Abstract
Vata is the governing factor in the maintenance of equilibrium in the universe as well as in the body. As age advances, the influence of Vata Dosha progresses, resulting in the process of gradual degeneration of the body. Sandhigatavata (osteoarthritis) is one of the consequences of this process, which is common in the elderly people. This is one of the major causes of chronic disability, affecting the quality of life. Prevalence of osteoarthritis in India is more among menopausal women. This study has been conducted to evaluate the efficacy of Ayurvedic multimodal management in Sandhigatavata and to provide better options to Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). In present clinical trial, 50 patients of Sandhigatavata have been registered and have been given Snehana, Svedana, Mriduvirechana, Matrabasti, and Jalaukavacharana, along with oral medications like Yogaraja Guggulu and Ashvagandha Churna. This multimodal therapy is being used in P.D. Patel Ayurved Hospital, Nadiad, since years, providing good relief to patients with Sandhigatavata. The results have been analyzed statistically by using the Student paired‘t’ test. The therapy showed highly significant (P < 0.001) beneficial effect on the clinical features of Sandhigatavata. On overall effect of therapy, 4% of the patients were relieved completely, while 24% have shown marked improvement, 50% moderate improvement, and 22% mild improvement. Results of follow-up showed that marked improvement decreased, but moderate improvement was steady. Continuing the study on a larger number of patients, with inclusion of more objective parameters to get better conclusions is suggested at the end of the study.
Keywords: Matrabasti, osteoarthritis, Sandhigatavata, Snehana, Svedana, Upanaha
Introduction
Physiological functions of the body will be governed by three Doshas, that is, Vata, Pitta, and Kapha. Vitiation of these Doshas leads in disease manifastation. In old age there is progressive decaying in the body structures resulting in various degenerative disorders including Sandhigatavata due to the predominance of Vata.[1] Osteoarthritis[2] (OA) of modern medical science is considered to be its close equivalent.[3]4] According to a survey, osteoarthritis tops all the ailments in the country. In India, the prevalence is more among women, especially menopausal women.[5] The current pharmacological management of osteoarthritis includes the administration of analgesics and Non Steroidal Anti-Inflammatory Drugs (NSAIDs), but their use neither provides adequate pain relief nor deceleration in disease process. In addition, NSAIDs are associated with adverse effects.[6,7] Due to which the use of alternative therapies is on the rise. The plan of the treatment in the study is based on the recommendations from classics for the treatment of Vatavyadhi (diseases essentially caused by Vata). A multimodal therapy in treating a disease is usual Ayurvedic therapy and it is being used in P.D. Patel Ayurved Hospital, Nadiad, since many years, providing good relief to the patients with Sandhigatavata. Yogaraja Guggulu and Ashvagandha Churna have reported to be beneficial in the management of Sandhigatavata (OA).[8] The objective of the present study is to evaluate efficacy of multimodal Ayurvedic management for Sandhigatavata.
Materials and Methods
Fifty clinically diagnosed patients of Sandhigatavata, involving knee joints, were selected from the Outdoor Patient Department (OPD) and hospitalized for a duration of 15 days in the Department of Kaya Chikitsa, in between December 2010 to July 2011. Special clinical proforma was prepared and findings were recorded at regular interval for proper assessment. The enrolled patients were advised to withdraw use of NSAIDs before starting the Ayurvedic management.
The patients were assessed before treatment and after the completion of 15 days of indoor treatment. After completion of indoor treatment, the patients were administered oral medicines. Follow-up with full clinical assessment was done after 15 days and 45 days.
Inclusion criteria
Individuals between the age group of 30 to 75 years of both genders having clinical features of Sandhigatavata as described in Ayurvedic classics,[9] as well as clinical features of osteoarthritis
Patients with affection of knee joint, presenting with Sandhishotha (swelling over joints), Sandhishula (pain in joints), Sandhigraha (stiffness in joints), Sprarshasahatva (tenderness), and Sandhisphutna (crepitus)[9,10,11,12]
Availability of at least 80% of the clinical features in patients was considered as an inclusion criteria for the present study. Radiology of the affected joints was not carried out because those patients who were included in the study have already been diagnosed radiologically.
Exclusion criteria
Patients below 30 years and above 75 years of age
Patients suffering with other forms of arthritis like Rheumatoid Arthritis (RA), psoriatic arthritis, gout, ankylosing spondylitis, infective arthritis, and Systemic Lupus Erythematosus (SLE)
Patients who had an association with other diseases like diabetes mellitus, hyper or hypothyroidism
Management of the patients
Mriduvirechana (mild purgation) with Eranda Sneha (seed oil of Ricinus communis Linn.), 30 – 35 ml, according to the Koshtha, with warm water, was administered on the third day after admission following Abhyanga and Svedana for two days. Koshtha was assessed on the basis of the patient's bowel habits and sensitivity. Patients of Mridu Koshtha were given 30 ml of Eranda sneha and patients of Madhyama and Krura Koshtha were given 35 ml of it. After a rest for one day, the following therapies and medicaments were administered
Abhyanga (oleation therapy) with Narayana Taila (Vata alleviating medicated oil)[13] for 11 days.
