Abstract
Background
Socioeconomic inequalities in health are ubiquitous in developed countries; however, whether these inequalities differ between women and men over time is less clear.
Objective
To estimate the potentially different health effects of changes in SEP on changes in health for working-age women and men over a 10-year period. Three main questions were addressed: 1) are there health differences between women and men over time, 2) do changes in SEP lead to health inequalities and 3) do changes in SEP impact health differently for women and men?
Methods
Generalized estimating equations models were used to analyze cycles 1–5 of the Canadian National Population Health Survey for four measures of health, number of chronic conditions, self-rated health, functional health, and mental distress, and three measures of SEP, income, education and employment status.
Results
Health inequalities by sex/gender and by changes in SEP were present for all four outcomes in age-adjusted models; however, after controlling for time-dependent social structure, behaviour, and psychosocial factors the relationships persisted only for chronic conditions and psychological distress. There was no evidence that these effects differed, over time, between women and men.
Conclusions
Men and women in this nationally-representative sample of Canadians do not differentially embody changes in SEP, though both sex/gender and changes in SEP independently impact health.
INTRODUCTION
Inequalities in health between women and men are a consequence of biological differences relating to sex and social differences produced by gender roles, opportunities and beliefs.[1] It is widely accepted that women have greater life expectancy than men, but suffer more morbidity;[2] however, emerging evidence suggests that the pattern of inequality is more variable and may depend on the choice of health indicator and the age groups examined.[3–9] Socioeconomic inequalities in health are equally well-described in most developed countries, with those more disadvantaged displaying worse health.[10–17] Similar to sex and gender, the extent and direction of socioeconomic inequalities are also variable. Some dimensions of health do not show simple or consistent patterning by socioeconomic position (SEP), others have flatter gradients, some show complex interaction patterns by age and sex[10, 15, 17] and several measures display cross-national variability.[11, 13] Compared to men, however, women generally experience poorer socioeconomic circumstances[18] and greater morbidity.[2]
The study of the intersection of these two dimensions of social inequality, namely sex/gender differences in socioeconomic inequalities in health, is relatively rare.[8, 19] It has been generally contended that women exhibit shallower socioeconomic gradients than men;[20–22] however, this perspective has been called to question by studies that show more variable patterns.[5, 8, 9, 18, 23–31] Assessing multiple outcomes over time, one study indicated that males indeed had steeper relative income gradients for high blood pressure, self-rated health, depression, heart trouble, trouble breathing, trouble feeding and sick days.[10] Another study found no longitudinal relative gradient differences between women and men based on occupational class; however, steeper male gradients based on education were present for chronic illnesses and respiratory symptoms and steeper female gradients were present for self-rated health and psychological distress. Furthermore, no education gradient differences were observed for asthma, obesity and height.[8] Longitudinal studies that employed only one outcome showed stronger relative female gradients for heart disease[23, 25] and depression[18] based on income[23, 25] and education,[18, 25] and similar income-mortality gradients for both sexes.[24, 31]
Few studies have examined the evolution of sex/gender and socioeconomic differences in health over time and have been able to account for changes in the multiple correlates of health, sex/gender, and SEP. The goal of this study was to estimate the potentially different health effects of changes in SEP for working-age women and men over a 10-year period. Using a longitudinal dataset that includes a number of potential time-dependent confounders (social structure, behavioural and psychosocial characteristics) and a longitudinal analysis that accounts for measured and unmeasured time-invariant within-individual characteristics, we examined the moderating effect of sex/gender on the relationship between SEP and health over time among middle-aged adults. Three main questions were addressed: 1) are there health differences between women and men over time, 2) do changes in socioeconomic position lead to health inequalities and 3) do changes in socioeconomic position impact health differently for women and men?
METHODS
Sample
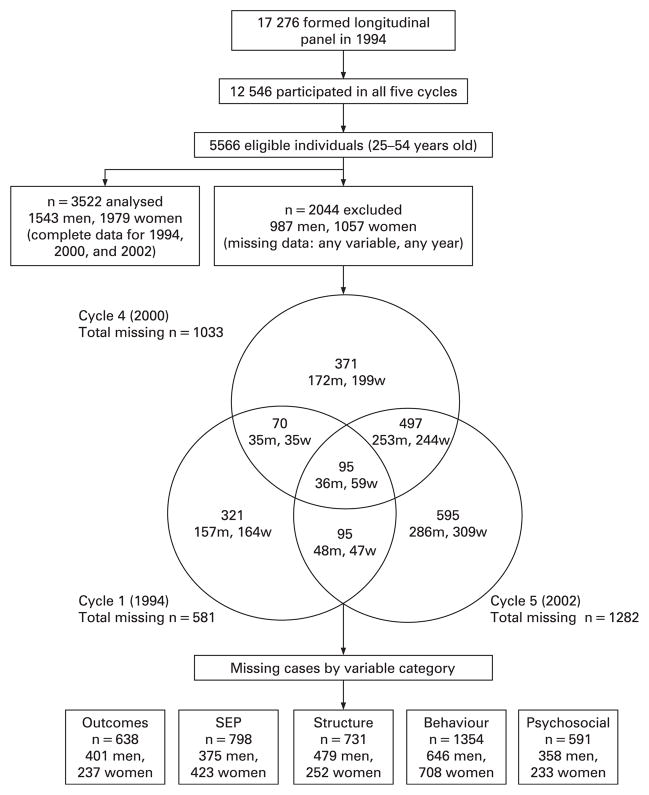
Data were obtained from the Canadian National Population Health Survey (NPHS), a nationally representative longitudinal household survey conducted by Statistics Canada.[32] Selected using multistage sampling, respondents were contacted every two years from 1994/95–2002/03 at the time of analysis. The overall response rates were: Cycle 1: 83.6%, Cycle 2: 92.8%, Cycle 3: 88.2%, Cycle 4: 84.8%, Cycle 5: 80.6%. The Cycle 1 response rate is based on the 20,095 persons initially selected to form the longitudinal panel, while the response rate for subsequent cycles is based on the 17,276 individuals who form the longitudinal panel. Cyclically adjusted sampling weights were used to account for non-response and attrition. As socioeconomic inequalities have been found to be strongest among middle-aged adults[8, 11, 15, 33], we focussed on working-aged participants aged 25–54 years in wave 1. After 10 years of follow-up, the oldest cohort members were 64 years of age and the legal retirement age in Canada is 65. We chose 25 as the minimum age because individuals are likely to be finished their education and entering the work-force by this time. Only participants with complete data at all three waves (N = 3522) were kept in the final sample for analysis (figure 1).
