Abstract
Aim
Response to stress can vary greatly between individuals. However, it remains unknown whether perceived impact of stress on health is associated with adverse health outcomes. We examined whether individuals who report that stress adversely affects their health are at increased risk of coronary heart disease (CHD) compared with those who report that stress has no adverse health impact.
Methods and results
Analyses are based on 7268 men and women (mean age: 49.5 years, interquartile range: 11 years) from the British Whitehall II cohort study. Over 18 years of follow-up, there were 352 coronary deaths or first non-fatal myocardial infarction (MI) events. After adjustment for sociodemographic characteristics, participants who reported at baseline that stress has affected their health ‘a lot or extremely’ had a 2.12 times higher (95% CI 1.52–2.98) risk of coronary death or incident non-fatal MI when compared with those who reported no effect of stress on their health. This association was attenuated but remained statistically significant after adjustment for biological, behavioural, and other psychological risk factors including perceived stress levels, and measures of social support; fully adjusted hazard ratio: 1.49 (95% CI 1.01–2.22).
Conclusions
In this prospective cohort study, the perception that stress affects health, different from perceived stress levels, was associated with an increased risk of coronary heart disease. Randomized controlled trials are needed to determine whether disease risk can be reduced by increasing clinical attention to those who complain that stress greatly affects their health.
Keywords: Epidemiology, Stress, Coronary heart disease, Prospective studies
See page 2658 for the editorial comment on this article (doi:10.1093/eurheartj/eht289)
Introduction
Research on stress has a long history1,2 with considerable evidence showing exposure to stress to be associated with adverse health outcomes including cardiovascular disease (CVD), diabetes, obesity, hypertension, major depression, and mortality, although these are not universal findings.3–10 Stress is experienced when a person feels that ‘environmental demands tax or exceed his or her adaptive capacity, resulting in psychological and biological changes that may place him or her at risk for disease’.11 Hence, the effects of a stressful situation may differ greatly between individuals, depending on the intrinsic and extrinsic resources available to them.
Despite recognized individual differences in responses to stressful situations (major life events, work demands, daily hassles, etc.), research in this domain has mostly focused on quantifying them and then examining their effects on mental and physical health.7,12–14 The consequence is that individual differences in response to stressful situations are not taken into account. A potential way of capturing these differences is to assess an individual's perception of stress impact on their health (different from perceived stress levels) and to assess whether this predicts clinically relevant health outcomes. However, to our knowledge, such studies are rare.15
The aim of this study was therefore to examine whether individuals' perception of the impact of stress on their health is associated with the risk of incident coronary heart disease (CHD) in a large prospective cohort study over an 18-year period. As a working hypothesis, we expect that individuals who report stress to affect their health would be at increased risk of incident CHD. We also hypothesize that this association is independent of perceived stress levels.
Materials and methods
Study sample and design
Data are drawn from the Whitehall II study,16 established in 1985 as a longitudinal study to examine the socioeconomic gradient in health and disease among 6895 men and 3413 women. All civil servants aged 35–55 years in 20 London-based departments were invited to participate; 73% agreed. The first screening (Phase 1) took place during 1985–88, and involved a clinical examination and a self-administered questionnaire. Subsequent phases of data collection have alternated between a postal questionnaire alone [Phases 2 (1989–90), 4 (1995–96), 6 (2001), and 8 (2006)] and a postal questionnaire accompanied by a clinical examination [Phases 3 (1991–93), 5 (1997–99), 7 (2002–04), and 9 (2007–09)]. All participants gave consent to participate and the University College London ethics committee approved this study.
The question on the perceived impact of stress on health was introduced to the Whitehall II study for the first time at Phase 3. Thus, this phase constitutes the ‘baseline’ in the present analyses. Surveillance for incident CHD events occurred from Phase 3 to Phase 9 for a maximum follow-up of 18.3 years.
Measures
Perceived impact of stress on health
To assess the perceived impact of stress on health, participants were asked the following question: ‘To what extent do you feel that the stress or pressure you have experienced in your life has affected your health?’ Response choices were: (i) ‘not at all’, (ii) ‘slightly’, (iii) ‘moderately’, (iv) ‘a lot’, or (v) ‘extremely’. To include categories in the analysis with sufficient numbers of persons, this variable was recoded into three categories as follows: 1 = ‘not at all’, 2 = ‘slightly or moderately’, and 3 = ‘a lot or extremely’.
Ascertainment of coronary heart disease events
CHD events were composed of fatal CHD and non-fatal CHD defined as first non-fatal myocardial infarction (MI). For fatal CHD, participants were flagged by the British National Health Service (NHS) Central Registry, who notified the date and cause of all deaths, classified as coronary if ICD-9 (International Classification of Diseases, 9th edn) codes 410–414 or ICD-10 (International Classification of Diseases, 10th edn) codes I20–I25 were present on the death certificate. Non-fatal MI was defined following MONICA criteria17 based on study electrocardiograms, hospital acute ECGs, and cardiac enzymes. From 1989 onwards, the NHS Hospital Episode Statistics (HES) database has provided reports of participants' diagnoses on discharge and procedure codes for all NHS hospitals in England.
