Abstract
Description of Vandhyatva is available in most of the Ayurvedic classics, including Nidana (diagnosis), Samprapti (etiopathogenesis), Lakshana (symptomatology), Bheda (types) and Chikitsa (treatment). In current study, efforts have been made to study the effect of Nasya and Matra Basti on anovulation (Beeja Dushti). Ovulation is under the control of Vata. Narayana Taila is attributed for its effect in Vandhyatva. 24 patients of female infertility having anovulatory factor, being diagnosed by Trans-Vaginal Sonography (TVS) for 2 consecutive cycles were divided in two groups. Patients in Group A (n = 12) administered the drug through Nasya and in Group B (n = 12) through Matra Basti. Ovulation occurred 36.36% of patients in group A and 66.16% of patients group B. Matra Basti showed better results than Nasya group on anovulation.
Keywords: Anovulation, infertility, Matra Basti, Narayana Taila, Nasya, Vandhyatva
Introduction
Procreation is a blessing that aids in transferring the genes from one generation to another and thus aid to evolution. Fertility is the capacity of a couple to reproduce or the state of being fertile. As successful pregnancy is a multi-step chain of events, even if one of the events or conditions is not met in the right amount of time pregnancy may not happen or reach to birth. Infertility by itself does not threaten physical health, but has a strong impact on the psychological and social well-being of the couples. Infertility can result in severe emotional stress. Couples often describe the “hope and despair” cycle, as they hope each month that they will finally conceive and then despair when once again it does not happen.
Proper functioning of four factors viz. Rutu, Kshetra, Ambu and Beeja is the prime requisites for Garbha (conception).[1] Beeja, most essential part among the four has been considered as Antahpushpa, i.e. ovum.[2] So anovulation can be included under Beeja Dushti.
Ovarian factor contribute 15-25% and is the second common cause of infertility.[3] Ovulatory factor is an important subset in infertility among women, accounting about 40% cases.[4]
Over the past few decades, modern medical field developed modalities like hormonal therapy, in-vitro fertilization, embryo transfer, gamete intra-fallopian transfer, etc., but with minimal success rate. Additionally these procedures are associated with adverse effects and are not affordable to all. Considering these inconveniencies, the population is turning towards traditional modalities like Ayurveda.
Tridoshas have an impact over all the process involved in ovulation. Vata stands for proliferation and division of cells (granulosa and theca cells), rupture of the follicle, etc.[5] Pitta is associated with its conversion power, like conversion of androgens to estrogen in Graffian follicle maturity of follicle by its function of Paka Karma.[6] Kapha stands as a building and nutritive factor. It binds all the cells together and gives nutrition for growth and development of the cells.
Among the three Doshas, Vata plays a major role in physiology and pathology of reproductive tract[7,8] and Basti is considered to be the best treatment for Vataja disorders.[9]
In addition to Basti, Nasya Karma (trans-mucosal nasal insufflations) has been preferred in cases of Vandhyatva.[10]
Considering this, it has been planned to evaluate the significance and impact of Basti and Nasya Karma in cases of infertility with special reference to anovulatory factor.
Materials and Methods
Selection of patients
Patients were selected from Out-Patient Department of Stree Roga and Prasooti Tantra Department and randomly grouped into two.
Inclusion criteria
Patients of child bearing age with a complaint of failure to conceive after 1 year of married life
Primary and secondary infertility with anovulatory factors
Age group 20-40 years.
Exclusion criteria
Disorders of reproductive tract such as tuberculosis, carcinoma, and congenital deformities of reproductive tract
Patients suffering from the other chronic illness, cardiac diseases, and thyroid disorders, etc
Infertility associated with other factors like tubal blockage, uterine factors, etc.
Ethical clearance
The study was cleared by the Institutional Ethics Committee. Prior to initiation of the study, written consent was taken from each patient. Patients were asked to withdraw their name from the study at any time without giving any reason if they wish.
Selection of drug
The drug selected in the present study is Narayana Taila,[11] advocated in Vata disorders including Vandhyatva; hence, selected in the study.
After examining the raw material for their authenticity at Pharmacognosy Laboratory, the drug (Narayana Taila) was prepared in the Pharmacy, Gujarat Ayurved University; Jamnagar, by following standard guidelines.
