Abstract
Background
Enterohemorrhagic Escherichia coli (EHEC) cause diarrhea-associated hemolytic uremic syndrome (D+ HUS) worldwide, but no systematic study of EHEC as the causative agents of HUS was performed in the Czech Republic. We analyzed stools of all patients with D+ HUS in the Czech Republic between 1998 and 2012 for evidence of EHEC infection. We determined virulence profiles, phenotypes, antimicrobial susceptibilities and phylogeny of the EHEC isolates.
Methodology/Principal Findings
Virulence loci were identified using PCR, phenotypes and antimicrobial susceptibilities were determined using standard procedures, and phylogeny was assessed using multilocus sequence typing. During the 15-year period, EHEC were isolated from stools of 39 (69.4%) of 56 patients. The strains belonged to serotypes [fliC types] O157:H7/NM[fliC H7] (50% of which were sorbitol-fermenting; SF), O26:H11/NM[fliC H11], O55:NM[fliC H7], O111:NM[fliC H8], O145:H28[fliC H28], O172:NM[fliC H25], and Orough:NM[fliC H25]. O26:H11/NM[fliC H11] was the most common serotype associated with HUS (41% isolates). Five stx genotypes were identified, the most frequent being stx 2a (71.1% isolates). Most strains contained EHEC-hlyA encoding EHEC hemolysin, and a subset (all SF O157:NM and one O157:H7) harbored cdt-V encoding cytolethal distending toxin. espPα encoding serine protease EspPα was found in EHEC O157:H7, O26:H11/NM, and O145:H28, whereas O172:NM and Orough:NM strains contained espPγ. All isolates contained eae encoding adhesin intimin, which belonged to subtypes β (O26), γ (O55, O145, O157), γ2/θ (O111), and ε (O172, Orough). Loci encoding other adhesins (efa1, lpfA O26, lpfA O157OI-141, lpfA O157OI-154, iha) were usually associated with particular serotypes. Phylogenetic analysis demonstrated nine sequence types (STs) which correlated with serotypes. Of these, two STs (ST660 and ST1595) were not found in HUS-associated EHEC before.
Conclusions/Significance
EHEC strains, including O157:H7 and non-O157:H7, are frequent causes of D+ HUS in the Czech Republic. Identification of unusual EHEC serotypes/STs causing HUS calls for establishment of an European collection of HUS-associated EHEC, enabling to study properties and evolution of these important pathogens.
Introduction
Enterohemorrhagic Escherichia coli (EHEC) are the pathogenic subgroup of Shiga toxin (Stx)-producing E. coli strains that cause human diseases including diarrhea, bloody diarrhea and hemolytic uremic syndrome (HUS). HUS is a severe, potentialy life-threatening condition characterized by non-immune hemolytic anemia, thrombocytopenia, and acute renal failure [1]. HUS caused by EHEC strains is typically preceded with diarrhea (and therefore designated D+ HUS), that usually begins as non-bloody and progresses to bloody after several days [1]. D+ HUS usually affects children under 5 years [1] and is the most common cause of acute renal insufficiency in children. It develops in 10–15% children infected with EHEC O157:H7 [1] and also complicates infections with other EHEC serotypes [2]–[9]. In addition to the kidneys, other organs can be affected during HUS including the central nervous system, the pancreas, the heart, the liver and the lungs [1]. The involvement of the central nervous system is the most severe and is associated with higher mortality [6]. The mortality of D+ HUS during the acute phase is <5%, and there is a high frequency of late renal or non-renal sequelae in survivors [10], [11].
Microvascular endothelial damage is the major pathological change underlying HUS [1], [12]. Stxs are presently the best characterised EHEC virulence factors that cause the microvascular endothelial injury [12]. Stxs are released by EHEC in the intestine, absorbed across the intestinal epithelium into the circulation, and transported to microcapillaries of the target organs, mainly the kidneys and the brain. Here Stxs bind to glycosphingolipids of the globo-series, which are abundantly expressed on both glomerular and brain microvascular endothelial cells [13], [14]. This triggers a complex cascade of events resulting in a multi-organ thrombotic process [12]. Although the Stx family is highly heterogeneous, not all Stx types have been associated with HUS [15], [16]. Stx2 is the most common Stx type found in EHEC isolated from HUS patients [3], [15]–[17], but Stx2c, Stx2d and Stx1 also occur in HUS-associated EHEC [3], [15]. In contrast, Stx2b, Stx2e, Stx2f and Stx2g have not been found at all or are found very rarely among HUS isolates [15], [16], [18]–[20]. A possible explanation for the epidemiological association of Stx2 with severe outcome of EHEC infections is the in vitro observation that Stx2 is significantly more cytotoxic towards human renal [21] and human brain [22] microvascular endothelial cells than Stx1.
The classical non-sorbitol-fermenting (NSF) EHEC O157:H7 is the predominant cause of HUS worldwide [1], [23], [24]. In addition, several other EHEC serotypes, the most frequent of which are O26:H11/NM (non-motile), O91:H21, O103:H2/NM, O111:H8/NM, O113:H21, and O145:H25/H28/NM, have been increasingly recognized as causes of HUS in Europe [3]–[5], [7], [17], [25]–[27], North America [8], South America [20], and Australia [28]. EHEC strains that have the capability of causing HUS have been designated HUSEC (HUS-associated E. coli) [3].
The role of EHEC as causes of HUS in the Czech Republic has not yet been systematically studied. Here, we investigated stool samples from all patients with D+ HUS hospitalized in pediatric centers in the Czech Republic between 1998 and 2012 for EHEC infection. We determined serotypes of the EHEC isolates, a subset of molecular and phenotypic characteristics, and their phylogenetic relationships. Moreover, we determined susceptibilities of the strains to a spectrum of antimicrobials.
Materials and Methods
Ethics Statement
This study was approved by the Ethical Committee of the University Hospital Motol, Prague, Czech Republic. Written informed consent for enrollment in the study and publication of patientś data was obtained from parents of all patients.
Patients and Stool Samples
During January 1998 to December 2012, stool samples from 56 patients with HUS were investigated for EHEC infection in the Reference Laboratory for E. coli and Shigella of the National Institute of Public Health in Prague, Czech Republic. This laboratory is specialized for diagnosis of EHEC infections and receives stools from all patients with HUS from this country. The patients originated from different regions of the Czech Republic and there were no apparent temporal or geographical linkages between them. Thirty-four of 56 patients (60.7%) were boys and 22 (39.3%) were girls. All patients were children (median age, 27.5 months; range, 10 to 85 months). Stool samples were collected between 2 and 15 days (median, 6 days) after the onset of prodromal diarrhea.
Case Definition
HUS was defined as a case of microangiopathic hemolytic anemia (hematocrit <30% with peripheral evidence of intravascular hemolysis), thrombocytopenia (platelet count <150,000 platelets/mm3), and renal insufficiency (serum creatinine concentration higher than the upper limit of the normal range for age) [1].
Detection of EHEC in and Isolation from Patients Stools
The stool samples were enriched in G.N. Enrichment Broth (Hajna) (Laboratorios Conda, Madrid, Spain) with novobiocin supplement (Oxoid, Hampshire, UK) for 5–7 hours (37°C, 180 rpm) and the enriched cultures were inoculated on Columbia blood agar, sorbitol MacConkey agar (SMAC), cefixime-tellurite (CT)-SMAC agar and enterohemolysin agar (all from Oxoid). Since 2008, the enrichment cultures were additionally examined for the presence of E. coli O157, O26, O103, O111, and O145 using an immunomagnetic separation (Dynabeads anti-E. coli O157, Dynabeads EPEC/VTEC O26, Dynabeads EPEC/VTEC O103, Dynabeads EPEC/VTEC O111, Dynabeads EPEC/VTEC O145) according to the manufactureŕs (Dynal, Oslo, Norway) protocol and subsequently plated on the above media. After overnight incubation at 37°C, bacterial growth from all four plates was collected in a tube containing 1ml of 0.85% NaCl; 100 µl of this suspension was dilluted 1∶10 in sterile distilled water, heated for 10 min at 100°C and centrifuged (12000 rpm, 10 min). Supernatant was used as a template for PCR with primers KS7-KS8, LP43-LP44, and SK1-SK2 which target stx 1a, stx 2a and eae, respectively [3], [15]. All stx-positive samples were further PCR tested for genes of O antigen biosynthetic clusters of E. coli O157, O26, O55, O111, O103, O145, O91 and O113 [29]–[31]. To isolate strains from samples with positive stx PCR results, bacterial suspensions were restreaked on SMAC, CT-SMAC and enterohemolysin agar plates. E. coli O157:H7 was isolated from SMAC and/or CT-SMAC using agglutination of sorbitol-negative colonies in O157 antiserum (Denka Seiken Ltd., Tokyo, Japan). EHEC of the major non-O157 serogroups (O26, O111, O145) were isolated from enterohemolysin agar based on their typical enterohemolytic phenotype combined with agglutination in antisera against the respective E. coli O antigens (Sifin, Berlin, Germany; Denka Seiken). If no sorbitol-negative or enterohemolytic colonies were present on SMAC/CT-SMAC or enterohemolysin agar, respectively, multiple colonies from these plates (altogether up to 50) were tested for stx 1a and stx 2a genes using PCRs described above. The isolates were confirmed as E. coli biochemically (API 20E; bioMérieux, Marcy l’Etoile, France) and using a MALDI-TOF mass spectrometer (Microflex LT, Bruker Daltonics, Germany). Mass spectra were processed using the BioTyper software with the version 3.2.1.0. database. Motility of the isolates was determined directly after isolation as follows: The strains were inoculated into the middle of tubes containing soft (0.5%) agar, incubated at 37°C and observed for growth daily. An isolate was considered motile if it spread out of the original inoculation site during 10 days. If there was no growth from the inoculation site during this time, the isolate was considered nonmotile (NM).