Covariates
Socio-demographic measures included age, sex, ethnicity, marital status, and socioeconomic position (SEP) assessed using the British civil service grade of employment at Phase 3.16
CVD risk factors were assessed using responses to the Phase 3 questionnaire and categorized as follows: smoking status (never, ex, and current); physical activity at recommended levels18 (≥2.5 h more of at least moderately energetic physical activity per week, coded as yes or no); high alcohol consumption in the previous week was defined as a consumption of more than 14 units for women and more than 21 units for men, with 1 unit corresponding to 8–10 g of alcohol; and daily fruit and vegetable intake (yes/no). The following biological CVD risk factors were measured at the Phase 3 clinical examination and were included in the analyses as continuous variables: systolic and diastolic blood pressures, total cholesterol, triglycerides, and body mass index (BMI). Diabetes was assessed via self-report of doctor diagnosis.
We also included additional covariates such as self-rated health (good or poor),19 perceived levels of stress (‘none’, ‘a little or a fair amount’, and ‘quite a lot or a great deal’),4 negative affect score (low, middle, and high),20 psychological distress score as measured by the general health questionnaire21 and measures of social support (social support at work, number of relatives, and number of friends seen monthly).
Statistical analyses
The associations of perceived impact of stress on health with baseline categorical variables were examined using a Chi-square test for heterogeneity. For continuous variables, heterogeneity was assessed using one-way analysis of variance.
We used Cox regression to examine the association between perceived impact of stress and incident CHD events. There was no evidence that this association was modified by sex (P = 0.67), and so data were pooled and sex-adjusted. The assumption of proportional hazards was checked by examining the interaction term between the perceived impact of stress on health and the logarithm of the follow-up period. It was non-significant (P = 0.11), confirming that the proportional hazards assumption was not violated.
Six serially adjusted models included the following covariates: sociodemographic factors (sex, age, ethnicity, marital status, and employment grade, Model 1); potential confounding factors or mediators including behavioural risk factors (Model 2); biological risk factors (Model 3); self-rated health; negative affect; psychological distress scores and measures of social support (Model 4); and perceived levels of stress (Model 5). In the final model, we adjusted for all of the covariates outlined above (Model 6). Survival curves according to the perceived impact of stress on health score categories were estimated using unadjusted and adjusted22 Kaplan–Meier survivor functions. Analyses were performed using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) and Stata 12 (StataCorp. College Station, TX, USA)’.
Results
A total of 8306 participants responded to the question on the perceived impact of stress on their health. Of those, 7268 had data on all 21 baseline covariates and were included in our analytical sample. The 1038 participants not included in the analyses owing to missing data on covariates were more likely than the included participants to be women (P = 0.004), non-white (P = 0.001), not married/cohabiting (P = 0.005), and older (P = 0.002). Overall, 39% of participants reported that stress has affected their health ‘not at all’, 53% ‘slightly or moderately’, and 8% ‘a lot or extremely “. The total number of coronary death or non-fatal incident MI cases over the follow-up was 352.
Table 1 displays the distribution of baseline covariates as a function of perceived impact of stress on health. Participants who reported that stress has affected their health “a lot or extremely” were more likely to be female, not married/cohabiting, from the lower occupational grade, non-white, current smokers, less likely to consume fruit and vegetables daily and to practice physical activity at recommended levels, more likely to have diabetes, high psychological distress and a high negative affect score, and to report poor self-rated health, low social support at work, and high perceived stress levels (all P ≤ 0.01).
Table 1.
Baseline characteristics of the sample and perceived impact of stress on health
| All N (%) | Perceived impact of stress on health n (%)/mean (SD) |
||||
|---|---|---|---|---|---|
| Variables | Not at all (n = 2835) | Slightly or moderately (n = 3849) | A lot or extremely (n = 584) | P value | |
| Age, years | 7268 (100) | 49.7 (6.1) | 49.3 (6.0) | 49.5 (6.0) | 0.10 |
