Abstract
Urolithiasis in pregnancy represents a major diagnostic and therapeutic challenge to the obstetrician, urologist, radiologist and anesthetist. It is a cause of major concern, considering the potential adverse effects of radiation exposure and of any invasive surgical procedure and anesthesia on the mother and fetus. Fortunately, with conservative management, 70-80% of symptomatic calculi pass spontaneously with no sequel. However, fever, infection, uncontrolled pain and progressive hydronephrosis are indications for surgical intervention when retrograde placements of a ureteral stent or a percutaneous nephrostomy tube are the most traditional options. The recent technological advances in stone fragmentation devices and the administration of safe anesthesia have forced clinicians to embark on more definitive stone management techniques in pregnancy. Ureteroscopy is considered the first definitive treatment of obstructive ureteral calculi during all trimesters of pregnancy, but also has limitations. Although generally avoided during pregnancy, percutaneous nephrolithotomy can be a good treatment choice in selected patients.
Keywords: Pregnancy, percutaneous nephrolithotomy, supine, ultrasound, urolithiasis
INTRODUCTION
The incidence of urolithiasis during pregnancy is 0.026-0.531%, complicating 1:200 to 1:2000 pregnancies, and may be a contributing factor in up to 40% of premature births.[1,2]
The relative percentage, type and frequency of urinary stones occurring during pregnancy are similar to those in nonpregnant stone formers.[3] However, stones in pregnancy may become symptomatic more frequently because of the physiologic dilatation of the collecting systems, allowing for migration of renal stones into the ureter, leading to obstruction and pain.[4]
Left- and right-side calculi occur with equal frequency, and ureteric stones seem to occur about twice as often as renal calculi. Interestingly, 80-90% of patients present in the second or third trimester of pregnancy, but rarely in the first trimester.[2]
Providentially, with conservative management, 70-80% of symptomatic calculi pass spontaneously with no sequel. However, fever, infection, uncontrolled pain and progressive hydronephrosis, occurring in 20-30% of the patients, are indications for surgical intervention.[4]
Retrograde placements of a ureteral stent or percutaneous nephrostomy tube are the most traditional surgical options. But, with continued advancement in endoscopic technology and endourologic techniques, definitive treatment has been aimed.
We report a pregnant patient manifesting with refractory symptomatic urinary stone in which percutaneous nephrolithotomy (PNL) was performed under ultrasound (US) guidance in a supine position approach.
CASE REPORT
A 24-year-old female patient, in her 22th week of pregnancy, presented with severe flank pain secondary to a 2.7 cm urinary stone located in the right renal pelvis that was detected by US [Figure 1]. Despite attempts at conservative management, with optimal analgesic treatment, a retrograde placement of a ureteral stent was necessary due to intractable pain [Figure 2]. However, 1 week later, the patient returned with flank pain refractory to analgesics, when she was submitted to ureteroscopy, but with no success.
Figure 1.

A 2.7 cm urinary stone located in the right renal pelvis detected by ultrasound
Figure 2.

Retrograde placement of a ureteral stent was necessary due to intractable pain
PNL was performed with US guidance (without fluoroscopy) and in a supine position [Figure 3a and b]. Fast and safe stone fragmentation through pneumatic energy and removal was possible [Figure 4a and b]. The patient was released from the hospital on the first postoperative day with no tube and pregnancy curse and labor occurred with no complications.
Figure 3.
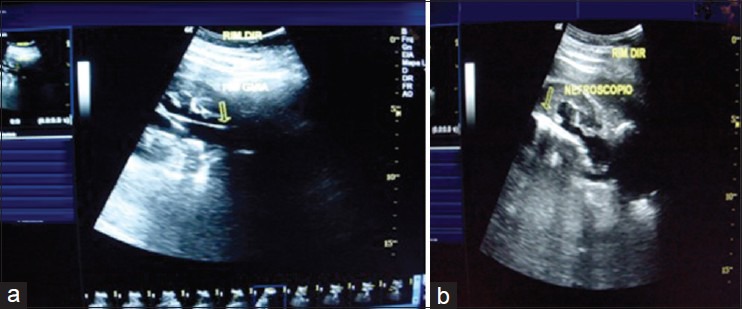
(a and b) Percutaneous nephrolithotomy was performed with ultrasound guidance (without fluoroscopy) and in a supine position
Figure 4.

