Abstract
Demographic shifts in China pose unprecedented challenges in the care of a rapidly growing older population. Sporadic reports suggest the recent emergence of institutional elder care in China, but little is currently known about this phenomenon. This study documents the growth, ownership, financing, staffing, and resident characteristics of elder care institutions using survey data collected in 2009 from Nanjing, China, supplemented with government registry data from seven additional major Chinese cities. Between one-half and two-thirds of facilities operating in these cities were founded in the last decade, primarily in the non-government sector. In Nanjing, government ownership dominated homes built before 1990 (96%) but was increasingly rare in the 1990s (60%) and in the 2000s (23%), a pattern observed in the other seven cities as well. In Nanjing, the average home now draws more than 80% of its daily operating revenues from private-pay or other non-government sources, and this share increases sharply with the recency of facility establishment. The majority (85%) of non-government-owned homes are receiving ongoing per-bed subsidies from the government. The lack of clinical staff characterizes the majority of study facilities; most care staff are rural migratory workers. There is considerable variability across facilities in the case-mix of residents in terms of functional dependence and acuity levels. These findings portray the emergence and rapid growth of a nascent industry of institutional long-term care in urban China and a fundamental shift in institutional ownership, financing, and clientele.
Keywords: aging, long-term care, non-government ownership, China
Upon its centennial anniversary, the Dongzhimen Elementary School in Beijing closed in 2003 and joined two other closed elementary schools in the same district to form a new one.1 In 2006, a private company renovated the school's old buildings to become the Three Harmonies Senior Citizens’ Home.2 The transformation of Dongzhimen Elementary School into a retirement home symbolizes several profound sociodemographic shifts in China—the shrinking of younger generations, a burgeoning older population, and accordingly, escalating needs for care of older adults that increasingly strain the Chinese family and engender new forms of elder care outside the traditional informal support network.
The prospects of population aging and its unprecedented challenges for elder care in China have been well documented.3–5 Current demographic projections suggest that the older population (≥65) in China will increase rapidly in the next 30 years, from 8.3% of the total population at present to 22.6% in 2040; the oldest old (≥80) will grow the fastest, from 1.4% today to 5.0% by 2040.6 Given China's enormous population base, these percentages translate into the largest absolute numbers of older people in the world, from roughly 112 million aged 65 and older and 19 million aged 80 and older today to 329 million and 73 million, respectively, by 2040. The older population is also living longer: at age 65, older Chinese today can expect to live an average of 16 additional years for women and 14 additional years for men.7
Traditionally, elder care in China has been confined to the familial sphere, long enshrined by the Confucian norm of filial piety. The Constitution of the People's Republic of China stipulates that “Parents have the duty to rear and educate their minor children, and children who have come of age have the duty to support and assist their parents” (Article 49),8 but demographic shifts and rapid socioeconomic changes have fueled growing concerns about whether the family alone will still be able to care for the rapidly increasing elderly population in China.9–12 In urban areas, the emerging “4:2:1” family structure, which consists of four grandparents, two adult children both without siblings, and one grandchild—a consequence of the one-child policy having been in effect since 1979—compounds these concerns.
Currently, no national health insurance program for older people (e.g., Medicare in the United States) or publicly funded safety net program covering health and long-term care (LTC) for the needy (e.g., Medicaid in the United States) exists in China. Hospital care for older Chinese is paid for primarily through fee-for-service, and after long hospital stays patients are discharged home without institutional or community-based postacute care.11 As is the case in the United States and elsewhere, most elderly Chinese prefer living in their own homes than in institutions.13 Despite recent government policy initiatives promoting the development of home- and community-based elder services, such as cash allowances for paid home care, community health centers, senior housing, recreational facilities, and adult day care programs,8,14 such services have not yet emerged as a viable LTC option for most elderly Chinese.
Until recently, institutional elder care was virtually unknown in China. The few facilities that existed were social welfare institutions run by the government, serving mentally retarded, deficient adults without families and childless older adults.8,15 Recent reports suggest that elder care homes owned and operated by non-government entities have proliferated across major urban centers in China,13,16–18 yet little is known about the characteristics of these institutions.
The objectives of this article are to document the growth, ownership, financing, staffing, and resident characteristics of elder care institutions using survey data recently collected from the city of Nanjing, China, and to use supplemental data from seven additional major cities in China to determine whether patterns seen in Nanjing are similar to those in other parts of the country.
