Key Points
A continued monoclonal protein response after ASCT in the absence of further therapy is prognostic in MM patients.
Abstract
Patients undergoing autologous stem cell transplantation (ASCT) for multiple myeloma (MM) undergo disease assessment approximately 100 days later. Some patients continue to have a decline in their serum or urine monoclonal protein after day 100 in the absence of additional therapy. We evaluated 430 MM patients who underwent ASCT within 12 months of their diagnosis and had not achieved a complete remission at day 100. Of these patients, 167 (39%) had a continued response after day 100 without additional therapy. When compared with patients who did not (n = 263), those who had a continued response had a longer progression-free survival (35 vs 13 months, P < .001), time to next therapy (43 vs 16 months, P < .001), and overall survival (96 vs 57 months, P < .001). This phenomenon of a continued response maintained prognostic value in a multivariable analysis and should be considered when interpreting posttransplant responses.
Introduction
After autologous stem cell transplantation (ASCT), patients with multiple myeloma (MM) have their tumor burden reassessed approximately 100 days later,1,2 the results of which classify their clinical response based on the International Myeloma Working Group (IMWG) criteria.3,4 Some patients continue to experience a decline in their monoclonal (M) protein, even after day 100, in the absence of additional therapy. Little is known about the clinical significance of this continued response. Thus, we reviewed the clinical outcomes of such MM patients who underwent their first ASCT and experienced a continued response.
Methods
After approval by the Mayo Clinic Institutional Review Board, we reviewed the outcomes of 430 MM patients who underwent their first ASCT at the Mayo Clinic, Rochester, within 12 months of their diagnosis between 1999 and 2012; moreover, none of them achieved a complete remission (CR) at day 100 nor did they undergo further consolidation with a second ASCT or maintenance therapy. All patients underwent repeat disease evaluation approximately 100 days after their transplantation that included a skeletal survey, bone marrow biopsy and protein electrophoresis of serum, and 24-hour urine collection (ie, SPEP/UPEP) with immunofixation (IFE) performed when no M-protein was measurable. Serum-free light-chain (sFLC) assay was routinely performed after it became clinically available and was the basis of measurable disease assessment in patients with unmeasurable serum and urine M-spikes. These evaluations were repeated at subsequent follow-up visits, except for the bone marrow biopsy, unless they were needed for further assessment of disease status. Informed consent was obtained according to the Declaration of Helsinki.
Responses were classified by the IMWG criteria.3 M-protein measurements at the time of diagnosis were used as the baseline for response assessments at day 100 and at subsequent evaluations until progression. Patients who had a subsequent decline in their M-protein on SPEP/UPEP or sFLC or had a change to a negative IFE status, which was subsequently confirmed on the next follow-up evaluation, were determined to have had a continued response.
Patients who had a fluorescent in-situ hybridization (FISH) analysis performed on their plasma cells were categorized as having high-risk disease if any of these abnormalities—t(4;14), t(14;16), or t(14;20)—were present at any time during their disease course, or there was a del17p noted any time before or within 30 days of the diagnosis.5-9 The Kaplan-Meier method was used to create progression-free survival (PFS), time to next therapy (TTNT), and overall survival (OS) curves, which were compared using the log-rank test. Multivariable analysis using the Cox proportional hazards model assessed the influence of various prognostic factors on PFS, TTNT, and OS.
Results and discussion
The demographics and clinical characteristics of these 430 patients are outlined in Table 1. One-hundred sixty-seven (39%) of these patients had a continued response at a median of 9.4 months (95% CI, 8-10) post-ASCT. Compared with the 263 (61%) patients who did not have a continued response, patients with a continued response had a longer PFS (35 months vs 13 months, P < .001) (Figure 1A), TTNT (43 months vs 16 months, P < .001) (Figure 1B), and OS (96 months vs 57 months, P < .001) (Figure 1C). Because the patients with a continued response achieved their best response at a median of 9.4 months from ASCT, a landmark analysis was performed to allow all 397 patients alive at 1 year post-ASCT to have the chance to maximize their response. The median PFS, TTNT, and OS from the 1-year landmark was 35, 43, and 96 months, respectively, for those with a continued response (n = 157) compared with 15, 17, and 60 months, respectively, for those without a continued response (n = 240), respectively (P < .001 for PFS, TTNT, and OS).
Table 1.