Posology
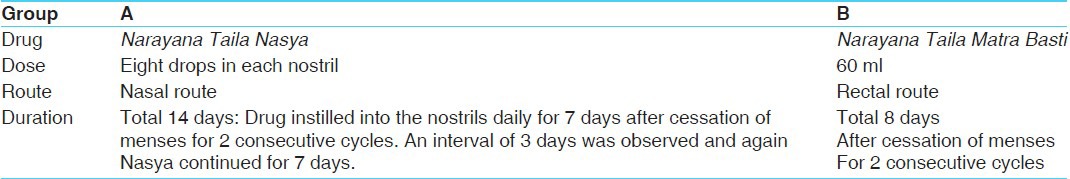
Dose, duration and route of administration are placed at Table 1.
Table 1.
Grouping and posology
Investigations
Routine hematological examination: Hemoglobin%, Total Count, Differential Count, Erythrocyte Sedimentation Rate (ESR), Pack Cell Volume (PCV)
Urine: Routine and microscopic.
Criteria for diagnosis
Trans-Vaginal Sonography (TVS) [Before Treatment (BT) and After Treatment (AT)] for the ovulation study
BT - 2 months
AT - 1 month.
TVS was carried out from day 9th of menstrual cycle up to at least 22nd day of the cycle to diagnose anovulation according to the growth of a follicle.
In all the patients, TVS was carried out for 2 consecutive cycles for final diagnosis.
To evaluate male factor, semen analysis of the partner was carried out.
Follow-up study
Follow-up study was conducted for 1 cycle after completion of the treatment.
Criteria for assessment
The result was assessed on the basis of follicular study (ovulation study).
Scoring pattern of follicle
0 = 0-12 mm
1 = 12-19 mm
2 = 19-23 mm
3 = Ovulated.
(For this scoring method, serial TVS was carried out to diagnose anovulation for consecutive 2 cycles.)
Overall effect of treatment
The overall effect was graded into four types:
Conceived: The patient's husband otherwise normal was conceived after the treatment
Complete remission: Ovulation occurred
Improved: Ovulation not occurred but only improvement in the size of follicles, i.e. 12-19 mm
Unchanged: No change in the growth of the follicle.
Observations
Total 24 patients were registered in the present study; out of them 22 completed the treatment (11 in each group) and 2 were dropped out (1 in each group).
In this study, 79.16% patients had primary infertility and 20.84% patients had secondary infertility. Nearly, 66.66% belonged to age group of 26-30 years; 45.83% patients had 6-10 years chronicity and 79.17% had taken hormonal treatment for infertility.
Total 54.17% of patients were having hirsutism. Obesity was found in 66.67% patients with Body Mass Index (BMI) of 25-29 while Svetasrava (white discharge) was found in 50% of the patients and breast secretion was present only in one patient. It shows that maximum have anovulation.
Maximum number of patients (58.33%) had regular menstrual history while 41.67% had irregular menses. Nearly 62.50% patients had moderate quantity of menses. 79.17% patients had painless menses. 66.67% patients had 4-6 days duration of menstrual period. 37.50% had inter-menstrual period of 25-28 days while 29.17% had an interval of 30-42 days followed by 25% with more than 42 days.
Chinta (worry) was present in all registered patients while Tanava (stress) was found in 83.33% followed by Bhaya (fear) in 33.83%, Krodha (anger) in 29.17%, Dainya and Shoka in 25%. It shows that stress was present in all the patients, which is one of the causes of anovulation.
54.17% reports of semen analysis showed certain abnormalities that may influence overall effect of the therapy.
Results
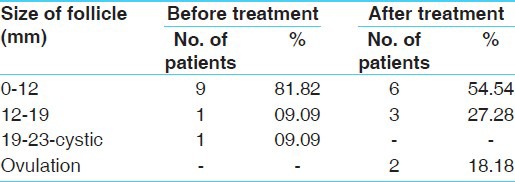
In Group A, average initial size of follicle was 0-12 mm in 9 patients (81.82%) with 12-19 mm follicle size in 1 patient, and >23 mm growth in one patient (9.09%). After treatment, 6 patients (54.54%) had follicular size of 0-12 mm, 3 patients (27.28%) had follicle size 12-19 mm (15 mm × 14 mm) and 2 patients (18.18%) reported ovulation [Table 2].
Table 2.
Effect of Narayana Taila Nasya on follicular growth and ovulation (Group A)
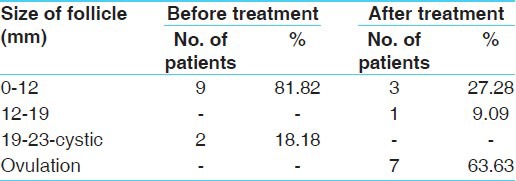
In Group B, average initial size of follicle was 0-12 mm in 9 patients (81.82%) and cystic growth was found in 2 patients (18.18%). After treatment, size of follicle was 0-12 mm in 3 patients (27.28%), 1 patient 9.09% had follicle size of 12-19 mm (14 mm) and 7 patients (63.63%) had ovulated [Table 3].
