Abstract
Purpose
Considerable research has demonstrated the negative psychosocial impact of cancer. Recent work has highlighted positive psychosocial outcomes. Research is now needed to evaluate the relationship between negative and positive impacts. This paper reports the development and validation of a measurement model capturing positive and negative psychosocial illness impacts.
Methods
The sample included 754 cancer patients on- or post-treatment. Item development was informed by literature review, expert input patient interviews and the results of a pilot study of 205 cancer patients, resulting in 43 positive and 46 negative items. Factor analyses were used to evaluate the dimensionality of the item pools. Analysis of variance (ANOVA) was used to examine relationships between psychosocial illness impact and other variables.
Results
Unidimensionality was demonstrated within but not across negative and positive impact items. ANOVA results showed differential relationships between negative and positive impacts, respectively, and patient sociodemographic and clinical variables.
Conclusion
Positive and negative psychosocial illness impacts are best conceptualized and measured as two independent factors. Computerized adaptive tests and short-form measures developed from this comprehensive psychosocial illness impact item bank may benefit future research and clinical applications.
Keywords: Psychosocial sequelae, Cancer, Cancer survivors, Bi-factor analysis
Introduction
Life threatening and chronic illnesses such as cancer can cause uncertainty about the future, interfere with coping and relationships [1–10]. Historically, psychosocial research has focused on cancer’s negative consequences, but a growing literature documents positive life changes including greater appreciation of life, changed priorities, closer relationships, and enhanced spirituality [11–23]. A broad conceptualization of reaction to illness, taking into account both positive and negative outcomes, has been advocated [24]. However, with few exceptions [25–28], existing measures target positive and negative life changes following cancer independently (e.g., Benefit-Finding scale [23, 29], COPE [30], Impact of Events Scale, IES [31], Perceived Benefit Scales [32], Stress-Related Growth Scale, SRGS [33], and Post-Traumatic Growth Inventory, PTGI [34]). Examining the full spectrum of the impact of the cancer experience by including both negative and positive perspectives helps to minimize potential socially desirable or self-enhancement response biases [23, 35]. Attempts have been made to address these concerns by including positive and negative items in scales such as the Life Impact Scale, LIS [25], and Impact of Cancer Scale, IOC [36, 37]. The LIS captures relationships/life outlook, health behaviors, and financial situation, with over half of the items addressing physical, behavioral, or practical issues rather than strictly psychosocial concerns. The IOC emphasizes concrete experiences across multiple domains, including physical, psychological, social, and spiritual/existential impacts.
These two measures use different approaches to produce separate positive and negative impact scores. The LIS asks participants to describe the impact of cancer using a neutral item stem (e.g., your exercise activities) and positive and negative Likert-type response options (0 = “does not apply,” 1 = “very negative” to 5 = “very positive”). Sub-scales are created using the number and magnitude of positive and negative responses. The IOC uses different positive and negative items (e.g., “worry about my future,” “take better care of self”) with a 5-point Likert scale response option (1 = “strongly disagree” to 5 = “strongly agree”) and yields both positive and negative impacts of cancer scores. These scales conceptualize positive and negative effects as coexisting within the same domain and eliminate the risk of an aggregated score yielding “no impact” if positive and negative impacts cancel one another [17, 38]. However, only a measure that includes different content assessing both positive and negative impacts (e.g., the IOC) establishes a conceptual framework in which they are not two sides of the same continuum.
Building on previous research, we sought to develop a measurement framework for positive and negative psychosocial illness impacts that capture the emotional, cognitive, and behavioral responses resulting from illness experiences, across the cancer disease/treatment continuum, from diagnosis to post-treatment survivorship. The item pool we describe here was informed by patient and expert input as well as qualitative and quantitative data. Items assess positive or negative psychosocial sequelae and highlight the contribution of the illness (e.g., “My illness has helped me become a better person”). Aiming to measure a cohesive latent construct, we focused entirely on psychosocial impact, rather than including practical changes (e.g., in finances). Given that psychosocial impact is experienced by people with various chronic diseases, items were worded in a general way to permit future adaptation to other illnesses. We also explored the relationship of demographic variables and psychosocial impact upon cancer experience in this report.
Methods
Development of the psychosocial illness impact (II) item pool
In a pilot study, we examined the relationship between positive and negative psychosocial illness impacts. Results guided development of the conceptual framework tested in the main study. Both the pilot and main studies were approved by the Institutional Review Board, and all participants provided informed consent.
Pilot study
A research team, consisting of four clinical psychologists and one occupational therapist, reviewed available scales measuring the psychosocial impact to patients from their diseases. Candidate measures included the IES, SRGS, and PTGI, and permission to include and possibly modify items was obtained from the respective authors. Candidate items were rejected or modified when deemed to be outside the scope of psychosocial impact, vague, confusing, redundant, or of uncertain valence. Wording was revised to standardize items and emphasize the impact from illness (e.g., “because of my illness”). New items were written to fill identified conceptual gaps. The resulting II item pool consisted of 46 items (23 positively worded and 23 negatively worded) including 19 newly written items, 11 from the IES [31], and 16 modified from existing scales (PTGI [34], SRGS [33], and Functional Assessment of Cancer Therapy-Cognition [39, 40]).
This item pool was evaluated using data from 205 oncology patients from the Chicago metropolitan area (average age 59.6 years, 59% female, 93.2% White). The largest proportion (25.9%) was diagnosed with breast cancer, followed by colorectal (15.1%), non-Hodgkin’s lymphoma (14.1%), leukemia (6.8%), and ovarian cancer (5.9%). Average time since diagnosis was 34 months (range: 0.5–302). All participants were receiving at least one treatment when this study was conducted (90.2% chemotherapy, 9.3% hormone therapy, and 5.9% radiation). The majority of patients were able to perform normal activities with either no (29.8%) or some (51.7%) symptoms.