Demographic and clinical characteristics of the 430 patients who had not achieved a CR at day 100 post transplant based on the presence or absence of a complete response
| Continued response (n = 167) | No continued response (n = 263) | |
|---|---|---|
| Variables | Median (range) | Median (range) |
| Age, y | 60 (32-75) | 60 (29-74) |
| Male, n,( %) | 92 (55%) | 176 (62%) |
| PCLI | ||
| At diagnosis | 0.4 (0-4) | 0.6 (0-14.4) |
| At transplant | 0.3 (0-6) | 0.2 (0-11) |
| Serum M spike | ||
| At diagnosis | 3.7 (0-9) | 3.1 (0-8.5) |
| At transplant | 1 (0-5.1) | 1 (0-6.9) |
| Urine M spike | ||
| At diagnosis | 0.4 (0-15.5) | 0.7 (0-22.6) |
| At transplant | 0.04 (0-10) | 0.09 (0-10) |
| BMPC, % | ||
| At diagnosis | 50 (2- 95) | 50 (2-100) |
| At transplant | 11 (1-95) | 17 (1-100) |
| LDH | ||
| At diagnosis | 150 (62-464) | 152 (51-617) |
| At transplant | 205 (68-1103) | 203 (74-729) |
| β2-microglobulin | ||
| At diagnosis | 3.6 (1-1447) | 3.9 (1-21) |
| At transplant | 2.4 (1-34) | 2.5 (1-34) |
| Creatinine | ||
| At diagnosis | 1.2 (0.4-5.7) | 1.2 (0.4-18.6) |
| At transplant | 0.9 (0.4-4.5) | 0.9 (0.4-3.5) |
| Albumin | ||
| At diagnosis | 3.7 (2.3-5.8) | 3.7 (2.3-5.3) |
| At transplant | 3.3 (1.9-4.8) | 3.4 (2-4.9) |
| FISH, n (%) | Available in 54 pts | Available in 87 pts |
| High-risk FISH | 7 (13%) | 15 (17%) |
| t(4,14) | 2 | 7 |
| t(14,16) | 2 | 1 |
| t(14,20) | 1 | 0 |
| Deletion 17p/mono 17 | 2 | 10 |
| ISS stage, n (%) | Available in 63 pts | Available in 94 pts |
| Stage 1 | 29 (46%) | 32 (34%) |
| Stage 2 | 13 (21%) | 27 (29%) |
| Stage 3 | 21 (33%) | 35 (37%) |
| Induction regimen, n (%) | ||
| Non-novel agent based | 78 (47%) | 87 (33%) |
| Novel agent based | 89 (53%) | 176 (67%) |
| Thalidomide based | 39 (23%) | 74 (28%) |
| Lenalidomide based | 43 (26%) | 76 (29%) |
| Bortezomib based | 17 (10%) | 42 (16%) |
| Conditioning regimen, n (%) | ||
| Melphalan 200 | 143 (86%) | 216 (82%) |
| Reduced dose Melphalan | 14 (8%) | 38 (14%) |
| Other (Mel/TBI, Zevalin/Mel) | 10 (6%) | 9 (4%) |
| IMWG status, n (%) | ||
| At transplant | ||
| CR | 3 (2%) | 13 (5%) |
| VGPR | 19 (11%) | 38 (14%) |
| PR | 93 (56%) | 123 (47%) |
| SD | 47 (28%) | 64 (24%) |
| PD | 5 (3%) | 15 (6%) |
| Missing | — | 10 (4%) |
| At day 100 | ||
| VGPR | 80 (48%) | 141 (54%) |
| PR | 77 (46%) | 109 (41%) |
| SD | 10 (6%) | 13 (5%) |
| At best continued response | ||
| sCR | 28 (17%) | — |
| CR | 55 (33%) | |
| VGPR | 37 (22%) | |
| PR | 43 (26%) | |
| SD | 4 (2%) | |
| History of antecedent PC disorder | 60 (36%) | 57 (22%) |
PR, partial response; sCR, stringent complete response, SD, stable disease; VGPR, very good partial response.
Figure 1.
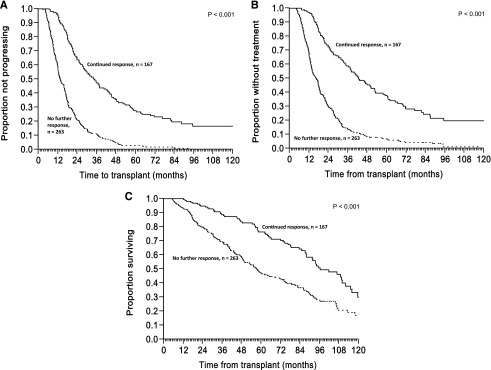
Impact of continued response after ASCT on survival outcomes. Shows the Kaplan-Meier curve (A) for PFS, (B) TTNT, and (C) OS after ASCT in patients not achieving a CR at day 100 based on the presence of a continued response or no further response.