Figure 1.
Follow-up of participants included in and excluded from analyses in the National Population Health Survey, 1994–2003. SEP, socioeconomic position.
Health Outcomes
Health was assessed using four indicators. First, was the number of chronic conditions (NCC), derived as a count of the number of long-term physician diagnosed chronic health conditions that had lasted or were expected to last six months or more. These include, asthma, fibromyalgia, arthritis or rheumatism, back problems, high blood pressure, migraine or headache, food or other allergies, bronchitis or emphysema, sinusitis, diabetes, epilepsy, heart disease, cancer, stomach or intestinal ulcers, effects of stroke, urinary incontinence, and acne requiring prescription medication. Second, self-rated health (SRH) was measured by a five item question that asked respondents to rate their own health on a 5-point scale from excellent (5) to poor (1). Third, functional health was measured using the Health Utilities Index-3 (HUI). The HUI score is based on a combination of eight sub-scales: vision, hearing, speech, mobility, dexterity, cognition, emotion, and pain/discomfort. Scores are defined on a scale anchored by dead=0.000 and perfect health=1.000 in increments of 0.001; however negative scores, with a minimum of -0.360, are also possible.[34] Negative scores represent states of health where respondents are deemed clinically alive, but lack all functional capacity to participate in social life (e.g. being in a coma and on mechanical life support). Finally, psychological distress was measured by a subset of items from the Composite International Diagnostic Interview (CIDI). Respondents were asked, during the month prior to the interview how often did you feel: (1) so sad that nothing could cheer you up; (2) nervous; (3) restless/fidgety (4) hopeless; (5) worthless; and (6) everything was an effort. Possible responses ranged from 0 (none of the time) to 4 (all of the time); therefore, composite scores ranged from 0 to 24 (higher scores indicate more distress). All four measures of health were treated as continuous and linear. Sensitivity analyses using different model specifications (e.g. log transformed) showed similar results.
Socioeconomic Position
Socioeconomic position (SEP) was assessed by income adequacy, highest level of education, and employment status. Income adequacy was calculated as the dollar distance between the individual’s gross equivalized household income in the past 12 months and the Canadian low-income cut-off (calculated annually to reflect inflation), adjusted for household size. Analyzing income adequacy as quintiles and as a dichotomous variable yielded similar results, thus for ease of interpretation the binary variable was deemed preferable. Highest level of education was categorized as individuals who did not complete secondary school (reference), secondary school graduate (coded as 1) or post-secondary graduate (2). Again, using a greater number of categories did not affect the final results. Finally, employment status was treated as a dichotomous variable that compared individuals who were employed to those who were inactive in the workforce (out of work, retired, disabled) during the past 12 months. Given the age of this cohort, the vast majority of individuals were employed and thus finer categorizations were not possible due to statistical imprecision. Moreover, a main activity variable was not collected at all waves and thus we were unable to identify individuals whose main daily task was housework and/or child rearing. The variance inflation factor (VIF) of these variables did not indicate a problem with multi-collinearity: all VIF scores were less than five.
Covariates
Following previous research,[2] variables from three broad categories of social determinants, social structure, health-related behaviours, and psychosocial factors, were included as time-dependent controls. These factors were found to vary by gender and to differentially contribute to the health of Canadian women and men in the first wave of the NPHS.[2] Social structure was measured by age, marital/partner status, household size, and social support. Health-related behaviours were represented by physical activity, body mass index (BMI), and smoking. Respondents’ psychosocial factors were assessed with the adjusted specific chronic stress index (number of stressors related to activity overload, financial difficulties and problems with relationships in day-to-day encounters; adjusted for personal/family situation) and sense of mastery index (measures the extent to which individuals believe that their life-chances are under their control); however, these indices were only measured during cycles 1, 4 and 5. Sensitivity analyses were performed to compare models with the full range of covariates, except chronic stress and mastery, using all five cycles of data to models using only three cycles of data. The results were similar, so analyses were restricted to cycles 1, 4 and 5 in order to incorporate the psychosocial dimension. The appendix provides further details on the measurement of each covariate.
Statistical Analysis
To describe the data for each cycle, weighted means and 95% confidence intervals were computed for each health outcome and weighted means and proportions were produced for each independent variable separately for women and men. In addition, the health outcomes and SEP of individuals who were excluded from the sample, but contributed some data, were also described in cross-section. The longitudinal analytic strategy entailed a three step process using Generalized Estimating Equations (GEE) regression models, also known as population averaged models. With GEE, the effect of a given exposure is interpreted as the effect on the average person, or a person selected at random from the population. To adjust for the correlation of individuals’ responses over time, GEE models utilize information from the factors that are constant within an individual, in addition to factors that are similar between individuals, to estimate the regression parameters.[35] The within-person correlation may be thought of as time-invariant individual propensity (measured and unmeasured) to develop illness. As such, biological susceptibility to poor health (genetic make-up, sex hormones, foetal development, etc.) as well as early life course factors known to impact adult health (childhood development, socialization into gender roles, parental and childhood SEP, etc.) were controlled for. Since aspects of both biological differences (sex) and social differences (gender) were accounted for in this analysis (inherently by GEE or with time-dependent controls), the variable used to differentiate women and men is termed sex/gender [36] in this paper.
The first step in the analysis was to evaluate longitudinal differences in health between women and men using age-adjusted and fully adjusted (structure, behaviour, and psychosocial) GEE models. Second, similar models were used to examine longitudinal health inequalities produced by changes in SEP. Finally, women’s and men’s differences in socioeconomic inequalities were examined by including a multiplicative interaction term for sex/gender and each of the SEP variables in both age-adjusted and fully adjusted models. Separate models for women and men were planned if any of the interaction terms were statistically significant at α-level < 0.05.
