during the 48 postoperative hours. Each patients was assessed for time to first rescue analgesia, verbal numerical rating pain scores (VNRS), number of rescue analgesic demands, nausea, vomiting, pruritus, and drowsiness by a blinded investigator at 0, 1, 3, 6, 12, 24 and 48 hours postoperatively.
Results
The TAP block group with levobupivacaine compared to the control group reduced VNRS significantly up to 12 hours postoperatively. There were no significant differences in time to first analgesia, number of rescue analgesics demands, nausea, vomiting, pruritus and drowsiness between the groups. There were no complications attributable to the TAP block.
Conclusion
Ultrasound-guided TAP block using 20 mL of 0.5% levobupivacaine provided effective postoperative analgesia during the 12 postoperative hours after an open appendectomy.
Keywords: Appendectomy, Postoperative pain, Nerve block, Ultrasonography
INTRODUCTION
Acute appendicitis is one of the causes for considerable abdominal pain and most common surgical emergency. Postoperative pain after an open appendectomy originates from somatosensory pain of the incision site and from visceroperitoneal pain of inflammatory tissue [1]. Postoperative pain including from an appendectomy can be managed with intermittent systemic analgesics such as opioids, ketamine, nonsteroidal anti-inflammatory drugs (NSAIDs), alpha-2 agonist, acetaminophen or continuous infusion of a mixture of drugs acting through different mechanisms [2]. Epidural block or local anesthetics injection at the incision site can be also used for pain control [3]. In recent years, transversus abdominis plane (TAP) block has been developed and considered as a peripheral nerve block for postoperative pain control after abdominal surgery including colon resection, caesarean section, prostatectomy, and laparoscopic cholecystectomy [4-7]. These studies suggested that TAP block used as a method of multimodal balanced analgesia reduces postoperative pain, opioid requirement during the 48 hours after surgery and adverse events from opioids such as sedation, nausea, vomiting, respiratory depression, and ileus. However, there have not been many studies on the efficacy of TAP block performed in open appendectomy patients.
Therefore, we conducted the present study to determine the analgesic efficacy of ultrasound guided TAP block (US-TAP block) with 20 mL of 0.5% levobupivacaine in open appendectomy patients under NSAID based standard pain control treatment.
METHODS
A randomized, double-blinded controlled clinical trial was carried out after obtaining approval from the regional ethics committee and written informed consent from the patients. We examined 44 American Society of Anesthesiology (ASA) physical status I and II patients, aged 20 to 70 years, scheduled to undergo an open appendectomy. Patients were excluded if there was a history of allergy to levobupivacaine, coagulopathy or infection at the needle insertion site. Patients who had a difficulty to cooperating were also excluded.
Patients were allocated into two groups with a randomized sequence table: one group to undergo US-TAP block with 0.5% levobupivacaine (TAP block group, n = 22) and the other group to receive standard care (control group, n = 22). The primary outcome was time to first analgesia after surgery. Assuming the median time to first analgesia for the control and TAP block groups is 15 and 35 minutes, respectively, a power analysis based on 80% power with a type I error of 0.05 determined that we needed 22 patients for each group. There was no significant difference between the two groups in age, weight, height, body mass index (BMI), sex, and ASA physical status (Table 1).
Table 1.