In a multivariate model, only lack of continued response predicted for worse PFS (hazard ratio [HR], 5.28; 95% CI, 2.33-13.1; P < .0001), whereas for TTNT, both elevated creatinine at diagnosis (HR, 1.70; 95% CI, 1.28-2.98; P = .003) and lack of continued response (HR, 10.0; 95% CI, 3.6-34.2; P < .001) were adverse factors. Furthermore, elevated creatinine at diagnosis (HR, 2.54; 95% CI, 1.38-4.87; P = .004), lack of continued response (HR, 7.4; 95% CI, 1.42-68.1; P = .015), older age (HR, 1.1; 95% CI, 1.03-1.19; P = .005), and high-risk MM (HR, 6.58; 95% CI, 1.43-31.5; P = .017) affected OS negatively.
This phenomenon of continued response may affect the interpretation of results generated from single-arm studies aiming to improve post-ASCT disease response with additional therapy.10,11 For example, 67% of patients in this study who had a continued response obtained a deeper response by IMWG criteria than predicted at day 100. Furthermore, using the day 100 response assessment for treatment decisions may be premature in patients who were predicted to have a continued response without further therapy. However, it should be noted that it was mainly patients with a VGPR by day 100 who had a higher likelihood of achieving a CR via continued response (85%) compared with patients with a PR (19%) or SD (0%) at day 100. Moreover, 155 (36%) of the 430 patients who did not achieve a continued response at day 100 progressed within 3 to 12 months after their transplant, suggesting that delaying any planned post-ASCT therapy in anticipation of a CR was not an appropriate choice for that group.
Previous studies have demonstrated that patients who have steep responses to high-dose therapy have plasma cell clones with an early precursor phenotype characterized by a higher proliferative index, making them very sensitive to chemotherapy but even more likely to have a recurrence, which accounts for their early relapse and decreased survival.11-15 We hypothesize that the slow reduction of paraprotein seen in our patients with a continued response reflects the presence of plasma cell clones with a more mature phenotype characterized by lower proliferative capacity and sensitivity to chemotherapy, but with a longer time to relapse and improved survival; moreover, these plasma cell clones gradually disappear with time when there is no ongoing self-renewal.11,16
Factors predicting a continued response included having an IgG isotype (P = .0007), history of an antecedent plasma cell disorder (P = .0485), and a day-100 bone marrow plasma cell (BMPC) percentage of ≤3 (P = .0014). These aforementioned clinical features may reflect the underlying mechanisms for a continued response such as the production and clearance of the M-protein. The production may vary based on the biology of the plasma cells (ie, history of an antecedent plasma cell disorder reflecting a lower proliferative or good-risk plasma cell clone17,18) as well as the extent of plasma cell burden,19 the latter being represented by the day-100 BMPC percentage. Moreover, the clearance of the M-protein can be affected by the isotype. For example, IgA and IgM molecules have half-lives of around 5 to 6 days, whereas it is around 21 days for IgG.20,21 Thus, the longer time to clear the IgG isotype may partly explain the higher proportion of continued or delayed response with IgG isotype.
There are a few limitations to this study, the first being its retrospective nature. The study design excluded patients already in CR at day 100 or who had received maintenance therapy; this could generate an unforeseen selection bias. Being a tertiary referral center, the history of previous antecedent plasma cell disorders may be incomplete in our patient cohort. Nevertheless, this study suggests that in MM patients undergoing ASCT, a continued response is prognostic and may have clinical implications on the use of additional posttransplant therapy, as well as on the design of future ASCT trials.
Acknowledgments
This work is supported in part by the Mayo Clinic Hematological Malignancies Program, the Paul Calabresi K12 Award (CA96028), and the National Cancer Institute, National Institutes of Health (CA 107476, CA 62242, CA100707, and CA 83724).
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: S.K.K. and W.I.G designed the study, collected and analyzed the data, and wrote the manuscript; and M.A.G., A.D., M.Q.L., Y.L., P.P.S, V.G., S.R.H., F.K.B., D.D., P.K., and A.R.M. contributed to writing and reviewing the manuscript.
Conflict-of-interest disclosure: A.D. received additional funding from Celgene, Millennium, Pfizer, and Janssen Pharmaceutical companies. The remaining authors declare no competing financial interests.
Correspondence: Shaji K. Kumar, Professor of Medicine, Division of Hematology, Mayo Clinic, 200 First St SW, Rochester, MN 55905; e-mail: kumar.shaji@mayo.edu.