Bashpasvedana (fomentation therapy with evaporation) with Nirgundipatra[14] (fresh leaves of Vitex nigundo Linn.) for 11 days
Nirgundipatra Upanaha was done for 11 days
Niruha Basti (proctocolonic administration of decoction) of Dashamula Kvatha (decoction of Dashamula) for one day (before lunch following Abhyanga and Svedana) followed by Matra Basti of 40 ml Narayana Taila (immediately after supper) was given for nine days
Yogaraja Guggulu,[15] 1 g, thrice a day, with warm water
Ashvagandha Churna (root powder of Withania somnnifera Dunal.) 3 g with warm milk was given in morning and evening before meals
Jalaukavacharana (leech application) was done on the patients on the eleventh day, if pain and stiffness were not relieved after Snehana, Svedana, Mriduvirechana, and Basti. This was repeated if required on the fifteenth day.
All formulations like Narayana Taila, Eranda Sneha, Dashamula Kvatha, Yogaraja Guggulu, and Ashvagandha Churna were prepared as per the standard guidelines under the supervision of the subject experts. Fresh leaves of Nirgundi were collected from the medicinal plant garden in the campus.
Pathyapathya (food regimen and behavioral advice)
On the day of Mriduvirechana, the patients were kept on semi-liquid recipe containing equal quantity of rice and mung beans in the evening. After this, patients were kept on usual food recommended by classics for the patients of Vata related diseases, that is, Mudgayusha (mung bean soup), chapatis of wheat flour, boiled vegetables, and rice. They were instructed not to take sour, fermented, or spicy food and to avoid Atishrama (heavy work), Ratrijagarana (night vigils) and Divasvapa (daytime sleep).
Criteria for assessment
The improvement was assessed with regard to the clinical features, on the basis of the scoring system [Tables 1 and 2].
Table 1.
Subjective criteria
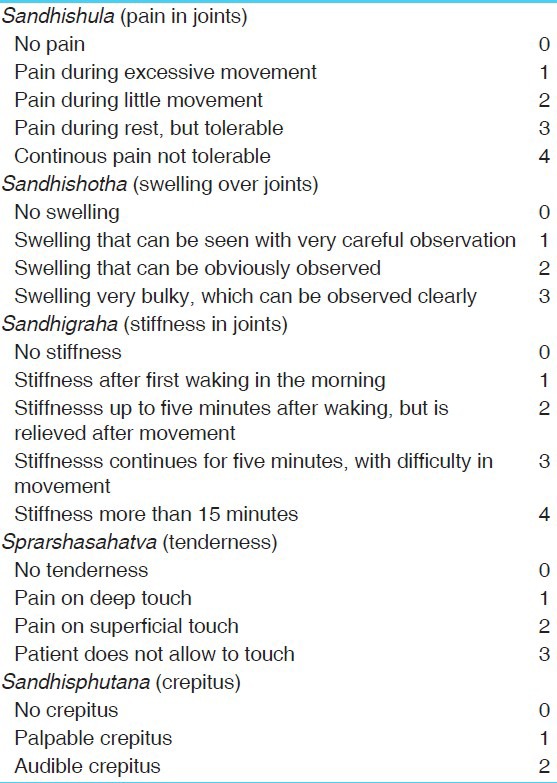
Table 2.
Overall assessment of therapy
Objective criteria
Improvement in range of movement was assessed before and after treatment with Goniometer.
Statistical analysis
The improvement was assessed on the basis of relief in the clinical features of the disease before and after treatment. The obtained results were analyzed by Students paired ‘t’ test.[16] The results were interpreted as highly significant if P < 0.001 and significant if P < 0.05 or P < 0.01.
