Abstract
Marijuana is used for psychoactive and recreational purpose. We report a case of fulminant hepatic failure following marijuana drug abuse who recovered following artificial support systems for acute liver failure. There is no published literature of management of marijuana intoxication with molecular adsorbent recirculation system (MARS). MARS is effective and safe in patients with fulminant hepatic failure following marijuana intoxication.
Keywords: Acute fulminant hepatitis, marijuana intoxication, molecular adsorbent recirculation system therapy
Introduction
Marijuana is found to have many physiological and pathophysiological functions, including mood alteration, motor and co-ordination activities. It is used for psychoactive and recreational purposes. The literature on hepatotoxicity following marijuana toxicity is scarce. There is no literature on molecular adsorbent recirculation system (MARS) therapy for hepatotoxicity following marijuana drug abuse. We report a case of fulminant hepatic failure following marijuana drug abuse successfully managed with MARS therapy.
Case Report
A 23-year-old male college student presented to the emergency department with a history of malaise, fatigue and vomiting of 1 week duration. He also had a history of yellowish discoloration of the sclera and breathlessness of 3 days and developed altered sensorium a day prior to presentation. There was no history of oliguria, hematuria, dysuria or graveluria. There was no history of focal weakness of limbs or seizures and bleeding manifestations. He had no significant past medical, surgical or family history. He had no drug allergy. His father gave a history of marijuana abuse for the past few months and denied history of smoking and alcohol. On examination, he was irritable pale and icteric, blood pressure was 130/80 mmHg. Cardio-respiratory examination was unremarkable. Abdomen was soft and showed no evidence of hepatosplenomegaly. Neurological examination revealed no evidence of focal neurological deficit or meningeal signs of irritation. His laboratory parameters are given in Table 1.
Table 1.
Sequential laboratory parameters of patient
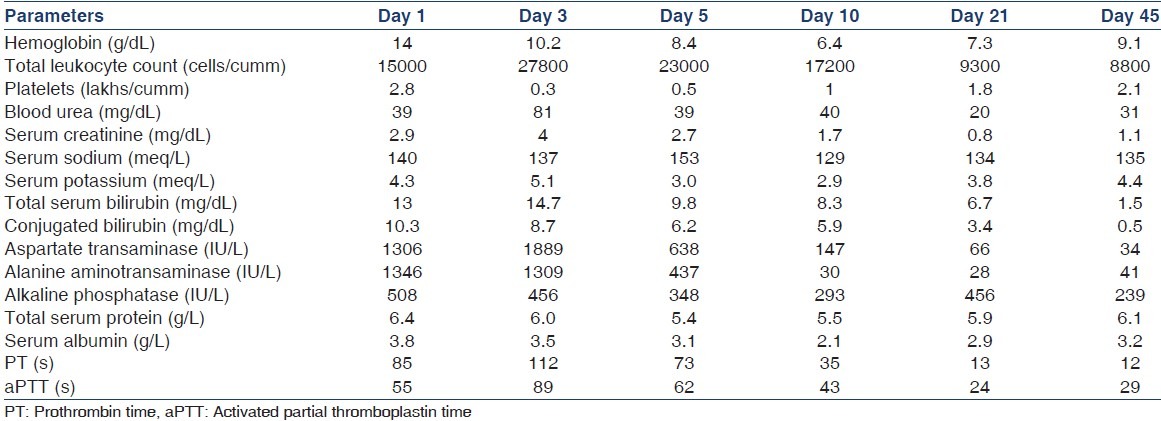
Tests for hepatitis A, hepatitis B, hepatitis C and E, human immunodeficiency virus, cytomegalovirus, parvovirus, Wilson’s disease, autoimmune hepatitis and acetaminophen induced hepatitis were all negative. Chest radiograph and ultrasonogram of the abdomen were normal. Blood and urine culture were sterile. Peripheral smear for malaria parasite, anti-dengue antibodies and leptospira serology were all negative. Cerebrospinal fluid analysis was unremarkable. Blood and urine for tetrahydrocannabinol (THC) were positive. The diagnosis of acute fulminant hepatitis secondary to marijuana abuse was considered as other causes of fulminant hepatic failure were all ruled out and blood and urine were positive for THC. He was given supportive care and antibiotics. His condition worsened over the next 2 days and developed respiratory distress requiring intubation and ventilator support. Sequential laboratory reports are shown in Table 1. On the 3rd day, he was initiated on extra-corporal liver-purification system; MARS. After three sessions of MARS, each lasting 8 h, there was a remarkable improvement in level of sensorium and biochemical parameters. He was extubated on the 6th day and by 10th day his liver parameters came down remarkably. He was discharged after 3 weeks. On follow-up, his biochemical parameters were normal.
Discussion
The main active chemical in marijuana is delta-9-THC discovered in 1964.[1] It was found to have many physiological and pathophysiological functions, including mood alteration, control of feeding and appetite, motor and co-ordination activities, analgesia, immune modulation and gut motility. It is used for psychoactive and recreational purposes.[2,3] Marijuana toxicity usually produces drowsiness, disorientation, confusion, cognitive disorganization, impaired judgment, hallucinations, paranoia and rarely toxic psychosis. Until 1969, there was no literature on hepatotoxicity following marijuana toxicity. Later, there have been several reports of hepatoxicity following marijuana chronic over dosage. The prevalence of hepatotoxicity, ranging from 17% to 66.7%[4] is higher when consumed in combination with alcohol. In a recent study by Borini et al.,[5] among users of only marijuana, hepatomegaly was observed in 57.7% and splenomegaly in 73.1% and slightly elevated aspartate transaminase, alanine aminotransaminase and alkaline phosphatase in 42.3%, 34.6% and 53.8% respectively. We report an unusual case of fulminant hepatic failure following marijuana drug abuse as other causes of fulminant hepatic failure were all ruled out and blood and urine for active metabolite of marijuana, THC was positive.
