Abstract
Depression is a psychiatric condition in which there is loss of interest in all pleasurable outlets, viz. food, sex, work, friends, hobbies and entertainment. The prevalence rate of the disease is 6-8% in women and 3-5% in men. Ayurveda, the science of life, provides systematic management principles for depression. Mamsyadi Kwatha is one such formulation stated by Yadavji Trikamji Acharya in Siddha Yoga Sangraha and Bheshaja Samhita, which is said to be effective in psychiatric conditions. The ingredients are Jatamansi (Nardostachys jatamansi), Ashwagandh (Withania somnifera) and Parasika Yavani (Hyocymus niger) in an 8:4:1 ratio, respectively. The test drug was subjected for antidepressant activity in experimental models. The models selected for anti depressant activity were behavioral despair test, anti-reserpine test and Chronic Fatigue Syndrome (CFS) test in albino mice. The test formulation showed significant inhibition of behavioural despair (P < 0.05), weak to moderate anti-reserpine activity - ptosis (P < 0.001), catatonia (P < 0.01), sedation (P < 0.01) and moderate effect in CFS test (P < 0.050). These effects clearly show that Mamsyadi Kwatha has an anti-depressant activity.
Keywords: Ashwagandha, catatonia, immobility time, Jatamansi, Mamsyadi Kwatha
Introduction
Ayurveda is the science of certainty and art of possibility. In Charaka Samhita it is stated that Ayurveda has no boundaries or limitations, it is not easy to acquire a comprehensive knowledge of the science of life. Therefore, one should put honest efforts to be in constant touch with this science. The wise considers the entire universe as their preceptor; it is only the unwise who consider it to be their enemy. One should therefore strive to obtain proper advice, which brings fame and which promotes longevity and nourishment that is acceptable to people.[1] It is mentioned that a disciple should always make efforts for the upliftment of his knowledge and adoption of such methods as would give him the good knowledge.
These words of Acharya Charaka depict the importance of a broad-spectra study. This experimental study is one among them. Although the Ayurvedic drugs have been in use since ages, it is essential to verify the efficacy of herbal drugs using the modern parameters. It is also helpful to elucidate the possible mode of action of the drug under trial in a particular clinical condition.
Depression is a condition characterized by altered mood. An estimated 3-5% of the world's population experiences depression on any given date. There is a loss of interest in all usually pleasurable outlets such as food, sex, work, friends, hobbies or entertainment. Diagnostic criteria include presence of depressed mood nearly every day, markedly diminished interest/pleasure in most or all activities and three or more of the following:
Poor appetite/significant weight loss/increased weight gain
Insomnia/hypersomnia
Psychosomatic agitation/retardation
Feeling of hopelessness
Loss of energy or fatigue
Feelings of worthlessness, self-approach or excessive or inappropriate guilt
Complaints of or evidence of diminished ability to think/concentrate
Recurrent thoughts of death, suicidal ideation, wish to be dead or attempted suicide.[2]
Community studies have shown that the prevalence rate of depression, defined by strict operational criteria, is approximately 6-8% for women and 3-5% for men. Depression is more common in lower social classes and among inner city dwellers. Women in their child bearing years are especially vulnerable.[3]
By seeing the above facts, it can be inferred that depression is the condition that needs more attention, appropriate management and prevention of recurrence. Ayurveda, the ancient treasure of health provides suitable management strategies, for this condition.
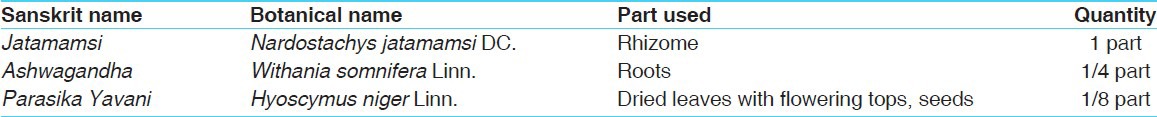
Mamsyadi Kwatha, an Ayurvedic formulation mentioned in Siddhayoga Sangraha of Yadavji Trikamji Acharya and Bheshaja Samhita is said to possess a very good effect in all psychological disorders. The components of Mamsyadi Kwatha are Jatamamsi (Nardostachys jatamansi DC.), Ashwagandha (Withania somnifera Linn.) and Parasika Yavani (Hyocymus niger Linn.) in an 8:4:1 ratio, respectively. It is a strong potent psycho neuro pharmacologically active compound and is subjected for antidepressant activity.[4,5] The current study attempts on evaluating anti-depressant activity of Mamsyadi Kwatha. In addition, anti-depressant activity of individual components of Mamsyadi Kwatha, viz. Jatamansi, Ashwagandha and Parasika Yavani is also attempted in the study.