| Sex | <0.001 | ||||
| Male | 5055 (69.6) | 2148 (75.8) | 2583 (67.1) | 324 (55.5) | |
| Female | 2213 (30.4) | 687 (24.2) | 1266 (32.9) | 260 (44.5) | |
| Marital status | <0.001 | ||||
| Married/cohabiting | 5585 (76.8) | 2287 (80.7) | 2913 (75.7) | 385 (65.9) | |
| Others | 1683 (23.2) | 548 (19.3) | 936 (24.3) | 199 (34.1) | |
| Occupational grade | <0.001 | ||||
| High | 2810 (38.7) | 1222 (43.1) | 1441 (37.4) | 147 (25.2) | |
| Intermediate | 3295 (45.3) | 1243 (43.8) | 1759 (45.7) | 293 (50.2) | |
| Low | 1163 (16.0) | 370 (13.1) | 649 (16.9) | 144 (24.7) | |
| Ethnicity | <0.001 | ||||
| White | 6605 (90.9) | 2649 (93.4) | 3452 (89.7) | 504 (86.3) | |
| Others | 663 (9.1) | 186 (6.6) | 397 (10.3) | 80 (13.7) | |
| Smoking | 0.01 | ||||
| Never | 3743 (51.5) | 1465 (51.7) | 1997 (51.9) | 281 (48.1) | |
| Ex | 2542 (35.0) | 1020 (36.0) | 1327 (34.5) | 195 (33.4) | |
| Current | 983 (13.5) | 350 (12.3) | 525 (13.6) | 108 (18.5) | |
| High alcohol intake | 0.07 | ||||
| No | 6249 (86.0) | 2410 (85.0) | 3332 (86.6) | 507(86.8) | |
| Yes | 1019 (14.0) | 425 (15.0) | 517 (13.4) | 77(13.2) | |
| Daily fruit and vegetables consumption | 0.001 | ||||
| No | 2787 (38.3) | 1022 (36.0) | 1520 (39.5) | 245 (42.0) | |
| Yes | 4481 (61.7) | 1813 (64.0) | 2329 (60.5) | 339 (58.0) | |
| Physical activity below recommended levels | <0.001 | ||||
| No | 2747 (37.8) | 1004 (35.4) | 1459 (37.9) | 284 (48.6) | |
| Yes | 4521 (62.2) | 1831 (64.6) | 2390 (62.1) | 300 (51.4) | |
| Diabetes | <0.001 | ||||
| No | 7199 (99.1) | 2819 (99.4) | 3810 (99.0) | 579 (97.6) | |
| Yes | 69 (0.9) | 16 (0.6) | 39 (1.0) | 14 (2.4) | |
| Body mass index | 7268 (100) | 25.1 (3.4) | 25.3 (3.8) | 25.7 (4.3) | 0.001 |
| Systolic blood pressure (mmHg) | 120.7 (13.1) | 120.6 (13.7) | 121.0 (14.4) | 0.86 | |
| Diastolic blood pressure (mmHg) | 79.6 (9.1) | 79.9 (9.4) | 80.2 (10.0) | 0.08 | |
| Total cholesterol (mmol/L) | 6.5 (1.2) | 6.5 (1.2) | 6.5 (1.2) | 0.73 | |
| Triglycerides (mmol/L) | 1.5 (1.2) | 1.5 (1.1) | 1.6 (1.1) | 0.34 | |
| Psychological distress score | 1.2 (2.8) | 3.5 (5.0) | 8.2 (8.3) | <0.001 | |
| Social support at work | 0.004 | ||||
| Low | 2258 (31.0) | 677 (23.9) | 1332 (34.6) | 249 (42.6) | |
| Middle | 2225 (30.6) | 852 (30.0) | 1229 (31.9) | 144 (24.7) | |
| High | 2126 (29.3) | 1028 (36.3) | 1004 (26.1) | 94 (16.1) | |
| Missing | 659 (9.1) | 278 (9.8) | 284 (7.4) | 97 (16.6) | |
| Number of relatives seen once or more monthly | 0.84 | ||||
| None | 2032 (28.0) | 805 (28.4) | 1049 (27.3) | 178 (30.5) | |
| One or more | 5170 (71.1) | 2007 (70.8) | 2761 (71.7) | 402 (68.8) | |
| Missing | 66 (0.9) | 23 (0.8) | 39 (1.0) | 4 (0.7) | |
| Number of friends seen once or more monthly | 0.75 | ||||
| None | 704 (9.7) | 275 (9.7) | 351 (9.1) | 78 (13.4) | |
| One or more | 6558 (90.2) | 2558 (90.2) | 3496 (90.8) | 504 (86.3) | |
| Missing | 6 (0.1) | 2 (0.1) | 2 (0.1) | 2 (0.3) | |
| Negative affect score | <0.001 | ||||
| Low | 2586 (35.6) | 1345 (47.4) | 1136 (29.5) | 105 (18.0) | |
| Middle | 2334 (32.1) | 933 (32.9) | 1237 (32.1) | 164 (28.1) | |
| High | 2348 (32.3) | 577 (19.6) | 1476 (38.3) | 315 (53.9) | |
| Self-rated health | <0.001 | ||||
| Good | 5492 (75.6) | 2520 (88.9) | 2587 (72.4) | 187 (32.0) | |
| Poor | 1776 (24.4) | 315 (11.1) | 1064 (27.6) | 397 (68.0) | |
| Perceived stress levels | <0.001 | ||||
| None | 490 (6.7) | 380 (13.4) | 91 (2.4) | 19 (3.3) | |
| A little or a fair amount | 5012 (69.0) | 2121(74.8) | 2662 (69.2) | 229 (39.2) | |
| Quite a lot or a great deal | 1766 (24.3) | 334 (11.8) | 1096 (28.5) | 336 (57.5) | |
Table 2 presents mutually adjusted associations between baseline covariates and incident CHD. Higher age, female sex, non-white ethnicity, current smoking, higher BMI, total cholesterol, poor self-rated health, and high exposure to stress were all associated with coronary death and incident non-fatal MI. Table 3 shows the associations between perceived impact of stress on health and the risk of CHD. In Model 1, where we adjusted the association for sociodemographic characteristics, participants who reported that stress has affected their health ‘a lot or extremely’ had 2.12 times higher (95% CI 1.52–2.98) risk of coronary deaths or incident non-fatal MI compared with those who responded ‘not at all’. After successive adjustments for health-related behaviours (Model 2), biological risk factors (Model 3), psychological distress, negative affect score, self-rated health and social support variables (Model 4), perceived stress levels (Model 5), and for all aforementioned variables (Model 6), the magnitude of this association was reduced but remained significant (HR = 1.49, 95% CI 1.01–2.22).