Table 3.
Effect of Narayana Taila Matra Basti on follicular growth and ovulation (Group B)
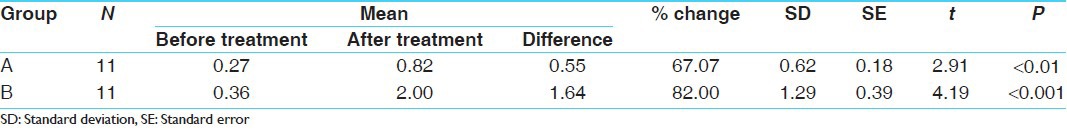
In Group A, the initial mean score of follicular size was 0.27, and was increased to 0.82 after treatment. This improvement was statistically significant (P < 0.01). In Group B, the initial mean score of follicular size was 0.36 that was increased to 2 after treatment. This improvement was also statistically highly significant (P < 0.001) [Table 4].
Table 4.
Effect of therapy on follicular size in 22 patients
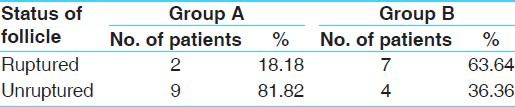
After treatment two patients of Group A 18.18% showed rupture of follicle while nine patients 81.82% had unruptured follicle. While in Group B, seven patients (63.64%) had ovulated and 4 (36.36%) patients had not ovulated [Table 5].
Table 5.
Effect of therapy on ovulation in 22 patients
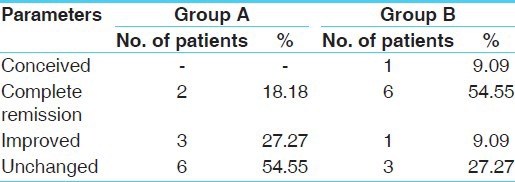
In Group A, none of the patient conceived after treatment. Complete remission, i.e. ovulation was found in 18.18% of patients. While 27.27% of patients were reported with improvement and 54.55% of patients had no change with treatment. In Group B, one patient (9.09%) conceived. Complete remission found in 54.55% of the patients. While 9.09% of patients reported with improvement and 27.27% of patients had no response to the treatment [Table 6].
Table 6.
Overall effect therapy on ovulation in 22 patients
Discussion
Ovulatory cause is an important subset in infertility among women, accounting about 40% of cases. Anovulatory or inability to produce to fertile ovum is growing problem due to change in life-style, faulty food habits, environments, stress, etc.
In the present study, maximum number of patients (66.66%) belonged to age group of 26-30 years, which is the most fertile period of women. The trend of late marriage is also increasing now a day because of higher education and social awareness of women. So, this may be probable causative factor and it is also because patients with infertility come to Ayurvedic line of treatment after trying modern medicine for a long time. Age related decline in female infertility can be attributed largely to progressive follicular depletion and a high incidence of abnormality in aging oocytes.[12]
Nearly 45.83% patients had 6-10 years chronicity and 79.17% had taken hormonal treatment for infertility. It shows that patients approach modern science and after failure or huge expenses they prefer to Ayurveda as their last hope, which will lead to chronicity of the disease.
Nearly 66.67% patients were found to be above with BMI in the range of 25-29, which is one of the causes of infertility and anovulation. Excess body fat may cause alteration in androgen and estrogen metabolism which in turn affect the Hypothalamo-Pitutary Ovarian (HPO) axis leading to ovarian dysfunction.[13]
All registered patients were found to be under psychological stress, which has a direct impact over fertility.[14] Catecholamines, prolactin, adrenal steroids, endorphins, and serotonin all affect ovulation and in turn are all affected by stress. Possibly this can be explained by a reduction in stress, and subsequently, alterations in the neuro endocrinologic characteristics of the infertile couple.[15]
In the present study, total 54.17% of male partners were detected with abnormal semen reports that affect the overall effect of therapy.
The Narayana Taila with its Katu, Tikta Rasa; Laghu, Ruksha Guna; Ushna Veerya and Katu Vipaka and Vata Kaphashamaka Doshaghnata ultimately leads to Karmas such as Deepana, Pachana, Vilayana, Anulomana, and Srotoshodhana resulting Amapachana and Vatakaphashamana, which may removes Sanga and Avarana leading to proper function of Vayu regulating Beejagranthi Karma resulting in Beejotsarga (ovulation).