METHODS
Data and Setting
Primary data collected from the city of Nanjing, China, in 2009 were used. One of China's ancient capitals and now the capital city of Jiangsu Province, Nanjing is located in the Yangtze River Delta approximately 150 miles west of Shanghai. As of 2008, the total population of Nanjing was roughly 7.6 million, of whom more than 10% were aged 65 and older.19
The target population consisted of all elder care homes located in the urban districts of Nanjing, as of June 2009. The operational definition of an elder care home used is a provider of institutional LTC services licensed by the city of Nanjing. Homes located in remote suburban or rural areas of the city were excluded because of travel considerations. From the official listing of all registered elder care homes maintained by the Nanjing Municipal Bureau of Civil Affairs, the government agency licensing social welfare and institutional elder care services, 148 target facilities were identified.
After a survey questionnaire was field tested, a group of 12 graduate students recruited from Nanjing University who the investigators (ZF, HZ) had trained administered it to all target facilities through on-site, face-to-face interviews with administrators. The questionnaire was modeled after the Online Survey Certification and Reporting instrument currently used in the United States for annual inspection and certification of nursing homes and adapted to fit the Chinese context. It gathered information at the facility level, including size, ownership, financing, staffing, and aggregated resident characteristics. The process of data collection, entry, and integration occurred over a 6-month period, from June to December 2009. Complete survey data were obtained from 140 of 148 (94.6%) elder care homes in urban Nanjing.
To supplement the detailed one-city survey, local government Web sites targeting all provincial capitals or major cities in China were queried. There are 34 province-level administrative units in China: 22 provinces, five autonomous regions, four municipalities, two special administrative regions (Hong Kong and Macau), and Taiwan. Seven of these cities had lists of licensed facilities including data on ownership or the date each facility was founded. Two (Beijing and Tianjin) posted the year of facility establishment, and six (Shanghai, Tianjin, Hangzhou (capital of Zhejiang province), Dalian (Liaoning province), Xiamen (Fujian province), and Anshan (Liaoning province)) had information on facility ownership. These data pertained to 2007 for Tianjin and 2009 for all remaining cities. The geographic locations of all study cities are shown in a map (Figure 1).
Figure 1.
Geographic location of study cities, China.
Main Study Measures
Growth
For Nanjing, Beijing, and Tianjin, a cumulative frequency distribution of all existing elder care homes in each city was constructed according to year of facility establishment and used as an approximate measure of growth. In Nanjing, each facility was further asked whether an expansion (e.g., new building construction, adding new beds) was currently underway to document planned future growth.
Ownership
In each of the seven cities with ownership information available, all facilities were classified as government or non-government. Government-owned homes may operate at the municipal, district, or street residential committee (the lowest level in the Chinese urban government administrative hierarchy) level. A variety of entities such as individuals, partners, a corporation, charities, or other non-government organizations may own and run non-government homes. It was sought to examine the changing relative shares of government and non-government homes.
Financing
In Nanjing, each facility was asked about the percentage of its daily operating revenues derived from each of three broad sources: government funding; private pay (including the residents’ own out-of-pocket money, their pensions, and transfers from adult children or relatives); and other sources (a residual category including, e.g., funds from charities or other non-government sources). In addition, each facility was asked whether it was receiving ongoing subsidies per occupied bed from the government.
Staffing
In Nanjing, basic demographic information was gathered about the current administrator and whether he or she was also the founder of the facility. It was also sought to determine whether the facility had a clear division of labor between direct personal care (e.g., help with dressing, bathing, eating, and toileting) and housekeeping (e.g., cleaning, laundry) staff. Information was collected on staffing levels (number of direct-care staff per 100 residents), the proportion of direct-care staff who were rural migratory workers, whether the facility housed direct-care staff and if so, the proportion of staff living on-site. Whether the facility employed professional nurses and physicians was also determined.
Resident Characteristics
In Nanjing, aggregate information was obtained on current residents in each facility, including basic demographics, payment source, and functional and clinical characteristics.
Analytical Approach
Stratified analyses are first presented, according to city, of the cumulative growth of elder care homes and ownership in the eight study cities (including Nanjing). Then, based on data collected from facilities in Nanjing, their financing, staffing, and resident characteristics are described according to ownership and facility age. The year of facility establishment was categorized into three categories: before 1990, during the 1990s, and during the 2000s.