To test the strength of the relationships, age-adjusted and fully adjusted interaction models were also computed using two other types of longitudinal regression, random effects and fixed effects. GEE and random effects both account for correlated data using within and between-individual information, whereas fixed effects use only within information and thus completely attribute the correlation of responses to the time-invariant characteristics of each person. Conclusions based on these models were similar to GEE. Analyses were performed using Stata SE 9 statistical software.[37]
RESULTS
Overview of the Data in Cross-Section
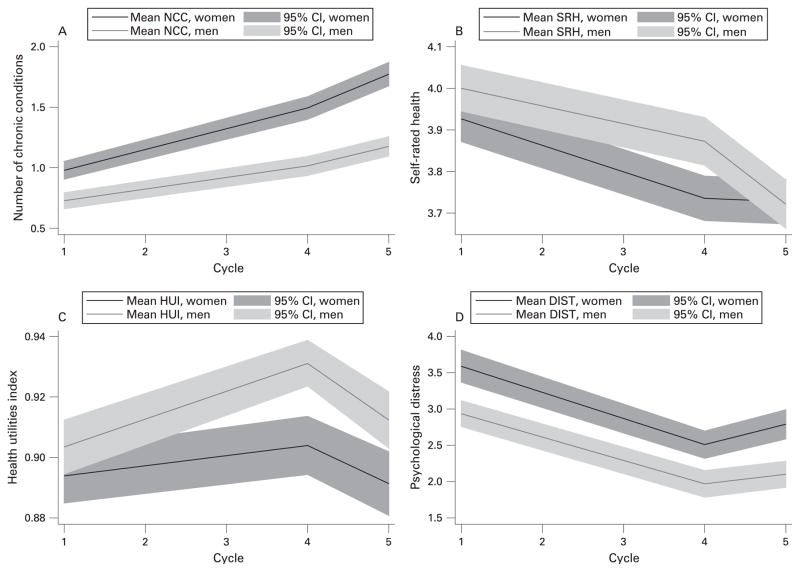
To get an overview of what is being modelled over time, Figure 2 contains the cross-sectional weighted means and 95% confidence intervals for the four health outcomes. It shows that the number of chronic conditions increased, self-rated health became worse, the health utilities index increased and then decreased, and mental distress lessened as the cohort aged. Overall, men had better health than women for each outcome, though the confidence intervals overlapped during some cycles. Table 1 displays the cross-sectional trends in SEP, structure, behaviour and psychosocial variables across survey waves. With regards to SEP, the proportion of individuals in the low income category decreased for both women and men over time, there were few transitions between education categories, and the proportion of employed individuals decreased for women, while it increased for men. Cross-sectional weighted means of the health outcomes and SEP proportions are presented in table 2 for those participants excluded from analysis because of incomplete data. Excluded individuals appeared to have worse health and lower SEP than those individuals who were analyzed. A sensitivity analysis was performed to compare GEE results of all eligible individuals except those missing for all three cycles (n=95) to the restricted sample (complete data for all three cycles). The results were similar.
Figure 2.
Weighted cross-sectional trajectories (means and 95% CIs) of health outcomes by cycle and sex/gender among working-aged Canadian women and men in the National Population Health Survey, 1994–2003. (A) Number of chronic conditions (NCCs); (B) self-rated health (SRH); (C) health utilities index (HUI); and (D) psychological distress (DIST). n = 1979 women, 1543 men.
Table 1.
Weighted cross-sectional means and percentages by cycle and sex/gender for socioeconomic position, social structure, behaviour and psychosocial measures among working-aged Canadian women and men in the National Population Health Survey, 1994–2003.
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Survey Cycle | 94/95 | 00/01 | 02/03 | 94/95 | 00/01 | 02/03 |
| Number of Observations | 1543 | 1543 | 1543 | 1979 | 1979 | 1979 |
| SEP Measures | ||||||
| Income Adequacy (%) | ||||||
| Middle/High (ref) | 90.2 | 96.1 | 96.4 | 87.5 | 92.3 | 93.3 |
| Low | 9.8 | 3.9 | 3.6 | 12.5 | 7.7 | 6.7 |
| Education (%) | ||||||
| < Secondary School (ref) | 14.4 | 12.9 | 12.7 | 12.8 | 11.3 | 11.1 |
| Secondary School Graduate | 40.5 | 40.6 | 41.0 | 46.3 | 44.8 | 44.1 |
| Post-secondary Graduate | 45.1 | 46.5 | 46.3 | 40.9 | 43.9 | 44.8 |
| Employment (%) | ||||||
| Inactive (ref) | 4.5 | 5.0 | 6.8 | 21.0 | 16.1 | 16.8 |
| Employed | 95.5 | 95.0 | 93.2 | 79.0 | 83.9 | 83.2 |
| Social Structure Measures | ||||||
| Age | 38.7 | 44.7 | 46.6 | 38.5 | 44.6 | 46.5 |
| Marital Status (%) | ||||||
| Unmarried (ref) | 22.9 | 21.5 | 22.3 | 24.1 | 24.2 | 24.5 |
| Married/cohabiting | 77.1 | 78.5 | 77.7 | 75.9 | 75.8 | 75.5 |
| Household Size | 3.2 | 3.1 | 3.1 | 3.3 | 3.2 | 3.1 |
| Social Support | 3.7 | 2.2 | 2.2 | 3.8 | 2.1 | 2.2 |
| Behavioural Measures | ||||||
| Smoking (pack-years) | 10.3 | 11.5 | 11.6 | 6.8 | 7.8 | 8.0 |
| Never Smoked (%) | ||||||
| Current/former smoker (ref) | 50.8 | 55.4 | 56.1 | 47.8 | 50.5 | 51.0 |
| Never smoked | 49.2 | 44.6 | 43.9 | 52.2 | 49.5 | 49.0 |
| Physical Activity Index (%) | ||||||
| Active (ref) | 17.4 | 18.0 | 23.6 | 15.2 | 16.0 | 20.8 |
| Moderate | 22.4 | 25.5 | 28.5 | 21.1 | 25.6 | 30.7 |
| Inactive | 60.2 | 56.5 | 47.9 | 63.7 | 58.4 | 48.5 |
| Body Mass Index (%) | ||||||
| Underweight | 0.4 | 0.7 | 0.7 | 2.7 | 1.5 | 1.8 |
| Normal weight (ref) | 39.1 | 30.4 | 28.5 | 58.4 | 50.7 | 46.6 |
| Overweight | 47.5 | 51.0 | 50.4 | 24.9 | 29.2 | 32.6 |
| Obese | 13.0 | 17.9 | 20.4 | 14.0 | 18.6 | 19.0 |
| Psychosocial Measures | ||||||
| Chronic Stress Index | 2.9 | 2.4 | 2.5 | 3.5 | 2.9 | 3.0 |
| Mastery | 20.5 | 20.3 | 19.9 | 19.9 | 20.0 | 19.5 |
Table 2.