Unidimensionality of items was examined using exploratory factor analysis (EFA) with varimax rotation (criterion: factor loading > 0.3; i.e., 2-tailed test, p < 0.01); Rasch analysis [41] was used to calculate item fit statistics (criterion: MnSq < 1.4). EFA results showed that all positive items had significant loadings (0.43–0.89) on Factor 1 while 19 negative items loaded on Factor 2 (0.30–0.79) and 4 negative items did not have significant loadings on either factor. We therefore analyzed negative (NII) and positive (PII) items separately using Rasch analysis. Six items did not meet the fit statistics criterion. Based upon results from both EFA and Rasch analysis, 8 items (2 positive and 6 negative) were removed from the pool. Both PII and NII scales had acceptable internal consistency (alpha = 0.95 and 0.93, respectively) and discriminated patients by the Eastern Cooperative Oncology Group performance status rating (ECOG PSR) (F(3,201) = 2.74, p < 0.05 for PII; F(3,201) = 10.03, p < 0.05 for NII). The correlation between the two scales was 0.071, p = 0.310 [42, 43]. These results suggest that negative and positive psychosocial illness impacts are two distinct concepts. We therefore chose to enhance PII and NII scales by assessing them separately in the current study.
Main study
Item pool generation
A clinician/investigator panel consisting of clinical psychologists and patient outcome researchers was formed to guide the development of the II item pool for the current study. Four psychosocial illness impact categories, representing both PII and NII, were identified through results from the pilot study, literature, and thematic review of definitions: Coping (PII)/Stress Response (NII), Social Connection (PII)/Social Isolation (NII), Self-concept (PII & NII), and Meaning and Spirituality (PII & NII). Item generation and classification into categories were conducted using the following steps. Panel members independently grouped items from the pilot study, and those generated from literature review, into the respective categories and later reached consensus on items for which there was disagreement. Cognitive interviews were conducted with cancer patients (N = 15) for their input on study themes and items. Feedback on Meaning and Spirituality was gathered from a team of chaplains to augment areas of expertise represented in the panel. After reviewing this input, the panel refined content area definitions and wrote items to cover content areas that were thought missing during the discussion. Items that were redundant, inapplicable, or vague were modified or excluded from the pool. As a result, a total of 89 items (43 positively worded and 46 negatively worded) were included for the field testing. Table 1 shows the conceptual model and example items within each category.
Table 1.
Psychosocial illness impact conceptual model
| Sub-domain | Positive impact |
Negative impact |
||
|---|---|---|---|---|
| Item n | Sample item | Item n | Sample item | |
| Self-concept | 9 | My illness has helped me discover I am stronger than I thought I was |
9 | Because of my illness, I feel worthless |
| (positive) Coping (negative) Stress Response |
10 | My illness has taught me how to adjust to things I cannot change |
13 | I have been upset about my illness |
| Meaning and Spirituality | 13 | My illness has helped me find strength in my faith or spiritual beliefs |
13 | Because of my illness, I get less comfort from my faith or spiritual beliefs |
| (positive) Social Connection (negative) Social Isolation |
11 | My illness has helped me become more aware of the love and support available from other people |
11 | Because of my illness, I feel isolated from others |
Sample
Participants (N = 754) were recruited from (1) oncology clinics in the Chicago metropolitan area (n = 249); (2) local and national support societies (CancerCare, The Wellness Community & Gilda’s Club) via internet (n = 256); and (3) an internet survey panel company (n = 249). Diagnoses and treatment information of groups 2 and 3 were collected via self-report. Eligibility criteria included a diagnosis of cancer and English fluency. Participants were primarily White (97.4%), women (61%), married, or living with a partner (61.2%) and had at least some college education (80%) and a household income higher than $50,000 (55.2%). They had an average age of 57.41 years (SD = 13.37); 30.59% were employed full time and 29.26% were retired. Participants had a wide range of cancer diagnoses: 29.3% breast, 9.9% colorectal, 8.9% prostate, 8.8% urological, and 8.1% gynecological. The average time since cancer diagnosis was 4.1 years (SD = 6.4) with 32.6% of participants diagnosed less than 1 year and 33.2% more than 5 years prior. A majority of participants (53.9%) received chemotherapy and 18.4% received radiation therapy; 23.2% had experienced a cancer recurrence. Specifically, 34% were receiving active treatment (9% with early stage, 13% with advanced stage, and 12% with unknown stage disease) and 62% were post-treatment (33% within 5 years of diagnosis and 29% more than 5 years since diagnosis). Most participants reported either no symptoms (49.8%) or being ambulatory with some symptoms (35.6%).
Analysis
We first evaluated dimensionality of items and used SAS (v9.1) [44] to perform the EFA and MPlus (v5.0) (Los Angeles, CA: Muthen and Muthen) for confirmatory factor analysis (CFA) and bi-factor analysis. Data were randomly divided into two datasets: Dataset 1 (n = 376) for EFA and Dataset 2 (n = 378) for CFA and bi-factor analysis. Using EFA, we determined the factor structure using the following criteria: (1) number of factors with eigenvalue > 1 [45]; (2) number of factors before the break in a scree plot [46]; and (3) factors that have explained variance > 5% [47]. Items with loadings greater than 0.4 were considered significant. Acceptable CFA results were indicated by Tucker-Lewis Index (TLI) [48] and comparative fit index (CFI) values of 0.90 or greater, root mean square error of approximation (RMSEA) less than 0.1, and item R-square > 0.3.
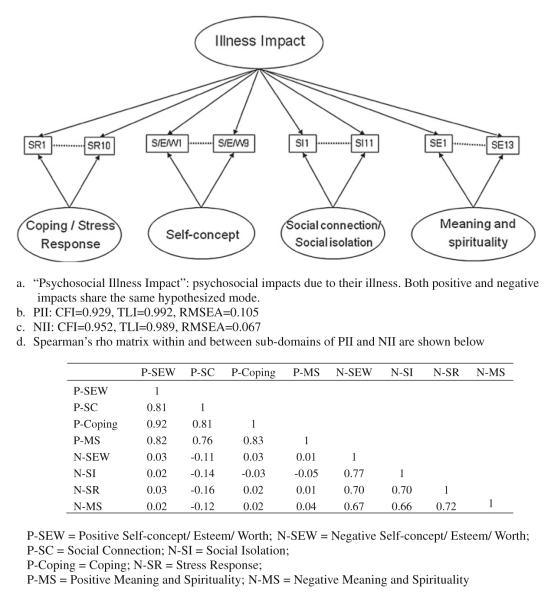
The II measurement model (Fig. 1) was determined based on the results of the bi-factor analysis, which better represents the current framework by capturing the general and sub-domains simultaneously. A bi-factor analysis is hypothesis-driven, consisting of a general factor (i.e., N-II and P-II) and local factors (4 sub-domains under the umbrella of N-II and P-II). The general and local factors are modeled as orthogonal and therefore the relationship between items and the general factor is not constrained to be proportional to the relationship between the first- and second-order factors as demonstrated in other hierarchical CFA. When the general factor explains covariance between items, uniformly high standardized loadings (i.e., >0.3) are seen for the general factor, indicating that it is appropriate to report a single score. Yet, investigators can choose to report sub-scale scores as tested in the hypothesized model. If the sub-domains represent demonstrably separate constructs, loadings on the general factor will not be uniformly high, leading one to reject the conclusion that the items are sufficiently unidimensional, making it more appropriate to report scores of sub-domains separately, but not a single overall score [49–51].