Phytoestrogens are plant derived substances whose structure results in chemical nature similar to endogenous estrogens of human. The main action of phytoestrogen is due to their adaptogenic activity. They may be beneficial in both hypoestrogenic and hyperestrogenic state in the body. Thus, they have mixed estrogenic and antiestrogenic action, depending on target tissues.[16,17]
The drugs of Narayana Taila have Prajasthapana, Rasayana, Balya, Brimhaniya properties, which may correct the function HPO axis subsequently resulting in proper functioning of the Beejagranthi. The drugs of Narayana Taila possess anti-oxidant, adaptogenic, immune-modulatory, etc., properties, which may help in relieving stress, age-decline, etc., (causes of anovulation).
Probable mode of action of Nasya and Matra Basti
Drug through nasal route reaches the Shringataka Marma (Siro Antarmadhyam) and spreads through nose, ear, eye, and tongue into Shira (head) eliminate morbid Doshas and ultimately promotes the normal physiological function.
Narayana Taila Nasya may stimulate olfactory nerves and limbic system, which in turn stimulates hypothalamus leading to stimulation of Gonadotropin Releasing Hormone (GnRH) neurons, regularizing GnRH pulsatile secretion, leading to ovulation. Phytoestrogenic or oestrogenic property of different components of Narayana Taila like, Shatavari,[18] Tila Taila[19] regulates neuropeptide Y activity, which in turn regulates the activity of gonadotropin secretion.[20]
Matra Basti given through Guda (rectal route) normalizes Apana Vayu leading to Vatanulomana and physiological functioning of Vata, which may help in turn for the extrusion of ovum from the follicle and ovulation.
Basti Dravya spreads all over the body, pacifies the aggravated Dosha along with Vyana Vayu leads to Samyaka Rasa Raktadi Dhatu Nirmana. Sukshma Bhaga of Rasa reaches the Beejagranthi, which regularizes the Beejotsarga with the help of normal Apana Vayu.
Matra Basti after absorption reaches into systemic circulation and the concept of Central Nervous System (CNS) resembles Enteric Nervous System (ENS) the endogenous opioids in the ENS specially endorphins (β-endorphin) are influenced which will affect GnRH release regularizing HPO axis regulating ovarian cycle and ovulation. Endogenous opioids are a group of peptides, which play an important role in the ovarian cycle through the inhibitory effect on GnRH secretion. Other pituitary hormones are also modulated by opiates. β-endorphin has been best known of the opioid related to the reproductive system regulating variety of pituitary hormones including gonadotrophins. β-endorphin has a role in the regulation of the normal ovarian cycle.[21]
Basti - stimulates - the ENS - generates the stimulatory signal for CNS - causes stimulation of the hypothalamus for GnRH and the pituitary for Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) with the help of neurotransmitters. Ovaries and the rectum-S2, -S3, and -S4 supply. Parasympathetic activity is mainly responsible for the Apana Vayu activity. Basti given through rectum will stimulate this parasympathetic nervine supply, which in turn helps for the release of ovum from the follicle in the ovary.
Conclusion
Oil is the best Shamana drug for Vata and many of the drugs of Narayana Taila possess phytoestrogenic constituents. Hence, the combination effects the process of ovulation. Antioxidant, immunomodulatory, adaptogenic properties helps in relieving stress and age related changes and help to regularize the functions of ovaries. Ovulation study with the TVS is the best diagnostic parameter to access the anovulation, but to see the effect of drug at hormonal level, hormonal study is required. Though ruptured follicle were more with group B treatment, conception rate was less which can be attributes to high incidence of male factor (45.45% have sperm abnormalities). At the end of the study, it can be concluded that, Matra Basti provides significant results over Nasya. If the therapy is clubbed with suitable oral medicines and male partner is treated appropriately, the conception rate can be increased.