Weighted cross-sectional means and percentages by cycle and sex/gender for health and socioeconomic position among working-aged Canadian women and men in the National Population Health Survey, 1994–2003, that were excluded from analysis for incomplete data.
| Survey Cycle | Men | Women | ||||
|---|---|---|---|---|---|---|
| 94/95 | 00/01 | 02/03 | 94/95 | 00/01 | 02/03 | |
| Health Outcomes | ||||||
| Number of Observations | 787 | 571 | 439 | 957 | 708 | 563 |
| Number of Chronic Conditions | 0.8 | 1.0 | 1.2 | 1.2 | 1.5 | 1.6 |
| Self-rated Health | 3.8 | 3.7 | 3.7 | 3.7 | 3.7 | 3.5 |
| Health Utilities Index | 0.9 | 0.9 | 0.9 | 0.9 | 0.9 | 0.9 |
| Psychological Distress | 3.2 | 2.2 | 2.3 | 4.1 | 3.1 | 2.8 |
|
| ||||||
| SEP Measures | ||||||
| Number of Observations | 736 | 591 | 449 | 773 | 579 | 471 |
| Income Adequacy (%) | ||||||
| Middle/High (ref) | 83.8 | 92.5 | 91.1 | 81.1 | 90.2 | 89.7 |
| Low | 16.2 | 7.5 | 8.9 | 18.9 | 9.8 | 10.3 |
| Education (%) | ||||||
| < Secondary School (ref) | 20.1 | 18.0 | 16.6 | 23.4 | 19.0 | 16.9 |
| Secondary School Graduate | 39.7 | 40.4 | 42.3 | 44.6 | 45.2 | 43.1 |
| Post-secondary Graduate | 40.2 | 41.6 | 41.1 | 32.0 | 35.8 | 40.0 |
| Employment (%) | ||||||
| Unemployed (ref) | 7.5 | 12.2 | 9.1 | 24.2 | 22.4 | 20.3 |
| Employed | 92.5 | 87.8 | 90.9 | 75.8 | 77.6 | 79.7 |
Effects of Sex/Gender and Changes in SEP on Health Over Time
In age-adjusted models, statistically significant differences in health between women and men were observed over time: men had fewer chronic conditions, higher HUI scores, and less mental distress than women, though there were no sex/gender differences in self-rated health (Table 3, model 1). Taking chronic conditions as an example, the average man in the population had 0.476 (95% CI -0.577, -0.376) fewer chronic conditions over the 10-year period than the average woman. In addition, people who experienced an increase in SEP over time had better health, and similarly those who decreased had worse health (Table 3, model 2). Those who changed from middle/high household income to low income had worse SRH and HUI scores, as well as more psychological distress compared to those who maintained their income level. Individuals with less than a high school education who attained their high school diploma or a post-secondary degree reported fewer chronic illnesses and better SRH and functional health than those who did not go back to school. Finally, those who became employed reported fewer chronic illnesses, rated their health to be better, had fewer functional limitations and suffered less mental distress than those who remained out of work, disabled, or retired.
Table 3.
GEE point estimates and 95% confidence intervals of changes in health due to longitudinal sex/gender differences and changes in socioeconomic position among working-aged Canadian women and men in the National Population Health Survey, 1994–2003. N = 3522.
| Variable | Model 1: Age-adjusted Sex/gender Differences | Model 2: Age-adjusted SEP Inequalities | Model 1 + 2: Fully adjusted2 Sex/gender & SEP | ||||
|---|---|---|---|---|---|---|---|
| β Coef | 95% CI | β Coef | 95% CI | β Coef | 95% CI | ||
| NCC1 | Male | − 0.476 | (−0.577, − 0.376) | − | − | −0.420 | (−0.522, − 0.317) |
| Low income | − | − | 0.043 | (−0.051, 0.137) | −0.011 | (−0.146, 0.124) | |
| High school graduate | − | − | 0.220 | (0.064, 0.376) | 0.234 | (0.079, 0.390) | |
| Post-secondary graduate | − | − | 0.217 | (0.066, 0.368) | 0.242 | (0.087, 0.398) | |
| Employed | − | − | − 0.250 | (−0.355, − 0.145) | −0.276 | (−0.410, − 0.143) | |
|
| |||||||
| SRH | Male | 0.059 | (−0.001, 0.118) | − | − | 0.034 | (−0.026, 0.094) |
| Low income | − | − | − 0.132 | (−0.204, − 0.060) | −0.056 | (−0.146, 0.034) | |
| High school graduate | − | − | 0.145 | (0.054, 0.237) | 0.081 | (−0.014, 0.176) | |
| Post-secondary graduate | − | − | 0.251 | (0.159, 0.344) | 0.164 | (0.068, 0.259) | |
| Employed | − | − | 0.220 | (0.145, 0.295) | 0.263 | (0.187, 0.338) | |
|
| |||||||
| HUI | Male | 0.016 | (0.007, 0.025) | − | − | 0.006 | (−0.003, 0.015) |
| Low income | − | − | − 0.024 | (−0.036, − 0.012) | −0.013 | (−0.029, 0.002) | |
| High school graduate | − | − | 0.012 | (−0.004, 0.027) | −0.003 | (−0.019, 0.013) | |
| Post-secondary graduate | − | − | 0.024 | (0.009, 0.039) | 0.004 | (−0.011, 0.012) | |
| Employed | − | − | 0.050 | (0.036, 0.064) | 0.057 | (0.039, 0.074) | |
|
| |||||||
| DIST | Male | − 0.642 | (−0.826, − 0.458) | − | − | −0.225 | (−0.401, − 0.049) |
| Low income | − | − | 0.798 | (0.551, 1.045) | 0.586 | (0.284, 0.888) | |
| High school graduate | − | − | − 0.058 | (−0.335, 0.219) | 0.288 | (0.031, 0.545) | |
| Post-secondary graduate | − | − | − 0.171 | (−0.453, 0.110) | 0.413 | (0.158, 0.667) | |
| Employed | − | − | − 0.562 | (−0.852, − 0.272) | −0.459 | (−0.739, − 0.179) | |
NCC = number of chronic conditions, SRH = self-rated health, HUI = health utilities index (functional health), DIST = psychological distress
Adjusted for structure (age, marital/partner status, household size, social support), behaviour (physical activity, BMI, smoking), and psychosocial (chronic stress, mastery)
Concurrently modeling sex/gender and SEP, while adjusting for social structure, health behaviours, and psychosocial characteristics, yielded similar results to the age-adjusted models for the number of chronic conditions and psychological distress, though not for SRH and HUI (Table 3, model 1+2). For HUI, significant disparities in sex/gender, income and education disappeared once fully adjusted. In addition, income and high school education no longer significantly predicted SRH in the fully adjusted model, although post-secondary education was still significant. Employment status, however, remained an important predictor for both SRH and HUI.