Table 2.
Mutually adjusted associations of baseline covariates with incident coronary heart outcomes
| Coronary death and incident non-fatal MI |
|||
|---|---|---|---|
| Variables | N events/N total | HR (95% CI) | P value |
| Age, years | 352/7268 | 1.08 (1.06–1.10) | <0.001 |
| Sex | |||
| Male | 291/5055 | 1 | |
| Female | 61/2213 | 0.33 (0.24–0.47) | <0.001 |
| Marital status | |||
| Married/cohabiting | 272/5585 | 1 | |
| Others | 80/1683 | 1.20 (0.90–1.53) | 0.17 |
| Occupational grade | |||
| High | 123/2810 | 1 | |
| Intermediate | 172/3295 | 1.29 (1.01–1.66) | 0.04 |
| Low | 57/1163 | 1.31 (0.89–1.94) | 0.17 |
| Ethnicity | |||
| White | 299/6605 | 1 | |
| Others | 53/663 | 1.80 (1.31–2.48) | <0.001 |
| Smoking | |||
| Never | 150/3743 | 1 | |
| Ex | 126/2542 | 1.06 (0.83–1.35) | 0.65 |
| Current | 76/983 | 2.03 (1.52–2.72)*** | <0.001 |
| High alcohol intake | |||
| No | 298/6249 | 1 | |
| Yes | 54/1019 | 0.91 (0.67–1.24) | 0.56 |
| Daily fruit and vegetable consumption | |||
| No | 158/2787 | 1 | |
| Yes | 194/4481 | 1.06 (0.85–1.32) | 0.60 |
| Physical activity below recommended levels | |||
| No | 228/4521 | 1 | |
| Yes | 124/2747 | 1.13 (0.88–1.39) | 0.40 |
| Diabetes | |||
| No | 346/7199 | 1 | |
| Yes | 6/69 | 1.20 (0.52–2.78) | 0.67 |
| Body mass index | 352/7268 | 1.06 (1.03–1.09) | <0.001 |
| Systolic blood pressure (mmHg) | 1.01 (1.00–1.02) | 0.09 | |
| Diastolic blood pressure (mmHg) | 1.02 (1.00–1.03) | 0.06 | |
| Total cholesterol (mmol/L) | 1.30 (1.18–1.43) | <0.001 | |
| Triglycerides (mmol/L) | 1.06 (1.00–1.13) | 0.07 | |
| Psychological distress score | 1.00 (0.98–1.02) | 0.87 | |
| Social support at work | |||
| Low | 1 | ||
| Middle | 0.94 (0.71–1.24) | 0.66 | |
| High | 0.93 (0.70–1.24) | 0.63 | |
| Missing | 1.02 (0.72–1.47) | 0.90 | |
| Number of relatives seen once or more monthly | |||
| None | 1 | ||
| One or more | 1.19 (0.93–1.53) | 0.18 | |
| Missing | 2.28 (1.04–5.03) | 0.04 | |
| Number of friends seen once or more monthly | |||
| None | 1 | ||
| One or more | 1.18 (0.79–1.77) | 0.41 | |
| Missing | 2.24 (0.28–17.94) | 0.45 | |
| Negative affect score | |||
| Low | 129/2586 | 1 | |
| Middle | 116/2334 | 1.03 (0.80–1.33) | 0.78 |
| High | 107/2348 | 0.94 (0.72–1.24) | 0.68 |
| Self-rated health | |||
| Good | 237/5492 | 1 | |
| Poor | 115/1776 | 1.33 (1.04–1.70)* | 0.02 |
| Perceived stress levels | |||
| None | 24/530 | 1 | |
| A little or a fair amount | 234/5279 | 1.25 (0.81–1.90) | 0.31 |
| Quite a lot or a great deal | 94/1766 | 1.71 (1.04–2.73)* | 0.03 |
*P < 0.05; **P < 0.01, ***P < 0.001.
Table 3.
Association of perceived impact of stress on health with coronary death and incident non-fatal myocardial infarction
| Perceived impact of stress on health |
|||
|---|---|---|---|
| ‘Not at all’ | ‘Slightly or Moderately’ | ‘A lot or extremely’ | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| N events / N participants | 127/2835 | 177/3849 | 48/584 |
| Adjustments: | |||
| Model 1: sex, age, ethnicity, marital status, occupational grade | 1.00 | 1.09 (0.86–1.37), P = 0.48 | 2.12 (1.52–2.98), P < 0.001 |
| Model 2: Model 1 + health-related behaviours | 1.00 | 1.08 (0.86–1.36), P = 0.50 | 2.03 (1.45–2.85), P < 0.001 |
| Model 3: Model 1 + biological risk factors | 1.00 | 1.05 (0.83–1.32), P = 0.70 | 1.89 (1.34–2.65), P < 0.001 |
| Model 4: Model 1 + other psychological factorsa | 1.00 | 1.05 (0.82–1.33), P = 0.75 | 1.82 (1.24–2.67), P = 0.002 |
| Model 5: Model 1 + perceived stress levels | 1.00 | 1.02 (0.80–1.29), P = 0.89 | 1.87 (1.31–2.68), P = 0.001 |
| Model 6: Model 1 + all aforementioned covariates | 1.00 | 0.97 (0.76–1.24), P = 0.76 | 1.49 (1.01–2.22), P = 0.04 |
aPsychological distress, negative affect score, self-rated health, social support at work, number of relatives and number of friends seen monthly.