Materials and Methods
Animals
Swiss albino mice (30 ± 10 g) of either sex were procured from the animal house attached to the institute, and they were housed in groups of six under standard laboratory conditions (temp. 23 ± 2°C, relative humidity 50-60%) with food (Amrut brand) and water ad libitum. All the experiments were performed only after the animals had acclimated to the laboratory conditions for at least 7 days and during morning hours (08.00-10.00 h). The experimental protocol was approved by the institutional animal ethics committee.
Test formulations
The raw materials [Table 1] were collected from the pharmacy attached to the institute and were subjected to pharmacognostical studies to authenticate them. The Kwatha of each drug and Mamsyadi Kwatha [Table 1] was prepared following the classical guidelines.[6] The Kwatha was prepared freshly each time just prior to administration to animals.
Table 1.
Ingredients of Mamsyadi Kwatha
Dose selection
The classical dose of Kwatha is 80 ml/day.[6] Dose fixation for the experimental animals was done on the basis of body surface area ratio by referring to the standard table of Paget and Barnes (1964).[7] On this basis the mouse dose was found to be 8 ml/kg. The test drug was administered orally to overnight - fasted animals with the help of a gastric catheter sleeved to a syringe.
Animal groupings
The selected animals were divided in to five groups and each group consisted of six animals.
Group - I (CG): Received distilled water as vehicle and served as the normal control group
Group - II (JKG): Received Jatamansi Kwatha in the dose of 8 ml/kg
Group - III (AG): Received Ashwagandha Kwatha in the dose of 8 ml/kg
Group - IV (PYG): Received Parasika Yavani Kwatha in the dose of 8 ml/kg
Group - V (MKG): Received Mamsyadi Kwatha in the dose of 8 ml/kg.
Behavioral despair test
Selected mice were divided in to five groups as mentioned above. This study was carried out after acute as well as chronic administration of test drugs. In the acute study, the test drug was administered only once whereas in the chronic study, the test drug was administered for 7 consecutive days. One hour after drug administration (in chronic study on 7th day), the mice were forced to swim individually in a glass jar (25 cm × 12 cm × 25 cm) containing fresh water to a height of 15 cm and maintained at 25° ± 2°C. After an initial 2-min period of vigorous activity, each animal assumed a typical immobile posture. A mouse was considered to be immobile when it remained floating in the water without struggling, making only minimum movements of its limbs necessary to keep its head above water. The total duration of immobility was recorded during the next 4 min of a total 6 min test. The changes in immobility periods were studied after administering drugs in separate groups of animals. Each animal was used only once.[8]
Chronic fatigue syndrome
The employed procedure was similar to that of the “Behavioral despair test”: This procedure was followed for 7 days. The drugs were administered according to grouping 1 h prior to the exposure to stimuli daily for 7 days. This chronic forced swimming produced depression and fatigue resembling chronic fatigue syndrome.[9]
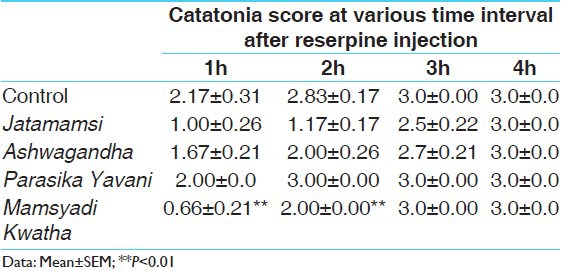
Anti-reserpine test
An hour after the drug administration, reserpine (2.5 mg/kg) was injected to the mice. They were then observed for ptosis, sedation, and catatonia at 1 h, 2 h, 3 h and 4 h after the injection. Scores from 0 to 3 were given according to the intensity of the symptoms. Catatonia was measured by using wooden blocks and a wire stand apparatus. Sedation was measured by putting the mice in the center of three concentric circles drawn on a rubber sheet. The scoring was done according to the time that the mice took to move away (vide gross behavior test). Ptosis was measured by grading the closing of eyelids.[10]
Statistical analysis
Results from the pharmacological screening were expressed as mean ± SEM. Difference between the control and treatments in the experiments were tested for significance using the unpaired Student's “t” test. Values of P < 0.05 were considered as statistically significant.