Demographic data and clinical characteristics
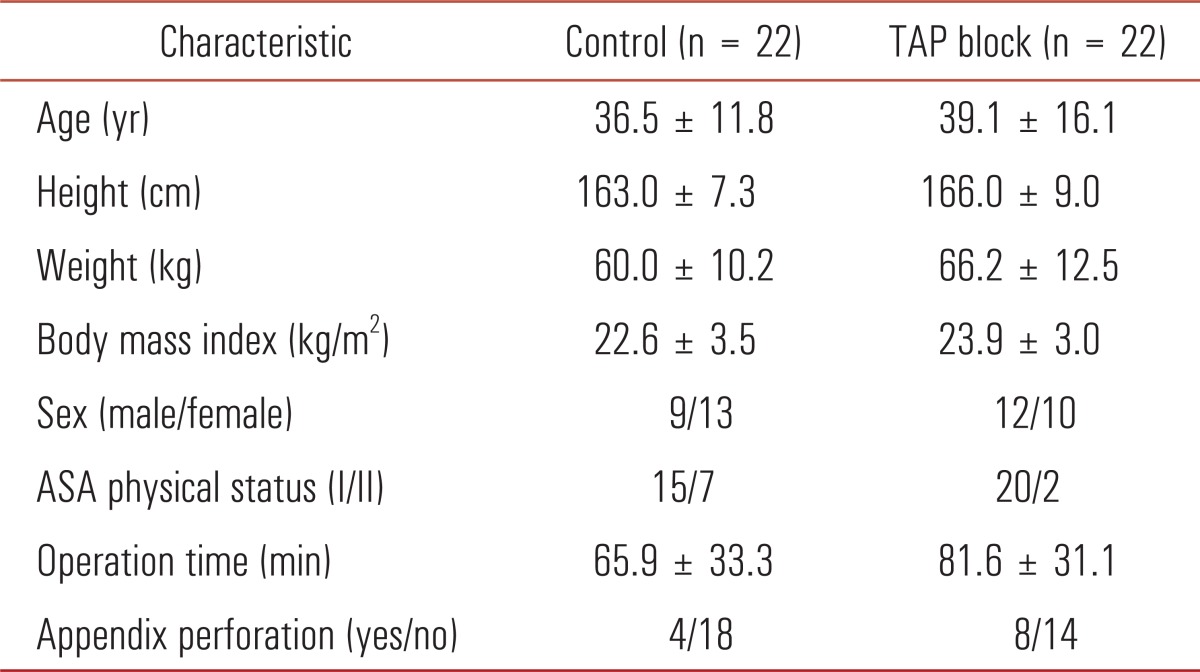
Values are presented as mean ± standard deviation. Control group received ultrasound transversus abdominis plane block with 20 mL of 0.9% normal saline. TAP block received ultrasound transversus abdominis plane block with 20 mL of 0.5% levobupivacaine.
TAP, transversus abdominis plane; ASA, American Society of Anesthesiologist.
All patients received standard general anesthetic management. Noninvasive blood pressure, electrocardiography, pulse oximetry, and capnometry were applied. Anesthesia was induced with glycopyrrolate 0.2 mg, midazolam 0.05 mg/kg, thiopental sodium 4 mg/kg, and fentanyl 1-2 µg/kg followed by mask ventilation and intubation for 90 seconds after injection rocuronium 0.6 mg/kg. Anesthesia was maintained with nitrous oxide, oxygen and sevoflurane. Sevoflurane was maintained as 2 volume % during surgery; additionally, fentanyl 0.5-1 µg/kg was injected to control blood pressure and heart rate within 20% of baseline. End-tidal carbon dioxide (CO2) was maintained at 30-35 mmHg.