RESULTS
Growth of Elder Care Institutions
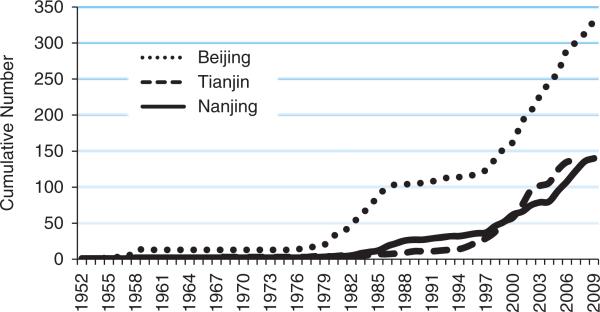
Figure 2 presents the cumulative distribution of elder care homes according to year of establishment, in the three cities with data available. All cities demonstrated dramatic growth of elder care homes. In Nanjing, for instance, there were only three facilities in 1980, but there were 27 by 1990, 52 by 2000, and 140 by 2009. Similar growth was observed in Beijing and Tianjin. Drawing upon Chinese census and population survey data, it was estimated that, in Nanjing, there were approximately 17 facility beds per 1,000 people aged 65 and older in 2009, nearly doubling the number in 2000 of nine beds per 1,000 older adults (results not shown).
Figure 2.
Cumulative growth of elder care homes over time in selected Chinese cities.
The majority (58%) of elder care homes in the three cities were founded in the last decade (2000–2009), 19% in the 1990s, and 24% before 1990 (Table 1). Between one-half and two-thirds of all homes now operating emerged in the last decade, and approximately one-third in the last 5 years. For instance, 63% of current facilities in Nanjing opened their doors in the last 10 years, 62% in Tianjin, and 54% in Beijing. In Nanjing, 22% of homes reported an expansion currently under way, more likely in newer and non-government homes (Table 2).
Table 1.
Distribution of Current Elder Care Homes in Selected Chinese Cities According to Year of Establishment and Ownership
| Year of Establishment and Ownership | Nanjing | Tianjin* | Beijing | Shanghai | Hangzhou | Dalian | Xiamen | Anshan | Total |
|---|---|---|---|---|---|---|---|---|---|
| Year established | |||||||||
| Before 1990, n (%) | 27 (19.3) | 11 (8.1) | 105 (31.7) | NA | NA | NA | NA | NA | 143 (23.6) |
| 1990s, n (%) | 25 (17.9) | 41 (30.1) | 49 (14.8) | NA | NA | NA | NA | NA | 115 (18.9) |
| 2000s, n (%) | 88 (62.9) | 84 (61.8) | 177 (53.5) | NA | NA | NA | NA | NA | 349 (57.5) |
| Total, n | 140 | 136 | 331 | 607 | |||||
| Ownership | |||||||||
| Government, n (%) | 61 (43.6) | 19 (15.2) | NA | 233 (42.2) | 33 (62.3) | 102 (40.0) | 3 (13.0) | 5 (8.3) | 456 (37.7) |
| Non-government, n (%) | 79 (56.4) | 106 (84.8) | NA | 319 (57.8) | 20 (37.7) | 153 (60.0) | 20 (87.0) | 55 (91.7) | 752 (62.3) |
| Total, n | 140 | 125 | 552 | 53 | 255 | 23 | 60 | 1,208 |
Totals are different for year established and ownership because information on ownership was not available for all homes.
NA = not available.
Table 2.