Fig. 1.
Measurement model used for bi-factor analysis
Lastly, using analysis of variance (ANOVA), we evaluated whether significantly different psychosocial impact exists across groups or levels of the following variables: gender, education, years since diagnosis, household incomes, and functional performance (see Tables 2, 3 for categories). The relationship between psychosocial illness impact and age was evaluated using Pearson correlations. We explored whether certain demographic and clinical variables were associated with different magnitudes of positive and negative psychosocial impacts.
Table 2.
ANOVA results for general positive psychosocial impact and its four components (i.e., local factors)
| P-II F(12,694) = 12.76, p<0.001 |
P-SEW F(12,694) = 10.54, p<0.001 |
P-SC F(12, 694) = 13.48, p<0.01 |
P-coping F(12,694) = 10.06; p<0.01 |
P-MS F(12,693) = 12.73, p<0.01 |
|
|---|---|---|---|---|---|
| Year since diagnosisa | F = 1.72 | F = 1.00 | F = 7.10* | F = 0.69 | F = 1.53 |
| Educationb | F = 8.15* | F = 6.24* | F = 2.6 | F = 7.02* | F = 13.31* |
| Genderc | F = 85.77* | F = 79.7* | F = 94.88* | F = 72.63* | F = 57.68* |
| Household incomed | F = 9.59* | F = 7.81* | F = 5.28* | F = 7.33* | F = 12.81* |
| Functional statuse | F = 4.52 | F = 0.82 | F = 11.0* | F = 1.48 | F = 6.08* |
P-II positive psychosocial impact, P-SEW self-concept/esteem/worth, P-SC Social Connection, P-Coping Coping, P-MS Meaning & Spirituality
p<0.01
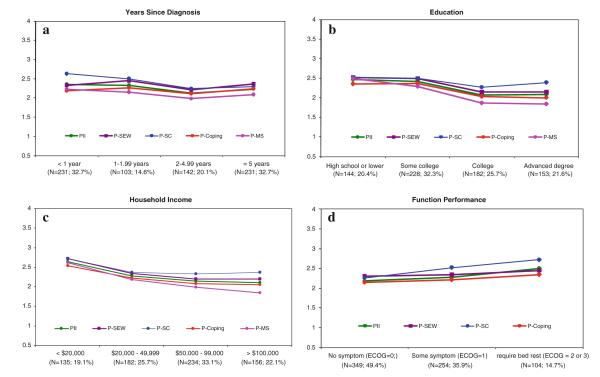
Those who had diagnosed of cancer less than 1 year had higher scores than those between 2 and 5 and those more than 5 years (see Fig. 3a)
“High school or lower” participants had higher scores than those with either a “college” or an “advanced degree”; participants with “some college” had higher scores than those with either a “college” or an “advanced degree” (see Fig. 3b)
Females had significantly higher scores than males on concepts measuring positive impacts
Those with household income <$20,000 had higher scores than other groups ($20,000–$49,000; $50,000–$99,999;>$100,000). Additionally, “$20,000–$49,999” group also had higher score than “>$100,000” group in “spiritual/existential impact” (see Fig. 3c)
For “Social connection,” participants with “no symptom” (ECOG PSR = 0) had lower scores than those with “some symptom” (ECOG PSR = 1) or “required bed rest” (ECOG PSR = 2 or 3). For “Meaning and spirituality,” participants with either “no symptom” or “some symptom” had lower scores than those “require bed rest.” (See Fig. 3d)
Table 3.
ANOVA results for general negative psychosocial impact and its four components (i.e., local factors)
| N-II F(12, 694) = 21.16; p<0.01 |
N-SEW F(12, 694) = 13.72, p<0.01 |
N-SI F(12, 693) = 24.29, p<0.01 |
N-SR F(12, 694) = 20.26, p<0.01 |
N-MS F(12, 694) = 6.86, p<0.01 |
|
|---|---|---|---|---|---|
| Year since diagnosisa | F = 10.12* | F = 4.19* | F = 6.25* | F = 15.68* | F = 3.5 |
| Education | F = 0.18 | F = 0.77 | F = 0.10 | F = 1.97 | F = 0.18 |
| Genderb | F = 18.15* | F = 9.51* | F = 13.09* | F = 26.41* | F = 3.39 |
| Household incomec | F = 8.20* | F = 8.26* | F = 14.82* | F = 3.89* | F = 3.39 |
| Functional statusd | F = 90.13* | F = 57.71* | F = 107.44* | F = 74.85* | F = 28.86* |
N-II negative psychosocial impact, N-SEW self-concept/esteem/worth, N-SI Social Isolation, N-SR Stress response, N-MS Meaning & spirituality
P<0.01
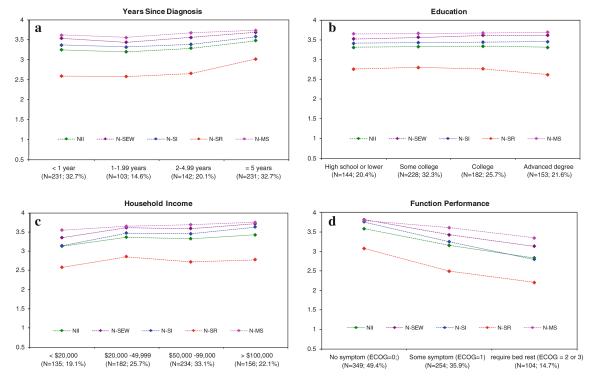
Those who had diagnosed of cancer less than 1 year had higher scores than those between 2 and 5 and those more than 5 years. Yet for “social-concept,” those who had diagnosed of cancer more than 5 years had higher scores than other three groups (i.e., <1, 1–2, and 2–5) (See Fig. 4a)
Females had significantly lower scores than males on concepts measuring negative impacts
Those with household income <$20,000 had lower scores than other groups ($20,000–$49,000; $50,000–$99,999; >$100,000). Additionally, “$50,000–$99,000” group also had lower scores than “>$100,000” group. Yet for “Stress response,” “<$20,000” group had lower scores than “$20,000–$49,999” group
Participants with “no symptom” had higher scores than those with either “some symptom” or “require bed rest,” and participants with “some symptom” had higher scores than those “require bed rest”
Results
Evaluation of dimensionality