Detection of other Enteric Bacterial Pathogens in Stools
The presence of Salmonella spp., Shigella spp., Yersinia enterocolitica, and Campylobacter jejuni in stools was sought using standard microbiological procedures.
Serotyping
stx positive colonies were serotyped using agglutination in polyvalent and monovalent E. coli O antisera (Denka Seiken Co., Ltd., Tokyo, Japan; Sifin, Berlin, Germany; Robert Koch Institute, Wernigerode, Germany) and H antisera (Denka Seiken). The presence of the O26, O55, O111, O145, O157, and O172 antigens was confirmed using PCRs targeting genes of the respective O antigen biosynthetic clusters [29]–[32]. The flagellin subunit–encoding fliC gene was subtyped using HhaI restriction fragment length polymorphism as described previously [7].
Genotypic Characteristics
PCRs were performed in a MyCycler Thermal Cycler (Bio-Rad, München, Germany) using reagents from Top-Bio (Prague, Czech Republic) and primers from Generi Biotech (Hradec Kralove, Czech Republic). All isolates were tested for stx 1a, stx 2a, and their subtypes (stx 1c, stx 2b, stx 2c, stx 2d stx 2e, stx 2f) using published PCR protocols [15], [16]. Genes encoding other toxins (cdt-V, EHEC-hlyA, α-hlyA), the EHEC serine protease EspP (espP), and adhesins (eae, efa1, lpfA O26, lpfA O157OI-141, lpfA O157OI-154, iha) were PCR detected as described previously [15], [33]–[38]. eae genes were subtyped according to Zhang et al. [39] (eae β, γ, ε) and Blanco et al. [40] (eae γ2/θ). espP genes were subtyped according to Brockmeyer et al. [36]. terE and ureD used as markers for the ter and ure gene clusters, which encode tellurite resistance urease production, respectively, were amplified as described previously [41], [42]. Genes within the O island (OI) 122 of EHEC O157:H7 strain EDL933 (efa1, sen, nleE, nleB, pagC) were detected using published PCR protocols [25], [43].
Phenotypic Characteristics
Utilization of sorbitol was tested on SMAC. Moreover, utilization of sorbitol, rhamnose and production of lysine decarboxylase (LDC) was evaluated according to the API 20E test kit (bioMérieux). Production of β-D-glucuronidase was investigated using COLItest (Erba Lachema, Brno, Czech Republic). Production of EHEC hemolysin and α hemolysin was sought using enterohemolysin agar and Columbia blood agar (Oxoid), respectively. Production of Stx was tested using a Vero cell cytotoxicity assay [2]. The Stx titer was defined as the highest dilution of culture supernatant that caused cytotoxicity in 50% cells after 3 days of incubation. The Stx types (Stx1, Stx2) were identified using VTEC-RPLA assay (Denka Seiken) according to the manufacturer’s instructions. Resistance to tellurite was determined based on the ability of the strains to grow on CT-SMAC. Urease production was determined using the API 20E test.
Antimicrobial Susceptibility Testing
Susceptibility to ampicillin, cefotaxime, ceftazidime, gentamicin, trimethoprim/sulfamethoxazole, ciprofloxacin, amikacin, meropenem, piperacillin/tazobactam, tigecycline, chloramphenicol, and nitrofurantoin was tested using the disk diffusion method according to EUCAST breakpoints [44] and standard recommendations [45].
Multilocus Sequence Typing (MLST)
MLST was performed by sequencing internal fragments of seven housekeeping genes (adk, fumC, gyrB, icd, mdh, purA, and recA) as described previously [3]. Sequences were analyzed and the minimum-spanning tree was constructed using the SeqSphere software version 0.9 beta.1 (Ridom GmbH, Münster, Germany). All alleles and sequence types (ST) were assigned in accordance with the MLST website (http://mlst.ucc.ie/mlst/dbs/Ecoli).
Results
Clinical Features
Among the 56 patients investigated, 52 (92.9%) had prodromal diarrhea, which was bloody in 31 (59.6%). HUS was diagnosed between 2 and 15 days (median, 6 days) after the onset of diarrhea. The median length of hospitalization was 17 days (range, 4 to 55 days). Three patients (5.4%) died during acute phase of HUS. The causes of the deaths were neurological complications (cerebral edema) in two patients (girls, 18 and 25 months old, both infected with EHEC O26:H11), one of whom also developed lung edema; one patient (boy, 30 months old, infected with sorbitol-fermenting (SF) EHEC O157:NM) died of acute renal failure. Deaths occurred between 3 and 6 days (median, 3 days) after HUS development.
Serotypes and fliC Genotypes of EHEC Isolates
Stool samples from 39 of 56 patients (69.6%) were positive in screening for stx 1a and/or stx 2a genes using PCR. EHEC strains were isolated from all of these 39 stx-positive stool samples. Thirty-seven isolates belonged to eight different serotypes and two were non-typeable (Orough) (Table 1). The most common serotype was O26:H11/NM (non-motile), which accounted for 16 (41%) of 39 isolates (Table 1). The second most common serotype was O111:NM (six of 39 isolates; 15.4%). NSF EHEC O157:H7/NM were isolated from five (12.8%) patients and an additional five patients (12.8%) were positive for SF EHEC O157:NM strains (Table 1). One isolate belonged to serotype O172:NM, which has been rarely isolated from patients with HUS [25].
Table 1. Serotypes and genotypic characteristics of EHEC strains isolated from patients with HUS in the Czech Republic, 1998–2012.
| Virulence locusa | Serotype (number of strains)b | |||||||
| O157:H7/NM (NSF) | O157:NM (SF) | O55:NM | O26:H11/NM | O111:NM | O145:H28 | O172:NM | Orough:NM | |
| fliC H7 (n = 5) | fliC H7 (n = 5) | fliC H7 (n = 2) | fliC H11 (n = 16) | fliC H8 (n = 6) | fliC H28 (n = 2) | fliC H25 (n = 1) | fliC H25 (n = 2) | |
| stx 1a | −c | – | – | + (1)c | + (2) | – | – | – |
| stx 2a | + (1) | + (4)d | + | + (15) | – | + | + | + |
| stx 1a +stx 2a | – | – | – | – | + (4) | – | – | – |
| stx 1a +stx 2c | + (2) | – | – | – | – | – | – | – |
| stx 2a +stx 2c | + (2) | – | – | – | – | – | – | – |
| cdt–V | + (1) | + | – | – | – | – | – | – |
| EHEC–hlyA | + | + (4) | – | + | + (4) | + | + | + |
| α–hlyA | – | – | – | – | – | – | – | – |
| espP e | + (α) | – | – | + (α) (9) | – | + (α) (1) | + (γ) | + (γ) |
| eae f | + (γ) | + (γ) | + (γ) | + (ß) | + (γ2/θ) | + (γ) | + (ε) | + (ε) |
| efa1 | +g | + | + | + | + | +g | + | + |
| lpfA O26 | – | – | – | + | + | – | – | – |
| lpfA O157/OI–141 | + | + | + | – | – | + | – | – |
| lpfA O157/OI–154 | + | + | + | – | – | – | – | – |
| iha | + | – | – | + | + (5) | + | – | – |
| terE | + | – | – | + | + (5) | + | – | – |
| ureD | + | – | – | + | + (5) | + | – | – |
| irp2 | – | – | – | + | – | – | – | – |
| fyuA | – | – | – | + | – | – | – | – |
The genes encode the following proteins: fliC, flagellar subunit of H antigen; stx, Shiga toxin; cdt-V, cytolethal distending toxin V; EHEC-hlyA, EHEC hemolysin; α-hlyA,
α hemolysin; espP, serine protease EspP; eae, intimin; efa1, EHEC factor for adherence; lpfA O26, major subunit of long polar fimbriae of EHEC O26; lpfA O157/OI-141 and lpfA O157/OI-154, major subunit of long polar fimbriae of EHEC O157 encoded on O island OI 154 and OI 141, respectively; iha, iron-regulated gene A homologue adhesin; terE, marker for tellurite resistence-encoding cluster; ureD, marker for ure cluster encoding urease production; irp2 and fyuA, markers for the high pathogenicity island (HPI) encoding iron uptake system.