Characteristics of Current Elder Care Homes in Nanjing (N = 140) According to Year of Establishment and Ownership
| Year Established |
Ownership |
|||||
|---|---|---|---|---|---|---|
| Characteristic | Total (N = 140) | Before 1990 (n = 27) | 1990s (n = 25) | 2000s (n = 88) | Government (n = 61) | Non-Government (n = 79) |
| Sources of daily operating revenues, %* | ||||||
| Government, mean ± SD | 19.5 ± 34.9 | 60.8 ± 43.7 | 19.2 ± 34.8 | 7.6 ± 20.3 | 42.2 ± 43.8 | 2.4 ± 4.1 |
| Private pay, mean ± SD | 79.3 ± 35.4 | 38.7 ± 43.5 | 79.3 ± 37.6 | 91.2 ± 20.7 | 56.9 ± 44.5 | 96.2 ± 7.2 |
| Other sources, mean ± SD | 1.2 ± 5.2 | 0.5 ± 2.1 | 1.5 ± 6.2 | 1.3 ± 5.5 | 0.8 ± 4.2 | 1.5 ± 5.8 |
| Receiving government bed subsidies, % | 70.0 | 37.0 | 48.0 | 86.4 | 50.8 | 84.8 |
| Structure and organization, % | ||||||
| Government ownership | 43.6 | 96.3 | 60.0 | 22.7 | - | - |
| Expansion currently under way | 22.1 | 12.0 | 21.7 | 26.4 | 19.0 | 26.0 |
| Hospital affiliated | 12.1 | 3.7 | 0.0 | 18.2 | 6.6 | 16.5 |
| Chain membership | 7.9 | 0.0 | 16.0 | 8.0 | 8.2 | 7.6 |
| Total number of beds, mean ± SD | 77.4 ± 84.4 | 86.3 ± 121.7 | 69.8 ± 58.0 | 76.8 ± 77.4 | 81.0 ± 94.4 | 74.6 ± 76.3 |
| Occupancy rate, mean ± SD | 75.2 ± 25.3 | 83.9 ± 22.8 | 80.2 ± 21.7 | 71.2 ± 26.3 | 83.1 ± 20.5 | 69.2 ± 27.1 |
| Staffing | ||||||
| Administrator | ||||||
| Age, mean ± SD | 49.3 ± 9.1 | 53.8 ± 7.9 | 51.1 ± 6.2 | 47.4 ± 9.6 | 51.4 ± 8.3 | 47.7 ± 9.4 |
| Female, % | 65.0 | 63.0 | 64.0 | 65.9 | 68.9 | 62.0 |
| Education, some college or higher, % | 39.3 | 22.2 | 28.0 | 47.7 | 31.2 | 45.6 |
| Founder of current facility, % | 48.6 | 3.7 | 28.0 | 69.0 | 21.3 | 70.5 |
| Separation of direct-care and housekeeping staff, % | 32.9 | 22.2 | 20.0 | 39.8 | 29.5 | 35.4 |
| Direct-care staff | ||||||
| Number of staff per 100 residents, mean ± SD | 18.1 ± 10.5 | 14.6 ± 9.5 | 15.9 ± 17.0 | 19.7 ± 7.8 | 14.8 ± 8.5 | 20.6 ± 11.2 |
| Percentage female, mean ± SD | 74.4 ± 20.6 | 81.0 ± 20.7 | 83.5 ± 19.9 | 69.9 ± 19.6 | 79.0 ± 18.3 | 70.9 ± 21.7 |
| Percentage middle school or more education, mean ± SD | 50.7 ± 38.6 | 59.8 ± 37.4 | 61.9 ± 41.0 | 44.8 ± 37.5 | 61.8 ± 38.3 | 42.3 ± 36.9 |
| Percentage rural migratory workers, mean ± SD | 55.0 ± 43.1 | 28.1 ± 38.6 | 48.1 ± 44.1 | 65.2 ± 40.6 | 37.7 ± 42.5 | 68.4 ± 38.9 |
| Facility provides housing for direct-care staff, % | 82.1 | 51.9 | 76.0 | 94.3 | 63.9 | 97.4 |
| If so, percentage of staff living in facility, mean ± SD | 93.4 ± 17.9 | 76.9 ± 30.6 | 91.8 ± 19.4 | 96.6 ± 12.6 | 86.2 ± 25.1 | 97.1 ± 11.2 |
| Any professional nurse, % | 29.3 | 18.5 | 16.0 | 36.4 | 27.9 | 30.4 |
| Any physician, % | 30.7 | 22.2 | 20.0 | 36.4 | 26.2 | 34.2 |
| Resident characteristics | ||||||
| Number of residents, mean ± SD | 50.7 ± 51.5 | 58.9 ± 57.0 | 46.0 ± 32.1 | 49.5 ± 54.3 | 58.9 ± 53.2 | 44.4 ± 49.5 |
| Percentage female, mean ± SD | 54.9 ± 21.5 | 38.3 ± 23.3 | 58.7 ± 24.5 | 58.8 ± 17.4 | 48.4 ± 24.4 | 60.0 ± 17.4 |
| Percentage aged 60, mean ± SD | 94.5 ± 10.7 | 92.9 ± 9.0 | 95.6 ± 6.7 | 94.7 ± 12.1 | 94.2 ± 7.5 | 94.7 ± 12.7 |
| Payment source (overlapping allowed), mean ± SD | ||||||
| Percentage private pay, out of pocket | 35.2 ± 40.2 | 14.1 ± 26.7 | 38.1 ± 36.7 | 40.7 ± 42.7 | 25.0 ± 37.0 | 43.2 ± 41.0 |
| Percentage private pay, with pensions | 61.0 ± 38.3 | 36.0 ± 39.3 | 68.2 ± 35.4 | 66.3 ± 36.2 | 50.0 ± 42.8 | 69.6 ± 32.2 |