References
- 1.Blade J, Samson D, Reece D, et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant. Br J Haematol. 1998;102(5):1115–1123. doi: 10.1046/j.1365-2141.1998.00930.x. [DOI] [PubMed] [Google Scholar]
- 2.Kumar S. Stem cell transplantation for multiple myeloma. Curr Opin Oncol. 2009;21(2):162–170. doi: 10.1097/CCO.0b013e328324bc04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Durie BG, Harousseau JL, Miguel JS, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006;20(9):1467–1473. doi: 10.1038/sj.leu.2404284. [DOI] [PubMed] [Google Scholar]
- 4.Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia. 2009;23(1):3–9. doi: 10.1038/leu.2008.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapoor P, Fonseca R, Rajkumar SV, et al. Evidence for cytogenetic and fluorescence in situ hybridization risk stratification of newly diagnosed multiple myeloma in the era of novel therapie. Mayo Clinic Proc. 2010;85(6):532–537. doi: 10.4065/mcp.2009.0677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar SK, Mikhael JR, Buadi FK, et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines. Mayo Clinic Proc. 2009;84(12):1095–1110. doi: 10.4065/mcp.2009.0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar S, Fonseca R, Ketterling RP, et al. Trisomies in multiple myeloma: impact on survival in patients with high-risk cytogenetics. Blood. 2012;119(9):2100–2105. doi: 10.1182/blood-2011-11-390658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avet-Loiseau H, Attal M, Moreau P, et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myelome. Blood. 2007;109(8):3489–3495. doi: 10.1182/blood-2006-08-040410. [DOI] [PubMed] [Google Scholar]
- 9.Gertz MA, Lacy MQ, Dispenzieri A, et al. Clinical implications of t(11;14)(q13;q32), t(4;14)(p16.3;q32), and −17p13 in myeloma patients treated with high-dose therapy. Blood. 2005;106(8):2837–2840. doi: 10.1182/blood-2005-04-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rabin N, Percy L, Khan I, Quinn J, D’Sa S, Yong KL. Improved response with post-ASCT consolidation by low dose thalidomide, cyclophosphamide and dexamethasone as first line treatment for multiple myeloma. Br J Haematol. 2012;158(4):499–505. doi: 10.1111/j.1365-2141.2012.09188.x. [DOI] [PubMed] [Google Scholar]
- 11.Sahebi F, Frankel PH, Farol L, et al. Sequential bortezomib, dexamethasone, and thalidomide maintenance therapy after single autologous peripheral stem cell transplantation in patients with multiple myeloma. Biol Blood Marrow Transplant. 2012;18(3):486–492. doi: 10.1016/j.bbmt.2011.12.580. [DOI] [PubMed] [Google Scholar]
- 12.van Rhee F, Bolejack V, Hollmig K, et al. High serum-free light chain levels and their rapid reduction in response to therapy define an aggressive multiple myeloma subtype with poor prognosis. Blood. 2007;110(3):827–832. doi: 10.1182/blood-2007-01-067728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boccadoro M, Marmont F, Tribalto M, et al. Early responder myeloma: kinetic studies identify a patient subgroup characterized by very poor prognosis. J Clin Oncol. 1989;7(1):119–125. doi: 10.1200/JCO.1989.7.1.119. [DOI] [PubMed] [Google Scholar]
- 14.JR H. Growth rate and responses to treatment in human myelomatosis. Br J Haematol. 1969;(16):607–617. doi: 10.1111/j.1365-2141.1969.tb00441.x. [DOI] [PubMed] [Google Scholar]
- 15.Belch A, Shelley W, Bergsagel D, et al. A randomized trial of maintenance versus no maintenance melphalan and prednisone in responding multiple myeloma patients. Br J Cancer. 1988;57(1):94–99. doi: 10.1038/bjc.1988.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singhal S, Powles R, Milan S, et al. Kinetics of paraprotein clearance after autografting for multiple myeloma. Bone Marrow Transplant. 1995;16(4):537–540. [PubMed] [Google Scholar]
- 17.Zhan F, Barlogie B, Arzoumanian V, et al. Gene-expression signature of benign monoclonal gammopathy evident in multiple myeloma is linked to good prognosis. Blood. 2007;109(4):1692–1700. doi: 10.1182/blood-2006-07-037077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar SK, Dingli D, Lacy MQ, et al. Outcome after autologous stem cell transplantation for multiple myeloma in patients with preceding plasma cell disorders. Br J Haematol. 2008;141(2):205–211. doi: 10.1111/j.1365-2141.2008.07069.x. [DOI] [PubMed] [Google Scholar]
- 19.Salmon SE, Smith BA. Immunoglobulin synthesis and total body tumor cell number in IgG multiple myeloma. J Clin Invest. 1970;49(6):1114–1121. doi: 10.1172/JCI106327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sigounas G, Harindranath N, Donadel G, Notkins AL. Half-life of polyreactive antibodies. J Clin Immunol. 1994;14(2):134–140. doi: 10.1007/BF01541346. [DOI] [PubMed] [Google Scholar]
- 21.Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–558. doi: 10.1038/clpt.2008.170. [DOI] [PubMed] [Google Scholar]