Figure 1 illustrates unadjusted Kaplan–Meier survival curves for cumulative survival free from incident CHD as a function of perceived impact of stress on health. The survival curve for incident CHD among participants who reported that stress affected their health ‘a lot or extremely’ differed significantly (log-rank test, P < 0.001) from those in the two other groups and the difference between the groups increased over time. Figure 2 illustrates the corresponding fully adjusted Kaplan–Meier survival curves. Although, the difference between the groups was smaller, the survival disadvantage for CHD incidence in participants who reported that stress affected their health ‘a lot or extremely’ was maintained upon adjustment for all covariates, confirming the results of the fully adjusted Cox regression model reported in Table 3.
Figure 1.
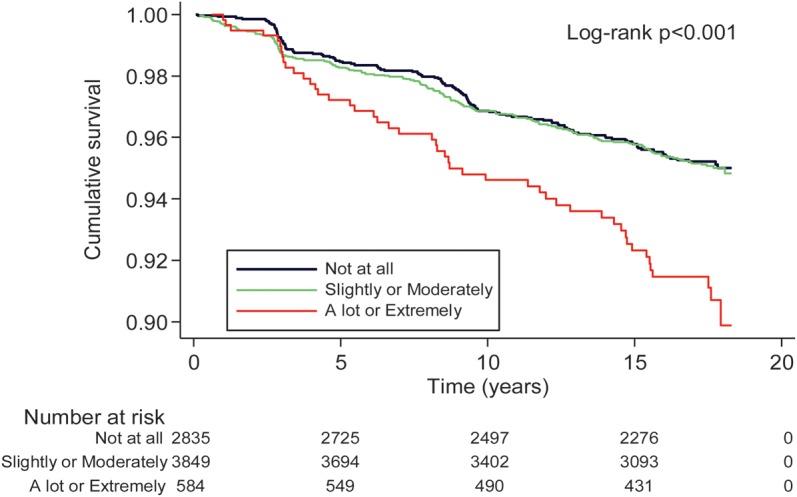
Unadjusted Kaplan–Meier survival curves showing the association between perceived impact of stress and incident CHD.
Figure 2.
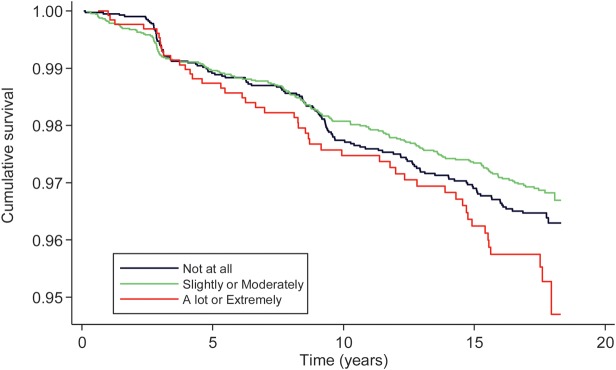
Kaplan–Meier survival curves showing the association between perceived impact of stress and incident CHD adjusted for sociodemographics, health behaviours, biological cardiovascular disease risk factors, self-rated health, negative affect, psychological distress, social support, and perceived levels of stress.
Sensitivity analyses
To test the robustness of our findings, we repeated the analyses excluding CHD events that occurred in the first 12 months of follow-up. These analyses provided a similar pattern of associations as those presented in Table 3; with the fully adjusted hazard ratio (HR) being: HR = 1.51 (95% CI 1.02–2.25), P = 0.04. To check that our results were not influenced by the categorization of participants into three groups, we repeated the analyses using the perceived impact of stress on health as a continuous variable in Cox regression models. In the fully adjusted model (model 6 of Table 3), a 1-unit increase in the perception of stress impact on health score was associated with an excess CHD risk of 15% [fully-adjusted HR = 1.15 (95% CI 1.01–1.29), P = 0.02]. This suggests that our findings were not dependent on categorization of the exposure variable.
We undertook additional analyses to check the shape of the association of perceived impact of stress on health with incident CHD by including it as a five-level categorical variable in the Cox regression model. In model 1, adjusted for sociodemographic characteristics, the risk of CHD across levels of the variable was 0.99 (0.77–1.27; P = 0.92) for participants who responded that stress affected their health ‘slightly’, 1.37 (1.00–1.87; P = 0.04) for those who reported ‘moderately’, 1.99 (1.37–2.85; P < 0.001) for those who responded ‘a lot’ and 3.04 (1.04–5.83; P = 0.001) for those who responded ‘extremely’ when compared with those who responded ‘not at all’. The corresponding fully adjusted HRs (95%, P values) were 0.91 (0.70–1.18, P = 0.46), 1.16 (0.83–1.63, P = 0.39), 1.45 (0.95–2.20, P = 0.08), and 2.19 (1.09–4.40, P = 0.03). This suggests a stepwise increase in risk, even though the risk is statistically significant or approaching significance at the top two categories of perceived impact of stress on health.