Observations and Results
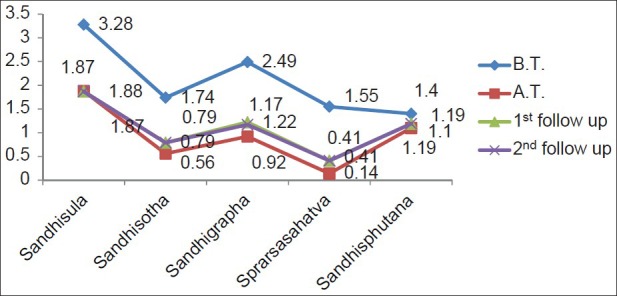
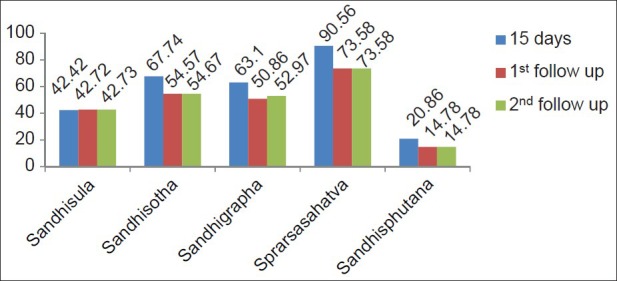
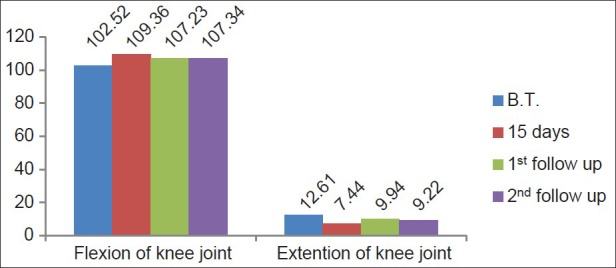
The demographic data of this study suggested that osteoarthritis is prevalent in 97.22% of the menopausal women [Table 3]. It was observed that highly significant results were found in all clinical features [Table 4]. Highly significant results were found even after 15 days of treatment (first follow-up) with most of the features, while a significant result was found in the symptom of Sandhisphutana [Table 5]. It was observed that relief, in percentage, found in patients after 45 days (second follow-up) was almost the same as that taken on the first follow-up [Table 6]. Highly significant relief was found in flexion of the knee joint and significant relief in the extension of the knee joint [Table 7] and after 15 days (first follow-up) [Table 8]. It was observed that extension of the knee joint was improved to 26.88%, in comparison to the first follow-up (21.22%). The improvement in knee flexion movements was statistically highly significant. [Table 9]. It was observed that a minor difference was found in the mean scores of clinical features after 15 days of treatment as indoor patients and in both follow-ups [Figure 1]. Sprarshasahatva was relived by 90.56% after 15 days of treatment, while 73.58% relief was found during follow-up [Figure 2]. It was observed that a minor difference was found in the mean score of range of movement of the knee joint after 15 days and in followup [Figure 3]. It was observed that the percentage of relief in extension of the knee joint was 41.03% after 15 days, which reduced in follow-up [Figure 4]. In the present study, 24% had marked improvement after 15 days of treatment, which reduced by 16% after the first follow-up and by 14% after the second follow-up, while 50% of the patients had moderate improvement after 15 days, which increased by 52% during the period of both follow-up assessments [Figure 5].
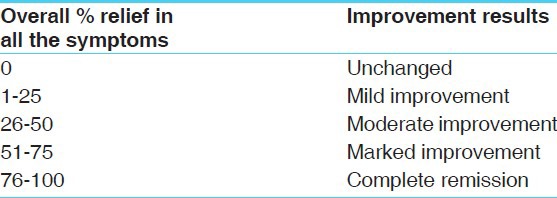
Table 3.
Observations
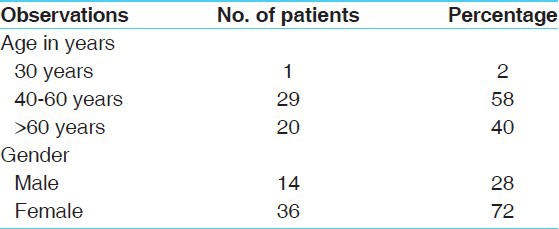
Table 4.
Effect of therapy on clinical features after 15 days of indoor treatment
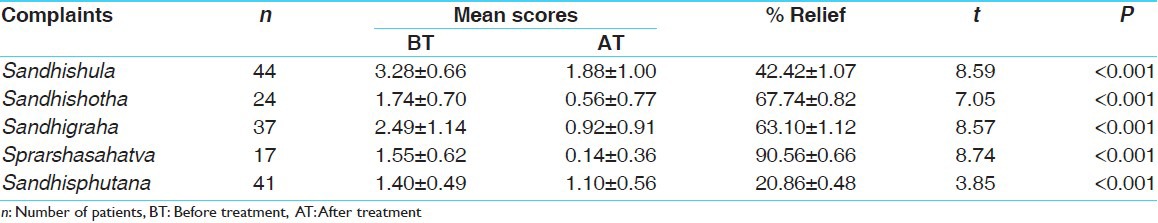
Table 5.