All NII items were reversed to the same direction as PII items. Thus, higher PII and NII scores both represent favorable (more positive and less negative) psychosocial illness impact. EFA results showed 11 factors had eigenvalues > 1 and only two of them had explained variance > 5%. The scree plot (Fig. 2) clearly shows two factors before the break. All PII items had significant loadings on Factor 1 (0.49–0.91) and Factor 1’s correlations with Factors 2, 3, and 4 were negligible (r = 0.09, 0.10, and −0.09, respectively). In terms of NII, Self-concept and Social Isolation items both loaded on Factor 2 (0.46–0.99). Stress Response items loaded on either Factors 2 or 4, with 5 of those 13 items having loadings greater than 0.4 on both factors. Negative Meaning and Spirituality items demonstrated significant loadings on either Factors 2 or 3. Item “Because of my illness, I am less able to attend usual religious services” did not show a significant loading on any of these factors. This item was excluded from further analyses. Moderate inter-factor correlations were found between Factor 2 and both Factors 3 and 4 (r(F2–F3) = 0.46; r(F2–F4) = 0.43, respectively), suggesting that NII items might be represented by a single factor.
Fig. 2.
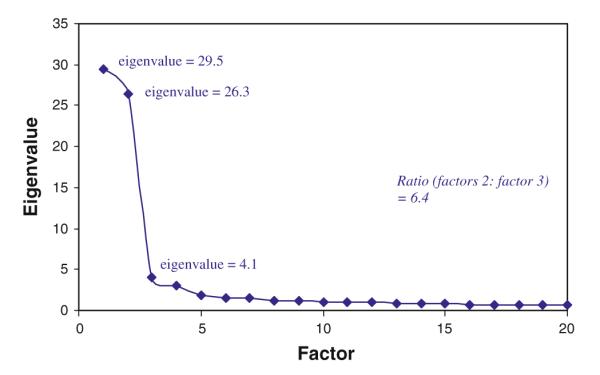
Scree plot from the results of EFA analysis on dataset 1 (n = 376)
Using Dataset 2, acceptable fit indices (CFI = 0.96; TLI = 0.96) were obtained from a 2-factor CFA where PII and NII were assigned to be two independent factors. We then conducted another 2-factor CFA, in which PII and NII factors were presumed correlated (producing CFI = 0.863, TLI = 0.951). That analysis also indicated that the correlation between PII and NII factors was negligible (r = 0.076). Thus, we concluded that PII and NII should be treated as two independent factors.
In bi-factor analysis, the general factor was defined as psychosocial illness impact (either PII or NII), and local factors were Coping/Stress Response, Social Connection/Social Isolation, Self-concept, and Meaning and Spirituality (Table 1). Both PII and NII were tested using the same hypothesized model but were analyzed separately given their negligible correlation. Bi-factor analysis showed all items had significant loadings on the general factor, with factor loadings ranging from 0.610 to 0.882 for PII and from 0.492 to 0.891 for NII. Acceptable fit indices were found for NII (CFI = 0.952, TLI = 0.989, RMSEA = 0.067) while borderline acceptable fit indices for PII (CFI = 0.929, TLI = 0.992, RMSEA = 0.105), confirming that the hypothesized model is valid for both. These results support the sufficient unidimensionality of PII and NII items, and two summation scores should be produced (PII & NII) with the recognition of four sub-domains represented by local factors.
When comparing item loadings between general and local factors, some items showed significant loadings on both. Loadings on the general factor were larger than those on all local factors except Stress Response and positive and negative Meaning & Spirituality. Specifically, Meaning and Spirituality items demonstrated loadings on the general and local factors that were of similar magnitudes. Likewise, 7 of 14 Stress Response items had loadings greater than 0.4 on both general and local factors. Six of these items used a frequency rating scale (“none of the time” to “all of the time”) and five (all from the IES) used a unique time context (“in the past 7 days”), whereas other Stress Response items used an intensity rating scale (“not at all” to “very much”) and no specific timeframe. These item format artifacts may have contributed to the cross-loading of these Stress Response items, but their high loadings (0.497–0.619) on the general factor suggest that these items characterize general negative psychosocial illness impact.
To confirm this, we conducted two additional bi-factor analyses. Five PII items, which had similar loading on both general and local factors or slightly higher loading on the local factor, were treated as a separate local factor. Results showed that although all PII items now had higher loadings on the general factor than on the local factor, a borderline CFI (0.89) was obtained, suggesting that including these five items in the originally assigned local factor produces a better fit. When cross-loading NII items were separated from their original local factors and treated as two new local factors, fit statistics were similar (CFI = 0.948, TLI = 0.987, RMSEA = 0.072) and the items had comparable loadings on both general and local factors. Therefore, from a measurement perspective, these items could be either included or excluded from the general factor. We opted to keep items in their original local factors for the sake of parsimony and content coverage.
PII and NII both demonstrated excellent internal consistency (alpha = 0.98 and 0.97, respectively). Item-scale correlations ranged from 0.61 to 0.84 for PII and from 0.45 to 0.74 for NII. Correlations within sub-domains are reported in Fig. 1, in which high Spearman’s rho values for the sub-domains are found within (range: 0.755–0.920 for PII; 0.659–0.767 for NII) but not across PII and NII (range: 0.003–0.157). Results again confirmed sufficient unidimensionality within, but not between, the NII and PII item pools.
