Abstract
Spontaneous intracranial hypotension (SIH) is a cause of new persistent headache, which disappears on recumbence and reappears in sitting/standing position (orthostatic headache). We present a case of orthostatic headache, where the patient was suspected to have SIH and was subjected to radionuclide cisternography (RNC) using 99m Technetium Diethylenetriaminepenta acetic acid for confirmation of diagnosis. After due consent from the patient, the radiotracer was injected intra-thecally and serial images were acquired until 24 h. The direct and indirect evidences of Cerebrospinal fluid (CSF) leakage, which were revealed in our study, provided objective evidence to the clinical diagnosis. RNC is an important investigation in diagnosing SIH and also identifying the site of CSF leak, which may aid the management.
Keywords: Cerebrospinal fluid leakage, orthostatic headache, radionuclide cisternography, spontaneous intracranial hypotension
INTRODUCTION
The international classification of headache disorders recognizes three subsets of low volume headache, one of them being Spontaneous intracranial hypotension (SIH).[1] SIH has been attributed to a breach of dural diverticulae or tearing of nerve root sheaths. There may be a clear trigger or at times it may occur without a precipitant.
SIH is not a common syndrome and clinical manifestations at times may make the diagnosis difficult. Detection of Cerebrospinal fluid (CSF) leak by radionuclide methods helps diagnosing SIH. We present a case where RNC was helpful in confirming the diagnosis of a suspected SIH.
CASE REPORT
A 31-year-old male presented to us with the chief complaints of headache and diplopia. The symptoms presented 15 days back when he suddenly developed occipital headache with neck stiffness followed by multiple episodes of vomiting occurring in the next 24 h. The pain was relieved within 15 min of lying down and recurred after 15 min of upright posture. This was followed by complaints of tinnitus and hyperacusis. A day later he also developed diplopia on looking to the left side. There was no history of fever, limb weakness, associated ear or nasal discharge, any trauma or prior lumbar puncture.
A lumbar puncture revealed low CSF opening pressure and on analysis, normal sugar, high protein content of 200 mg/dl with 10 cells (all lymphocytes) was seen. No organisms were seen on microscopy and culture was negative. A Magnetic resonance imaging (MRI) brain with gadolinium contrast was performed, which showed diffuse pachymeningeal enhancement [Figure 1]. SIH was suspected and the patient was referred to the Department of Nuclear Medicine for radionuclide cisternography (RNC).
Figure 1.
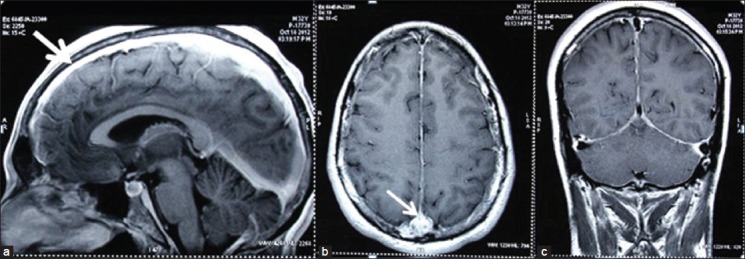
Gadolinium enhanced T1 weighted (1a) Sagittal (1b) Axial and (1c) coronal magnetic resonance imaging (MRI) images showed diffuse and linear enhancement of the meninges along the entire cerebral convexities (thick arrow) and the inter hemispheric fissure (thin arrow)
After explaining the procedure, a written consent was obtained from the patient and 10 mCi of 99m Technetium Diethylenetriaminepenta acetic acid was injected via a lumbar puncture into the sub-arachnoid space. Serial images were obtained (Philips Precedence 16 single-photon computed emission tomography — computed tomography [SPECT-CT]) in anterior, posterior, and lateral views with the patient in supine position at 1 h, 2 h, 4 h and 24 h. Gradual ascent of tracer was seen along the spinal axis. There was early visualization of the kidneys and bladder on the 1 h delayed image [Figure 2]. Subtle extra-dural tracer accumulation of radiotracer was noted in the region of upper thoracic spine on the right side in the 2 h anterior and posterior delayed images [Figure 2]. Inadequate ascent of tracer over the higher cerebral convexities was noted in the 24 h delayed image [Figure 2].
Figure 2.
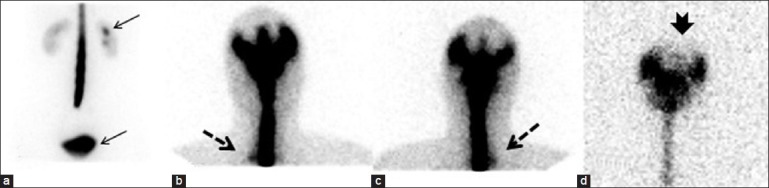
Anterior and posterior images of 99m Technetium Diethylenetriaminepenta acetic acid cisternography in a patient of spontaneous intracranial hypotension. (2a) 1 h anterior view of lumbar region showed early visualization of both kidneys and bladder (thin arrows). (2b) 2 h anterior view and (2c) 2 h posterior view images showed mild extra-dural radiotracer accumulation in the region of right upper thoracic spine (dotted arrows). (2d) 24 h posterior view image showed inadequate ascent of tracer over the higher cerebral convexities (notched arrow)
Patient started recovering with bed-rest and good hydration, and was discharged after full recovery with conservative management.