Interactive Effects between Sex/Gender and Changes in SEP on Health Over Time
Overall, the interaction terms between sex/gender and SEP were not statistically significant in either age-adjusted or fully adjusted GEE models (table 4). As significant differences between women and men were not present in the fully adjusted models for either SRH or HUI, the results for the interaction between sex/gender and SEP (also non-significant) are not shown. In addition, interaction models using random effects and fixed effects regression were mainly similar (results not shown).
Table 4.
GEE point estimates and 95% confidence intervals of changes in health due to interaction effects between gender and changes in socioeconomic position among working-aged Canadian women and men in the National Population Health Survey, 1994–2003. N = 3522.
| Variable | Model 3: Age-adjusted Interaction | Model 3: Fully-adjusted2 Interaction | |||
|---|---|---|---|---|---|
| β Coef | 95% CI | β Coef | 95% CI | ||
| NCC1 | Male | −0.158 | (−0.492, 0.175) | −0.142 | (−0.515, 0.231) |
| Low income | −0.005 | (−0.150, 0.140) | −0.037 | (−0.233, 0.160) | |
| Low income*male | 0.088 | (−0.093, 0.270) | 0.060 | (−0.200, 0.320) | |
| High school graduate | 0.240 | (0.019, 0.461) | 0.278 | (0.049, 0.501) | |
| High school graduate*male | −0.093 | (−0.402, 0.216) | −0.087 | (−0.385, 0.212) | |
| Post-secondary graduate | 0.225 | (0.010, 0.439) | 0.272 | (0.046, 0.497) | |
| Post-secondary grad*male | −0.051 | (−0.349, 0.248) | −0.061 | (−0.359, 0.237) | |
| Employed | −0.159 | (−0.280, −0.037) | −0.216 | (−0.369, −0.062) | |
| Employed*male | −0.248 | (−0.493, −0.002) | −0.238 | (−0.549, 0.074) | |
|
| |||||
| DIST | Male | −0.230 | (−0.981, 0.520) | 0.196 | (−0.501, 0.893) |
| Low income | 0.878 | (0.551, 1.204) | 0.709 | (0.318, 1.010 | |
| Low income*male | −0.236 | (−0.736, 0.263) | −0.302 | (−0.920, 0.316) | |
| High school graduate | −0.163 | (−0.593, 0.267) | 0.328 | (−0.049, 0.705) | |
| High school graduate*male | 0.117 | (−0.440, 0.674) | −0.085 | (−0.597, 0.427) | |
| Post-secondary graduate | −0.290 | (−0.736, 0.156) | 0.453 | (0.062, 0.845) | |
| Post-secondary grad*male | 0.179 | (−0.389, 0.746) | −0.079 | (−0.592, 0.434) | |
| Employed | −0.359 | (−0.703, −0.015) | −0.364 | (−0.683, −0.044) | |
| Employed*male | −0.480 | (−1.121, 0.161) | −0.358 | (−0.984, 0.267) | |
NCC = number of chronic conditions, DIST = psychological distress
Adjusted for structure (age, marital/partner status, household size, social support), behaviour (physical activity, BMI, smoking), and psychosocial (chronic stress, mastery)
DISCUSSION
The health of men and women in this nationally-representative sample of Canadians was not differentially impacted by changes in SEP, though both sex/gender and changes in SEP independently affected health. For the health outcomes examined here the magnitude of the effects of declining (or improving) SEP was similar for Canadian men and women. Poorer health across all outcomes, however, was observed for women, those whose income levels declined, those who did not finish at least high school, and those who were inactive in the labour force. After controlling for time-varying social structure, health-related behaviours and psychosocial factors, these effects persisted only for chronic conditions and psychological distress
Previous Research
The widely accepted view that men have generally steeper socioeconomic gradients in health than women[20–22] was not supported by this investigation or several other longitudinal studies.[8, 18, 23–25, 31] Men’s steeper gradients, when observed, have often been attributed to either methodological artefact or the differential exposure/vulnerability of men and women to the determinants of health.[2, 3, 20, 38] The lack of differential gradients in the NPHS may be partly explained by the control of both differential vulnerability and exposure in this analysis. The GEE models accounted for time-invariant illness propensity through the inclusion of within-individual information to adjust for correlated data. In addition, multiple time-dependent variables related to gender, namely social structure, health-related behaviours, and psychosocial factors, controlled for many of women’s and men’s differences in social exposures that may have arisen over the course of the survey. If the steeper socioeconomic gradients observed among men in previous studies were largely due to uncontrolled gender differences in vulnerability or exposure, it is understandable that we did not observe such gradient differences.
The possibility of methodological artefacts contributing to these findings must also be considered. Differences in reporting between women and men and socioeconomic groups have often been thought to contribute to gradient differences (or similarities).[40–42] As reporting bias is an inherent problem to survey research, Statistics Canada has used the best available measures to help minimize differential reporting in the NPHS.[32] Moreover, recent research has claimed that the threat of reporting bias is smaller than originally thought.[40–42] Sex/gender differences in socioeconomic gradients may also be the result of choices in measures of SEP and/or health outcome.[8, 21] However, despite using three measures of SEP (which were not found to be multi-collinear) and four measures of health, men did not exhibit steeper gradients. Furthermore, finer categorizations of SEP displayed similar results.