| Percentage welfare recipients | 16.0 ± 31.7 | 48.8 ± 45.6 | 19.8 ± 32.4 | 5.0 ± 16.0 | 33.6 ± 42.2 | 2.8 ± 5.6 |
| Health and functioning, mean ± SD | ||||||
| Percentage independent | 47.1 ± 36.2 | 68.5 ± 32.2 | 55.3 ± 37.6 | 38.0 ± 33.9 | 61.3 ± 34.5 | 35.9 ± 33.7 |
| Percentage needing assistance with eating | 18.4 ± 23.3 | 10.1 ± 21.8 | 8.3 ± 10.3 | 23.6 ± 24.8 | 12.3 ± 22.6 | 22.9 ± 22.9 |
| Percentage needing assistance with dressing | 40.1 ± 34.1 | 15.8 ± 24.9 | 27.8 ± 34.7 | 50.5 ± 31.7 | 22.8 ± 29.7 | 52.8 ± 31.5 |
| Percentage needing assistance with walking | 40.8 ± 32.3 | 22.8 ± 27.0 | 26.1 ± 26.9 | 50.2 ± 31.6 | 25.7 ± 27.0 | 52.0 ± 31.5 |
| Percentage with dementia | 23.2 ± 26.5 | 17.5 ± 24.3 | 11.8 ± 16.6 | 28.2 ± 28.2 | 20.7 ± 28.7 | 25.2 ± 24.7 |
| Percentage physically restrained | 7.5 ± 17.8 | 4.9 ± 18.1 | 2.3 ± 5.4 | 9.8 ± 19.5 | 6.2 ± 17.2 | 8.5 ± 18.2 |
| Percentage bladder incontinence | 27.4 ± 30.0 | 20.3 ± 31.6 | 20.8 ± 25.3 | 31.4 ± 30.4 | 22.2 ± 30.6 | 31.4 ± 29.2 |
| Percentage bowel incontinence | 20.8 ± 26.4 | 12.8 ± 24.4 | 15.2 ± 21.8 | 24.8 ± 27.6 | 14.1 ± 24.1 | 25.9 ± 27.1 |
| Percentage with pressure ulcers | 1.0 ± 3.1 | 0.3 ± 1.1 | 1.0 ± 4.1 | 1.2 ± 3.2 | 0.6 ± 2.1 | 1.3 ± 3.6 |
| Percentage receiving tube feeding | 2.0 ± 6.9 | 1.5 ± 4.9 | 0.2 ± .6 | 2.6 ± 8.1 | 1.4 ± 4.9 | 2.4 ± 8.1 |
| Percentage receiving tranquilizers | 2.2 ± 5.0 | 3.1 ± 7.4 | 1.5 ± 4.3 | 2.1 ± 4.3 | 1.7 ± 4.0 | 2.6 ± 5.7 |
Mean percentages add up to 100%, per column.
SD = standard deviation.
Ownership
The distribution of homes according to ownership in each of the seven cities with data available is summarized in Table 1. Government ownership was below 50% in all cities but Hangzhou (62%) and was especially low in Tianjin (15%), Xiamen (13%), and Anshan (8%). In Nanjing, the share of government homes decreased according to the era of establishment: from 96% of facilities built before 1990 to 60% of those in the 1990s and below 23% of those that emerged in the last decade (Table 2).
Financing
In Nanjing, the average elder care home drew less than 20% of its daily operating revenues from government funding and more than 80% from private-pay (79.3%) and other (1.2%) non-government sources (Table 2, first data column). Government funding accounted for more than 60%, on average, of daily operating revenues in homes built before 1990, in contrast to 19% and less than 8% in homes built in the 1990s and 2000s, respectively. Overall, 70% of all homes reported receiving ongoing per-bed subsidies from the government. This proportion varied according to when the homes were established: 37% of homes built before 1990, 48% of those in the 1990s, and 86% of those in the 2000s. Although nearly 85% of non-government-owned homes were receiving ongoing per-bed subsidies from the government, this amounted to just over 2% of their daily operating revenues, with the remaining 98% coming from private-pay or other sources. In contrast, only half of government-owned homes reported receiving subsidies per occupied bed, but, on average, nearly 58% of their daily operating revenues came from private-pay or other sources, with the remaining 42% from government funding; this finding reveals a highly mixed financing model even in government homes.