Variables associated with illness impact
The following analyses were conducted using both general factors and each local factor. Age was significantly (p < 0.001) correlated with PII and its sub-domains in a negative direction, with coefficients ranging from −0.140 (Coping) to −0.230 (Social Connection). In contrast, age was significantly correlated with NII (which was reverse scored) and its sub-domains in a positive direction, with coefficients ranging from 0.246 (negative Self-concept) to 0.359 (Stress Response). These results indicate that older participants reported both less positive and negative psychosocial impacts of illness.
ANOVA results showed that gender, income, education, time since diagnosis, and performance status were significantly (p < 0.01) associated with illness impact as a whole as well as its individual components. Results are summarized in Tables 2 (PII) and 3 (NII), and comparisons of group means are depicted in Figs. 3a–d (PII) and 4a–d (NII). Tukey’s post hoc comparisons showed that women reported more positive and less negative psychosocial illness impacts as reflected in scores on all sub-domains except negative Meaning and Spirituality, in which no significant differences were found. Likewise, participants with lower income reported more PII and less NII. Participants with less formal education reported more PII; however, no significant differences related to educational level were found for NII.
Fig. 3.
Mean comparisons across sub-groups for positive psychosocial impact (P-II) as well as its local factors (P-SEW self-concept/esteem/worth, P-SC Social Connection, P-Coping Coping, P-MS Meaning & Spirituality)
Years since cancer diagnosis were significantly associated with NII but not PII, except for positive Social Impact. Specifically, results suggest that both NII and PII, in general, and positive social impact diminish over time. Lastly, participants with higher functional performance reported less PII in sub-domains of Social Impact and Meaning & Spirituality and less NII across all sub-domains.
Discussion
Both positive and negative psychosocial impacts of illness are undeniable realities for most patients throughout their experiences with cancer and other life threatening illnesses. As conceptualizations of psychosocial adaptation in chronic illness and subsequent interventions increasingly acknowledge that positive and negative sequelae can coexist at different levels within the same sub-domains or content areas, comprehensive measures are needed in order to more fully capture patients’ experiences. Such measures should be applicable throughout the cancer care continuum so that patients’ scores can be compared over time, as they progress through different disease and treatment phases.
Recent measures have included items assessing both positive and negative sequelae. Additionally, measures should move away from simple problem checklists and instead assess latent constructs. In this study, we sought to develop a measurement framework to capture positive and negative psychosocial effects across the disease/treatment continuum. Of particular interest was the dimensionality of the psychosocial illness impact construct and how positive and negative sequelae related to one another and to other patient variables.
We created our psychosocial illness impact item pool using expert and patient input, as well as qualitative and quantitative data, at various points in the development process. Results of our pilot study established the foundation for the current study. We developed and tested a conceptual framework of positive and negative illness impacts (NII & PII), consisting of four content areas as shown in Fig. 1: Coping/Stress Response, Social Connection/Social Isolation, Self-concept, and Meaning and Spirituality. Bi-factor analysis results verified this framework supporting one single P-II or N-II score. However, sub-domain-specific scores can be reported in a psychometrically sound manner if investigators are interested in specific sub-domains. Our results provide an empirical basis for further development of a comprehensive measurement model in which positive and negative illness impacts are two distinct factors each comprised of four sub-domains corresponding to the content areas mentioned above. While these sub-domains represent important, conceptually distinct content areas, the prevailing driver of the patients’ reports relates to whether the illness impact is positive or negative. This is consistent with the common observation that general positive and negative effects are also essentially uncorrelated [25–27].
Results of our study suggested that PII and NII are two independent concepts, are each sufficiently unidimensional, and can adequately be represented by two summation scores. Differential associations with sociodemographic and clinical variables between PII and NII further confirmed our results. For example, more positive impact was reported by study participants who were younger, female, and had lower income and education levels. More negative impact was also reported by study participants who were younger, female, and had lower income levels, as well as by participants who were more recently diagnosed and had poorer functional status. This is consistent with the literature in which, compared to older cancer survivors, younger survivors report greater positive benefits in their lives due to the cancer experience [14, 26, 37] while also reporting greater negative life disruption [25, 52, 53]. Although a cancer diagnosis and treatment can be exceedingly stressful, most individuals adapt well over time [54]. Among patients who complete treatment and whose cancer is in remission or otherwise controlled, their psychological adjustment and quality of life is comparable to the general population by 1–2 years post-diagnosis [7, 55, 56]. These findings are consistent with our findings that more recently diagnosed individuals had worse negative impacts than those who were further out from treatment.
Other findings present a more equivocal picture when compared to existing research. For example, a gender difference in cancer experiences is not consistently supported by the cancer literature [37, 57–60]. Regarding measures of socioeconomic status (e.g., income and education), associations with positive impact are often mixed, revealing positive, negative, and no associations (see Stanton et al. [60] for a review). In contrast, associations with negative impact and income level are more consistent and are likely impacted by concurrent factors such as limited access to healthcare, poor or no insurance coverage, and underutilization of services. Zebrack and colleagues [37] have noted a significant link between lower income and greater negative impact from the cancer experience. Although the exact relationship between some sociodemographic variables and illness impact remains to be clarified, our results, taken together, corroborate a framework in which negative and positive psychosocial illness impacts are independent factors, not opposite ends of a spectrum.
We consider the current study to be a starting point for future work that carefully examines how best to conceptualize and measure the psychosocial impact of illness, but it is not without limitations. First, because the II items emphasize the contribution of the illness (e.g., “My illness has helped me…” or “Because of my illness…”), the measure requires that respondents make attributional judgments; how this affects scores has not been evaluated. A qualitative study to evaluate patient perception of various formats of similar item content is warranted. Second, the term “impact” implies a degree of causality that we are unable to determine from this cross-sectional dataset. A longitudinal study tapping patient experience from diagnosis to long-term survivorship can help model the experience trajectory in a more precise manner. Third, the population is a convenience sample and the majority of participants were White. The degree and type of illness impact experiences may vary as a function of race/ethnicity; therefore, future studies should include more diverse samples. Fourth, although we sought to include participants across the entire disease/treatment continuum, we did not stratify recruitment based upon these criteria (e.g., newly diagnosed, currently on-treatment, post-treatment). Future development in this area should determine its suitability for use across the treatment continuum, which will be paramount in longitudinal studies tracking psychosocial illness impact over time.