Effect of therapy on clinical features during first follow-up
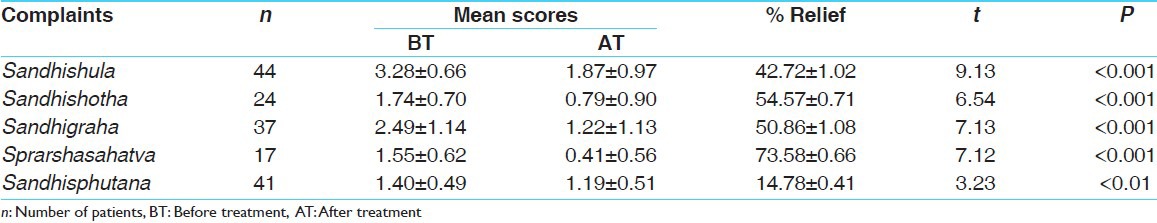
Table 6.
Effect of therapy on clinical features second follow-up
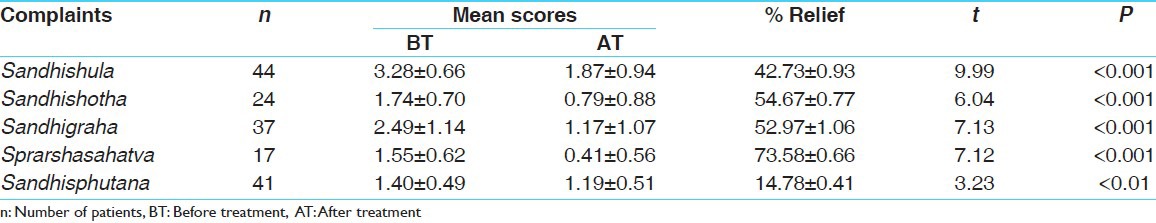
Table 7.
Effect of therapy on range of movement of knee joint after 15 days of indoor treatment
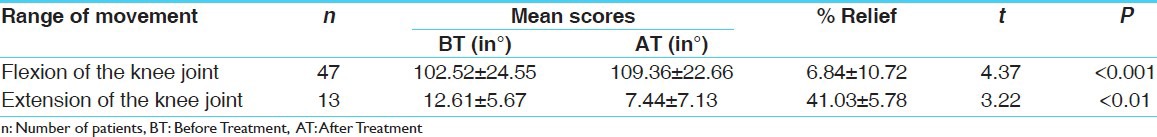
Table 8.
Effect of therapy on range of movement of knee joint during first follow-up
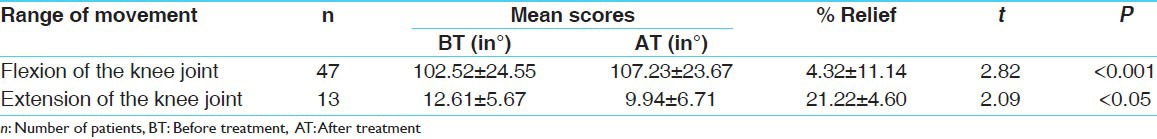
Table 9.
Effect of therapy on range of movement of the knee joint during second follow-up
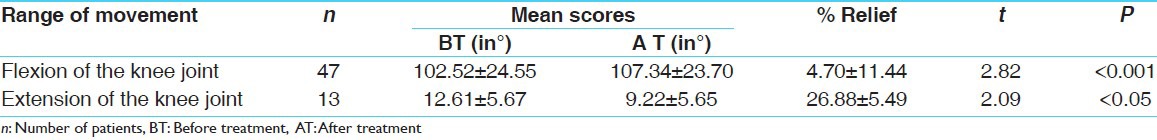
Figure 1.
Comparison of mean scores in clinical features (knee joint osteoarthritis)
Figure 2.
Comparison of percentage improvement in clinical features (knee joint osteoarthritis)
Figure 3.
Comparison of mean scores in degree of range of movement of knee joint osteoarthritis
Figure 4.
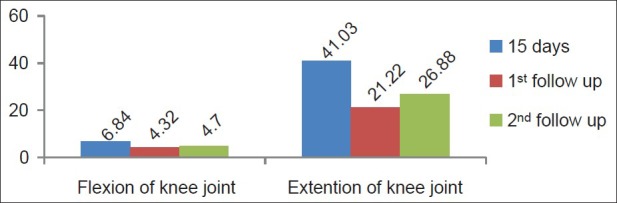
Comparison of percentage improvement in degree of range of movement of knee joint osteoarthritis
Figure 5.