Serotypes were determined using conventional and molecular serotyping; the fliC genes indicated were present in both motile and non-motile strains of each respective serotype; NSF, non-sorbitol-fermenting; SF, sorbitol-fermenting.
−, the gene was absent; +, the gene was present (if the gene was not present in all strains of the respective serotype, the numbers of positive strains are indicated in parenthesis).
one strain lost stx gene before subtyping.
espP subtypes are indicated in parentheses.
eae subtypes are indicated in parentheses.
a truncated efa1 gene [34] was present in EHEC O157:H7 and one O145:H28 isolate; complete efa1 was present in all other strains.
Seven of 10 O157 isolates (two NSF and all five SF), six of 16 (37.5%) O26 isolates, and all O111, O55, O172 and Orough isolates were non-motile, making conventional H typing impossible (Table 1). Subtyping of fliC genes encoding the flagellar subunit of the H antigens demonstrated that the non-motile O157 and O26 isolates contained fliC H7 and fliC H11, respectively, which was also present in motile isolates of these serotypes. The non-motile isolates of serogroups O111, O55 and O172 contained fliC H8, fliC H7, and fliC H25, respectively (Table 1), allowing rapid molecular H typing. fliC H25 was also present in both Orough:NM isolates (Table 1).
None of the 39 patients from whom EHEC strains were isolated had other intestinal bacterial pathogens (Salmonella spp., Shigella spp., Y. enterocolitica, C. jejuni) in their stools.
Seasonal Distribution of EHEC Serotypes
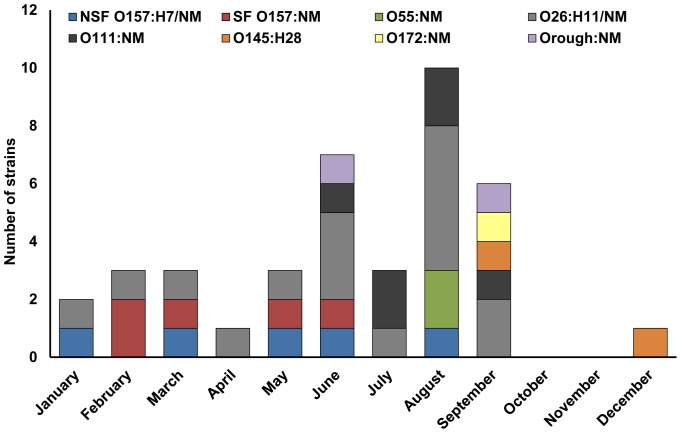
Most EHEC strains (29 of 39; 74.4%) were isolated during the warm period of the year (May to September) (Figure 1). However, no clear seasonality in occurrence of particular serotypes was observed. NSF O157:H7/NM strains were isolated from January through August and SF O157:NM from February to June. O26:H11/NM isolates were almost equally distributed throughout the year (Figure 1).
Figure 1. Seasonal distribution of EHEC strains of different serotypes isolated from patients with HUS in the Czech Republic, 1998–2012.
stx Genotypes
stx genes were present in all 39 EHEC isolates upon isolation, but one strain (SF O157:NM) lost its stx gene during laboratory subcultures before stx subtyping could be performed. Three different stx alleles (stx 1a, stx 2a, stx 2c), which through different combinations gave rise to five stx genotypes, were identified among the remaining 38 strains (Table 1). The stx 2a genotype was the most frequent, being present in 27 of 38 (71.1%) strains. The stx 2a genotype was identified in all strains of serotypes O157:NM (SF), O55:NM, O145:H28, O172:NM, Orough:NM, and in the majority (15 of 16) of O26:H11 strains (Table 1). Only one of five NSF EHEC O157 isolates contained the stx 2a as the only stx gene. The other four NSF O157 strains harbored stx 2c in combination with either stx 1a or stx 2a gene. stx 2c did not occur in any other serotype (Table 1). stx 1a as the only stx gene was found in three of 38 strains (7.9%) including one of 16 EHEC O26:H11 and two of six O111:NM strains (Table 1).
Non-stx Virulence Genes
Strains of all but one serotype (O55:NM) contained genes encoding non-Stx toxins including cytolethal distending toxin V (Cdt-V) and/or EHEC hemolysin (Table 1). Both cdt-V and EHEC-hlyA genes were present in four of five SF O157:NM strains and in one NSF O157:H7 strain (Table 1). EHEC-hlyA, but not cdt-V, was present in all strains of serotypes O26:H11/NM, O145:H28, O172:NM, and Orough:NM, and in four NSF O157:H7/NM and four O111:NM isolates (Table 1). None of the 39 strains contained α-hlyA gene encoding α hemolysin (Table 1). All or most strains of serotypes O157:H7/NM (NSF), O26:H11/NM, O145:H28, O172:NM and Orough:NM contained the espP gene encoding the plasmid-encoded serine protease EspP [36]. Subtyping of the espP genes demonstrated that the O157:H7/NM, O26:H11/NM and O145:H28 strains contain espPα, whereas the O172:NM and Orough:NM strains contain espPγ; each of these espP alleles encodes proteolytically active EspP [36]. espP was absent from all strains of serotypes O157:NM (SF), O55:NM, and O111:NM (Table 1).
All 39 EHEC isolates contained the eae gene encoding intimin, the major adhesin of EHEC. Four different eae subtypes (ß, γ, γ2/θ, ε) were identified, which were associated with particular serotypes. The eae γ allele was broadly distributed (being present in all O157, O55, and O145 strains), whereas the other eae alleles (ß, γ2/θ, ε) were usually restricted to one serotype (Table 1). In addition to eae, genes encoding other established or putative adhesins were found in the EHEC isolates. The efa1 gene encoding the EHEC factor for adherence (Efa-1) [34] was present in strains of all serotypes (Table 1), but it was truncated in NSF O157:H7/NM and in one of O145:H28 strains as reported previously for E. coli O157:H7 [34]. In contrast, loci encoding other adhesins (lpfA O26, lpfA O157OI-141, lpfA O157OI-154, iha) were restricted to only some serotypes (Table 1).
Other Loci
All NSF O157:H7/NM, O26:H11/NM, and O145:H28 strains, and five of six O111:NM strains contained terE and ureD genes, which were used as markers for the gene clusters encoding tellurite resistance and urease production, respectively. These loci were found in none of the strains of the other serotypes (Table 1). The irp2 and fyuA genes, which are components of the iron-uptake system encoded in the high pathogenicity island (HPI) identified in EHEC by Karch et al. [46] were present only in strains of serotype O26:H11/NM (Table 1).
Presence of OI 122 in EHEC Isolates
The presence of OI 122 in EHEC strains, and the gene content of this genomic island (i.e. the presence of pagC, nleE, nleB, sen, and efa1 loci) correlate with virulence of EHEC strains [25], [43]. In accordance with their origin from patients with HUS, the EHEC strains characterized in this study contained a complete OI 122 (serotypes O157:H7/NM, O55:NM, O111:NM, and one O145:H28 strain) or an incomplete OI 122 which lacked only pagC (serotypes O26:H11, O172:NM, Orough:NM, and one O145:H28 strain) (Table 2).
