Abstract
Background:
In hair transplantation, the survival rate of harvested grafts depends upon many factors like maintenance of hydration, cold temperature, reduced mechanical handling and asepsis. All these factors are favourably improved if time out of body is reduced significantly. We have tried a modification called direct hair transplantation in the existing follicular unit extraction technique, in which the follicular unit grafts are implanted as soon as they are harvested. In this article, we have described the detailed methodology and a series of 29 patients who underwent direct hair transplantation.
Aim:
To evaluate the efficacy and feasibility of direct hair transplantation.
Subjects and Methods:
The patients willing to undergo hair transplantation by the technique of follicular unit extraction were enrolled for the surgery. After administration of local anaesthesia, the recipient sites were created. Thereafter, the processes of scoring the skin with a motorized punch, graft extraction and implantation were performed simultaneously. These patients were followed up to look for the time period of initiation of hair growth, the growth achieved at the end of 6–8 months and any adverse events. The results of patients with noticeable improvement in the photographs and reduction in baldness grade were taken as ‘good’, whereas, in other patients, it was classified as ‘poor’.
Results:
All patients were males with age ranging from 21 to 66 years (median 30 years). Twenty-six patients had androgenetic alopecia, 1 patient had traction alopecia and 2 patients had scarring alopecia. Twenty-seven patients showed ‘good’ results, whereas 2 patients showed ‘poor’ results.
Conclusion:
Direct hair transplantation is a simple and feasible modification in the follicular unit extraction technique. It is an efficacious surgical treatment modality for baldness.
Keywords: Androgenetic alopecia, follicular unit extraction, hair transplantation
INTRODUCTION
Hair transplantation is a surgical modality for the treatment of androgenetic alopecia.[1] Hair follicles in the occipital scalp are harvested and then planted on to the frontal scalp, and less often to the vertex. There are two methods of harvesting the follicles from the occipital scalp. In the first method, also called follicular unit transplantation (FUT), a strip is harvested from the occipital scalp, whereas in the second method individual follicular units are harvested. The latter is called follicular unit extraction (FUE).[1]
The survival rate of the harvested graft depends upon multiple exogenous factors. The most important ones are graft hydration, cold temperature, prevention of infection and mechanical trauma.[2] The transit time between graft harvesting and implantation is also an important determinant of the survival rate.[2,3] The transit time, if reduced to a large extent, significantly improves the rate of graft survival by favourably improving all the other factors. It will reduce the chances of desiccation, infection, mechanical trauma, and grafts getting heated up. So, we tried a modification called direct hair transplantation (DHT), in which we implanted the graft as soon as it was harvested.
SUBJECTS AND METHODS
All patients willing to undergo FUE technique of hair transplantation were explained about this modification of DHT, its advantages and the minor procedural differences. After a detailed counselling, the patients willing to undergo DHT were enrolled for the surgery.
Pre operative evaluation
Blood investigations were performed which included haemoglobin, total leukocyte count, differential leucocyte count, platelet count, bleeding time, clotting time, prothrombin time, activated plasma thromboplastin time, random blood sugar, anti-retrovirus 1 and 2 serology, Hepatitis B surface antigen and anti Hepatitis C were performed. The blood pressure and body weight were also recorded. A clearance for hair transplant surgery was taken from general physician and if all the tests were normal, then a written informed consent was taken for the surgery.
Step 1: Administration of local anaesthesia
Position
The patient was made to lie down on the operation theatre table in prone and supine positions for the complete ring block.
The ring block was administered in the frontal and occipital scalp using a 31 G needle, infiltrating 2% xylocaine with adrenaline. Thereafter, tumescent anaesthesia was administered using 30 ml normal saline, 30 ml of 2% xylocaine, 1 ml triamcinolone (40 mg/ml), half ampoule (0.5 ml) of adrenaline (1:1000), and 4 ml of bupivacaine (5 mg/ml).
After administering, the tumescent anaesthesia, 3-4 test grafts are scored and extracted (details described in step 3), to look for the size and length of the grafts.
Step 2: Creation of recipient sites
Position
Supine
Then, we created the recipient sites in the frontal scalp using a cut to size blade mounted on the handle. While creating the sites, they were counted simultaneously and the sites equal to the number of planned grafts were made.