Results
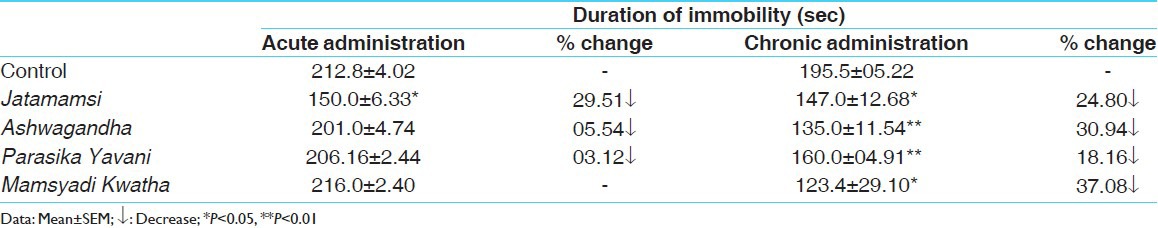
Acute treatment with Mamsyadi Kwatha failed to reduce the immobility duration of mice in comparison with the control group. However, on chronic administration, all the ingredients as well as Mamsyadi Kwatha significantly reduced the immobility duration in comparison with the control group; among them, the observed result in the Mamsyadi Kwatha - treated group was found to be better [Table 2].
Table 2.
Effect on behavioural despair in mice
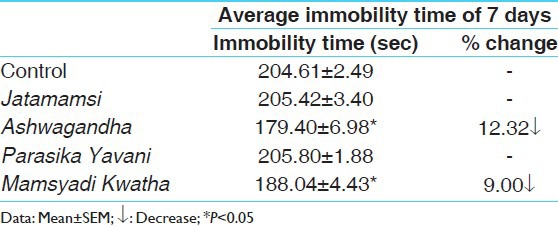
An apparent and statistically non-significant reduction in immobility time was observed in the Mamsyadi Kwatha - treated mice subjected to CFS [Table 3]. However, when the 7 days average immobility time was calculated, the Ashwagandha and Mamsyadi Kwatha - treated groups showed significant decrease in immobility time in comparison with the control group [Table 4].
Table 3.
Effect on chronic fatigue syndrome in mice
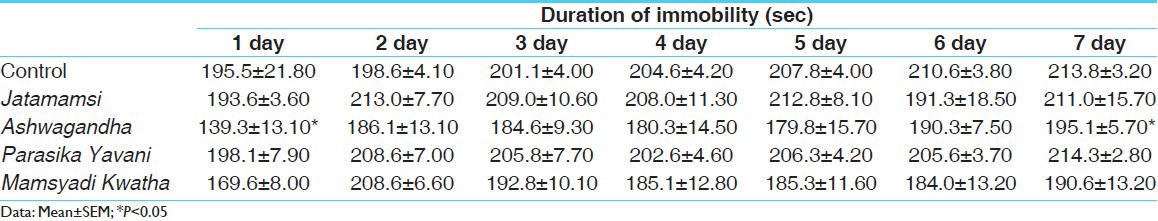
Table 4.
Effect on chronic fatigue syndrome in mice
Data related to the effect of Mamsyadi Kwatha on catatonia, sedation, and ptosis scores in anti-reserpine test have been provided in Tables 5-7. Pre-treatment with Mamsyadi Kwatha significantly attenuated these parameters at the 1st and 2nd h of reserpine injection. However, at 3 h and 4 h Mamsyadi Kwatha failed to attenuate these parameters with the significant extent in comparison to control group.