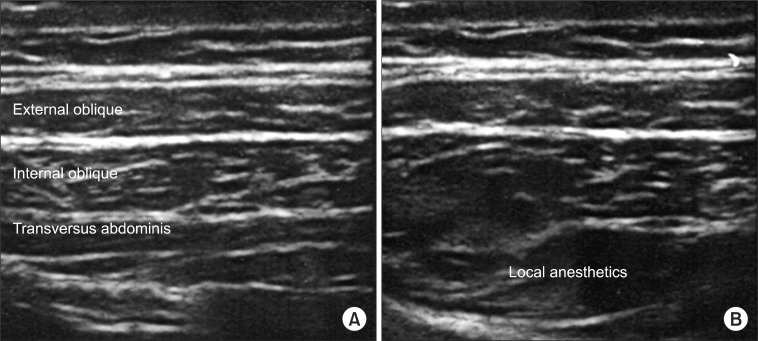
When vital signs were stable after intubation, experienced anesthesiologist who did TAP block more than 10 times performed the TAP block under ultrasound guidance with a Sonosite M-Turbo ultrasound device and a 5 to 12 MHz linear transducer (Sonosite, Bothell, WA, USA). After draping the needle insertion site, the probe was placed transversely on the level of the right anterior axillary line between the 12th rib and the iliac crest, and the external oblique, internal oblique and transversus abdominis muscles were identified (Fig. 1A). A 22-gauge, 50-mm needle (Stimuplex, B. Braun, Melsungen, Germany) was inserted medial to the probe by the in-plane technique and advanced in a lateral direction. When the tip of the needle reached the TAP between the internal oblique and transversus abdominis muscles, 1 mL of 0.5% levobupivacaine and normal saline were injected into the patients of the TAP block group and control group, respectively, after negative aspiration, and the spread of the drugs was confirmed. Then, the remaining 19 mL was injected. Adequate diffusion of the drug was certified by an oval-shaped hypoechoic fluid pocket at TAP with real-time ultrasound imaging (Fig. 1B). Besides checking negative aspiration and seeing needle did not puncture peritoneum or visceral organs on US view, the surgeon confirmed if peritoneum or visceral organs were intact for operation. At the end of the surgery, the total dose of intraoperative fentanyl was recorded. Pain intensity was assessed as the verbal numerical rating scale (VNRS: 0, no pain; 10, the severest pain imaginable) at arrival in the recovery room (time 0) and at 1, 3, 6, 12, 24 and 48 hours postoperatively. Every assessment of VNRS was performed by a blinded interviewer, and pain was scored under two conditions: at rest (VNRSr) and at coughing (VNRSc). Nausea/vomiting and dizziness events were also recorded. When the VNRSr was greater than 4 in the recovery room, ketorolac tromethamine (Ketorac, Daewoo Pharm Co., Busan, Korea) 30 mg as a rescue analgesic was given. After transfer to the ward, the patient was managed with a standard protocol including injection of ketorolac tromethamine 30 mg every 12 hours. When the VNRSr was higher than 4 or the patient wanted an analgesic, a rescue analgesic was given. When a patient refused a drug, even the basic protocol analgesic was not injected. All given analgesics at the recovery room and ward were recorded as doses and time given. And the time of first analgesia was recorded.
Fig. 1.
(A) Abdominal muscles and fascia before injection. (B) Abdominal muscles and fascia after 20 mL injection of local anesthetics to transversus abdominis plane.
Statistical analyses were performed using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Pain scores at each time period were compared using the Mann-Whitney U test. Total number of analgesics, intraoperative fentanyl use and the time to first analgesia were analyzed using Student t-test. Categorical variables were compared using chi-square analysis or Fisher exact test. In all tests, data with a P < 0.05 were considered statistically significant.
RESULTS
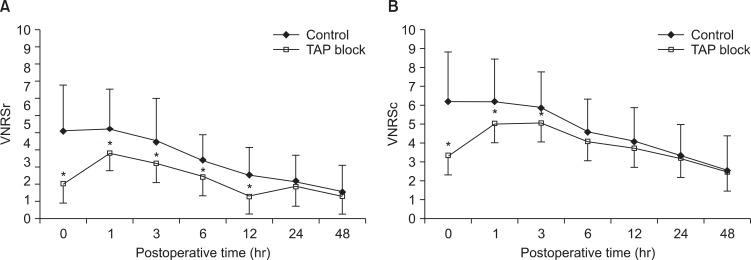
The VNRSr was lower in the TAP block group than in the control group at 0, 1, 3, 6 and 12 hours. The VNRSc at 0, 1 and 3 hours was lower in the TAP block group than in the control group (Fig. 2).
Fig. 2.
VNRSr (A) and VNRSc (B) change according to the time. Control group received ultrasound transversus abdominis plane block with 20 mL of 0.9% normal saline. TAP block received ultrasound transversus abdominis plane block with 20 mL of 0.5% levobupivacaine. VNRSr, verbal numerical rating scale at resting state; VNRSc, verbal numerical rating scale at coughing; TAP, transversus abdominis plane. *P < 0.05 compared with the control group.