Step 3: DHT
Position
The patient was made to sit on a stool (height 45 cm., width 43 cm) with the head reclining forwards and resting on a comfortable pillow placed upon a table (height 93 cm., width 38 cm.). After this, the physician stood on the left side of the patient. The operating physician wore medical loupes with 4× magnifications, and working distance of 50 cm.
Position 1
Patient looking towards his left side while resting his right cheek and temporal area on the pillow [Figure 1].
Figure 1.

Patient looking towards left side
Position 2
Patient looking towards his right side and resting his left cheek and temporal area on the pillow [Figure 2].
Figure 2.

Patient looking towards his right side
Position 3
Patient looking downwards and his forehead resting on the edge of the stool [Figure 3].
Figure 3.

Patient looking downwards
The graft extraction was carried out in 2 stages. The first stage, also called ‘scoring’ involved making the skin incision using 0.9 mm blunt punch and the motorized SAFE SCRIBETM (introduced by Dr. James Harris, USA). The dull punch was advanced inside the skin up to 2.5–3 mm. The second stage, involved extraction of the grafts that were scored using the forester forceps (Ellis instruments, USA). While the process of scoring was going on, simultaneous graft extraction and implantation was initiated. After scoring for 100–150 grafts, which took around 5–10 minutes, the patient was made to sit erect and the head was lifted off the table. By this time, most of the grafts had been extracted and some of them had been implanted. Thereafter, in the erect position, the remaining grafts were extracted and implantation of all the extracted grafts was completed. In this position, some of the buried or the grafts difficult to extract were extracted by the physician. Also, regions requiring high density were implanted by the physician.
Thereafter, the scoring was again restarted in the adjacent donor region by the physician sitting on the left side of the patient. Thus, the ‘time out of body’ or the transit time varied from 1 minute to 5 minutes.
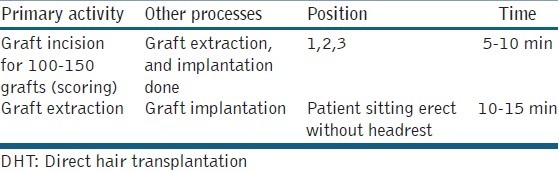
Approximate time period elapsed in the various steps of transplantation is summarized in Table 1.
Table 1.
Two stages of DHT