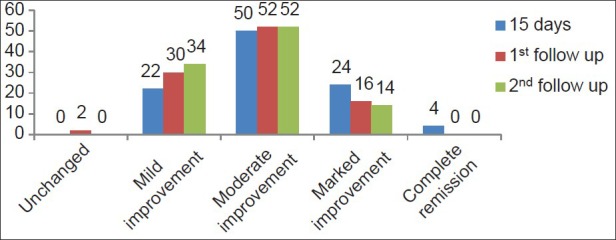
Overall effect of therapy
Discussion
In the present study, it is observed that most of the female patients developed Sandhigatavata during the menopausal period. This supports estrogen deficiency as a risk of OA.[17]
In present study, highly significant (P < 0.001) effect was found in Sandhishula, Sandhishotha, Sandhigraha, and Sandhisphutana in both knee joints. This also supported a previous clinical study conducted, showing a marked reduction in pain and improvement in movements.[18] The beneficial effect of Abhyanga, Svedana, and Matrabasti was also found reported.[4]
Probable mode of action
Mriduvirechana
Treatment of Sandhigatavata usually begins with a basic process like Mriduvirechana. It cleanses the body to restore patency of the Srotasa, which improve the access of healing material as well as nourishment to the body components. In addition, this also helps in maintaining or restoring the optimum equilibriumin Tridosha.
Eranda Taila is indicated for Mriduvirechana in Vatavyadhichikitsa.[19] The Eranda Beeja, having Vibhedana (purgative), Srotoshodhana (channel-cleansing), and Anulomana, (directing Vata in the right direction) actions,[20] is used for Mriduvirechana. Eranda Taila has Vatahara[21] action and it is the best among the medicaments used for Virechana (purgative therapy).[22] Mriduvirechana performed with Eranda Taila after Purvakarma (the preparatory procedures), that is, Abhyanga and Svedana, eliminates the Dosha from the body through Koshtha, without any complication.
Abhyanga
Taila (oil) used in Abhyanga has Snigdha (unctuous), Guru (heavy), and Mridu (soft) properties, which are opposite to the properties of Vata. Abhyanga reduces the provoked Vata, which is responsible for the decay in the Dhatus and for manifestation of features like pain, stiffness, and crackes. According to modern studies, massage stimulates blood circulation and assists the lymphatic system, improving the elimination of waste throughout the body. Absorption through the skin can be enhanced by suspending the drug in an oily vehicle and rubbing it on the skin.[23] Thus, the medicaments used as massage are absorbed through the skin.
Svedana
Svedana is specially indicated in symptoms like Sankocha (contraction or flexion), Ayama (extension), Shula (pain), Stambha (stiffness), Gaurava (heaviness), and Supti (numbness).[24] These are the usual clinical manifestations of Sandhigatavata. Svedana has actions like Stambhaghna (cures stiffness), Svedakarakatva (creates perspiration), Gauravaghna (cures heaviness), and so on.[25]
Nirgundipatra upanaha
Upanaha (poultice sudation) is a type of Svedana indicated in classics[26] as one of the components in the treatment of Sandhigatavata.[27] Studies have revealed the fact that lipid medium is highly suitable for penetration of the drug molecule through stratum corneum.[28] On this basis, it can be assumed that the oil used in Nirgundipatra Upanaha serves as a lipoidal medium for penetration of the drug molecules of Nirgundi and exerts an immediate anti-inflammatory[29] effect. Moreover heat applied with Nirgundipatra upanaha increases the local circulation and thus the rate of drug absorption. Nirgundi possesses Vedanasthapana (analgesic) and Shothahara (anti-inflammatory) actions.[14] In most of the Nighantus it has been used for treating disorders characterized by Shopha (swelling) and Shula (pain).[30] Its preventive effect on the development of formaldehyde-induced experimental arthritis has been observed.[31] The present study supports these earlier observations and recommendations by the Nighantus.
Niruha Basti
This Basti given for one day before Matrabasti, cleanses the colon and prepares a good atmosphere for the Matrabasti material to come in contact with the colon wall and exert its medicinal effect.
Matrabasti
Matrabasti is a form of Sneha Basti. It is convenient and comfortable in administration. It nourishes the body, promotes the strength, and cures Vata-related diseases.[32] Basti, through its action on Vata and Agni, promotes the formation of Dhatus. The colon is considered as main seat of Vata, and Vata-alleviating substances administered through the rectocolonic route in Matrabasti are able to have their optimum effect on the seat of Vata.