Discussion
Main findings
In this study, we sought to examine the prospective association between perceived impact of stress on health and incidence of CHD over 18 years. We found that participants who perceived stress to have affected their health ‘a lot or extremely’ had an increased risk of CHD, assessed using coronary deaths and incident MI. This association was independent of a wide range of mediators/confounders including perceived stress levels, personality, and self-rated health.
Findings in the context of the literature
To the best of our knowledge, the present study is the first to examine the association between individuals' perception of the impact of stress on their health and incidence of CHD in a large population-based cohort. We are aware of only one previous study which examined the association of individual's perception that stress affects their health with self-rated health, psychological distress, and all-cause mortality. These results, using the 1998 US National Health Interview Survey,15 were consistent with our results and showed individuals who perceived that stress had affected their health were more likely to report poor self-rated health and high psychological distress. However, associations with CHD were not examined in the study and perception of stress affecting health was not associated with all-cause mortality. A possible explanation is that all-cause mortality is a non-specific outcome, given the hypothesis that perceived stress has a specific effect on CHD and the overwhelming evidence for the deleterious effects of stress on the heart.3
The results of the present study are based on a large and well-characterized cohort with clinically validated endpoints tracked over an extended period of time. We were able to control for a wide range of health-related behaviours, measured biological parameters, and psychological factors. The novel aspect of our study is in the assessment of individuals' ‘perception of stress impact on their health’ rather than their ‘perceived stress levels’, the latter being common in the existing literature.10,13 The Whitehall II study is known for its investigation of the influence of stress on health outcomes (CHD in particular), but most of it focusses on work stress, often conceptualized using the job-strain model.23–29 Our focus is not work stress. By assessing individuals' ‘perception of stress impact on their health’, we believe that the present conceptualization is more likely to account for individuals' differences in responses to stress and in stress-related outcomes.
As hypothesized, we found that perceived impact of stress on health predicted CHD incidence independently of perceived stress levels. Importantly, the association between perceived stress levels and CHD in our analysis was attenuated and no longer significant when perceived impact of stress on health was included in the Cox regression model adjusted for sociodemographic characteristics [from a HR of 1.77 (95%CI 1.12–2.80) to HR of 1.56 (95% CI.0.96–2.52)]. This suggests that perceived impact of stress on health may mediate the association between perceived stress levels and CHD incidence. This is consistent with the idea that the response to stress (exposure to the same level of work stress for example) may differ greatly between individuals.11 Thus, assessment of individuals' perception of the impact of stress on their health in addition to their perceived stress levels is important in understanding the association between stress and health.
Interpretation and possible explanation of study results
There is little research on the perceived impact of stress on health and health outcomes. However, the association between stress and CHD has been examined and several mechanisms proposed.4,24 Psychological stress may trigger CHD events through biological mechanisms,30 including imbalanced sympathetic–parasympathetic activity (exaggerated heart rate and blood pressure),31 alteration of neuroendocrine axes (increased cortisol secretion),32 and activation of inflammatory systems (elevated cytokine levels).33 Psychological stress may also influence the risk of CHD more indirectly via health-damaging behaviours24,30 such as smoking, physical inactivity, or heavy alcohol consumption. In the present study, to take into account the potential influence of these factors on the association between perception of the impact of stress on health and CHD, we adjusted analyses for psychological distress, negative affect, measures of social support, and self-rated health in multivariate models. We found that these variables explained part (27%) of the association between perceived adverse impact of stress on health and CHD, but the association remained statistically significant. Biological risk factors explained 22% of the association, whereas health behaviours only 8%. Thus, our results suggest that psychological, biological, and behavioural mechanisms are plausible. However, it should be noted that all these factors were assessed at one point in time. Thus, the importance of the contribution of each set of variables might have been underestimated in the present study.
Limitations
In interpreting the present results, it is important to note some limitations. First, the study did not include blue collar or unemployed workers; thus, it is not representative of the general population limiting the generalizability of our findings. Second, participants were asked to report the impact of stress on their health using a single item. Although there is some recent research demonstrating the reliability and validity of single-item measures of psychological stress,12 use of a single item might have introduced some misclassification bias. Third, although we have adjusted for a wide range of covariates, there could be residual confounding or unmeasured risk factors that contribute to the association between perceived adverse impact of stress and incident CHD.
Conclusion and implications
Despite these potential limitations, the present findings represent an important contribution to research on stress. Relating individuals' perceptions of adverse effects of stress on health with their future risk of CHD has far-reaching theoretical and clinical implications. From a theoretical perspective, this implies that the perceived impact of stress on health is a valid concept and should be considered for inclusion in future studies on the association between stress and health. From a clinical perspective, these findings suggest that participant's perception of the impact of stress on their health may indeed be accurate, with regard to it being associated with adverse health outcomes. Thus, complaints of adverse stress impact on health should not be ignored as they may indicate increased risk of developing CHD. Assessing a subjective perception of adverse impact of stress on health might be considered as a part of managing patients with stress-related complaints in clinical settings. Given the robustness of the association between the perceived impact of stress on health and incident CHD after multivariate adjustment for a range of covariates, it is reasonable to assume that a simple question, such as the one used in the present study, could be used in general or specialized care settings.