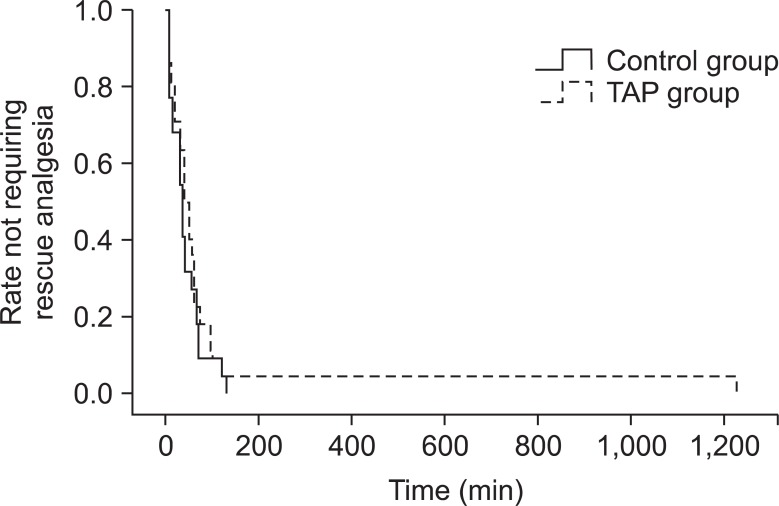
Intraoperative injected fentanyl was significantly less in the TAP block group than in the control group. The time to first analgesia was 100.2 ± 254.3 minutes in the TAP block group and 40.9 ± 34.7 minutes in the control group, but the difference was not statistically significant (Fig. 3). The number of analgesics in the first 24 and 48 hours was also not statistically different (Table 2).
Fig. 3.
A Kaplan-Meier graph of the time to first rescue analgesia. Control group received ultrasound transversus abdominis plane block with 20 mL of 0.9% normal saline. Transversus abdominis plane (TAP) block received ultrasound transversus abdominis plane block with 20 mL of 0.5% levobupivacaine.
Table 2.
Analgesic requirements for open appendectomy
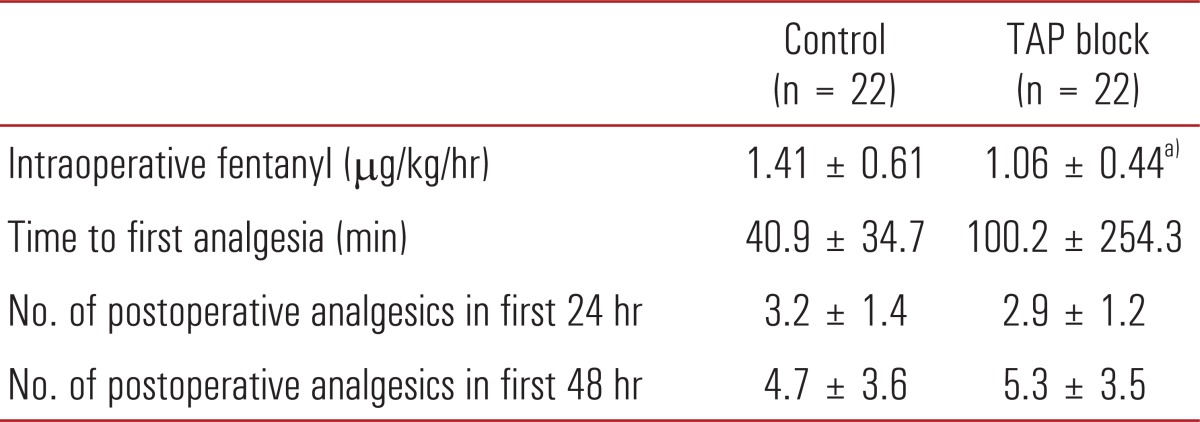
Values are presented as mean ± standard deviation. Control group received ultrasound transversus abdominis plane block with 20 mL of 0.9% normal saline. Transversus abdominis plane (TAP) block received ultrasound transversus abdominis plane block with 20 mL of 0.5% levobupivacaine.
a)P < 0.05 compared with the control group.
In all 44 patients, there were no peritoneal punctures, bowel perforations, pneumoperitoneum, bleeding, and infection at the needle insertion site.