In the current study, we gathered input from patients to improve item content coverage and format as well as refined the measurement framework. This measurement framework informed the subsequent development of a calibrated psychosocial illness impact item bank that is part of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS; www.nihpromis.org) and beyond the scope of this paper. In future studies, we will expand the current item pool and calibrate illness impact item banks, using Item Response Theory (IRT) models. Although comprehensive, the item pool is too long to be administered in clinical research or practice. Yet, applications from an IRT-calibrated item bank such as dynamic computerized adaptive tests and static short-form measures can overcome this barrier by only selecting the most informative items targeting to the persons’ levels on the latent trait at the time of survey. These applications can help clinicians and researchers better understand patients’ cancer experiences longitudinally [61–65] and assist with the development of interventions to minimize negative and maximize positive psychosocial impacts of illness.
Fig. 4.
Mean comparisons across sub-groups for negative psychosocial impact (N-II) as well as its local factors (N-SEW self-concept/esteem/worth, N-SI Social Isolation, N-SR Stress response, N-MS Meaning & spirituality
Acknowledgments
This project was supported by the National Cancer Institute (CA60068, PI: David Cella). Special acknowledgements to Kelly Dineen, Ph.D. and Kimberly Davis, Ph.D. for their contributions to the item pool development used for the pilot study, and Jacquelyn George and Rachel Hanrahan for coordinating the study.
Appendix 1.
Table 4.
Positive illness impact: item descriptions, sub-domains (local factors) and factor loadings
| Item description | Sub-domain | Factor loading |
|
|---|---|---|---|
| General factor |
Local factor |
||
| PII1 My illness has helped me learn to handle difficult times | Self-concept/esteem/ worth |
0.863 | 0.168 |
| PII2 My illness has helped me discover I am stronger than I thought I was | 0.847 | 0.348 | |
| PII3 My illness has helped me become more comfortable with who I am | 0.835 | 0.045 | |
| PII4 My illness has helped me become a stronger person | 0.846 | 0.202 | |
| PII5 My illness has helped me feel better about my ability to handle problems | 0.856 | 0.258 | |
| PII6 My illness has given me confidence | 0.845 | 0.139 | |
| PII7 My illness has helped me be more confident in my ability to cope | 0.861 | 0.251 | |
| PII8 My illness has helped me see how strong I can be | 0.833 | 0.331 | |
| PII9 My illness has helped me become a better person | 0.875 | −0.051 | |
| PII10 My illness has helped me know who I can count on in times of trouble | Social connection | 0.69 | 0.432 |
| PII11 My illness has helped me have more compassion for others | 0.815 | 0.084 | |
| PII12 My illness has helped me learn to ask others for help | 0.654 | 0.49 | |
| PII13 My illness has helped relationships become more meaningful | 0.773 | 0.323 | |
| PII14 My illness has brought my family closer together | 0.695 | 0.526 | |
| PII15 My illness has made me more connected to my family | 0.687 | 0.544 | |
| PII16 My illness has led me to meet people who have become some of my best friends | 0.636 | 0.154 | |
| PII17 My illness has helped me become more aware of the love and support available from other people |
0.748 | 0.416 | |
| PII18 My illness has helped me realize who my real friends are | 0.727 | 0.356 | |
| PII19 My illness has helped me learn to receive help from others | 0.694 | 0.494 | |
| PII20 My illness has helped me appreciate people in my life more | 0.783 | 0.355 | |
| PII21 My illness has helped me become more willing to express my emotions | Coping | 0.827 | −0.051 |
| PII22 My illness has helped me accept the way things work out | 0.796 | 0.32 | |
| PII23 My illness has helped me learn to deal better with uncertainty | 0.85 | 0.165 | |
| PII24 My illness has helped me pursue new interests | 0.724 | −0.177 | |
| PII25 My illness has taught me how to adjust to things I cannot change | 0.776 | 0.307 | |
| PII26 My illness has helped me take things as they come | 0.794 | 0.369 | |
| PII27 My illness has taught me to be patient | 0.822 | 0.138 | |
| PII28 My illness has led me to deal better with stress and problems | 0.843 | 0.084 | |
| PII29 My illness has led me to be more accepting of things | 0.794 | 0.307 | |
| PII30 My illness has helped me be less easily bothered by little things | 0.803 | 0.172 | |
| PII31 My illness has helped me appreciate each day more fully | Meaning and spirituality |
0.835 | 0.013 |
| PII32 My illness has helped me establish a new path for my life | 0.794 | 0.129 | |
| PII33 My illness has helped me learn my life is more meaningful | 0.882 | 0.057 | |
| PII34 My illness has given me a greater appreciation for life | 0.842 | 0.053 | |
| PII35 My illness has helped me have a stronger faith | 0.673 | 0.685 | |
| PII36 My illness has helped my spiritual growth | 0.706 | 0.629 | |
| PII37 My illness has helped me develop a deeper sense of purpose in my life | 0.876 | 0.16 | |
| PII38 My illness has helped me feel peaceful | 0.831 | 0.092 | |
| PII39 My illness has helped me find comfort in my faith or spiritual beliefs | 0.671 | 0.679 | |
| PII40 My illness has helped me find strength in my faith or spiritual beliefs | 0.665 | 0.708 | |
| PII41 My illness has given me a sense of peace | 0.809 | 0.102 | |
| PII42 My illness has helped me feel closer to God | 0.638 | 0.72 | |
| PII43 My illness has helped me find strength in prayer | 0.61 | 0.727 | |
Appendix 2.
Table 5.