Table 5.
Effect on ptosis parameter in anti-reserpine test
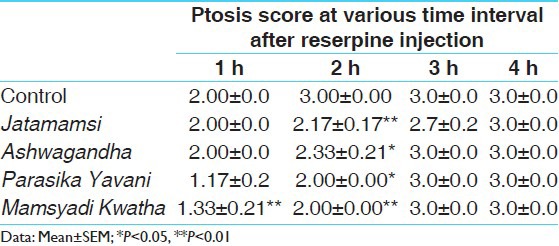
Table 7.
Effect on sedation parameter in anti-reserpine test
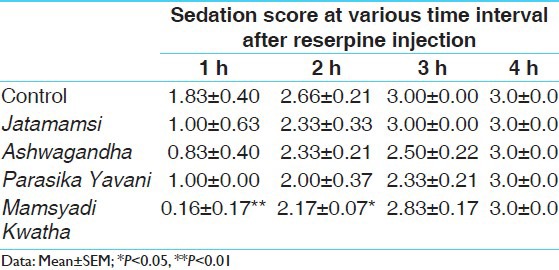
Table 6.
Effect on catatonia parameter in anti-reserpine test
Discussion
Behavioral despair test is the most frequently used experimental model to study antidepressant activity. The model is valid for a broad spectrum of anti-depressants, mainly including tricyclics and MAO inhibitors, which significantly decrease immobility time in FST.[11] Immobility is thought to reflect either a failure to persist in escape - directed behavior after persistent stress or the development of passive behavior that disengages the animal from active forms of coping with stressful stimuli.[12] In the present study on acute single dose administration, only Jatamansi produced significant anti-depressant activity. However, on chronic administration all the three ingredients and the test formulation produced significant inhibition of behavioural despair in mice. The observed effect may be attributed to blockage of 5–HT reuptake or MAO inhibition.
The CFS - has a multifunctional etiology. It is due to abnormality of the hypothalamic – pituitary adrenal axis and mild hypo-cortisolism of central origin. Decrease in plasma levels of 3-methoxy-4 hydroxy phenyl glycol, one of the catecholamine metabolites and significant increase in basal plasma levels of serotonin metabolites, 5-hydroxy indole acetic acid - are the other abnormalities observed.[9]
Reserpine-induced ptosis, catatonia, and sedation are due to depletion of noradrenaline, dopamine and 5-hydroxy tryptamine content in concentrated neurons.13 It can be suggested that the test drugs possess a weak antagonizing effect against this mechanism. Being a poly herbal formulation with proven anti-depressant and other CNS activities of Jatamansi,[14,17] Ashwagandha,[18,19] and Parasika Yavani[20] may attribute role multiple active principles in observed activity profile.
Conclusion
From the above observations, it can be concluded that Mamsyadi Kwatha possesses anti-depressant activity. Being a poly herbal formulation, the observed activity profile may be attributed to one or more bioactive principles present in the components of this formulation. However further studies are required to determine the exact mechanism.