Table 2. Presence of OI 122 among EHEC isolates from HUS patients.
| Locus ofOI 122 | Serotype (number of strains) | |||||||
| O157:H7/NM (NSF) | O157:NM (SF) | O55:NM | O26:H11/NM | O111:NM | O145:H28 | O172:NM | Orough:NM | |
| fliC H7 (n = 5) | fliC H7 (n = 5) | fliC H7 (n = 2) | fliC H11 (n = 16) | fliC H8 (n = 6) | fliC H28 (n = 2) | fliC H25 (n = 2) | fliC H25 (n = 1) | |
| pagC | + | + | + | – | + | + (1)a | – | – |
| nleE | + | + | + | + | + | + | + | + |
| nleB | + | + | + | + | + | + | + | + |
| sen | + | + | + | + | + | + | + | + |
| efa1 | + | + | + | + | + | + | + | + |
| OI-122b | C | C | C | I | C | C (1)I (1) | I | I |
pagC was present in one strain.
C, complete OI 122 (all genes tested present); I, incomplete OI 122 (pagC absent).
Phenotypes
All but one strain (SF O157 which lost stx gene) expressed Stx as demonstrated by cytotoxicity of their culture supernatants to Vero cells (Table 1). The Stx type produced by each strain determined using a latex agglutination assay correlated with stx genotype. Specifically, strains harboring stx 1a only produced Stx1a only, those harboring stx 2a only produced Stx2a only, and those harboring stx 1a+stx 2a produced both Stx1a and Stx2a (Table 1, Table 3). Stx2c produced by O157:H7 strains with stx genotypes stx 1a+stx 2c or stx 2a+stx 2c was detected using the Stx2 latex reagent (Table 3). EHEC hemolysin was expressed by all EHEC-hlyA-harboring strains of serotypes O157:H7/NM (NSF), O111:NM, O145:H28, and by 15 of 16 EHEC-hlyA-containing O26:H11/NM. No EHEC hemolysin production was observed in EHEC-hlyA-positive SF EHEC O157:NM strains or in strains of serotypes O172:NM and Orough:NM (Table 3). In accordance with the absence of α-hlyA gene (Table 1), none of the 39 EHEC isolates produced a hemolytic phenotype on blood agar (Table 3) Tellurite resistance was expressed in all strains of serotypes O157:H7/NM (NSF), O26:H11/NM, O111:NM, and O145:H28 which contained the terE gene, as demonstrated by their ability to grow on CT-SMAC. In contrast, none of the above strains, which also contained ureD, produced urease (Table 3). Sorbitol was utilized by all strains except for NSF O157:H7/NM, O172:NM, and Orough:NM as demonstrated by the appearance of their colonies on SMAC and using API 20E test. Rhamnose was utilized by all NSF O157:H7/NM, O111:NM, and O145:H28 strains, but not by strains of the other serotypes (Table 3). All strains except those belonging to serotypes O111:NM, O172:NM and Orough:NM produced lysine decarboxylase (Table 3). All strains but NSF O157:H7/NM produced ß-D-glucuronidase (Table 3).
Table 3. Phenotypes of EHEC strains isolated from patients with HUS in the Czech Republic.
| Phenotypea | Serotype (number of strains) | |||||||
| O157:H7/NM (NSF) | O157:NM (SF) | O55:NM | O26:H11/NM | O111:NM | O145:H28 | O172:NM | Orough:NM | |
| fliC H7 (n = 5) | fliC H7 (n = 5) | fliC H7 (n = 2) | fliC H11 (n = 16) | fliC H8 (n = 6) | fliC H28 (n = 2) | fliC H25 (n = 1) | fliC H25 (n = 2) | |
| Vero cell titerb | 32–128 | 16–512 | 32–64 | 16–128 | 64–2048 | 256–1024 | 128 | 512 |
| Stx 1c | –d | – | – | + (1)d | + (2) | – | – | – |
| Stx 2c | + (3) | + (4) | + | + (15) | – | + | + | + |
| Stx1+Stx2c | + (2) | – | – | – | + (4) | – | – | – |
| EHEC–Hly | + | – | – | + (15)e | + (4) | + | –e | –e |
| α–Hly | – | – | – | – | – | – | – | – |
| CT–SMAC growth | + | – | – | + | + (5) | + | – | – |
| Urease | – | – | – | – | – | – | – | – |
| SMAC | – | + | + | + | + | + | – | – |
| SOR | – | + | + | + | + | + | – | – |
| RHA | + | – | – | – | + | + | – | – |
| LDC | + | + | + | + | – | + | – | – |
| GLR | – | + | + | + | + | + | + | + |
EHEC-Hly, EHEC hemolysin production; α-Hly, α hemolysin production; growth on CT-SMAC, indicator of tellurite resistance; urease, urease production; SMAC, utilization of sorbitol on sorbitol MacConkey agar; SOR, utilization of sorbitol (API 20E); RHA, utilization of rhamnose (API 20E); LDC, production of lysine decarboxylase; GLR, production of ß-D-glucuronidase.
The highest dilution of culture supernatant which caused cytotoxicity in 50% Vero cells after 3 days.
Production of Stx1 and Stx2 tested using the VTEC - RPLA kit.
−, the phenotype was absent; +, the phenotype was present (the numbers in parentheses indicated numbers of positive strains in the case that not all strains expressed the respective phenotype).
one O26:H11 and O172:NM and Orough:NM strains did not express EHEC-hlyA gene.
Antimicrobial Susceptibility
Nine of 39 EHEC isolates including five of 16 O26:H11/NM strains, and four of six O111:NM strains were resistant to ampicillin. One of these O26 isolates was also resistant to trimethoprim/sulfamethoxazole. One additional isolate (O145:H28) was resistant to chloramphenicol. All the other 29 strains including all 10 O157 isolates were susceptible to all 12 antimicrobials tested (ampicillin, cefotaxime, ceftazidime, gentamicin, trimethoprim/sulfamethoxazole, ciprofloxacin, amikacin, meropenem, piperacillin/tazobactam, tigecycline, chloramphenicol, and nitrofurantoin).
Phylogeny of EHEC Associated with HUS
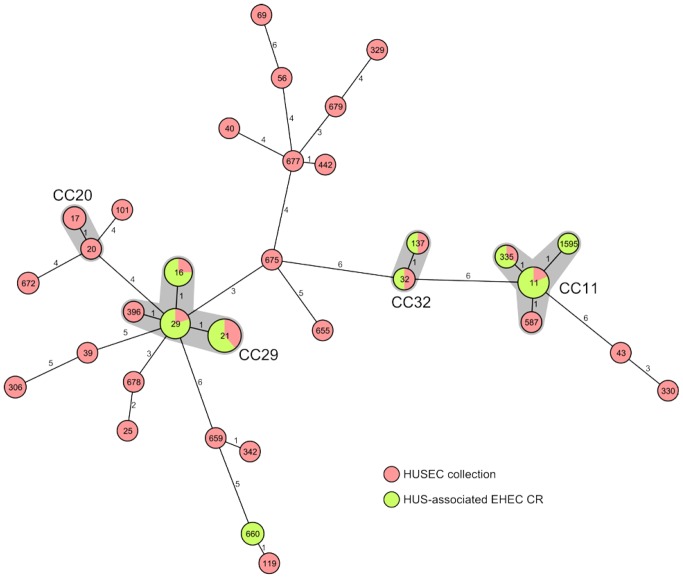
MLST analysis of the 39 EHEC isolates resulted in nine different STs. Whereas eight of the nine STs clustered into three CCs (CC11, CC29, CC32), ST660 formed a separate clone not clustering into any known CC (Table 4). All EHEC O157:H7/NM (NSF) and O157:NM (SF) belonged, with a single exception (ST1595, which is a single locus variant (slv) of ST11) to ST11 (CC11). Both O55:NM strains (ST335) grouped as a slv of ST11 into the same CC (CC11) as EHEC O157:H7/NM. EHEC O26:H11/NM were equally distributed among two different STs, ST21 and ST29, which clustered together into CC29. The ST29 is composed of strains belonging to the new, highly virulent EHEC O26 clone, which is widespread in Europe [7]. All six strains of serotype O111:NM belonged to ST16 (a slv of ST29) and grouped to CC29 together with EHEC O26 (Table 4). Both O145:H28 strains clustered into CC32 and belonged to ST32 and ST137, respectively, which are slvs. The O172:NM strain and both Orough:NM strains belonged to ST660, suggesting that they have a similar genomic background. Accordingly, a PCR analysis for the presence of the O172 biosynthetic cluster gave a positive result in all three strains demonstrating that they are all genetically O172. Phylogenetic relationships of the Czech HUS-associated strains, the distribution of strains of different serotypes into CCs and the comparison to the HUSEC collection [3] (www.ehec.org) are shown in Figure 2. Interestingly, this comparison revealed the presence of two STs that were not associated with HUS previously, namely ST660 and ST1595.