Implications of the Study
The results of this study do not preclude the possibility of differences in socioeconomic inequalities among women and men in Canada. Given the boundaries of observational research and the measurement of health and SEP in the NPHS, it is possible that sex/gender differences in socioeconomic gradients have gone undetected. However, given that results were robust to three different types of models using a large sample over a 10-year period, it is unlikely that Canadian men and women experience socioeconomic mobility differently.
One possible explanation for the lack of gradient differences is that this study reflects a context-specific situation, whereby SEP affects middle-aged Canadians similarly in 1994–2003 because of some unmeasured cohort effects. Individuals in this study were born between 1939 and 1959: Canadian women of this age group have attained similar education levels to men and are well-represented in the paid workforce.[43] In contrast, a British study that observed steeper socioeconomic gradients for men in the 1990s noted that women were often financially dependent on their male counterparts, 25–64% were housewives, and among those women who were employed, nearly half worked part-time.[44] Whereas SEP may not have as much of an impact on the health of British women, because of their relatively lower participation in the workforce, SEP may in fact have a similar meaning to the health of middle-aged Canadian women and men given their more similar involvement in the paid labour market.
Our study however, was not designed to answer this specific question: first, because our employment variable contrasted employed individuals (full or part-time) with those who were either out of work, retired or disabled, and second because it dealt only with the Canadian context. Future Canadian studies on this topic should use finer-grained categorizations of labour force participation, as our dichotomy may have obscured gender differences in full-time versus part-time and domestic work, as well as retirement (after ten years of follow-up, the oldest members would have been 60–64 years old); women are more likely to engage in part-time and domestic work [22] and take early retirement.[45] However, the true test of these effects is likely to only come from cross-national studies, which should examine whether differential (or similar) involvement in the paid labour market along those heterogeneous statuses may be at the root of these international inconsistencies in gender differences in socioeconomic inequalities in health. At the very least the results of our study emphasize the importance of re-examining over-generalized patterns in different historical and national contexts.
The lack of gradient differences between men and women in the NPHS may also be a consequence of the nature of the research questions examined. Previously observed cross-sectional sex/gender differences in socioeconomic inequalities may reflect baseline differences between men and women that may or may not persist over time. In contrast, the relationship of interest in longitudinal studies is the health impact of changes in SEP over time. Hence, it is possible that men and women indeed have different socioeconomic gradients at any given point in time (with men more often exhibiting stronger inequalities), although a change in SEP may not affect the health of men and women differentially. Cross-sectional and longitudinal research address very different questions and both types of analyses contribute to our understanding of the embodiment of SEP.
Strengths and Limitations
The major strengths of this research lie in the design of the survey and the methods of analysis employed. With respect to design, the NPHS is longitudinal, has a large sample size, is nationally representative, and makes use of extensively validated instruments for data collection. The statistical modeling techniques included weighting of the data, robust standard error correction, and testing for model misspecification. In addition, comparisons of the chosen longitudinal model, GEE, to other available models (i.e. fixed effects and random effects) yielded similar results.
This study, however, is not without its limitations. These are observational data spanning only ten years of follow-up. However, the inclusion of multiple time-dependent controls, in addition to using longitudinal models which account for within-individual heterogeneity, was an effort to reduce the likelihood of confounding, which is a common threat to observational studies. Another point of consideration is that time lag between SEP and the development or incidence of a given health outcome was not addressed.
As in any large-scale longitudinal survey, non-response and sample attrition may lead to selection bias if those who do not respond or who drop out of the survey are not representative of the target population. Multi-stage stratified probability sampling of participants and the use of cyclically adjusted sampling weights were an attempt to best reflect the 1994 Canadian population. Finally, information or misclassification bias could be problematic, as the data are self-reported; however, the NPHS has taken measures to help reduce misclassification[32] and the severity of this bias is contested in controlled research settings.[40–42] If present, it is difficult to know whether, confounding, selection bias, and/or misclassification would lead to an attenuation or an increase in the observed effect size.[46]
Conclusions
Although sex/gender and changes in SEP both independently impact the health of middle-aged men and women in the NPHS over time, there is no evidence to suggest that men embody changes in SEP to a greater extent than women. The absence in this study of the assumed “general pattern” of men’s steeper socioeconomic gradients [20] and its inconsistency in other longitudinal studies, highlight the need for more longitudinal research in other settings using similar datasets and modeling techniques. In addition, analyzing socioeconomic inequalities in health by specific roles, attitudes or opportunities (which may be typified by sex/gender, but are not restricted to either men or women) may elucidate what exactly about being a man or woman may result in differential socioeconomic gradients.
What is already known
Sex/gender and socioeconomic inequalities in health are ubiquitous in developed countries: women and those with lower socioeconomic position tend to have higher morbidity.
Examining the potentially different health impacts of changes in socioeconomic position over time is necessary to help resolve the debate on whether men exhibit steeper socioeconomic gradients than women.
What this study adds
Middle-aged Canadian men and women do not differentially embody changes in socioeconomic position, though both gender and changes in socioeconomic position independently impact health.
These results demonstrate the importance of re-examining over-generalized patterns in different contexts.