Surgical assistants were allocated the duty of counting the harvested grafts (as singles, doubles, triples and 4/5 haired grafts) and continuously spraying cold normal saline on to the planted grafts in the frontal scalp. After the surgery, the patient was advised to have betadine scrub at the occipital scalp, and normal saline spray on the frontal planted area. Antibiotics in the form of amoxicillin-clavulanic acid combination and anti-inflammatory agents in the form indomethacin-serratiopeptidase combination were prescribed for 7 days. Thereafter, patients were followed-up at monthly intervals.
The time period at which the growth started becoming noticeable and became significantly appreciable were noticed. The results were classified into 2 categories:
Patients with ‘good’ growth: Those who had noticeable photographic improvement and reduction in baldness grade according to the basic and specific classification (BASP) of male patterned baldness.[4]
Patients with ‘poor’ growth: Those who didn’t have noticeable photographic improvement and no reduction in the baldness grade according to the BASP of male patterned baldness.[4]
RESULTS
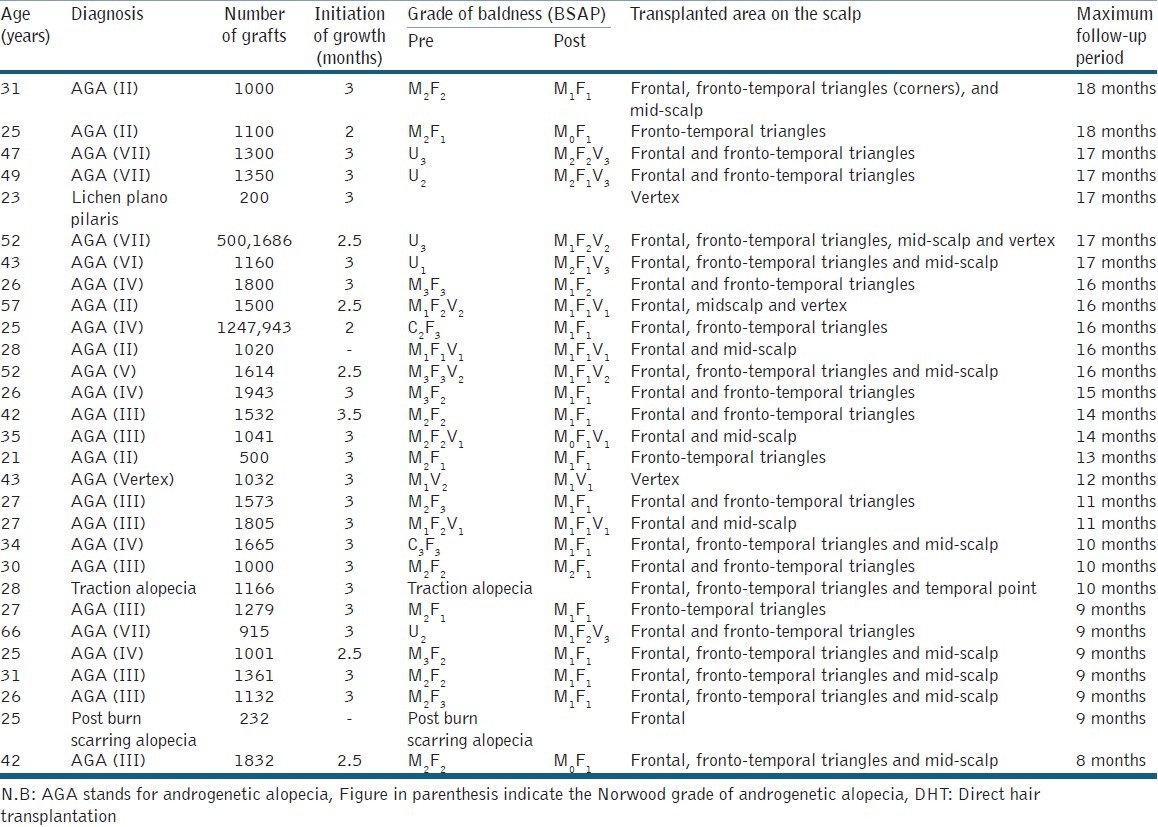
All the patients were males with age ranging from 21 to 66 years. All patients had androgenetic alopecia with Norwood grades ranging from grade II to VII, except 3 patients who had lichen plano-pilaris, post burn scarring alopecia and tractional alopecia. Their hair growth started becoming visible after 2–3 months and ‘good’ results were obtained in 27 patients after a follow up period varying from 8 to 18 months. The patients who had ‘poor’ result included one patient with grade II pattern of baldness with diffuse thinning of frontal scalp and another patient with scarring alopecia who underwent grafting of 232 grafts. Some of the patient with ‘good’ results are shown in Figures 4 and 5.
Figure 4.

(a) Pre operative photograph of patient with traction alopecia (b) Post operative photograph of patient with traction alopecia (1166 grafts)
Figure 5.

(a)Pre-operative operative photograph of patient 12 (1614 grafts) (b)Post operative photograph of patient 12 after 10 months (1614 grafts)
The details of the patients undergoing this DHT procedure have been summarized in the Table 2.
Table 2.
Summary of patients undergoing DHT
The adverse events noticed were persistent pain due to perineural inflammation in donor region in two patients which subsided after 2–3 months. One patient was administered tablet paracetamol 500 mg twice a day for 10 days and then only in case of pain. The other patient was prescribed methycobalamin for 2 months after consulting with neurologist. No other significant adverse events were noted in other patients.