Jalaukavacharana
Charaka Samhita mentions that if a disease does not respond to the application of opposite principles like Shita–Ushna (cold–hot) or Snigdha – Ruksha (unctuous – dry), vitiation of Rakta Dhatu must be considered.[33] In such a condition Raktamokshana is one of the recommendations. Hence, in the present study Raktamokshana (blood-letting) has been done by applying Jalauka (leech) in 31 patients, as it is easy and does not produce complications. Although Sandhigatavata is essentially a Vata-disorder affecting the Sandhi structures, secondary involvement of the Rakta Dhatu is possible in these 31 patients, which is evident with the classical Upashaya - Anupashaya test described earlier. According to conventional medicine also, this is not purely a degenerative condition. This is why the earlier name osteoarthrosis is now accepted as osteoarthritis.
Yogaraja Guggulu
It contains Tridosha Shamaka (pacifier of three Doshas, that is, Vata, Pitta, Kapha) and Rasayana (rejuvenative) actions and it is recommended for the management of all Vata Rogas.[15] Guggulu possesses anti-inflammatory and analgesic actions. It helps in prevention against degenerative changes that may occur in bones and joints due to arthritis. Guggulu reduces inflammation and joint stiffness as well as pain associated with arthritis, and increases joint mobility.[34] Earlier pharmacological studies on Guggulu have established its anti-inflammatory and anti-arthritic activities in formaldehyde-induced arthritis, in albino rats.[35] Significant anti-inflammatory and anti-arthritic activities of oleo-gum resin has been reported against carragenun-induced rat paw edema, granuloma pouch, as well as adjuvant arthritis.[36] A study presented at a recent meeting of the American College of Rheumatology, has shown that herbal Ayurvedic therapy consists of Guggulu, which is as effective in treating knee osteoarthritis as a commonly prescribed medication (Celebrex) and Glucosamine, and with fewer side effects. In addition, the Guggulu has been shown to be a potent inhibitor of the enzyme, Nuclear Factor Kappa-light-chain-enhancer of activated B cells (NFKB), which regulates the body's inflammatory response. There are several studies that show decreased inflammation and joint swelling after administration of the extracts of Guggulu resin.[37]
Narayana Taila
Taila (sesame oil) itself is a potent Vata-alleviating substance. Its Vatashamaka action is enhanced when it is processed with Vatashamaka drugs like Patala (Stereospermum suaveolens DC.), Ashvagandha (Withania somnnifera Dunal.), Agnimantha (Clerodendrum phlomidis Linn. f.), Atibala (Sida cordifolia Linn.), and the like, in preparing Narayana Taila. Narayana Taila can be administered through any route in Vata Roga.[13] In current study, it is used for Abhyanga and Matrabasti.
Ashvagandha Churna
It possesses Shothahara (anti-inflammatory), Vatahara, Vedanasthapana, Shulaprashamana (analgesic), and Rasayana (rejuvenative) actions.[38] Withania somnifera (Ashvagandha), has shown a significant anti inflammatory activity.[39] A study reported that an extract of the root powder of Withania somnifera has a chondroprotective effect on the damaged human osteoarthritic cartilage matrix in 50% of the patients tested.[40]
In this clinical trial a majority of patients, that is, 56% had a chronicity between one and five years, and were taking NSAIDs repeatedly. After starting the therapy, the patients did not need NSAIDs for symptomatic relief. In the assessment during the first outdoor follow-up it was observed that marked improvement was reduced in comparison to improvement found after 15 days of indoor treatment in the patients, while patients with moderate improvement remained the same in both the follow-up assessment periods [Figure 5]. This shows that the indoor treatment consists of manual therapies and least activities, as indoor patients contributed to marked and faster improvement in the first fortnight, which reduced initially at home, due to the absence of manual therapies and possibly increased activities, but became steady later on.
It is an incurable, but manageable disease, which is why the repetitive use of manual therapies is needed for a long time.
No adverse reaction of any procedure or oral medicaments were found during treatment, either as inpatients or as outpatients.
Conclusion
It can be concluded from the present study that Sandhigatavata is commonly found mostly in menopausal females. The present study reveals that multimodal Ayurveda treatment provided highly significant relief in Sandhigatavata of the knee joint. This also shows the importance of manual therapies. The improvement remains steady even after 45 days of outdoor treatment. This shows the stable efficacy of the treatment. It is noticed that relief of symptoms has been found in spite of stopping NSAIDs in the patients. Sandhigatavata is Yapya (manageable) in nature, so repetitive use of this therapy is needed. This therapy is safe and effective in the management of Sandhigatavata.