Table 4. Phylogeny of EHEC isolated from HUS patients in the Czech Republic determined by MLST.
| Serotype | Total no.of strains | ST (no. of strains) | CC |
| O157:H7/NM (NSF) | 5 | 11 (4)1595 (1) | 1111 |
| O157:NM (SF) | 5 | 11 (5) | 11 |
| O55:NM | 2 | 335 (2) | 11 |
| O26:H11/NM | 16 | 21 (8) 29a (8) | 2929 |
| O111:NM | 6 | 16 (6) | 29 |
| O145:H28 | 2 | 32 (1)137 (1) | 3232 |
| O172:NM | 1 | 660 | n.a. |
| Orough:NM | 2 | 660 (2) | n.a. |
ST, sequence type; CC, clonal complex; n.a., not assigned.
ST29 strains belong to the new EHEC O26 clone [7].
Figure 2. Phylogeny of EHEC associated with HUS in the Czech Republic.
Minimum-spanning tree illustrating the clonal relationship between HUS-associated EHEC from the Czech Republic (green) and the HUSEC collection [3] (red) based on MLST allelic profiles. Each MLST sequence type (ST) is represented by a node named with its ST. The size of the node is proportional to the number of isolates reported in this study sharing the same ST. The number on the connecting lines indicates the number of alleles that were different between the two connected nodes. In addition, for the major serogroups (e.g. O157, O26) the STs and their corresponding clonal complexes (CC) were given and shaded in grey.
Discussion
In this 15-year study we systematically investigated stools of patients with HUS for the evidence of EHEC infection. We demonstrate that approximately 70% of patients with D+ HUS contained EHEC strains in their stool samples. Similar to other European countries, EHEC associated with HUS in the Czech Republic involved strains of serogroup O157 and also several non-O157 serogroups. Notably, SF EHEC O157:NM, which were first identified in Germany [47] and later in other European countries [25], [48]–[51], accounted for 50% of all EHEC O157 strains isolated from HUS patients in the Czech Republic during 1998–2012. All SF O157:NM isolates from the Czech Republic possessed stx 2a gene, similar to such strains from Germany, but not stx 1a which was identified in SF O157:NM isolated in Norway [50]. The most prevalent EHEC serotype associated with HUS in the Czech Republic is O26:H11/NM, a situation similar to that reported from Italy [26]. Our ability to isolate EHEC strains from all stool samples that tested positive for stx genes in the initial PCR screening demonstrates that the EHEC isolation procedure used in this study enables to identify reliably both O157 and non-O157 EHEC strains. In accordance with other studies [3], [37], [49], the large percentage of the Czech EHEC isolates were non-motile. This suggests that non-motility might either be an inherent characteristic of EHEC, in particular of some serogroups, or that such strains rapidly lose their motility in vitro, after they have left the host gastrointestinal tract. This observation underlines the importance of the fliC genotyping as an easy, rapid and reliable procedure for molecular H typing of EHEC isolates.
All EHEC isolated from HUS patients in the Czech Republic were eae-positive as are also most HUS-associated EHEC in other studies [5], [8], [15], [17]. It has been shown in different studies that the rate of eae-negative strains among HUS EHEC isolates is low [3], [17], [28]. Mellmann et al. [3] reported that only 16 from 524 (3.1%) EHEC isolates from HUS patients were eae-negative. Among them was E. coli O104:H4 strain (HUSEC41) [3], which is closely related to the E. coli O104:H4 strain that caused the largest ever recorded outbreak of HUS in Germany in 2011 [52], [53], with many secondary cases having occurred worldwide including the Czech Republic [54]. The O104:H4 outbreak strain isolated in 2011 from an American tourist with diarrhea who traveled to Prague from North Germany [54] is the only eae-negative EHEC isolated in this country from humans until now. Because stx-positive/eae-negative strains would have been detected using our PCR screening system, we assume that the absence of eae-negative strains among EHEC isolated from HUS patients in the Czech Republic in this study is due to low number of isolates resulting, in turn, from a low number of HUS cases that occur in this country (4–5 per year).
SF EHEC O157:NM caused several HUS outbreaks throughout Europe, the largest of which involved Germany [55], [56], Scotland [57] and Norway [58]. Such strains differ from O157:H7 phenotypically, in particular by their ability to ferment sorbitol and produce β-D-glucuronidase, susceptibility to tellurite, lack of EHEC hemolysin expression and non-motility [41], [47], and by expression of non-Stx toxins that may contribute to the pathogenesis of EHEC-mediated diseases. Specifically, Cdt-V, which causes irreversible injury to microvascular endothelial cells [59], the major targets affected during HUS, is produced by the majority of SF EHEC O157:NM strains [35], but only by a small subset of EHEC O157:H7, which belong to particular phage types [59]. Accordingly, all SF EHEC O157:NM and one NSF O157:H7 strain analyzed in this study harbored the loci encoding Cdt-V (Table 1). EHEC hemolysin, another toxin with a potential endothelium-injuring capacity [60], was regularly expressed by EHEC O157:H7, but not by SF O157:NM strains analyzed in this study (Table 3). Several studies suggest that infections with SF EHEC O157:NM more often progress to HUS [56]–[58] than those with NSF O157 [61] and that patients infected with SF O157:NM have a higher risk of death [56]–[58] than those infected with EHEC O157:H7 [61]. In both German large outbreaks caused by SF EHEC O157:NM strains the case-fatality ratio was 11% [55], [56] compared to <1% reported for outbreaks caused by NSF EHEC O157:H7 [61]. In agreement with the high virulence of SF EHEC O157:NM strains, this strain was the cause of death in one patient in our study. The other two fatal cases were associated with infection by EHEC O26:H11, one of which belonged to the new highly virulent clone, which has emerged in Europe [7] and accounted for 50% of all O26 EHEC O26 isolated in this study.
EHEC O157:H7 have evolved from an E. coli O55:H7 ancestor possessing the locus of enterocyte effacement (LEE) by acquisition of Stx-encoding bacteriophages, virulence plasmid and transition of somatic antigen from O55 to O157 [62]–[64]. Leopold et al. [63] and others [65], [66] provided evidence of limited diversity in SF O157:NM, much unlike the large biodiversity of EHEC O157:H7. We show that the NSF and SF O157 isolates described here all belong to the same clonal complex (CC11); multilocus variable number tandem repeat analysis (MLVA) and single nucleotide polymorphism (SNP) analysis of the Czech strains is underway to more extensively compare the phylogenetic relationships of these strains and to compare them with strains from other countries [63], [67], [68].
Tellurite resistance is a diagnostically important feature enabling isolation of EHEC strains from CT-SMAC where normal intestinal flora are suppressed. In our study tellurite resistance occurred in all NSF EHEC O157, all O26 and both O145 isolates and in five of six O111 strains. All these strains also contained the ure cluster encoding urease production but none of them produced urease, in accordance with observations that ure genes are usually not expressed in EHEC strains [42]. The absence of both ter and ure loci in one O111:NM strain (Table 1) suggest that the strain have lost these loci, as have been previously reported for EHEC O157:H7 and attributed to deletions within OIs 43 and 48 that harbor these loci [69].
Antimicrobial susceptibility testing demonstrated resistance to one (9 isolates) or two (1 isolate) antimicrobials in 25.6% of the Czech EHEC strains studied. The resistance was associated with non-O157 EHEC serogroups. This situation is similar to that in Finland and Belgium where antimicrobial resistance was reported in 21.4% and 44.7% of EHEC patientś isolates, respectively, and it was more frequent in non-O157 than in O157 strains [70], [71]. As in our study, none of the isolates from these countries was resistant to meropenem or imipenem, ciprofloxacin and amikacin. In contrast to our findings, multidrug resistance occurred in 24.1% of the Belgian [71] and in 7.1% of the Finnish EHEC isolates [70], as well as in an EHEC O145:H- strain that caused a multistate outbreak of diarrhea and HUS in the United States [72]. The extended-spectrum β-lactamase (ESBL) phenotype, which was identified in an EHEC O26 human isolate in another Belgian study [73], and which is one of the typical features of the EHEC O104:H4 strain that caused the large 2011 outbreak in Germany [53], [74] was not tested in the Czech EHEC HUS isolates in this study. Compared to EHEC, E. coli strains isolated from urine of patients with urinary tract infections or from blood cultures of patients with sepsis are more often multiresistant [75] or express the ESBL phenotype [76], [77].