DISCUSSION
There have been a lot of innovations in the current medical practice of hair transplantation. The concept of FUE or the Follicular unit extraction) procedure was first described by Rassman et al.[5] This method has advantages of avoiding a linear scar and less post-operative pain. However, it has disadvantages of increased surgical times, graft fragility and increased cost to the patient.[6] In 2006, a new innovative instrument called the surgically advanced follicular extraction (SAFE) system was introduced by Dr. Harris, with extremely low transaction rates of an average 6.14%.[7] All the pioneers in this field have developed their modifications in the extraction technique, and it has been variably described as the Wood’s, FUSE and the CIT technique.[8–10]
Great advances are being made in the field of hair transplant surgery with the aim of optimizing the results. Bernstein et al., proposed certain key points to consider ensuring maximum graft survival. First, the graft remains susceptible to injury from the moment it leaves the body and is totally secure at the recipient site (i.e., until 8th postoperative day). In another study, they demonstrated the chances of mechanical graft dislodging are reduced by 6th day, there was no risk by the 9th day and prevention of crusting formation reduced the time during which the graft is at the risk of dislodgement. Second, they emphasize continuous supervision of the staff throughout the procedure to ensure optimal graft handling. Other factors reducing graft survival are mechanical injury (transaction during dissection, crushing by forceps during implantation), dehydration, chemical solutions, heat and hypoxia. Last but not the least, desiccation is the most damaging injury.[11]
Desiccation has been proven to be the most damaging injury in another study by Gandelman et al. They found that significant light and electron microscopic changes were observed in the grafts subject to desiccation. No such changes were observed in the grafts subject to controlled crushing, bending or stretching.[12]
Another important factor termed as the ‘H’ or the ‘Human’ factor was proposed as the cause of many poor results by Greco. He suggested that improper graft handling during all stages of the surgery, staff fatigue or a cavalier attitude to graft handling were the contributor to the ‘H-factor’.[13]
This concept of immediate graft implantation has been mentioned by Rose et al.[14] However, at the time of performing FUE, it seemed difficult to do immediate implantation after extraction in all the positions. Therefore, we did some modifications in the standard FUE procedure to make it possible and called it DHT. The standard FUE procedure involves three steps: Graft extraction, followed by creation of recipient sites and then graft implantation.[15] However, for the DHT technique, we changed the above mentioned sequence of events. We first created the recipient sites and then started the procedure of graft extraction and immediate graft implantation. We also devised specialized patient sitting stool and head-resting table for this purpose [Figures 1–3]. In the stage 2 of DHT [Table 1], when the patient’s head is in the erect position, the grafts that are difficult to extract and implant are done by the physician only. As the physician is the most experienced member of the team, the difficult grafts are not wasted and are implanted without mechanical trauma. While the physician is scoring the skin with the blunt punch, the surgical assistants are simultaneously busy in extracting and implanting the grafts. Thus, more people are working at a time and the whole process is better streamlined to ensure better graft survival. Lastly, there is no need of storing the grafts in any storage solution like chilled-ringer lactate, normal saline or platelet rich plasma unlike in the standard FUE procedure.
In the standard FUE procedure, the time taken for extraction of all the grafts varies from 1–3 h (depending upon the number of grafts and the extraction speed of the surgeon, which varies from 500–1000 grafts/h). Thereafter, the time taken for creation of recipient sites varies from 15–30 min and for graft implantation, it varies from 1 to 2 h. Thus, the ‘time out of body’ of the harvested grafts varies from 1 to 2 h. But, in the DHT procedure, since the steps of scoring, extraction and implantation are initiated simultaneously, the ‘time out of body’ of the harvested grafts varies from 2 to 20 min. To complete the 2 stages of DHT [Table 1] for every 100–150 grafts, the time period varies from 10 to 25 min.
The advantages of reducing the ‘time out of body’ of the harvested grafts are manifold. First and foremost, the survival rates are improved. Limmer performed an in vivo ‘time out of body’ study using chilled NS with follicular unit grafts to study the micrograft survival rates. The results were, 2 h, 95%; 4 h, 90%; 6 h, 86%; 8 h, 88%; 24 h, 79%; 48 h, 54%. He related a good ‘rule of thumb’, stating that the loss was roughly 1%/h. Better storage solutions may improve these statistics.[3] Second, since the FUE grafts are more skinny and fragile than the FUT grafts, they are likely to grow better if implanted soon after extraction. Third, the standard FUE procedure involves the role of operating physician during the initial extraction process only. Thereafter, the implantation is performed by surgical assistants making the possibility of improper graft handling. The need for continuous staff supervision is obviated in the DHT technique. The harvested grafts always remained in front of the eyes of the operating physician, so the chances of graft handling by the staff are minimized. Lastly, the standard FUE procedure requires the patient to lie prone during scoring and graft extraction (initial 3–4 h), whereas, in DHT, the patient remains in sitting position during the whole process. During this period, the patient discomfort is more in FUE as compared to DHT.
The disadvantage faced in the DHT method is that the ease of implantation is less in sitting position.