(a) Retrieved stones (b) Final aspect
DISCUSSION
Diagnostic difficulties of patients presenting with urinary stone disease in pregnancy must be emphasized with incorrect diagnosis of appendicitis, diverticulitis and placental abruption in 28% of the patients in whom a stone was subsequently confirmed. Real-time US is the most commonly used imaging method in pregnancy, and several measures have been recommended to enhance its performance (Pelvic diameter, Color Doppler imaging, Resistive index, Ureteric jets).[1,5]
Magnetic resonance imaging is confirmed as a safe option, but should be reserved for special cases when US fails to provide the diagnosis.[5] The radiation dose of computed tomography (CT) and, particularly, pelvic CT, can be high thus precluding its routine use during pregnancy.[1]
The risk associated with radiation, fetal teratogenesis, carcinogenesis and mutagenesis depends critically on the gestational age and the amount of radiation delivered.[1]
Although exposure to <50 mGy (5 rads) is not associated with an increase in fetal anomalies and pregnancy loss, the International Commission on Radiological Protection recommends a lower threshold of 10 mGy (1 rad), below which no related adverse fetal events have been noted.[5]
With regard to obstetric complications, renal colic may induce premature onset of labor, which may be stopped by pain control or spontaneous stone passage. Women who have obstructive uropathy may also present with preeclampsia or isolated hypertension, which has been successfully alleviated with relief of the obstruction.[3,4]
Inhalation anesthetic agents (nitrous oxide, halothane, cyclopropane) are lipid-soluble and thus easily cross the placenta; animal models have shown that these agents have significant teratogenicity.[1] Exposure to volatile gas agents in the first trimester of pregnancy is estimated to carry a relative risk of 0.5% of a morphogenetic anomaly. Regional techniques of anesthesia are therefore recommended in the first trimester, and general anesthesia should be avoided if possible.[6] If an elective procedure is required, it is recommended to temporize and defer intervention until the second trimester, when fetal risks are minimal.[7]
Despite attempts at conservative management, surgical intervention may ultimately be required. Retrograde placement of an indwelling ureteral stent is well established, consisting of a simple procedure with low complications.[8]
However, irritative lower urinary tract symptoms attributable to the stent and rapid stent encrustation (attributed to hypercalciuria and hyperuricosuria of pregnancy) are often observed. To avoid stent encrustation, some urologists recommend stent exchange every 4-8 weeks.[9]
An alternative means of obtaining urinary drainage is the placement of a percutaneous nephrostomy tube, but disadvantages of an external tube are the inconvenience of dealing with a collection device, the risk for accidental dislodgement, bacterial colonization and infection.[9]
Thus, these two treatment options are fast becoming obsolete because of their limitations and as a result of the greater success rates reported with ureteroscopy offering definite treatment, being first-line treatment for pregnant patients who have failed expectant management.[3] Furthermore, a critical review of the suggested contraindications confirmed that pregnancy remains a strict contraindication to shock wave lithotripsy.[8]
Improvements in instruments and lithotripsy technology (including ultrasound, pneumatic devices, the holmium: yttrium-aluminum-garnet laser and flexible nephroscopes) have expanded the capability of percutaneous stone disintegration, with stone-free rates of >90%.[9]
PNL is generally a safe treatment option and is associated with a low complication rate; however, it has been avoided during pregnancy because of the significant fluoroscopy time required and the need for the patient to be in the prone position.[5]
The US guidance allows the surgeon to safely identify the kidney and the pelvic system, as well as surrounding organs, and is better suited to gain optimum access and avoid complications. If the percutaneous tract is created and the procedure conducted by a well-trained team, the morbidity attributable to percutaneous renal surgery (bleeding and injury to the kidney or adjacent organs) can be significantly reduced.[9]
The supine position approach for PNL was first described by Valdivia and colleagues in 1987, and they subsequently reported their extensive experience with this technique over 11 years.[10]
The purported advantages of the supine position are the ability to complete the procedure using a local anesthetic while maintaining easy access to the urethra and ureteral orifice.
A supine position may be worth considering, especially for patients with co-morbidities likely to increase anesthetic-related risks in a prone position[10] and also in pregnancy.
CONCLUSION
Selection of the appropriate intervention must take into consideration the capabilities and limitations of the institution and should respect the wishes of the patient and clinical judgment of the urologist, obstetrician and anesthesiologist. When providing rational approach to each patient, on experienced center, PNL, through US guidance in a supine position, should be remembered as a feasible, highly efficient and safe treatment option for refractory symptomatic urolithiasis during pregnancy.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Biyani CS, Joyce AD. Urolithiasis in pregnancy. I: pathophysiology, fetal considerations and diagnosis. BJU Int. 2002;89:811–8. doi: 10.1046/j.1464-410x.2002.02772.x. [DOI] [PubMed] [Google Scholar]
- 2.Drago JR, Rohner TJ, Jr, Chez RA. Management of urinary calculi in pregnancy. Urology. 1982;20:578–81. doi: 10.1016/0090-4295(82)90302-8. [DOI] [PubMed] [Google Scholar]
- 3.Lifshitz DA, Lingeman JE. Ureteroscopy as a first line intervention for ureteral calculi in pregnancy. J Endourol. 2002;16:19–22. doi: 10.1089/089277902753483664. [DOI] [PubMed] [Google Scholar]
- 4.Swanson SK, Heilman RL, Eversman WG. Urinary tract stones in pregnancy. Surg Clin North Am. 1995;75:123–42. doi: 10.1016/s0039-6109(16)46539-4. [DOI] [PubMed] [Google Scholar]
- 5.Valentin J. Pregnancy and medical radiation. (1-43).Ann ICRP. 2000;30:iii–viii. doi: 10.1016/s0146-6453(00)00037-3. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen H, Finster M. Anaesthetic risk in the pregnant surgical patient. Anaesthesiology. 1979;51:439–51. doi: 10.1097/00000542-197911000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Goldfarb R, Neerhut G, Lederer E. Management of acute hydronephrosis of pregnancy by ureteral stenting: risk of stone formation. J Urol. 1989;141:921–2. doi: 10.1016/s0022-5347(17)41053-6. [DOI] [PubMed] [Google Scholar]
- 8.Semins MJ. Management of stone disease in pregnancy. Curr Opin Urol. 2010;20:174–7. doi: 10.1097/MOU.0b013e3283353a4b. [DOI] [PubMed] [Google Scholar]
- 9.Osman M, Wendt-Nordahl G, Heger K, Michel MS, Alken P, Knoll T. Percutaneous nephrolithotomy with ultrasonography-guided renal access: experience from over 300 cases. BJU Int. 2005;96:875–8. doi: 10.1111/j.1464-410X.2005.05749.x. [DOI] [PubMed] [Google Scholar]
- 10.Valdivia Uria JG, Valle Gerhold J, Lopez Lopez JA, Villarroya Rodriguez S, Ambroj Navarro C, Ramirez Fabián M, et al. Technique and complications of percutaneous nephroscopy: Experience with 557 patients in the supine position. J Urol. 1998;160:1975–78. doi: 10.1016/s0022-5347(01)62217-1. [DOI] [PubMed] [Google Scholar]