Negative illness impact: item descriptions, sub-domains (local factors), and factor loadings
| Item description | Sub-domain | Factor loading |
|
|---|---|---|---|
| General factor |
Local factor |
||
| NII1 Because of my illness, I feel that I am a failure | Self-concept/ esteem/worth |
0.776 | 0.428 |
| NII2 Because of my illness, I feel useless | 0.848 | 0.265 | |
| NII3 Because of my illness, I feel like less of a person | 0.841 | 0.298 | |
| NII4 Because of my illness, I feel people have lost respect for me | 0.734 | 0.249 | |
| NII5 Because of my illness, I feel worthless | 0.856 | 0.474 | |
| NII6 Because of my illness, I feel inferior to others | 0.785 | 0.35 | |
| NII7 Because of my illness, I am unhappy with my physical appearance | 0.737 | 0.026 | |
| NII8 Because of my illness, I do not have a lot of confidence | 0.779 | 0.271 | |
| NII9 Because of my illness, I have a negative attitude toward myself | 0.829 | 0.254 | |
| NII10 Because of my illness, I feel like I am a burden to my family | Social isolation | 0.833 | −0.247 |
| NII11 Because of my illness, I have trouble asking others for help | 0.724 | 0.114 | |
| NII12 Because of my illness, I have lost contact with some people | 0.728 | 0.507 | |
| NII13 Because of my illness, I feel isolated from others | 0.868 | 0.217 | |
| NII14 Because of my illness, I feel disconnected from others | 0.848 | 0.269 | |
| NII15 My illness makes me feel like a burden to others | 0.871 | −0.173 | |
| NII16 My illness has caused communication problems in my family | 0.737 | 0.305 | |
| NII17 Because of my illness, I am not as close to family/friends | 0.684 | 0.453 | |
| NII18 Because of my illness, I have fewer people to count on | 0.788 | 0.421 | |
| NII19 Because of my illness, I have lost some close relationships | 0.665 | 0.6 | |
| NII20 Because of my illness, some people have distanced themselves from me | 0.745 | 0.484 | |
| NII21 Because of my illness, I am worried about what will happen in the future | Stress response | 0.722 | 0.331 |
| NII22 Because of my illness, I find myself more easily bothered by little things | 0.69 | 0.048 | |
| NII23 Because of my illness, I have difficulty accepting that things are not always in my control | 0.741 | 0.146 | |
| NII24 My illness has interfered with my ability to enjoy life | 0.816 | 0.086 | |
| NII25 I have been upset about my illness | 0.745 | 0.332 | |
| NII26 I have thought about my illness when I did not mean to | 0.586 | 0.606 | |
| NII27 I have had trouble falling asleep or staying asleep, because of images or thoughts about my illness that come into my mind |
0.619 | 0.534 | |
| NII28 I have had waves of strong feelings about my illness | 0.618 | 0.622 | |
| NII29 Images about my illness have popped into my mind | 0.497 | 0.678 | |
| NII30 Any reminder has brought back feelings about my illness | 0.592 | 0.565 | |
| NII31 How often do you think about the possibility of your illness coming back | 0.575 | 0.537 | |
| NII32 How upsetting is the idea of your illness coming back | 0.591 | 0.421 | |
| NII33 How likely do you think it is that your illness will come back | 0.492 | 0.285 | |
| NII34 Because of my illness, my faith has weakened | Meaning and spirituality |
0.622 | 0.685 |
| NII35 Because of my illness, I feel I have been given more than I can take | 0.788 | 0.073 | |
| NII36 Because of my illness, I am losing my faith | 0.645 | 0.71 | |
| NII37 Because of my illness, I have trouble feeling peace of mind | 0.812 | 0.178 | |
| NII38 Because of my illness, my life lacks meaning | 0.891 | −0.096 | |
| NII39 My illness has weakened my spiritual beliefs | 0.611 | 0.749 | |
| NII40 My illness has interrupted my spiritual growth | 0.663 | 0.585 | |
| NII41 Because of my illness, my life does not have a purpose | 0.805 | −0.147 | |
| NII42 Because of my illness, I question the purpose of my life | 0.761 | −0.044 | |
| NII43 Because of my illness, I get less comfort from my faith or spiritual beliefs | 0.552 | 0.675 | |
| NII44 Because of my illness, I feel punished by God | 0.644 | 0.274 | |
| NII45 Because of my illness, I find it hard to pray | 0.646 | 0.663 | |
References
- 1.Charmaz K. Experiencing chronic illness. In: Albrecht GL, Fitzpatrick R, Susan SC, editors. Handbook of social studies in health and medicine. Sage; London, Thousand Oaks, Calif.: 2000. pp. 277–292. [Google Scholar]
- 2.Cordova MJ, et al. Frequency and correlates of post-traumatic-stress-disorder like symptoms after treatment for breast cancer. Journal of Consulting and Clinical Psychology. 1995;63:6–981. doi: 10.1037//0022-006x.63.6.981. [DOI] [PubMed] [Google Scholar]
- 3.Derogatis LR, et al. The prevalence of psychiatric disorders among cancer patients. The Journal of the American Medical Association. 1983;249(6):751–757. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 4.Kornblith AB. Psychosocial adaption of cancer survivors. In: Holland JC, editor. Psycho-oncology. Oxford University Press; New York, New York: 1998. pp. 223–254. [Google Scholar]
- 5.Moyer A, Salovey P. Psychosocial sequelae of breast cancer and its treatment. Annals of Behavioral Medicine. 1996;18:110–125. doi: 10.1007/BF02909583. [DOI] [PubMed] [Google Scholar]
- 6.Stanton AL, Collins CA, Sworowski LA. Adjustment to chronic illness: Theory and research. In: Baum A, Revenson TA, Singer J, editors. Handbook of health psychology. Lawrence Erlbaum Associates; Mahwah, N.J.: 2001. pp. 387–403. [Google Scholar]
- 7.Zabora J, et al. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 8.Hewitt M, et al. From cancer patient to cancer survivor: Lost in transition. National Academies Press; Washington, D.C.: 2006. [Google Scholar]
- 9.Adler NE, Page A, Institute of Medicine Committee on Psychosocial Services to Cancer Patients/Families in a Community . Cancer care for the whole patient: Meeting psychosocial health needs. National Academies Press; Washington, D.C.: 2008. [PubMed] [Google Scholar]
- 10.Reuben SH, et al. Living beyond cancer: Finding a new balance: President’s cancer panel 2003–2004 annual report. US Department of Health and Human Services; Washington, D.C.: 2004. [Google Scholar]