In a recent paper, by Bernstein et al., an idea of pre-making the recipient sites and thereafter, a deliberate delay (up to 24 h) has been proposed as additional measures to increase graft survival. They proposed that by making the sites first, the time grafts are out of the body will be reduced and a deliberate delay will make the older sites to exhibit stickiness, which makes it easier to place grafts and have less popping.[15]
The FUE technique is a well-established method of hair restoration nowadays, and we agree that the experienced FUE surgeons who have high extraction speeds of 500–1200 grafts/h can extract and implant the grafts with 1–2 h. If the graft storage is done under ideal conditions of cold temperature and hydration is maintained, then the graft survival is fine and the results of the surgery are good. The aim of describing this technique is just to outline another way of performing FUE. It is a well-known fact that hair transplant surgery is a combination of art and science. All the well-established surgeons, at both national and international level, have minor as well as major differences in their techniques of hair transplantation. But, they have mastered their own methods by continuous practice. Similarly, to attain mastery in the DHT technique, constant practice and diligence is required.
CONCLUSION
DHT procedure significantly reduces the transit time as compared to the current procedure of FUE, and thus minimizes the physical handling, mechanical trauma, chances of desiccation, hypoxia, infection and grafts getting heated up. It is an efficacious surgical modality for hair restoration. Although it may appear slightly more difficult and longer procedure for the traditional FUE surgeon in the beginning, with more practice and after improvement of expertise, it may take lesser time and turn out to be easier.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bernstein RM, Rassman WR. Follicular unit transplantation. In: Haber RS, Stough DB, editors. Hair Transplantation. Philadelphia: Elsevier Saunders; 2006. pp. 91–8. [Google Scholar]
- 2.Parsley WM, Perez-Meza D. Review of factors affecting the growth and survival of follicular grafts. J Cutan Aesthet Surg. 2010;3:69–75. doi: 10.4103/0974-2077.69014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Limmer R. Micrograft survival. In: Stough D, Haber R, editors. Hair Replacement. St. Louis: Mosby; 1996. pp. 147–9. [Google Scholar]
- 4.Lee WS, Ro BI, Hong SP, Bak H, Sim WY, Kim do W, et al. A new classification of pattern hair loss that is universal for men and women: Basic and specific (BASP) classification. J Am Acad Dermatol. 2007;57:37–46. doi: 10.1016/j.jaad.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 5.Rassman WR, Bernstein RM, McClellan R, Jones R, Worton E, Uyttendaele H. Follicular unit extraction: Minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28:720–8. doi: 10.1046/j.1524-4725.2002.01320.x. [DOI] [PubMed] [Google Scholar]
- 6.Harris JA. Follicular unit extraction. Fascial Plast Surg. 2008;24:404–13. doi: 10.1055/s-0028-1102904. [DOI] [PubMed] [Google Scholar]
- 7.Harris JA. New methodology and instrumentation for follicular unit extraction: Lower follicle transection rates and expanded patient candidacy. Dermatol Surg. 2006;32:56–61. doi: 10.1111/1524-4725.2006.32006. [DOI] [PubMed] [Google Scholar]
- 8.Woods R, Campbell AW. Chest hair micrografts display extended growth in scalp tissue: A case report. Br J Plast Surg. 2004;57:789–91. doi: 10.1016/j.bjps.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Dua A, Dua K. Follicular unit extraction hair transplant. J Cutan Aesthet Surg. 2010;3:76–81. doi: 10.4103/0974-2077.69015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cole JP. Status of individual follicular group harvesting. Hair Transplant Forum Int. 2009;19:20. [Google Scholar]
- 11.Bernstein RM, Rassman WR. Follicular unit transplantation: 2005. Dermatol Clin. 2005;23:393–414. doi: 10.1016/j.det.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Gandelman M, Mota AL, Abrahamsohn PA, De Oliveira SF. Light and electron microscopic analysis of controlled injury to follicular unit grafts. Dermatol Surg. 2000;26:25–30. doi: 10.1046/j.1524-4725.2000.99161.x. [DOI] [PubMed] [Google Scholar]
- 13.Greco J. The H-factor in micrografting procedures. Hair Transplant Forum Int. 1996;6:16–8. [Google Scholar]
- 14.Rose PT. The latest innovations in hair transplantation. Facial Plast Surg. 2011;27:366–77. doi: 10.1055/s-0031-1283055. [DOI] [PubMed] [Google Scholar]
- 15.Bernstein RM, Rassman WR. Pre-making recipient sites to increase graft survival in manual and robotic FUE procedures. Hair Transplant Forum Int. 2012;4:128–31. [Google Scholar]