The spectrum of EHEC serotypes associated with HUS in the Czech Republic raises the question about reservoirs of these pathogens and sources of human infections in this country. Prevalence of EHEC in cattle feces in the Czech Republic was investigated by Alexa et al. [78]. EHEC shedding was observed in 70% to 100% animals in three different diary farms. EHEC isolates belonged to serogroups O26, O103, O157, O128, and O54, the former three being isolated from HUS patients in our study. Čížek et al. [79] studied the occurence of EHEC O157 in diary farms in the Czech Republic. EHEC O157 strains harboring stx 1, stx 2, eae, and EHEC-hlyA genes were detected in four of 192 in-line filters examined. Several additional studies identified various animal species as sources of outbreaks or sporadic cases of EHEC infections in this country. In 1995, four cases of HUS in children caused by EHEC O157:H7 were associated with consumption of unpasteurised milk from a farm goat who shed the causative EHEC O157:H7 strain in its feces [80]. Three years later, SF EHEC O157:NM strains were isolated from two siblings (one with HUS and the other with diarrhea) and an epidemiologically associated cow, and a direct contact with the animal was implicated as a possible infection transmission route [81]. This was the first evidence that cattle can be a reservoir of SF EHEC O157 and a source of human diseases [81]. Altogether, these studies demonstrate that similar to other countries [27], [40], [61], cattle and other domestic animals are reservoires of EHEC in the Czech Republic and can be sources of the infection for humans.
We conclude from our data that EHEC strains including O157:H7/NM and a spectrum of non-O157 serotypes are important causes of pediatric D+ HUS in the Czech Republic. Although the spectrum of EHEC serotypes resembles that found in other European countries, the finding of serotypes O172:NM[fliC H25] and Orough:NM[fliC H25], which are not members of the German HUSEC collection [3] (www.ehec.org) indicates the need for creating an European collection of HUS-associated EHEC. This collection would enable complex studies of virulence characteristics, mechanisms of adaptation to the human host and evolution of these pathogens, as well as development of optimized methods for their detection.
Acknowledgments
We thank Dr. Blanka Horová (Department of Microbiology, Hospital Na Bulovce, Prague), Dr. Eliška Bébrová (Institute of Medical Microbiology, University Hospital Motol, Prague) Mgr. Tereza Škapová (Public Health Institute, Ostrava), Mgr. Eva Krejčí (Public Health Institute, Ostrava), PhD, Dr. Lenka Ryšková (Department of Microbiology, University Hospital, Hradec Kralove), Dr. Miroslava Brndiarová (University Hospital, Martin), Dr. Jana Salášková (University Hospital, Hradec Kralove), Dr. Jan Saitz (University Hospital Olomouc) and Dr. Alena Ševčíková (University Hospital Brno) for their kind support during the study. Excellent technical assistance of Miluše Vašáková, Hana Pihávková and Jakub Mach (National Institute of Public Health, Prague) is greatly appreciated.
Funding Statement
The authors have no support or funding to report.
References
- 1. Tarr PI, Gordon CA, Chandler WL (2005) Shiga toxin-producing Escherichia coli and the haemolytic uraemic syndrome. Lancet 365: 1073–1086. [DOI] [PubMed] [Google Scholar]
- 2. Schmidt H, Geitz C, Tarr PI, Frosch M, Karch H (1999) Non-O157:H7 pathogenic Shiga toxin-producing Escherichia coli: phenotypic and genetic profiling of virulence traits and evidence for clonality. J Infect Dis 179: 115–123. [DOI] [PubMed] [Google Scholar]
- 3. Mellmann A, Bielaszewska M, Köck R, Friedrich AW, Fruth A, et al. (2008) Analysis of collection of hemolytic uremic syndrome-associated enterohemorrhagic Escherichia coli . Emerg Infect Dis 14: 1287–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Espié E, Grimont F, Mariani-Kurkdjian P, Bouvet P, Haeghebaert S, et al. (2008) Surveillance of hemolytic uremic syndrome in children less than 15 years of age, a system to monitor O157 and non-O157 Shiga toxin-producing Escherichia coli infections in France, 1996–2006. Pediatr Infect Dis J 27: 595–601. [DOI] [PubMed] [Google Scholar]
- 5. Käppeli U, Hächler H, Giezendanner N, Beutin L, Stephan R (2011) Human infections with non-O157 Shiga toxin-producing Escherichia coli, Switzerland, 2000–2009. Emerg Infect Dis 17: 180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zieg J, Dusek J, Marejkova M, Limrova P, Blazek D, et al. (2012) Fatal case of diarrhea-associated hemolytic uremic syndrome with severe neurologic involvement. Pediatr Int 54: 166–167. [DOI] [PubMed] [Google Scholar]
- 7. Bielaszewska M, Mellmann A, Bletz S, Zhang W, Köck R, et al. (2013) Enterohemorrhagic Escherichia coli O26:H11/H-: A new virulent clone emerges in Europe. Clin Infect Dis 56: 1373–1381. [DOI] [PubMed] [Google Scholar]
- 8. Brooks JT, Sowers EG, Wells JG, Greene KD, Griffin PM, et al. (2005) Non-O157 Shiga toxin-producing Escherichia coli infections in the United States, 1983–2002. J Infect Dis 192: 1422–1429. [DOI] [PubMed] [Google Scholar]
- 9. Schimmer B, Nygard K, Eriksen HM, Lassen J, Lindstedt BA, et al. (2008) Outbreak of haemolytic uraemic syndrome in Norway caused by stx2-positive Escherichia coli O103:H25 traced to cured mutton sausages. BMC Infect Dis 8: 41 doi: 10.1186/1471-2334-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bláhová K, Janda J, Kreisinger J, Matejková E, Sedivá A (2002) Long-term follow-up of Czech children with D+ hemolytic-uremic syndrome. Pediatr Nephrol 17: 400–403. [DOI] [PubMed] [Google Scholar]
- 11. Rosales A, Hofer J, Zimmerhackl LB, Jungraithmayr TC, Riedl M, et al. (2012) Need for long-term follow-up in enterohemorrhagic Escherichia coli-associated hemolytic uremic syndrome due to late-emerging sequelae. Clin Infect Dis 54: 1413–1421. [DOI] [PubMed] [Google Scholar]
- 12. Zoja C, Buelli S, Morigi M (2010) Shiga toxin-associated hemolytic uremic syndrome: pathophysiology of endothelial dysfunction. Pediatr Nephrol 25: 2231–2240. [DOI] [PubMed] [Google Scholar]
- 13. Betz J, Bielaszewska M, Thies A, Humpf HU, Dreisewerd K, et al. (2011) Shiga toxin glycosphingolipid receptors in microvascular and macrovascular endothelial cells: differential association with membrane lipid raft microdomains. J Lipid Res 52: 618–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Betz J, Bauwens A, Kunsmann L, Bielaszewska M, Mormann M, et al. (2012) Uncommon membrane distribution of Shiga toxin glycosphingolipid receptors in toxin-sensitive human glomerular microvascular endothelial cells. Biol Chem 393: 133–147. [DOI] [PubMed] [Google Scholar]
- 15. Friedrich AW, Bielaszewska M, Zhang W, Pulz M, Kuczius T, et al. (2002) Escherichia coli harboring Shiga toxin 2 gene variants: frequency and association with clinical symptoms. J Infect Dis 185: 74–84. [DOI] [PubMed] [Google Scholar]
- 16. Scheutz F, Teel LD, Beutin L, Piérard D, Buvens G, et al. (2012) Multicenter evaluation of a sequence-based protocol for subtyping Shiga toxins and standardizing Stx nomenclature. J Clin Microbiol 50: 2951–2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ethelberg S, Olsen KE, Scheutz F, Jensen C, Schiellerup P, et al. (2004) Virulence factors for hemolytic uremic syndrome, Denmark. Emerg Infect Dis 10: 842–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Prager R, Fruth A, Siewert U, Strutz U, Tschäpe H (2009) Escherichia coli encoding Shiga toxin 2f as an emerging human pathogen. Int J Med Microbiol 299: 343–353. [DOI] [PubMed] [Google Scholar]