References
- 1.Sushruta . Sushruta Samhita, Sharira Sthana, 2/33. Reprint edition. Varanasi: Surabharati Prakashana; 2003. [Google Scholar]
- 2.Kashyapa . In: Kashyapa Samhita, Khila Sthana, 9/11. Reprint edition. Pandita Hemaraja Sharama, Sri Satyapala Bhisagacharya., editors. Varanasi: Chaukhambha Sanskrit Sansthan; 2009. [Google Scholar]
- 3.Dutta DC. Text Book of Gynaecology Including Contraception. In: Konar H, editor. 4th ed Reprint. Ch. 15. Calcutta: New Central Book Agency; 2007. p. 216. [Google Scholar]
- 4.Insler V, Lunenfeld B. 2nd ed. Edinburgh, London, Madrid, Melbourne, New York and Tokyo: Churchill Livingstone; 1999. Infertility: Male and Female. [Google Scholar]
- 5.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sutra Sthana, Vatakalakaliya Adhyaya, 12/8. 4th ed. Jadavaji Trikamji Acharya., editor. Varanasi: Chaukhambha Sanskrit Sansthan; 1994. p. 79. [Google Scholar]
- 6.Ibidem. Charaka Samhita, Sutra Sthana, Vatakalakaliya Adhyaya, 12/11. :80. [Google Scholar]
- 7.Ibidem. Charaka Samhita, Chikitsa Sthana, Yonivyapat Chikitsa Adhyaya, 30/115. :639. [Google Scholar]
- 8.Vagbhata . In: Ashtanga Hridaya, Uttar Tantra, Guhyaroga Pratishedha, 34/23. Reprint 9th ed. Bhishgacharya Harishastri Paradkara Vaidya., editor. Varanasi: Chaukhambha Orientalia; 2005. p. 898. [Google Scholar]
- 9.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sutra Sthana, Yajjhapurashiya Adhyaya, 25/40. 4th ed. Jadavaji Trikamji Acharya., editor. Varanasi: Chaukhambha Sanskrit Sansthan; 1994. p. 132. [Google Scholar]
- 10.Kashyapa . In: Kashyapa Samhita, Kalpa Sthana-Shatpushpa Shatavari Kalpadhyaya 5/23-25. Reprint edition. Pandita Hemaraja Sharama, Sri Satyapala Bhisagacharya., editors. Varanasi: Sanskrit Sansthan; 2004. [Google Scholar]
- 11.Shrangdhara . Shrangdhara Samhita, Madhyama Khanda, 9/101-106, Commentary by Dr. Brahmanand Tripathi. Reprint edition. Varanasi: Chaukhambha Surbharati Prakashan; 2006. [Google Scholar]
- 12.Speroff L, Fritz MA. 7th ed. Noida: Gopson Paper Ltd. Jaypee Brothers; 2005. Clinical Gynaecologic Endocrinology and Infertility, Part IV; pp. 1017–8. [Google Scholar]
- 13.Rajan R. 4th ed Reprint. New Delhi: Jaypee Brothers; 2004. Postgraduate Reproductive Endocrinology; p. 347. [Google Scholar]
- 14.Agnivesha, Charaka, Dridhabala . In: Charaka Samhita, Sharira Sthana, Atulyagotriya, 2/7. Reprint edition. Vaidya Jadavaji Trikamji Acharya., editor. Varanasi: Chaukhambha Prakashan; 2007. [Google Scholar]
- 15.Seibel MM, Taymor ML. Emotional aspects of infertility. Fertil Steril. 1982;37:137–45. doi: 10.1016/s0015-0282(16)46029-2. [DOI] [PubMed] [Google Scholar]
- 16.Phytoestrogen therapy for menopausal symptoms? BMJ. 2001;323:354. doi: 10.1136/bmj.323.7309.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheichi LM, Lobascio A, Valerio T. Phytoestrogen-containing food and prevention of postmenopausal osteoporosis and CV disease. Minerva Ginecol. 1999;51:343–8. [PubMed] [Google Scholar]
- 18.Bopana N, Saxena S. Asparagus racemosus – Ethnopharmacological evaluation and conservation needs. J Ethnopharmacol. 2007;110:1–15. doi: 10.1016/j.jep.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Wu WH, Kang YP, Wang NH, Jou HJ, Wang TA. Sesame ingestion affects sex hormones, antioxidant status, and blood lipids in postmenopausal women. J Nutr. 2006;136:1270–5. doi: 10.1093/jn/136.5.1270. [DOI] [PubMed] [Google Scholar]
- 20.Speroff L, Fritz MA. 7th ed. Noida: Gopson Paper Ltd. Jaypee Brothers; 2005. Clinical Gynaecologic Endocrinology and Infertility, Part I; p. 155. [Google Scholar]
- 21.Rajan R. Postgraduate Reproductive Endocrinology. 4th ed Reprint. New Delhi: Jaypee Brothers; 2004. pp. 201–5. [Google Scholar]