DISCUSSION
We investigated the analgesic effect of US-TAP block with 20 mL of 0.5% levobupivacaine in patients undergoing an open appendectomy who were managed by standard pain control treatment using NSAIDs. In our study, the VNRS at the resting state was lower in the TAP block group in the first 12 hours and the VNRS at coughing was lower in the TAP block group in the first 3 hours than that of the control group.
Many studies have been conducted to determine the analgesic effect of TAP block under different conditions of abdominal surgeries, local anesthetics, doses and concentrations of drugs and time of block [4-12]. Preoperative TAP block in a major operation such as hysterectomy, cesarean delivery and large bowel resection reduced pain scores, opioid requirements in the first 24 hours and side effects of opioids, and increased the time to first analgesics. Thus, these studies suggested TAP block has a positive effect [4-6]. Other studies on TAP block in laparoscopic cholecystectomy and open appendectomy also reported positive results in which pain scores and morphine requirements in the first 24 hours were lower in the TAP block group than in the control group [7,10]. However, some studies showed different results. Ortiz et al. [11] compared TAP block and local anesthetic infiltration to trocar insertion sites in laparoscopic cholecystectomy and showed no differences in pain scores and analgesic requirements. Sandeman et al. [12] also reported no differences in postoperative analgesics between the TAP block group and control group for laparoscopic appendectomy in children. In this study, the pain scores were lower in the TAP block group during the first 12 hours after surgery, but there were no statistically significant differences between the two groups in the time to first analgesia and total analgesic requirements. Most positive results were from studies on elective major operations and most hospitals have their own standard perioperative management regimens including fluid therapy and pain control. Therefore, there were not many alterations on perioperative care among the patients. Additionally, blocking somatosensory pain from a large incision site of major surgery by TAP block was useful. However, in cholecystectomy or appendectomy, patients experienced visceroperitoneal pain prior to surgery and treated first at a local primary clinic or emergency room. For this reason, the preoperative condition of the patient and management such as duration or intension of pain, NSAIDs or opioids prescribed and degree of hydration were variable and influenced the effect of TAP block. A relatively small incision 2 to 3 cm in size also affects the efficacy of TAP block. All these factors could explain why our results were different from previous studies.
The duration of TAP block has been shown to be variable. McDonnell et al. [5,6] reported that pain scores and morphine requirements were reduced in the first 24 hours after large bowel resection by TAP block using 0.375% levobupivacaine and in the first 48 hours after cesarean delivery by using 0.75% ropivacaine. Carney et al. [4] studied the effect of TAP block with 0.75% ropivacaine and reported that the pain intensity decreased in the first 36 hours after surgery and morphine requirements was were reduced during the first 48 hours. In addition, Niraj et al. [10] used 0.5% bupivacaine with a TAP block in an open appendectomy, and the morphine requirements and pain scores decreased in the first 24 hours. In this study, we used 0.5% levobupivacaine and the effect continued during the first 12 hours. The pain intensity was maximum at postoperative hour 1 and 3. For all time periods after the first 12 hours, the VNRSs were less than 3 in both groups and that result could be because open appendectomy is minor surgery with only a small incision site. Difference of VNRS between two groups was small because VNRSs were low, so the difference was not statistically significant after 12 hours. For this reason, the duration of the TAP block in this study was shorter than that of previous studies.
The TAP block caused a 25% reduction in the amount of intraoperative fentanyl used compared with the control group. Preoperative TAP block blocked the somatosensory pain of the incision site and reduced intraoperative opioid requirements and postoperative side effects such as nausea and sedation. This is an advantage of using a TAP block.
TAP block is widely appliable procedure. Although we studied in only adult patients, TAP block is considered to have few limitations of age. Several studies reported positive results of TAP block in wide range of age even neonates or infants under 1 year old [13,14]. However, in pediatric patients, there is no general consensus about doses or concentrations of drug and same pain assessment method such as VNRS cannot be used. Therefore, we limited to adult patients in this study. Recently, TAP block showed effective pain control in morbidly obese patients who had bariatric surgery [15]. We did not consider BMI in patient selection, BMI range in this study showed 17.6 to 32.5 kg/m2. Though morbidly obese patients are not common in Korea, when TAP block is carried in these patients, convex probe of ultrasound should be used instead of linear probe considering thickness of fat.