References
- 1.Vagbhatta . Vagbhatta, Ashtanga Hridayam, Sutrasthana, Ayushkamiya Adhyaya, 1/7. English translation by KRS Murthy. Vol. 1. Varanasi: Chaukhambha Sanskrit Samsthan; 2009. p. 6. [Google Scholar]
- 2.Shah SN, editor. 7th ed. Mumbai: Association of Physician of India; 2003. API Textbook of medicine; p. 1152. [Google Scholar]
- 3.Bhatt S, Gupta V, Srikanth N. WHO India Country Office Collaborative Study: Technical Report. New Delhi: CCRAS, Dept. of AYUSH, Ministry of H and FW, Govt. of India; 2007. [Last accessed on 2011 Aug 5]. Feasibility of Integrating Ayurveda with Modern System of Medicine in a Tertiary Care Hospital for Management of Osteoarthritis (Knee): An Operational Study. Available from: http://www.ccras.nic . [Google Scholar]
- 4.Shah M, Mehta CS, Shukla VD, Dave AR, Bhatt NN. A Clinical study of Matra Vasti and an Ayurvedic indigenous compound drug in the management of Sandhigatavata (Osteoarthritis) AYU. 2010;31:210–7. doi: 10.4103/0974-8520.72399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennett, Coleman and Co. Ltd; c2013. [Updated on 2007 Sep 6, Last accessed on 2011 Jul 31]. Times of India.com [article on Internet]. Osteoarthritis is India's No. 1 ailment. Available from: http://www.articles.timesofindia.indiatimes.com/2007-09-06/india/27968801_1_tns-arogya-osteoarthritis-hiv-and-cancer . [Google Scholar]
- 6.About.com [article on Internet]. Eustice C. Guide to Osteoarthritis, Part 4 of 5-Osteoarthritis Medications and Other Drug Options. About.com. c2013. [Updated on 2007 Apr 7, Last accessed on 2011 Aug 5]. Available from: http://www.arthritis.about.com/od/oa/a/Osteo_arthritis_4.htm .
- 7.Sweden: Theheart.org by WebMD; c1999-2012. [Updated on 2010 Sept 8, Last accessed on 2011 Aug 26]. Theheart.org [article on Internet] NSAID use associated with future stroke in healthy population. Available from: http://www.theheart.org/article/1119849 . [Google Scholar]
- 8.Bhatt S, Gupta V, Srikanth N. New Delhi: CCRAS, Dept. of AYUSH, Ministry of H and FW, Govt. of India; 2007. Feasibility of Integrating Ayurveda with Modern System of Medicine in a Tertiary Care Hospital for Management of Osteoarthritis (Knee): An Operational Study. CCRS, WHO India Country Office Collaborative Study: Technical Report; p. 10. [Google Scholar]
- 9.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita – Vol. 2, Chikitsa Sthana, Vatavyadhichikitsa Adhyaya, 28/37. Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 783. [Google Scholar]
- 10.Sushruta . In: Sushruta Samhita-Vol. 1, Nidana Sthana, Vatavyadhinidana Adhyaya, 1/28. Sharma AR, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 458. [Google Scholar]
- 11.Madhavakara . In: Madhava Nidanam-Vol. 1, Vatavyadhinidana Adhyaya, 22/21. 32nd ed. Upadhyaya Y, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2002. p. 463. [Google Scholar]
- 12.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita – Vol. 2, Chikitsa Sthana, Vatavyadhichikitsa Adhyaya, 28/37. Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 784. [Google Scholar]
- 13.Sharangadharacharya . In: Sharangadhara Samhita, Madhyama Khanda, Ghrita Taila Kalpana Adhaya, 9/101-110. Tripathi B, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2002. p. 233. [Google Scholar]
- 14.Sharma PC, Yelne MB, Dennis TJ, Joshi A. Vol. 3. New Delhi: Central council of Research in Ayurveda and Siddha, Dept. of AYUSH, Ministry of H and FW, Govt. of India; 2001. Database on medicinal plants used in Ayurveda; p. 451. [Google Scholar]
- 15.Sharangadharacharya . In: Sharangadhara Samhita, Madhyama Khanda, Vataka Kalpana Adhyaya, 7/56-69. Tripathi B, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2002. p. 203. [Google Scholar]
- 16.Mahajan BK. 6th ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2006. Methods in biostatics for medical students and research workers; pp. 147–50. [Google Scholar]
- 17.Mahajan A, Tandon V, Verma S, Sharma S. Osteoarthritis and Menopause. J Indian Rheumatol Assoc. 2005;13:21–5. [Google Scholar]