- 19. Prager R, Fruth A, Busch U, Tietze E (2011) Comparative analysis of virulence genes, genetic diversity, and phylogeny of Shiga toxin 2g and heat-stable enterotoxin STIa encoding Escherichia coli isolates from humans, animals, and environmental sources. Int J Med Microbiol 301: 181–191. [DOI] [PubMed] [Google Scholar]
- 20. Rivas M, Miliwebsky E, Chinen I, Roldán CD, Balbi L, et al. (2006) Characterization and epidemiologic subtyping of Shiga toxin-producing Escherichia coli strains isolated from hemolytic uremic syndrome and diarrhea cases in Argentina. Foodborne Pathog Dis 3: 88–96. [DOI] [PubMed] [Google Scholar]
- 21. Louise CB, Obrig TG (1995) Specific interaction of Escherichia coli O157:H7- derived Shiga-like toxin II with human renal endothelial cells. J Infec Dis 172: 1397–1401. [DOI] [PubMed] [Google Scholar]
- 22. Bauwens A, Bielaszewska M, Kemper B, Langehanenberg P, von Bally G, et al. (2011) Differential cytotoxic actions of Shiga toxin 1 and Shiga toxin 2 on microvascular and macrovascular endothelial cells. Thromb Haemost 105: 515–528. [DOI] [PubMed] [Google Scholar]
- 23. Banatvala N, Griffin PM, Greene KD, Barrett TJ, Bibb WF, et al. (2001) The United States national prospective hemolytic uremic syndrome study: microbiologic, serologic, clinical, and epidemiologic findings. J Infect Dis 183: 1063–1070. [DOI] [PubMed] [Google Scholar]
- 24. Lynn RM, O’Brien SJ, Taylor CM, Adak GK, Chart H, et al. (2005) Childhood hemolytic uremic syndrome, United Kingdom and Ireland. Emerg Infect Dis 11: 590–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Buvens G, Piérard D (2012) Virulence profiling and disease association of verocytotoxin-producing Escherichia coli O157 and non-O157 isolates in Belgium. Foodborne Pathog Dis 9: 530–535. [DOI] [PubMed] [Google Scholar]
- 26. Tozzi E, Caprioli A, Minelli F, Gianviti A, De Petris L, et al. (2003) Shiga toxin–producing Escherichia coli infections associated with hemolytic uremic syndrome, Italy, 1988–2000. Emerg Infect Dis 9: 106–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chase-Topping ME, Rosser T, Allison LJ, Courcier E, Evans J, et al. (2012) Pathogenic potential to humans of bovine Escherichia coli O26, Scotland. Emerg Infect Dis 18: 439–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Elliott EJ, Robins-Browne RM, O’Loughlin EV, Bennett-Wood V, Bourke J, et al. (2001) Nationwide study of haemolytic uraemic syndrome: clinical, microbiological, and epidemiological features. Arch Dis Child 85: 125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Paton AW, Paton JC (1998) Detection and characterization of Shiga toxigenic Escherichia coli by using multiplex PCR assays for stx 1, stx 2, eaeA, enterohemorrragic E. coli hlyA, rfb O111, and rfb O157 . J Clin Microbiol 36: 598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Perelle S, Dilasser F, Grout J, Fach P (2004) Detection by 5′-nuclease PCR of Shiga-toxin producing Escherichia coli O26, O55, O91, O103, O111, O113, O145 and O157:H7, associated with the world´s most frequent clinical cases. Mol Cell Probes 18: 185–192. [DOI] [PubMed] [Google Scholar]
- 31. D´Souza JM, Wang L, Reeves P (2002) Sequence of the Escherichia coli O26 O antigen gene cluster and identification of O26 specific genes. Gene 297: 123–127. [DOI] [PubMed] [Google Scholar]
- 32. Guo H, Feng L, Tao J, Zhang C, Wang L (2004) Identification of Escherichia coli O172 O-antigen gene cluster and development of a serogroup-specific PCR assay. J Appl Microbiol 97: 181–190. [DOI] [PubMed] [Google Scholar]
- 33. Schmidt H, Beutin L, Karch H (1995) Molecular analysis of the plasmid-encoded hemolysin of Escherichia coli O157:H7 strain EDL 933. Infect Immun 63: 1055–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Janka A, Bielaszewska M, Dobrindt U, Karch H (2002) Identification and distribution of the enterohemorrhagic Escherichia coli factor for adherence (efa1) gene in sorbitol-fermenting Escherichia coli O157: H-. Int J Med Microbiol 292: 207–214. [DOI] [PubMed] [Google Scholar]
- 35. Janka A, Bielaszewska M, Dobrindt U, Greune L, Schmidt MA, et al. (2003) Cytolethal distending toxin gene cluster in enterohemorrhagic Escherichia coli O157:H- and O157: H7: characterization and evolutionary considerations. Infect Immun 71: 3634–3638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Brockmeyer J, Bielaszewska M, Fruth A, Bonn ML, Mellmann A, et al. (2007) Subtypes of the plasmid-encoded serine protease EspP in Shiga toxin-producing Escherichia coli: distribution, secretion, and proteolytic activity. Appl Environ Microbiol 73: 6351–6359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bielaszewska M, Köck R, Friedrich AW, von Eiff C, Zimmerhackl LB, et al. (2007) Shiga toxin-mediated hemolytic uremic syndrome: time to change the diagnostic paradigm? PLoS One 2: e1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Toma C, Martínez Espinosa E, Song T, Miliwebsky E, Chinen I, et al. (2004) Distribution of putative adhesins in different seropathotypes of Shiga toxin-producing Escherichia coli . J Clin Microbiol 42: 4937–4946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhang WL, Köhler B, Oswald E, Beutin L, Karch H, et al. (2002) Genetic diversity of intimin genes of attaching and effacing Escherichia coli strains. J Clin Microbiol 40: 4486–4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Blanco M, Blanco JE, Mora A (2004) Serotypes, virulence genes, and intimin types of Shiga toxin (Verotoxin)-producing Escherichia coli isolates from cattle in Spain and identification of a new intimin variant gene (eae-ξ). J Clin Microbiol 42: 645–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bielaszewska M, Tarr PI, Karch H, Zhang W, Mathys W (2005) Phenotypic and molecular analysis of tellurite resistance among enterohemorrhagic Escherichia coli O157:H7 and sorbitol-fermenting O157:NM clinical isolates. J Clin Microbiol 43: 452–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Friedrich AW, Köck R, Bielaszewska M, Zhang W, Karch H, et al. (2005) Distribution of the urease gene cluster and urease activity among enterohemorrhagic Escherichia coli O157 from humans. J Clin Microbiol 43: 546–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Karmali MA, Mascarenhas M, Shen S, Ziebell K, Johnson S, et al. (2003) Association of genomic O island 122 of Escherichia coli EDL 933 with verocytotoxin-producing Escherichia coli seropathotypes that are linked to epidemic and/or serious disease. J Clin Microbiol 41: 4930–4940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.EUCAST. EUCAST MIC and Zone diameter breakpoint tables. (2012) Available: http://www.eucast.org/antimicrobial_susceptibility_testing/breakpoints/.Accessed 22 October 2012.
- 45.EUCAST. Antimicrobial susceptibility testing EUCAST disk diffusion method. (2012) Available: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Disk_test_documents/Manual_v_2.1_EUCAST_Disk_Test.pdf.Accessed 22 October 2012.