Although, stress, anxiety, and worry are thought to have increased in recent years,34–36 we found that only participants (8%) who reported stress to have affected their health ‘a lot or extremely’ had an increased risk of CHD. In the future, randomized controlled trials are needed to determine whether disease risk can be reduced by increasing clinical attention to those who complain that stress greatly affects their health.
Funding
The Whitehall II study is supported by grants from the Medical Research Council; British Heart Foundation; National Heart Lung and Blood Institute (R01HL036310), US, NIH and the National Institute on Aging (R01AG013196 and R01AG034454), US, NIH. H.N. is supported by a grant from Institut de Recherche en Santé Publique (IReSP). M.K. is supported by the Medical Research Council (K013351), the EU OSH ERA Research Programme, the Academy of Finland, the US National Institutes of Health (R01HL036310, R01AG034454) and an ESRC professorship. J.V. is supported by the EU ERA-AGE2 Research Programme. M.J.S. is supported by a grant from the British Heart Foundation. A.S.-M. is supported by a ‘European Young Investigator Award’ from the European Science Foundation, and the National Institute on Aging, NIH (R01AG013196, R01AG034454).
Acknowledgements
We thank all participating civil service departments and their welfare personnel, and establishment officers; the Occupational Health and Safety Agency; the Council of Civil Service Unions; all participating civil servants in the Whitehall II study; and all members of the Whitehall II study team. The Whitehall II Study team comprises research scientists, statisticians, study coordinators, nurses, data managers, administrative assistants and data entry staff, who made the study possible.
Conflict of interest: none declared.
References
- 1.Selye H. The Physiology and Pathology of Exposure to Stress. Montreal, Canada: Acta, Inc; 1950. [Google Scholar]
- 2.Selye H. Stress and the general adaptation syndrome. BMJ. 1950;1:1383–92. doi: 10.1136/bmj.1.4667.1383. doi:10.1136/bmj.1.4667.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51:1237–46. doi: 10.1016/j.jacc.2007.12.024. doi:10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosengren A, Tibblin G, Wilhelmsen L. Self-perceived psychological stress and incidence of coronary artery disease in middle-aged men. Am J Cardiol. 1991;68:1171–5. doi: 10.1016/0002-9149(91)90189-r. doi:10.1016/0002-9149(91)90189-R. [DOI] [PubMed] [Google Scholar]
- 5.Macleod J, Smith GD, Heslop P, Metcalfe C, Carroll D, Hart C. Psychological stress and cardiovascular disease: empirical demonstration of bias in a prospective observational study of Scottish men. BMJ. 2002;324:1247. doi: 10.1136/bmj.324.7348.1247. doi:10.1136/bmj.324.7348.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–87. doi: 10.1001/jama.298.14.1685. doi:10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 7.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130:601–30. doi: 10.1037/0033-2909.130.4.601. doi:10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370:1089–100. doi: 10.1016/S0140-6736(07)61305-1. doi:10.1016/S0140-6736(07)61305-1. [DOI] [PubMed] [Google Scholar]
- 9.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360–70. doi: 10.1038/nrcardio.2012.45. doi:10.1038/nrcardio.2012.45. [DOI] [PubMed] [Google Scholar]
- 10.Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110:1711–6. doi: 10.1016/j.amjcard.2012.08.004. doi:10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 12.Littman AJ, White E, Satia JA, Bowen DJ, Kristal AR. Reliability and validity of 2 single-item measures of psychosocial stress. Epidemiology. 2006;17:398–403. doi: 10.1097/01.ede.0000219721.89552.51. doi:10.1097/01.ede.0000219721.89552.51. [DOI] [PubMed] [Google Scholar]
- 13.Kivimaki M, Virtanen M, Elovainio M, Kouvonen A, Vaananen A, Vahtera J. Work stress in the etiology of coronary heart disease—a meta-analysis. Scand J Work Environ Health. 2006;32:431–42. doi: 10.5271/sjweh.1049. doi:10.5271/sjweh.1049. [DOI] [PubMed] [Google Scholar]
- 14.Duijts SFA, Zeegers M, Borne BV. The association between stressful life events and breast cancer risk: a meta-analysis. Int J Cancer. 2003;107:1023–29. doi: 10.1002/ijc.11504. doi:10.1002/ijc.11504. [DOI] [PubMed] [Google Scholar]
- 15.Keller A, Litzelman K, Wisk LE, Maddox T, Cheng ER, Creswell PD, Witt WP. Does the perception that stress affects health matter? The association with health and mortality. Health Psychol. 2012;31:677–84. doi: 10.1037/a0026743. doi:10.1037/a0026743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marmot M, Brunner E. Cohort Profile: the Whitehall II study. Int J Epidemiol. 2005;34:251–6. doi: 10.1093/ije/dyh372. doi:10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- 17.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. doi:10.1161/01.CIR.90.1.583. [DOI] [PubMed] [Google Scholar]