- 18.Ruparel S, Patel K, Gupta S. Primary study on Sandhigatavata w.s.r. to osteoarthritis. Sci J Panchkarma. 2010;10:11. [Google Scholar]
- 19.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita – Vol. 2, Chikitsa Sthana, Vatavyadhichikitsa Adhyaya, 28/85. Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 792. [Google Scholar]
- 20.Anonymous. 1st ed. Vol. 3. New Delhi: Dept. of AYUSH, Ministry of Health and Family Welfare; 2003. Ayurvedic Pharmacopoeia of India; p. 52. Part 1. [Google Scholar]
- 21.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita – Vol. 1, Sutra Sthana Yajjapurushiya Adhyaya, 25/40. Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 468. [Google Scholar]
- 22.Ibidem. Charaka Samhita, Vol. 1, Sutra Sthana, Snehadhyaya, 13/12. :256. [Google Scholar]
- 23.Brunton LL, editor. 12th ed. New Delhi: McGraw-Hill Professional; 2011. Goodman and Gilman's The Pharmacological Basis of Therapeutics; p. 22. [Google Scholar]
- 24.Agnivesha, Charaka, Dridhabala . Charaka Samhita – Vol. 1, Sutra Sthana Svedadhyaya, 14/24. In: Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 286. [Google Scholar]
- 25.Ibidem. Charaka Samhita, Vol. 1, Sutra Sthana, Langhana-Brihaniya Adhyaya, 22/11. :424. [Google Scholar]
- 26.Sushruta . In: Sushruta Samhita-Vol. 2, Chikitsa Sthana, Svedavacharaniyachikitsa Adhyaya, 32/3. Sharma AR, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 416. [Google Scholar]
- 27.Ibidem. Shusruta Samhita, Vol. 2, Chikitsa Sthana, Vatavyadhichikitsitam, 4/8. :205. [Google Scholar]
- 28.Benson HA. Transdermal drug delivery: Penetration enhancement techniques. Curr Drug Deliv. 2005;2:23–33. doi: 10.2174/1567201052772915. [DOI] [PubMed] [Google Scholar]
- 29. [Last accessed on 2011 Aug 5]. Available from: http://www.sbcollegeofpharmacy.com/research_pub5.htm .
- 30.Bapalal Vaidya. Nighantu Adarsha, Vol. 2, Nirgundyadi Varga. Vadodara: Gujarat Pustakalaya Sahayaka Sahakari Mandali; 1999. p. 803. [Google Scholar]
- 31.Chaturvedi GN, Singh RH. Experimental studies on the antiarthritic effect of certain indigenous drugs. Indian J Med Res. 1965;53:71–80. [PubMed] [Google Scholar]
- 32.Agnivesha, Charaka, Dridhabala . Charaka Samhita – Vol. 2, Siddhi Sthana Snehavyapadasiddhi Adhyaya, 4/53. In: Shastri K, editor. Varanasi: Chaukhambha Sanskrit Samsthan; 2004. p. 1013. [Google Scholar]
- 33.Ibidem. Charaka Samhita, Vol. 1, Sutra Sthana, Vidhishonitiya Adhyaya, 24/17-18. :445. [Google Scholar]
- 34.Demand Media Inc; c2013. [Updated on 2010 May 03, Last accessed on 2011 Aug 27]. Live Strong.com [article on Internet] Shiflko R. Benefits of Guggulu. Available from: http://www.livestrong.com/article/115826-benefits-guggul . [Google Scholar]
- 35.Gujral M, Sareen K, Tangri KK, Amma MK, Roy AK. Antiarthritic and anti-inflammatory activity of gum guggul (Balsamodendron mukul Hook) Indian J Physiol Pharmacol. 1960;4:267–73. [PubMed] [Google Scholar]
- 36.Arora RB, Kapoor V, Gupta SK, Sharma RC. Isolation of a crystalline steroidal compound from Commiphora mukul and its anti-inflammatory activity. Indian J Exp Biol. 1971;9:403–4. [PubMed] [Google Scholar]
- 37.Chopra Center Healing Wisdom.com [article on Internet] Patel S. Ayurvedic Approaches to Osteoarthritis–Part I. Healng Wisdom. c2013. [Posted on 2011 Mar 17, Last accessed on 2011 Aug 5]. Available from: http://www.chopracenterhealingwisdom.com/?p=9 .
- 38.Sharma PC, Yelne MB, Dennis TJ, Joshi A. New Delhi: Central council of Research in Ayurveda and Siddha, Dept. of AYUSH, Ministry of H and FW, Govt. of India; 2001. Database on medicinal plants used in Ayurveda-Vol.3; p. 88. [Google Scholar]
- 39.Mishra LC, Singh BB. Scientific basis for the therapeutic use of Withania somnifera (Ashvagandha): A Review. Altern Med Rev. 2000;5(4):334–46. [PubMed] [Google Scholar]
- 40.Sumantran VN, Kulkarni A, Boddul S, Chinchwade T, Koppikar SJ, Harsulkar A, et al. Chondroprotective potential of root extracts of Withania somnifera in osteoarthritis. J Biosci. 2007;32:299–307. doi: 10.1007/s12038-007-0030-3. [DOI] [PubMed] [Google Scholar]