The standard pain control regimen for open appendectomy patients at our hospital is the use of NSAIDs rather than opioids or patient controlled analgesia (PCA). As seen in Fig. 2, the maximal pain intensity period was during the first 3 hours and decreased after that. During this period, TAP block reduced the VNRS by 20-60%. Especially during the first hour from the end of surgery in the recovery room, pain dropped by 60% and it was the biggest decline. Considering the VNRS was smaller than 3 after 12 hours, pain control in the immediate postoperative period can have an important role in improving the postoperative quality of life. An emergency appendectomy is usually performed after work during the day. As result of this study, if TAP block can reduce pain without opioids during the immediate postoperative period which is often night time, it will be very helpful to patients who are susceptible or vulnerable to opioids. And in this manner, we can increase the satisfaction of patient and reduce the length of the hospital stay.
Cost of US-TAP block might vary widely from hospital to hospital. The price of local anesthetics, the ultrasound cost and the procedure fee are main portion of US-TAP block cost. The overall cost of TAP block is about 110,000 Korean Won in Ewha Womans University Mokdong Hospital, it is slightly lower price than intravenous-PCA (IV-PCA) and higher than routine injections of opioids or NSAIDs. In aspect of satisfaction, analgesic effect of US-TAP block is comparable to IV-PCA and more excellent than injections of analgesics. Therefore, US-TAP block is more cost-effective method for pain control.
In conclusion, US-TAP block using 20 mL of 0.5% levobupivacaine in open appendectomy patients is a safe and effective method for postoperative pain control.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Aida S, Baba H, Yamakura T, Taga K, Fukuda S, Shimoji K. The effectiveness of preemptive analgesia varies according to the type of surgery: a randomized, double-blind study. Anesth Analg. 1999;89:711–716. doi: 10.1097/00000539-199909000-00034. [DOI] [PubMed] [Google Scholar]
- 2.Buvanendran A, Kroin JS. Useful adjuvants for postoperative pain management. Best Pract Res Clin Anaesthesiol. 2007;21:31–49. doi: 10.1016/j.bpa.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 3.White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101(5 Suppl):S5–S22. doi: 10.1213/01.ANE.0000177099.28914.A7. [DOI] [PubMed] [Google Scholar]
- 4.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transverses abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–2060. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 5.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106:186–191. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 6.McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 7.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–368. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transverses abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth. 2009;103:726–730. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 9.Bharti N, Kumar P, Bala I, Gupta V. The efficacy of a novel approach to transversus abdominis plane block for postoperative analgesia after colorectal surgery. Anesth Analg. 2011;112:1504–1508. doi: 10.1213/ANE.0b013e3182159bf8. [DOI] [PubMed] [Google Scholar]
- 10.Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601–605. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37:188–192. doi: 10.1097/AAP.0b013e318244851b. [DOI] [PubMed] [Google Scholar]
- 12.Sandeman DJ, Bennett M, Dilley AV, Perczuk A, Lim S, Kelly KJ. Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: a prospective randomized trial. Br J Anaesth. 2011;106:882–886. doi: 10.1093/bja/aer069. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs A, Bergmans E, Arul GS, Thies KC. The transversus abdominis plane (TAP) block in neonates and infants: results of an audit. Paediatr Anaesth. 2011;21:1078–1080. doi: 10.1111/j.1460-9592.2011.03628.x. [DOI] [PubMed] [Google Scholar]
- 14.Fredrickson M, Seal P, Houghton J. Early experience with the transverses abdominis plane block in children. Paediatr Anaesth. 2008;18:891–892. doi: 10.1111/j.1460-9592.2008.02591.x. [DOI] [PubMed] [Google Scholar]
- 15.Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transverses abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23:548–553. doi: 10.1007/s11695-012-0819-5. [DOI] [PubMed] [Google Scholar]