- 18.Azevedo Da Silva M, Singh-Manoux A, Brunner EJ, Kaffashian S, Shipley MJ, Kivimäki M, Nabi H. Bidirectional association between physical activity and symptoms of anxiety and depression: the Whitehall II study. Eur J Epidemiol. 2012;27:537–46. doi: 10.1007/s10654-012-9692-8. 1–10 doi:10.1007/s10654-012-9692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh-Manoux A, Gueguen A, Martikainen P, Ferrie J, Marmot M, Shipley M. Self-rated health and mortality: short- and long-term associations in the Whitehall II study. Psychosom Med. 2007;69:138–43. doi: 10.1097/PSY.0b013e318030483a. doi:10.1097/PSY.0b013e318030483a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nabi H, Kivimäki M, De Vogli R, Marmot MG, Singh-Manoux A. Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. BMJ. 2008;337:a118. doi: 10.1136/bmj.a118. doi:10.1136/bmj.a118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nabi H, Singh-Manoux A, Shipley M, Gimeno D, Marmot MG, Kivimäki M. Do psychological factors affect inflammation and incident coronary heart disease: the Whitehall II Study. Arterioscler Thromb Vasc Biol. 2008;28:1398–406. doi: 10.1161/ATVBAHA.108.167239. doi:10.1161/ATVBAHA.108.167239. [DOI] [PubMed] [Google Scholar]
- 22.Nieto FJ, Coresh J. Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol. 1996;143:1059–68. doi: 10.1093/oxfordjournals.aje.a008670. doi:10.1093/oxfordjournals.aje.a008670. [DOI] [PubMed] [Google Scholar]
- 23.Virtanen M, Ferrie JE, Singh-Manoux A, Shipley MJ, Vahtera J, Marmot MG, Kivimäki M. Overtime work and incident coronary heart disease: the Whitehall II prospective cohort study. Eur Heart J. 2010;31:1737–44. doi: 10.1093/eurheartj/ehq124. doi:10.1093/eurheartj/ehq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M, Badrick E, Kivimäki M, Marmot M. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J. 2008;29:640–8. doi: 10.1093/eurheartj/ehm584. doi:10.1093/eurheartj/ehm584. [DOI] [PubMed] [Google Scholar]
- 25.Kivimäki M, Nyberg ST, Batty GD, Shipley MJ, Ferrie JE, Virtanen M, Marmot MG, Vahtera J, Singh-Manoux A, Hamer M. Does adding information on job strain improve risk prediction for coronary heart disease beyond the standard Framingham risk score? The Whitehall II study. Int J Epidemiol. 2011;40:1577–84. doi: 10.1093/ije/dyr078. doi:10.1093/ije/dyr078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuper H, Singh-Manoux A, Siegrist J, Marmot M. When reciprocity fails: effort-reward imbalance in relation to coronary heart disease and health functioning within the Whitehall II study. J Occup Environ Med. 2002;59:777–84. doi: 10.1136/oem.59.11.777. doi:10.1136/oem.59.11.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bosma H, Peter R, Siegrist J, Marmot M. Two alternative job stress models and the risk of coronary heart disease. Am J Public Health. 1998;88:68–74. doi: 10.2105/ajph.88.1.68. doi:10.2105/AJPH.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marmot MG, Bosma H, Hemingway H, Brunner E, Stansfeld S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350:235–9. doi: 10.1016/s0140-6736(97)04244-x. doi:10.1016/S0140-6736(97)04244-X. [DOI] [PubMed] [Google Scholar]
- 29.Bosma H, Marmot MG, Hemingway H, Nicholson AC, Brunner E, Stansfeld SA. Low job control and risk of coronary heart disease in Whitehall II (prospective cohort) study. BMJ. 1997;314:558–65. doi: 10.1136/bmj.314.7080.558. doi:10.1136/bmj.314.7080.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. doi:10.1161/01.CIR.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 31.Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension. 2000;35:880–6. doi: 10.1161/01.hyp.35.4.880. doi:10.1161/01.HYP.35.4.880. [DOI] [PubMed] [Google Scholar]
- 32.Brunner EJ, Hemingway H, Walker BR, Page M, Clarke P, Juneja M, Shipley MJ, Kumari M, Andrew R, Seckl JR, Papadopoulos A, Checkley S, Rumley A, Lowe GD, Stansfeld SA, Marmot MG. Adrenocortical, autonomic, and inflammatory causes of the metabolic syndrome: nested case–control study. Circulation. 2002;106:2659–65. doi: 10.1161/01.cir.0000038364.26310.bd. doi:10.1161/01.CIR.0000038364.26310.BD. [DOI] [PubMed] [Google Scholar]
- 33.von Kanel R, Mills PJ, Fainman C, Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med. 2001;63:531–44. doi: 10.1097/00006842-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Vagg PR, Spielberger CD. The job stress survey: assessing perceived severity and frequency of occurrence of generic sources of stress in the workplace. J Occup Health Psychol. 1999;4:288–92. doi: 10.1037//1076-8998.4.3.288. doi:10.1037/1076-8998.4.3.288. [DOI] [PubMed] [Google Scholar]
- 35.Spielberger CD, Reheiser EC. The job stress survey: measuring gender differences in occupation stress. J Soc Behav Pers. 1994;9:199–218. [Google Scholar]
- 36.Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100–13. doi: 10.1177/070674370605100206. [DOI] [PubMed] [Google Scholar]