Staffing
Thirty-three percent of facilities in Nanjing reported that they stipulated a division of labor by clearly differentiating staff who provide direct personal care and those who provide housekeeping services (Table 2). The average home employed 18 direct-care workers per 100 residents. In a typical facility, rural migratory workers constituted 55% of direct-care staff, and this proportion was notably higher in newer and non-government facilities. Most facilities (82%) provided housing for their direct-care staff, and in these facilities, more than 93% of direct-care staff were living on-site. This arrangement was more common in newer and non-government facilities. Professional nurses or physicians were employed in fewer than one-third of all facilities (29% and 31%, respectively).
Resident Characteristics
On average, 35% of residents were paying out of pocket, and 61% were paying all, or part, of the fees from their pensions (Table 2). Publicly supported welfare recipients made up only 16% of residents, who were largely concentrated in government facilities (34%); few were in non-government homes (3%). In homes built before 1990, 49% of residents were welfare recipients, versus 20% in homes built in the 1990s and 5% in facilities in the last decade.
Forty-seven percent of residents in an average facility were independent in daily functioning (Table 2), although this proportion was substantially higher in government (61%) than non-government (36%) facilities. Overall, 18% of residents required assistance with eating, 40% with dressing, and 41% with walking; each of these proportions was significantly higher in non-government than in government-owned facilities. On average, 23% of residents were reported to have dementia, 27% were bladder incontinent, and 21% were bowel incontinent. Fewer than 8% of residents were physically restrained, and relatively few had pressure ulcers (1%), were tube fed (2%) or were receiving tranquilizers (2%). Again, residents with each of these conditions were more frequently found in non-government than in government-owned facilities.
DISCUSSION
Results from this study are significant in many respects. In this section, the discussion is focused on matters related to institutional ownership and financing—two salient characteristics that define the nature of Chinese elder care institutions and have undergone dramatic transformations over the past 2 decades. Patterns of staffing and resident case-mix are also commented briefly on, followed by study limitations.
The data document the rapid growth of elder care homes in recent years, especially over the last decade, in urban Nanjing and a number of major urban centers. In Nanjing, the government owns 44% of facilities, and most of the growth in recent years is in the non-government sector. In a significant number of these homes, planned expansions are underway. This phenomenon represents a fundamental shift from the not-so-distant past, when institution-based elder care was rare and dominated by government ownership for a highly select social welfare–dependent population.16,17 Looming on the horizon is a rapidly developing industry of formal LTC institutions in urban China.
Accompanying the ownership shift are significant changes in the patterns of financing of institutional elder care. In Nanjing, current facilities rely on private-pay and other non-government sources for more than 80% of their daily operating revenues. The revenue share of private-pay and other non-government sources is much higher in the newer facilities (92%) than in homes built in the 1990s (81%) or before 1990 (39%). These findings suggest that elder care institutions have been increasingly financed through consumers’ private payments and less by government funding, which used to support institutional services.16,20
Regardless of ownership, the majority of homes receive subsidies per occupied bed from the government. Some 85% of non-government homes receive subsidies, although these constitute merely 2% of their daily operating revenues. These seemingly contradictory results are consistent with recent government policy shifts in Nanjing and other Chinese cities. In recent years, the central and local governments have actively encouraged the development of elder care institutions by the private sector through increased financial inducements per bed built for new construction and the aforementioned ongoing subsidies per occupied bed, regardless of type of residents.8,21 The government has implemented welfare reform since the mid 1990s to decentralize the financing and operation of welfare institutions to reduce the cost burden.17,22 The Nanjing municipal government provides financial inducement for new construction in the amount of roughly 2,000 yuan to 4,000 yuan ($300–600) per new bed and an ongoing operating subsidy of approximately 80 yuan (~$12) per occupied bed per month,23,24 but the amounts allocated may vary across districts within the city. These amounts, especially the operating subsidies, are small, but because most residents are paying privately as well, these construction and operating inducements are enough to underpin much of the observed growth.
For non-government facilities, an additional, important dimension of ownership pertains to whether a facility is for profit or not for profit, a distinction that may have a bearing on the quality of care provided, as demonstrated in numerous studies in the West.25 How this distinction is going to affect care quality will probably become an important matter in the future of Chinese LTC. In Nanjing, all non-government facilities are licensed as not-for-profit entities, but in reality, distinguishing between for-profit and not-for-profit operations is complicated, given difficulties in monitoring financial flows within and outside of the facility and because property rules and definitions are different and more nuanced in the Chinese context than is the case in the West.