DISCUSSION
SIH is a rare syndrome with incidence estimated at 5/100,000 per year and a female preponderance.[2] The pathogenesis is considered to be related to CSF leak via small dural defects leading to a reduction in CSF volume and thus CSF pressure.[3,4] The most common presentation is with a postural headache, which is characteristically exacerbated by upright position and relieved when the patient is recumbent. The pain can be severe, incapacitating and constant or throbbing. It may be generalized or localized to the frontal or occipital region. It may be associated with nausea, vomiting, neck stiffness, horizontal diplopia, blurring of vision, photophobia, field defects, vertigo, tinnitus, dysgeusia, unilateral facial numbness, and weakness.[3,5,6,7] Conservative methods like bed rest are the first line treatment.[8] If not effective, interventional methods like autologous epidural blood patch are used. A report suggested that early blind epidural blood patching within one week of onset is effective; demonstrating complete cure in 77% patients after one (57%) or two (20%) blood patches.[9]
CSF opening pressure on lumbar puncture is low (less than 60 mmHg) or even normal. CSF analysis may be normal or show lymphocytic pleocytosis, increased protein content and normal glucose levels. Cytology and bacteriology are normal.[3,5] An MRI with gadolinium contrast is regarded as a more useful investigation in comparison to a brain CT scan. The MR image appearance in SIH is usually diffuse pachymeningeal enhancement limited to the duramater,[5,7] most likely cause being compensatory dilatation of the dural veins. The leakage site is not easy to detect in a brain MRI since the whole spine scan is not available in most cases.
RNC is the key diagnostic investigation for SIH. It was introduced in 1964 by Dichiro[10] and in most of the reported cases it has been shown to be a sensitive tool to detect CSF leak,[3,6,7] to guide the level of injection of blood patch for leak suppression and to evaluate the therapeutic effect. There are two kinds of findings seen on a RNC done for SIH, the Direct and the Indirect or surrogate signs of CSF leakage. The direct sign of leak is diffusion and accumulation of radiotracer into the extra-arachnoid space. The surrogate markers of CSF leak include limited ascent of the tracer to the cerebral convexities in most of the cases and early appearance of radiotracer in the bladder suggestive of unusually rapid uptake of the radiotracer into the circulation via the epidural venous plexus. Direct evidence of leak is seldom described, perhaps because of the leakage below the limit of resolution of the study.[11] Our patient showed only subtle extradural leakage, which might have been easily overlooked. However, the indirect signs are sufficient to establish a diagnosis of CSF leakage. Thus, in our case, RNC documented both indirect and direct signs and clearly localized CSF leak site in the upper portion of thoracic spine.
In conclusion, RNC is an effective method in diagnosing and localizing CSF leakage in a case with suspected SIH. It is worthwhile applying RNC to evaluate postural headache in patients without a remarkable history of trauma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. Cephalalgia. (2nd edition) 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286–96. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]
- 3.Rando TA, Fishman RA. Spontaneous intracranial hypotension: Report of two cases and review of the literature. Neurology. 1992;42:481–7. doi: 10.1212/wnl.42.3.481. [DOI] [PubMed] [Google Scholar]
- 4.Pannullo SC, Reich JB, Krol G, Deck MD, Posner JB. MRI changes in intracranial hypotension. Neurology. 1993;43:919–26. doi: 10.1212/wnl.43.5.919. [DOI] [PubMed] [Google Scholar]
- 5.Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc. 1997;72:400–13. doi: 10.4065/72.5.400. [DOI] [PubMed] [Google Scholar]
- 6.Chung SJ, Kim JS, Lee MC. Syndrome of cerebral spinal fluid hypovolemia: Clinical and imaging features and outcome. Neurology. 2000;55:1321–7. doi: 10.1212/wnl.55.9.1321. [DOI] [PubMed] [Google Scholar]
- 7.Spelle L, Boulin A, Tainturier C, Visot A, Graveleau P, Pierot L. Neuroimaging features of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 1997;62:291–2. doi: 10.1136/jnnp.62.3.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goadsby PJ, Boes C. New daily persistent headache. J Neurol Neurosurg Psychiatry. 2002;72:ii6–ii9. doi: 10.1136/jnnp.72.suppl_2.ii6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berroir S, Loisel B, Ducros A, Boukobza M, Tzourio C, Valade D, et al. Early epidural blood patch in spontaneous intracranial hypotension. Neurology. 2004;63:1950–1. doi: 10.1212/01.wnl.0000144339.34733.e9. [DOI] [PubMed] [Google Scholar]
- 10.Dichiro G. NEW radiographic and isotopic procedures in neurological diagnosis. JAMA. 1964;188:524–9. [PubMed] [Google Scholar]
- 11.Hsu C, Chen Y, Chuang Y, Huang Y. Radionuclide cisternography in spontaneous intracranial hypotension: A case report and literature review. Ann Nucl Med Sci. 2004;17:45–50. [Google Scholar]