Acknowledgments
Sources of Funding: Serena Luchenski, Master’s Training Award provided by Fonds de la recherche en santé Québec; Fellowship Award provided by the Québec Inter-University Centre for Social Statistics Matching Grants Program; Top-up Grant provided by Canadian Institutes of Health Research operating grant MOP-77800 (PI: Amélie Quesnel-Vallée). Amélie Quesnel-Vallée, Canadian Institutes of Health Research operating grant MOP-77800; Career award (Chercheur-boursier Junior 1) provided by Fonds de la recherche en santé Québec
APPENDIX: MEASUREMENT OF COVARIATES IN THE NATIONAL POPULATION HEALTH SURVEY, 1994–2003
|
Social Structure
| ||
| Age | Continuous | Age on the day of interview in 1994 |
| Marital/partner status | Binary | 0 = married, common-law, living with a partner, 1 = single (never-married), widowed, separated, divorced |
| Household size | Continuous | Number of individuals living in the household |
| Social Support | Ordinal 0–4 | Cycles 1& 2, social support was measured by the perceived social support index which is composed of four items on whether respondents feel that they have someone they can confide in, someone they can count on, someone who can give them advice and someone who makes them feel loved. In cycles 3–5, social support was measured by four separate indices, corresponding to each of the four items that the perceived social support index measured. These indices were summed and quartiles were calculated to be able use a similar 0–4 scoring method as the perceived social support index in cycles 1&2. |
|
| ||
|
Health-related Behaviours
| ||
| Physical activity | Ordinal 1–3 | Active (amount of exercise required for cardiovascular benefit), moderate (some health benefits, but no cardiovascular benefit), and inactive categories were derived from a continuous variable that calculated the energy expenditure (frequency, duration, MET value) for a range of leisure activities. |
| Body mass index | Ordinal 1–4 | BMI is weight in kg/(height in m)2. Individuals were classified as 1 = underweight (BMI <18.5), 2 = normal (>18.5 and <25.0), 3 = overweight (>25.0 and <30.0), and 4 = obese (>30.0). |
| Smoking (Pack-years) | Continuous | Pack-years (number of packs smoked per year x the number of years smoked) were computed from multiple variables in the dataset, including data for current, former, occasional, and never smokers |
| Smoking (Never smoked) | Binary | As the pack-years variable was highly skewed towards 0, an additional control was created to account for those that never smoked. 1= never smoked 0 = smoker in any capacity |
|
| ||
|
Psychosocial Factors
| ||
| Chronic stress | Ordinal 0–16 | This index measures the total number of stressors respondents were exposed to. The range of the final score (as well as the number of questions) varies as a function of the respondents’ personal situation. For example, for partnered persons, questions about relationship with partner are included. For persons not partnered, the index contains a question on the difficulty of finding someone compatible. For persons who have children, questions about children become part of the index. |
| Mastery | Ordinal 0–35 | This index measures the extent to which individuals believe that their life-chances are under their control. There are 7 items in the index and responses are on a 5-point scale |
Footnotes
Competing Interests: None
Contributor Information
Amélie Quesnel-Vallée, Email: amelie.quesnelvallee@mcgill.ca, Department of Sociology, Department of Epidemiology, Biostatistics and Occupational Health, McGill University.
Serena Luchenski, Department of Epidemiology, Biostatistics and Occupational Health, McGill University.
John Lynch, Department of Epidemiology, Biostatistics and Occupational Health, McGill University.
References
- 1.Rieker PP, Bird CE. Rethinking gender differences in health: why we need to integrate social and biological perspectives. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 2):40–7. doi: 10.1093/geronb/60.special_issue_2.s40. [DOI] [PubMed] [Google Scholar]
- 2.Denton M, Prus S, Walters V. Gender differences in health: a Canadian study of the psychosocial, structural and behavioural determinants of health. Soc Sci Med. 2004;58:2585–600. doi: 10.1016/j.socscimed.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 3.McDonough P, Walters V. Gender and health: reassessing patterns and explanations. Soc Sci Med. 2001;52:547–59. doi: 10.1016/s0277-9536(00)00159-3. [DOI] [PubMed] [Google Scholar]
- 4.Macintyre S, Hunt K, Sweeting H. Gender differences in health: are things really as simple as they seem? Soc Sci Med. 1996;42:617–24. doi: 10.1016/0277-9536(95)00335-5. [DOI] [PubMed] [Google Scholar]
- 5.Gorman BK, Read JG. Gender disparities in adult health: An examination of three measures of morbidity. Journal J Health Soc Behav. 2006;47:95–110. doi: 10.1177/002214650604700201. [DOI] [PubMed] [Google Scholar]
- 6.Emslie C, Hunt K, Macintyre S. Problematizing gender, work and health: the relationship between gender, occupational grade, working conditions and minor morbidity in full-time bank employees. Soc Sci Med. 1999;48:33–48. doi: 10.1016/s0277-9536(98)00287-1. [DOI] [PubMed] [Google Scholar]
- 7.Lahelma E, Martikainen P, Rahkonen O, et al. Gender differences in illhealth in Finland: patterns, magnitude and change. Soc Sci Med. 1999;48:7–19. doi: 10.1016/s0277-9536(98)00285-8. [DOI] [PubMed] [Google Scholar]
- 8.Matthews S, Manor O, Power C. Social inequalities in health: are there gender differences? Soc Sci Med. 1999;48:49–60. doi: 10.1016/s0277-9536(98)00288-3. [DOI] [PubMed] [Google Scholar]
- 9.Duetz MS, Abel T, Niemann S. Health measures - Differentiating associations with gender and socio-economic status. Eur J Public Health. 2003;13:313–9. doi: 10.1093/eurpub/13.4.313. [DOI] [PubMed] [Google Scholar]
- 10.Frank JW, Cohen R, Yen I, et al. Socioeconomic gradients in health status over 29 years of follow-up after midlife: the Alameda county study. Soc Sci Med. 2003;57:2305–23. doi: 10.1016/j.socscimed.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Knesebeck OV, Verde PE, Dragano N. Education and health in 22 European countries. Soc Sci Med. 2006;63:1344–51. doi: 10.1016/j.socscimed.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 12.van Lenthe FJ, Schrijvers CTM, Droomers M, et al. Investigating explanations of socioeconomic inequalities in health - The Dutch GLOBE study. Eur J Public Health. 2004;14:63–70. doi: 10.1093/eurpub/14.1.63. [DOI] [PubMed] [Google Scholar]