As with staffing, the data reveal a high proportion of direct-care staff who are rural migratory workers, suggesting that urban elder care homes are becoming an outlet for internal migration. What is unique about these staff is that the majority of them are being housed in the facilities, a finding not surprising given their temporary residence status in the city. By providing housing, it would appear that elder care homes serve an important social solution to the urban housing shortage for rural migrants, consistent with the on-site housing of construction workers routinely seen in Chinese cities.
Few facilities have clinical staff, such as professional nurses and physicians, available. Meanwhile, the sickest residents are more likely to be found in the newest, non-government homes. This suggests that the private sector is meeting the new market demand for seriously impaired older adults who can no longer be cared for at home by families. Furthermore, there are no large differences in staffing levels across different types of homes, suggesting that non-government homes have a higher-acuity case-mix that may not always be appropriate given their current staffing levels.
This profile of current elder care home residents in Nanjing reveals considerable variability across facilities in residents’ functional dependence and acuity levels. Thus, “nursing home,” as generally used in several recent reports on Chinese LTC,11,13,26 would appear to be a poor catch-all term for existing LTC institutions in China. Nonetheless, in historical perspective, the observed heterogeneity in case-mix in today's elder care homes in Nanjing would represent a close view of what U.S. nursing homes were early in the 1960s or 1970s, before the advent of Diagnosis Related Groups, when hospital length of stay was longer and a postacute industry had yet to develop.
This study has several limitations. The primary survey data are restricted to one city, which, like the seven additional cities providing supplemental information, is located in eastern China, limiting the generalization of the findings to other metropolitan areas in the country. Nevertheless, similarities in the observed pattern of growth and ownership shifts across multiple major cities suggest that the findings in Nanjing are likely to be broadly representative of facilities in many other major cities across China. Furthermore, elder care home administrators were relied upon to respond, but it was not possible to audit each facility's finances, although because they did not see the data collectors as part of the government system, and there was not much of a formal inspection process, the administrators had no reason to be wary of their responses. In addition, resident-level data, particularly information about residents’ family situation, social support, and individual circumstances leading to institutionalization, were not collected.
Despite its rapid growth, this new industry of institutional LTC in urban China is smaller than in Europe and the United States, both in terms of the number of facilities and bed supply. Because China's population is aging rapidly, the demand for institutional LTC services will increase, further fueling their development in the decades to come. Based on findings from this study, the greatest growth is anticipated in private and proprietary facilities. Meanwhile, if government construction inducements and ongoing operating subsidies continue, Chinese policy-makers will soon face mounting pressures to develop a more-formal regulatory structure such as that in the United States and other industrialized countries.
ACKNOWLEDGMENTS
The authors appreciate the assistance of the 12 graduate students at the School of Social and Behavioral Sciences, Nanjing University, in the collection of study data.
This study was supported, in part, by a grant from the National Institutes of Health Fogarty International Center (R03TW008142).
Sponsor's Role: The funder had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
IRB Approvals: The institutional review boards of Brown University and Nanjing University approved this study.
Footnotes
Author Contributions: All authors contributed to the study concept and design and participated in analysis and interpretation of data. ZF drafted the manuscript. HJZ, XF, CL, MS, and VM contributed to critical revision of subsequent drafts of the manuscript and agreed on the final version.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
REFERENCES
- 1.Xinhua Net . 100-year old elementary school relocated: Former Dongzhimen Elementary School students no longer scattered around (in Chinese) Beijing Youth Daily; Beijing: Feb 18, 2003. [Google Scholar]
- 2.Osnos E. China Ages at Alarming Rate: Graying Population Clouds Economic Future, Threatens Major Strain on Public-Welfare System. Chicago Tribune; Chicago: 2007. [Google Scholar]
- 3.Zeng Y, George L. Family dynamics of 63 million (in 1990) to more than 330 million (in 2050) elders in China. [February 4, 2011];Demogr Res. 2000 :2. Available at http://www.demographic-research.org/Volumes/Vol2/5/
- 4.Li Q, Reuser M, Kraus C, et al. Ageing of a giant: A stochastic population forecast for China, 2006–2060. J Populat Res. 2009;26:21–50. [Google Scholar]
- 5.Jackson R, Howe N. The Graying of the Middle Kingdom: The Demographics and Economics of Retirement Policy in China. Center for Strategic & International Studies; Washington, DC: 2004. [Google Scholar]
- 6.Kinsella K, He W. An Aging World: 2008. International Population Reports. U.S. Census Bureau; Washington, DC: 2009. [Google Scholar]
- 7.United Nations . World Population Prospects: The 2006 Revision. Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat; New York: 2007. [Google Scholar]
- 8.State Council Information Office [December 12, 2006];China Publishes a White Paper on Its Undertakings for the Aged [on-line] Available at http://www.china.org.cn/english/China/191990.htm.