References
- 1.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Vimana Sthana, Apasmar Nidana, 8/14. Reprint edition. Vaidya Jadavaji Trikamji Acharya., editor. Varanasi: Chaukhamba Orientalia; 2011. p. 264. [Google Scholar]
- 2.Edwards CR, Bouchier IA, Haslett C, Chilvers ER, editors. 17th ed. New York: Churchill Livingstone; 1995. Davidson's Principles and Practice of Medicine; pp. 1000–1. [Google Scholar]
- 3.Thomas CL. 17th ed. New Delhi: Jaypee Brothers; 1993. Tabers Cyclopedic Medical Dictionary; pp. 519–20. [Google Scholar]
- 4.Yadavaji Trikamji Acharya, Siddha Yoga Sangraha. 8th ed. Nagpur: Shri Baidyanatha Ayurveda Bhavana Ltd; 1984. p. 86. [Google Scholar]
- 5.Gujarath Rajya Bheshaja Samiti., editor. Bheshaja Samita (Ayurvedic pharmacopeia) Ayur- Swasthya Mantralaya, Gujarath state, Ahmedabad; 803 [Google Scholar]
- 6.Sharangadhara . Sharangadhara Samhita, Madhyama Khanda, 2/3, commentary by Bhishagwara Adhamalla and Pandit Kashiram Vaidya. Varanasi: Krishnadas Academy; 1986. pp. 144–5. [Google Scholar]
- 7.Paget GE, Barnes JM. Evaluation of drug activities. In: Lawrence DR, Bacharach AL, editors. Pharmacometrics. Vol. 1. New York: Academic Press; 1964. p. 161. [Google Scholar]
- 8.Porsolt RD, Bertin A, Jalfre M. Behaviour despair in mice: A primary screening test for anti-depressants. Arch Int pharmacodyn Ther. 1977;229:327–36. [PubMed] [Google Scholar]
- 9.Kaur G, Kulkarni SK. Reversal of forced swimming induced chronic fatigue in mice by anti depressant and herbal psychotropic drugs. Indian Drugs. 1998;35:771–7. [Google Scholar]
- 10.Sheth UK, Dadkar NK, Kamath UG. Bombay: Kothari Book Depot; 1972. Selected Topics in Experimental Pharmacology. [Google Scholar]
- 11.Schildkraut JJ. The catecholamine hypothesis of affective disorders: A review of supporting evidence. Am J Psychiatr. 1965;122:509–22. doi: 10.1176/ajp.122.5.509. [DOI] [PubMed] [Google Scholar]
- 12.Borsini F, Meli A. Is the forced swimming test a suitable model for revealing antidepressant activity? Psychopharmacol (Berl) 1988;94:147–60. doi: 10.1007/BF00176837. [DOI] [PubMed] [Google Scholar]
- 13.Satoskar RS, Bhandarkar SD, Rege NN. 21st ed. Mumbai: Popular Prakashan; 2009. Pharmacology and Pharmacotherapeutics; pp. 181–2. [Google Scholar]
- 14.Dhingra D, Goyal PK. Inhibition of MAO and GABA: Probable mechanism for anti-depressant like activity of Nardostachys jatamansi DC in mice. Indian J Exp Biol. 2008;46:212–8. [PubMed] [Google Scholar]
- 15.Prabhu V, Karanth KS, Rao A. Effects of Nardostachys jatamansi on biogenicamines and inhibitory amino-acids in the rat-brain. Planta Med. 1994;60:114–7. doi: 10.1055/s-2006-959429. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad M, Yousuf S, Khan MB, Hoda MN, Ahmad AS, Ansari MA, et al. Attenuation by Nardostachys jatamansi of 6-hydroxydopamine-induced parkinsonism in rats: Behavioral, neurochemical, and immunohistochemical studies. Pharmacol Biochem Behav. 2006;83:150–60. doi: 10.1016/j.pbb.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Joshi H, Parle M. Nardostachys jatamansi improves learning and memory in mice. J Med Food. 2006;9:113–8. doi: 10.1089/jmf.2006.9.113. [DOI] [PubMed] [Google Scholar]
- 18.Schliebs R, Liebmann A, Bhattacharya SK, Ashok K, Ghoshal S, Volkar B. Systemic administration of defined extracts from Withania somnifera (Indian Ginseng) and Shilajit differentially affects cholinergic but not glutamatergic and GAB Aergic markers in rat brain. Neurochem Int. 1997;30:181–90. doi: 10.1016/s0197-0186(96)00025-3. [DOI] [PubMed] [Google Scholar]
- 19.Malhotra CL, Mehta VL, Prasad K, Das PK. Studies on Withania ashwagandha, Kaul. IV. The effect of total alkaloids on the smooth muscles. Indian J Physiol Pharmacol. 1965;9:9–15. [PubMed] [Google Scholar]
- 20.Kong JM, Goh NK, Chia LS, Chia TF. Recent advances in traditional plant drugs and orchids. Acta Pharmacol Sin. 2003;24:7–21. [PubMed] [Google Scholar]