- 46. Karch H, Schubert S, Zhang D, Zhang W, Schmidt H, et al. (1999) A genomic island, termed high-pathogenicity island, is present in certain non-O157 Shiga toxin-producing Escherichia coli clonal lineages. Infect Immun 67: 5994–6001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Karch H, Wiss R, Gloning H, Emmrich P, Aleksić S, et al. (1990) Hemolytic-uremic syndrome in infants due to verotoxin-producing Escherichia coli . Dtsch Med Wochenschr 115: 489–495. [DOI] [PubMed] [Google Scholar]
- 48. Orth D, Grif K, Zimmerhackl LB, Würzner R (2009) Sorbitol-fermenting Shiga toxin-producing Escherichia coli O157 in Austria. Wien Klin Wochenschr 121: 108–112. [DOI] [PubMed] [Google Scholar]
- 49. Eklund M, Bielaszewska M, Nakari UM, Karch H, Siitonen A (2006) Molecular and phenotypic profiling of sorbitol-fermenting Escherichia coli O157:H- human isolates from Finland. Clin Microbiol Infect 12: 634–641. [DOI] [PubMed] [Google Scholar]
- 50. Brandal LT, Løbersli I, Stavnes TL, Wester AL, Lindstedt BA (2012) First report of the Shiga toxin 1 gene in sorbitol-fermenting Escherichia coli O157:H-. J Clin Microbiol 50: 1825–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pollock KG, Locking ME, Beattie TJ, Maxwell H, Ramage I, et al. (2010) Sorbitol-fermenting Escherichia coli O157, Scotland. Emerg Infect Dis 16: 881–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Frank C, Werber D, Cramer JP, Askar M, Faber M, et al. (2011) Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany - Preliminary report. N Engl J Med 19: 1771–1780. [DOI] [PubMed] [Google Scholar]
- 53. Bielaszewska M, Mellmann A, Zhang W, Köck R, Fruth A, et al. (2011) Characterisation of the Escherichia coli strain associated with an outbreak of haemolytic uraemic syndrome in Germany, 2011: a microbiological study. Lancet Infect Dis 11: 671–676. [DOI] [PubMed] [Google Scholar]
- 54. Marejková M, Roháčová H, Reisingerová M, Petráš P (2012) An imported case of bloody diarrhea in the Czech Republic caused by a hybrid enteroaggregative hemorrhagic Escherichia coli (EAHEC) O104:H4 strain associated with the large outbreak in Germany, May 2011. Folia Microbiol 57: 85–89. [DOI] [PubMed] [Google Scholar]
- 55. Ammon A, Peterson LR, Karch H (1999) A large outbreak of hemolytic uremic syndrome caused by an unusual sorbitol-fermenting strain of E. coli O157:H–. J Infect. Dis 179: 1274–1277. [DOI] [PubMed] [Google Scholar]
- 56. Alpers K, Werber D, Frank C, Koch J, Friedrich AW, et al. (2009) Sorbitol-fermenting enterohaemorrhagic Escherichia coli O157:H- causes another outbreak of haemolytic uraemic syndrome in children. Epidemiol Infect 137: 389–395. [DOI] [PubMed] [Google Scholar]
- 57. Rosser T, Dransfield T, Allison L, Hanson M, Holden N, et al. (2008) Pathogenic potential of emergent sorbitol-fermenting Escherichia coli O157:NM. Infect Immun 76: 5598–5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Haugum K, Lindstedt BA, Løbersli I, Kapperud G, Brandal LT (2012) Identification of the anti-terminator qO111:H- gene in Norwegian sorbitol-fermenting Escherichia coli O157:NM. FEMS Microbiol Lett 329: 102–110. [DOI] [PubMed] [Google Scholar]
- 59. Friedrich AW, Lu S, Bielaszewska M, Prager R, Bruns P, et al. (2006) Cytolethal distending toxin in Escherichia coli O157:H7: spectrum of conservation, structure, and endothelial toxicity. J Clin Microbiol 44: 1844–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Aldick T, Bielaszewska M, Zhang W, Brockmeyer J, Schmidt H, et al. (2007) Hemolysin from Shiga toxin-negative Escherichia coli O26 strains injures microvascular endothelium. Microbes Infect 9: 282–290. [DOI] [PubMed] [Google Scholar]
- 61. Rangel JM, Sparling PH, Crowe C, Griffin PM, Swerdlow DL (2005) Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982–2002. Emerg Infect Dis 11: 603–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Feng P, Lampel KA, Karch H, Whittam TS (1998) Genotypic and phenotypic changes in the emergence of Escherichia coli O157:H7. J Infect Dis 177: 1750–1753. [DOI] [PubMed] [Google Scholar]
- 63. Leopold SR, Magrini V, Holt NJ, Shaikh N, Mardis ER, et al. (2009) A precise reconstruction of the emergence and constrained radiations of Escherichia coli O157 portrayed by backbone concatenomic analysis. Proc Natl Acad Sci U S A 106: 8713–8718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bono JL, Smith TP, Keen JE, Harhay GP, McDaneld TG, et al. (2012) Phylogeny of Shiga toxin-producing Escherichia coli O157 isolated from cattle and clinically ill humans. Mol Biol Evol 29: 2047–2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Jenke C, Harmsen D, Weniger T, Rothganger J, Hyytia-Trees E, et al. (2010) Phylogenetic analysis of enterohemorrhagic Escherichia coli O157, Germany, 1987–2008. Emerg Infect Dis 16: 610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Jenke C, Leopold SR, Weniger T, Rothgänger J, Harmsen D, et al. (2012) Identification of intermediate in evolutionary model of enterohemorrhagic Escherichia coli O157. Emerg Infect Dis 18: 582–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Izumiya H, Pei Y, Terajima J, Ohnishi M, Hayashi T, et al. (2010) New system for multilocus variable-number tandem-repeat analysis of the enterohemorrhagic Escherichia coli strains belonging to three major serogroups: O157, O26, and O111. Microbiol Immuno 54: 569–577. [DOI] [PubMed] [Google Scholar]
- 68. Jenke C, Lindstedt BA, Harmsen D, Karch H, Brandal LT, et al. (2011) Comparison of multilocus variable-number tandem-repeat analysis and multilocus sequence typing for differentiation of hemolytic-uremic syndrome-associated Escherichia coli (HUSEC) collection strains. J Clin Microbiol 49: 3644–3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bielaszewska M, Middendorf B, Tarr PI, Zhang W, Prager R, et al. (2011) Chromosomal instability in enterohaemorrhagic Escherichia coli O157:H7: impact on adherence, tellurite resistance and colony phenotype. Mol Microbiol 79: 1024–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Eklund M, Scheutz F, Siitonen A (2001) Clinical isolates of non-O157 Shiga toxin-producing Escherichia coli: serotypes, virulence characteristics, and molecular profiles of strains of the same serotype. J Clin Microbiol 39: 2829–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Buvens G, Gheldre Y, Dediste A, Moreau AI, Mascart G, et al. (2011) Incidence and virulence determinants of verocytotoxin-producing Escherichia coli infections in the Brussels-capital region, Belgium, in 2008–2010. J Clin Microbiol 50: 1336–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Folster JP, Pecic G, Taylor E, Whichard J (2011) Characterization of isolates from an outbreak of multidrug-resistant, Shiga toxin-producing Escherichia coli O145 in the United States. Antimicrob Agents Chemother 55: 5955–5956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Buvens G, Bogaerts P, Glupczynski Y, Lauwers S, Piérard D (2010) Antimicrobial resistance testing of verocytotoxin-producing Escherichia coli and first description of TEM-52 extended-spectrum β-lactamase in serogroup O26. Antimicrob Agents Chemother 54: 4907–4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Bielaszewska M, Idelevich EA, Zhang W, Bauwens A, Schaumburg F, et al. (2012) Effects of antibiotics on Shiga toxin 2 production and bacteriophage induction by epidemic Escherichia coli O104:H4 strain. Antimicrob Agents Chemother 56: 3277–3282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. van der Donk CF, van de Bovenkamp JH, De Brauwer EI, De Mol P, Feldhoff KH, et al. (2012) Antimicrobial resistance and spread of multi drug resistant Escherichia coli isolates collected from nine urology services in the Euregion Meuse-Rhine. PLoS One 7(10): e47707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hrabák J, Empel J, Bergerová T, Fajfrlík K, Urbášková P, et al. (2009) International clones of Klebsiella pneumoniae and Escherichia coli with extended-spectrum β-lactamases in a Czech hospital. J Clin Microbiol 47: 3353–3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tumbarello M, Sanguinetti M, Montuori E, Trecarichi EM, Posteraro B, et al. (2007) Predictors of mortality in patients with bloodstream infections caused by extended-spectrum-beta-lactamase-producing Enterobacteriaceae: importance of inadequate initial antimicrobial treatment. Antimicrob Agents Chemother 51: 1987–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Alexa P, Konstantinova L, Zajacova-Sramkova Z (2011) Faecal shedding of verotoxigenic Escherichia coli in cattle in the Czech Republic. Veterinarni Medicina 56: 149–155. [Google Scholar]
- 79. Čížek A, Dolejská M, Novotná R, Haas D, Vyskočil M (2007) Survey of Shiga toxigenic Escherichia coli O157 and drug-resistant coliform bacteria from in-line milk filters on dairy farms in the Czech Republic. J Appl Microbiol 104: 852–860. [DOI] [PubMed] [Google Scholar]
- 80. Bielaszewska M, Janda J, Bláhová K, Minaříková H, Jílková E, et al. (1997) Human Escherichia coli O157:H7 infection associated with consumption of unpasteurised goat´s milk. Epidemiol Infect 119: 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bielaszewska M, Schmidt H, Liesegang A, Prager R, Rabsch W, et al. (2000) Cattle can be a reservoir of sorbitol-fermenting Shiga toxin-producing Escherichia coli O157:H- strains and a source of human diseases. J Clin Microbiol 38: 3470–3473. [DOI] [PMC free article] [PubMed] [Google Scholar]