- 9.Zhan HJ. Chinese care giving burden and the future burden of elder care in life-course perspective. Int J Aging Human Develop. 2002;54:267–290. doi: 10.2190/GYRF-84VC-JKCK-W0MU. [DOI] [PubMed] [Google Scholar]
- 10.Jiang L. Changing kinship structure and its implications for old-age support in urban and rural China. Populat Stud. 1995;49:127–145. [Google Scholar]
- 11.Flaherty JH, Liu ML, Ding L, et al. China: The aging giant. J Am Geriatr Soc. 2007;55:1295–1300. doi: 10.1111/j.1532-5415.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- 12.Zhang H. Who will care for our parents? Changing boundaries of family and public roles in providing care for the aged in urban China. Care Manage J. 2007;8:39–46. doi: 10.1891/152109807780494087. [DOI] [PubMed] [Google Scholar]
- 13.Chu LW, Chi I. Nursing homes in China. J Am Med Dir Assoc. 2008;9:237–243. doi: 10.1016/j.jamda.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Wu B, Carter MW, Goins RT, et al. Emerging services for community-based long-term care in urban China: A systematic analysis of Shanghai's community-based agencies. J Aging Soc Policy. 2005;17:37–60. doi: 10.1300/J031v17n04_03. [DOI] [PubMed] [Google Scholar]
- 15.Wu B, Mao Z, Xu Q. Institutional care for elders in rural China. J Aging Soc Policy. 2008;20:218–239. doi: 10.1080/08959420801977632. [DOI] [PubMed] [Google Scholar]
- 16.Shang X. Moving toward a multi-level and multi-pillar system: Changes in institutional care in two Chinese cities. J Soc Policy. 2001;30:259–281. [Google Scholar]
- 17.Wong L, Tang J. Non-state care homes for older people as third sector organisations in China's transitional welfare economy. J Soc Policy. 2006;35:229–246. [Google Scholar]
- 18.Zhan HJ, Liu G, Guan X, et al. Recent developments in institutional elder care in China: Changing concepts and attitudes. J Aging Soc Policy. 2006;18:85–108. doi: 10.1300/J031v18n02_06. [DOI] [PubMed] [Google Scholar]
- 19.Chen G, Liang J. Nanjing Publishing House; Nanjing: 2008. Population and Socioeconomic Development in Nanjing (in Chinese). [Google Scholar]
- 20.Ikels C. Maddox G, Lawton MP, editors. Chinese kinship and the state: Shaping of policy for the elderly. Annu Rev Gerontol Geriatr. 1993;13:123–146. [Google Scholar]
- 21. [February 4, 2011];Xinhua News. Beijing Encourages Private Nursing Homes. April 19, 2005 [online] Available at http://www.china.org.cn/english/Life/126277.htm.
- 22.Croll EJ. Social welfare reform: Trends and tensions. China Quart. 1999:684–699. doi: 10.1017/s030574100000343x. [DOI] [PubMed] [Google Scholar]
- 23. [March 26, 2010];Jiangsu News. Subsidies of 80 Yuan per Resident per Month to Non-government Owned Elder Care Homes (in Chinese) [on-line] Available at http://jsnews.jschina.com.cn/nj/201003/t346244.shtml.
- 24.Xinhua Net [August 28, 2009];Converting a Community Hospital into Elderly Rehab Center Should Not Be That Difficult (in Chinese) [on-line] Available at http://www.js.xinhuanet.com/xin_wen_zhong_xin/2009-08/28/content_17527859.htm.
- 25.Comondore VR, Devereaux PJ, Zhou Q, et al. Quality of care in for-profit and not-for-profit nursing homes: Systematic review and meta-analysis. BMJ. 2009;339:2732. doi: 10.1136/bmj.b2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flaherty JH. Nursing homes in China? J Am Med Dir Assoc. 2009;10:453–455. doi: 10.1016/j.jamda.2009.06.006. [DOI] [PubMed] [Google Scholar]