- 13.Silventoinen K, Lahelma E. Health inequalities by education and age in four Nordic countries, 1986 and 1994. J Epidemiol Community Health. 2002;56:253–8. doi: 10.1136/jech.56.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Power C, Matthews S, Manor O. Inequalities in self-rated health: explanations from different stages of life. Lancet. 1998;351:1009–14. doi: 10.1016/S0140-6736(97)11082-0. [DOI] [PubMed] [Google Scholar]
- 15.Ford G, Ecob R, Hunt K, et al. Patterns of class inequality in health through the lifespan: class gradients at 15, 35 and 55 years in the west of Scotland. Soc Sci Med. 1994;39:1037–50. doi: 10.1016/0277-9536(94)90375-1. [DOI] [PubMed] [Google Scholar]
- 16.Anitua C, Esnaola S. Changes in social inequalities in health in the Basque Country. J Epidemiol Community Health. 2000;54:437–43. doi: 10.1136/jech.54.6.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asthana S, Gibson A, Moon G, et al. The demographic and social class basis of inequality in self reported morbidity: an exploration using the Health Survey for England. J Epidemiol Community Health. 2004;58:303–7. doi: 10.1136/jech.2002.003475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ross CE, Mirowsky J. Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Soc Sci Med. 2006;63:1400–13. doi: 10.1016/j.socscimed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Macintyre S, Hunt K. Socio-economic Position, Gender and Health: How Do They Interact? J Health Psychol. 1997;2:315–34. doi: 10.1177/135910539700200304. [DOI] [PubMed] [Google Scholar]
- 20.Macintyre S. Inequalities in health: is research gender blind? In: Leon D, Walt G, editors. Poverty, Inequality and Health. New York: Oxford University Press; 2001. pp. 247–62. [Google Scholar]
- 21.Koskinen S, Martelin T. Why are socioeconomic mortality differences smaller among women than among men? Soc Sci Med. 1994;38:1385–96. doi: 10.1016/0277-9536(94)90276-3. [DOI] [PubMed] [Google Scholar]
- 22.Elo IT, Preston SH. Educational differentials in mortality: United States, 1979–85. Soc Sci Med. 1996;42:47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- 23.Andersen I, Osler M, Petersen L, et al. Income and risk of ischaemic heart disease in men and women in a Nordic welfare country. Int J Epidemiol. 2003;32:367–74. doi: 10.1093/ije/dyg073. [DOI] [PubMed] [Google Scholar]
- 24.McDonough P, Williams DR, House JS, et al. Gender and the socioeconomic gradient in mortality. J Health Soc Behav. 1999;40:17–31. [PubMed] [Google Scholar]
- 25.Thurston RC, Kubzansky LD, Kawachi I, et al. Is the association between socioeconomic position and coronary heart disease stronger in women than in men? Am J Epidemiol. 2005;162:57–65. doi: 10.1093/aje/kwi159. [DOI] [PubMed] [Google Scholar]
- 26.Diaz MDM. Socio-economic health inequalities in Brazil: gender and age effects. Health Econ. 2002;11:141–54. doi: 10.1002/hec.649. [DOI] [PubMed] [Google Scholar]
- 27.Hemstrom O. Health inequalities by wage income in Sweden: The role of work environment. Soc Sci Med. 2005;61:637–47. doi: 10.1016/j.socscimed.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 28.Wu J, Liu YL, Rao KQ, et al. Education-related gender differences in health in rural China. Am J Public Health. 2004;94:1713–6. doi: 10.2105/ajph.94.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: do gender, age, and ethnicity matter? Soc Sci Med. 2004;58:1171–80. doi: 10.1016/s0277-9536(03)00288-0. [DOI] [PubMed] [Google Scholar]
- 30.Denton M, Walters V. Gender differences in structural and behavioral determinants of health: an analysis of the social production of health. Soc Sci Med. 1999;48:1221–35. doi: 10.1016/s0277-9536(98)00421-3. [DOI] [PubMed] [Google Scholar]
- 31.McDonough P, Duncan GJ, Williams D, House J. Income Dynamics and Adult Mortality in the United States, 1972 through 1989. Am J Public Health. 1997;87:1476–83. doi: 10.2105/ajph.87.9.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Statistics Canada. National Population Health Survey Household Component Cycle 5 (2002–2003) Longitudinal Documentation. Ottawa: 2004. [Google Scholar]
- 33.McCullough ME, Laurenceau JP. Gender and the Natural History of Self-Rated Health: A 59-Year Longitudinal Study. Health Psychol. 2004;23:651–5. doi: 10.1037/0278-6133.23.6.651. [DOI] [PubMed] [Google Scholar]
- 34.Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40:113–28. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 35.StataCorp. Stata Longitudinal/Panel Data Reference Manual Release 9. College Station, Texas: Stata Press; 2005. [Google Scholar]
- 36.Moerman CJ, van Mens-Verhulst Gender-sensitive epidemiological research: suggestions for a gender-sensitive approach towards problem definition, data collection and analysis in epidemiological research. Psychology, Health and Medicine. 2004;9(1):41–52. [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 9. College Station, Texas: StataCorp LP; 2005. [Google Scholar]
- 38.Reiker PP, Bird CE. Sociological Explanations of Gender Differences in Mental and Physical Health. In: Conrad PAF, editor. The Handbook of Medical Sociology. Englewood Cliffs, NJ: Prentice Hall; 2000. pp. 98–113. [Google Scholar]
- 39.Mustard CA, Etches J. Gender differences in socioeconomic inequality in mortality. J Epidemiol Community Health. 2003;57:974–80. doi: 10.1136/jech.57.12.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Macintyre S, Ford G, Hunt K. Do women ‘over-report’ morbidity? Men’s and women’s responses to structured prompting on a standard question on long standing illness. Soc Sci Med. 1999;48:89–98. doi: 10.1016/s0277-9536(98)00292-5. [DOI] [PubMed] [Google Scholar]
- 41.Macintyre S, Der G, Norrie J. Are there socioeconomic differences in responses to a commonly used self report measure of chronic illness? Int J Epidemiol. 2005;34:1284–90. doi: 10.1093/ije/dyi200. [DOI] [PubMed] [Google Scholar]
- 42.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender Differences in the Comparison of Self-Reported Disability and Performance Measures. J Gerontol. 1997;52A:M19–M26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 43.Statistics Canada. Women in Canada 2000: A Gender-Based Statistical Report. Ottawa: Ministry of Industry; 2000. [Google Scholar]
- 44.Rahkonen O, Arber S, Lahelma E, et al. Understanding income inequalities in health among men and women in Britain and Finland. Int J Health Serv. 2000;30:27–47. doi: 10.2190/VBJT-5LFB-62Y0-4Y29. [DOI] [PubMed] [Google Scholar]
- 45.Kieran P. Early retirement trends. Perspectives on Labour and Income: The Online Edition. 2001;2 http://www.statcan.ca/english/freepub/75-001-XIE/00901/ar-ar200109_01_a.html. [Google Scholar]
- 46.Rothman KJ. Epidemiology: An Introduction. New York: Oxford University Press; 2002. [Google Scholar]