There is no specific antidote for marijuana overdose or ingestion. Activated charcoal may prevent further absorption from the gut if ingestion is within a couple of hours, but clinical data is lacking on efficacy. It is not possible to enhance elimination of THC from the blood or tissues. Benzodiazepine was considered for patients presenting with anxiety. The effect of cannabinoid antagonist, 41716A [N-(piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide hydrochloride] in animal models of rat and rhesus monkey produced reversible, dose-dependent antagonism of the discriminative stimulus properties of delta 9-THC.[6] However, the effect of SR141716A on blocking or reversing the cannabis intoxication in humans is lacking.
The most important aspect of treatment of fulminant hepatic failure is to provide good intensive care support. Careful attention should be paid to fluid management and hemodynamics. Monitoring of metabolic parameters, surveillance for infection, maintenance of nutrition, and prompt recognition of gastrointestinal bleeding are crucial. Though artificial support systems for kidney failure have been widely available for the past several decades, it is only recently that they have become a promising treatment modality for fulminant hepatic failure. They are mainly used temporarily as a bridge to liver transplantation or until the liver regenerates and to date, have no impact on survival.[7,8] It is thought that toxins contribute to the clinical picture of fulminant hepatic failure. These mechanical liver-support devices filter toxins. MARS was designed to remove large molecular and albumin bound toxins. MARS is performed with an albumin-containing dialysate, which is recycled in a closed loop that contains a charcoal cartridge, an anion exchanger resin adsorber and a conventional hemodialyzer. It was 1st applied in the treatment of acute liver failure in 1993 by stange et al.[9] Thereafter it has been used as a bridge to liver transplantation.[10,11] It has also been used to treat various poisoning with or without liver failure such as acetaminophen, amanita phalloides, phenytoin, lamotrigine, theophylline and calcium channel blockers.[12] To date there is no published literature on the use of MARS therapy for hepatotoxicity following marijuana drug abuse.
We report a patient with hepatotoxicity following marijuana abuse successfully managed with MARS therapy. However, it is unclear whether THC is also removed by MARS, which needs further investigation.
Conclusion
MARS is an effective and safe means of treating fulminant hepatic failure of any etiology. However, studies are required to focus on the optimal timing of initiation and intensity of MARS albumin liver dialysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gaoni Y, Mechoulam R. Isolation, structure and partial synthesis of an active constitute of Hashish. J Am Chem Soc. 1964;80:1646. [Google Scholar]
- 2.Mechoulam R. The pharmacohistory of cannabis sativa. In: Mechoulam R, editor. Cannabinoids as Therapeutic Agents. Boca Raton: CRC Press; 1986. pp. 1–18. [Google Scholar]
- 3.Indian Hemp Drugs Commission Marujuana: Report of the Indian Hemp Drug Commission 1893-1894. Maryland Silver Spring: 1969. [Google Scholar]
- 4.Hochman JS, Brill NQ. Chronic marihuana usage and liver function. Lancet. 1971;2:818–9. doi: 10.1016/s0140-6736(71)92771-1. [DOI] [PubMed] [Google Scholar]
- 5.Borini P, Guimarães RC, Borini SB. Possible hepatotoxicity of chronic marijuana usage. Sao Paulo Med J. 2004;122:110–6. doi: 10.1590/S1516-31802004000300007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiley JL, Lowe JA, Balster RL, Martin BR. Antagonism of the discriminative stimulus effects of delta 9-tetrahydrocannabinol in rats and rhesus monkeys. J Pharmacol Exp Ther. 1995;275:1–6. [PubMed] [Google Scholar]
- 7.Santoro A, Mancini E, Buttiglieri S, Krause A, Yakubovich M, Tetta C. Extracorporeal support of liver function (II part) Int J Artif Organs. 2004;27:176–85. doi: 10.1177/039139880402700304. [DOI] [PubMed] [Google Scholar]
- 8.Rifai K, Ott M, Bahr MM, Schneider A, Manns MP. Liver replacement therapy. Reliable indications in acute liver failure. Internist (Berl) 2003;44:1485–90. doi: 10.1007/s00108-003-1076-4. [DOI] [PubMed] [Google Scholar]
- 9.Stange J, Mitzner S, Ramlow W, Gliesche T, Hickstein H, Schmidt R. A new procedure for the removal of protein bound drugs and toxins. ASAIO J. 1993;39:M621–5. [PubMed] [Google Scholar]
- 10.Stange J, Mitzner SR, Risler T, Erley CM, Lauchart W, Goehl H, et al. Molecular adsorbent recycling system (MARS): Clinical results of a new membrane-based blood purification system for bioartificial liver support. Artif Organs. 1999;23:319–30. doi: 10.1046/j.1525-1594.1999.06122.x. [DOI] [PubMed] [Google Scholar]
- 11.Stange J, Mitzner SR, Klammt S, Freytag J, Peszynski P, Loock J, et al. Liver support by extracorporeal blood purification: A clinical observation. Liver Transpl. 2000;6:603–13. doi: 10.1053/jlts.2000.7576. [DOI] [PubMed] [Google Scholar]
- 12.Wittebole X, Hantson P. Use of the molecular adsorbent recirculating system (MARS™) for the management of acute poisoning with or without liver failure. Clin Toxicol (Phila) 2011;49:782–93. doi: 10.3109/15563650.2011.624102. [DOI] [PubMed] [Google Scholar]