- 11.Affleck G, Tennen H. Construing benefits from adversity: adaptational significance and dispositional underpinnings. Journal of Personality. 1996;64(4):899–922. doi: 10.1111/j.1467-6494.1996.tb00948.x. [DOI] [PubMed] [Google Scholar]
- 12.Andrykowski MA, Brady MJ, Hunt JW. Positive psychosocial adjustment in potential bone marrow transplant recipients: Cancer as a psychosocial transition. Psycho-Oncology. 1993;2(261):276. [Google Scholar]
- 13.Antoni MH, Carver CS. Cognitive behavioral stress management intervention effects on benefit finding in breast cancer patients. Psychosocial and physiological correlates. Paper presented at the society of behavioral medicine, twenty-fourth annual meeting; Salt Lake City, UT. 2003. [Google Scholar]
- 14.Bellizzi KM. Expressions of generativity and post-traumatic growth in adult cancer survivors. The International Journal of Aging and Human Development. 2004;58(4):267–287. doi: 10.2190/DC07-CPVW-4UVE-5GK0. [DOI] [PubMed] [Google Scholar]
- 15.Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychology. 2006;25(1):47–56. doi: 10.1037/0278-6133.25.1.47. [DOI] [PubMed] [Google Scholar]
- 16.Cordova MJ, et al. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychology. 2001;20(3):176–185. [PubMed] [Google Scholar]
- 17.Park CL, Lechner SC. Measurement issues in assessing growth following stressful life experiences. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth: Research and practice. Lawrence Erlbaum Associates; Mahwah, N.J.: 2006. pp. 47–67. [Google Scholar]
- 18.Petrie KJ, et al. Positive effects of illness reported by myocardial infarction and breast cancer patients. Journal of Psychosomatic Research. 1999;47:537–543. doi: 10.1016/s0022-3999(99)00054-9. [DOI] [PubMed] [Google Scholar]
- 19.Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22(5):487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- 20.Taylor SE. Adjustment to Threatening Events: A Theory of Cognitive Adaptation. American Psychologist. 1983;38(11):1161–1173. [Google Scholar]
- 21.Tedeschi RG, Park CL, Calhoun LG. The LEA series in personality and clinical psychology. Lawrence Erlbaum Associates; Mahwah, N.J.: 1998. Post-traumatic growth: Positive change in the aftermath of crisis. [Google Scholar]
- 22.Tomich PL, Helgeson VS. Five years later: A cross-sectional comparison of breast cancer survivors with healthy women. Psycho-Oncology. 2002;11(2):154–169. doi: 10.1002/pon.570. [DOI] [PubMed] [Google Scholar]
- 23.Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology. 2004;23(1):16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- 24.Tedeschi RG, Calhoun LG. Trauma and transformation: Growing in the aftermath of suffering. Sage; Thousand Oaks, CA: 1995. [Google Scholar]
- 25.Bellizzi KM, et al. Positive and negative life changes experienced by survivors of non-Hodgkin’s lymphoma. Annals of Behavioral Medicine. 2007;34(2):188–199. doi: 10.1007/BF02872673. [DOI] [PubMed] [Google Scholar]
- 26.Bower JE, et al. Perceptions of positive meaning and vulnerability following breast cancer: Predictors and outcomes among long-term breast cancer survivors. Annals of Behavioral Medicine. 2005;29(3):236–245. doi: 10.1207/s15324796abm2903_10. [DOI] [PubMed] [Google Scholar]
- 27.Curbow B, et al. Loss and recovery themes of long-term survivors of bone marrow transplants. Journal of Psychosocial Oncology. 1993;10(4):1–13. [Google Scholar]
- 28.Curbow B, et al. Personal changes, dispositional optimism, and psychological adjustment to bone marrow transplantation. Journal of Behavioral Medicine. 1993;16(5):423–443. doi: 10.1007/BF00844815. [DOI] [PubMed] [Google Scholar]
- 29.Antoni MH, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 30.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 31.Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 32.McMillen JC, Fisher RH. The perceived benefit scales: Measuring perceived positive life changes after negative events. Social Work Research. 1998;22(3):173–187. [Google Scholar]
- 33.Park CL, Cohen LH, Murch RL. Assessment and prediction of stress-related growth. Journal of Personality. 1996;64(1):71–105. doi: 10.1111/j.1467-6494.1996.tb00815.x. [DOI] [PubMed] [Google Scholar]
- 34.Tedeschi RG, Calhoun LG. The post-traumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 35.Calhoun LG, Tedeschi RG. Receiving benefits in traumatic events: Some issues for practicing psychologists. The Journal of Training and Practice in Professional Psychology. 1991;5(1):45–52. [Google Scholar]
- 36.Zebrack BJ, et al. Assessing the impact of cancer: Development of a new instrument for long-term survivors. Psycho-Oncology. 2006;15(5):407–421. doi: 10.1002/pon.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zebrack BJ, et al. The impact of cancer and quality of life for long-term survivors. Psycho-Oncology. 2008;17(9):891–900. doi: 10.1002/pon.1300. [DOI] [PubMed] [Google Scholar]
- 38.Frazier P, et al. Correlates of levels and patterns of positive life changes following sexual assault. Journal of Consulting and Clinical Psychology. 2004;72(1):19–30. doi: 10.1037/0022-006X.72.1.19. [DOI] [PubMed] [Google Scholar]
- 39.Vardy J, et al. Assessing cognitive function in cancer patients. Supportive Care in Cancer. 2006;14(11):1111–1118. doi: 10.1007/s00520-006-0037-6. [DOI] [PubMed] [Google Scholar]
- 40.Lai JS, et al. Evaluating the dimensionality of perceived cognitive function. Journal of Pain and Symptom Management. 2009;37(6):982–995. doi: 10.1016/j.jpainsymman.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andrich D. A rating formulation for ordered response categories. Psychometrika. 1978;43:561–573. [Google Scholar]
- 42.Lai JS, Rosenbloom S, Cella D. Presented at ‘Advances in Health Outcomes Measurement: Exploring the Current State and the Future Applications of Item response Theory, Item Banks, and Computer-adaptive Testing’. Drug Information Association and National Cancer Institute; Bethesda, MD, U.S.A: Jun 23–25, 2004. Using Item Response Theory (IRT) to build illness impact item banks in cancer. sponsored by. [Google Scholar]
- 43.Lai JS, et al. Building core HRQL measures: Positive and negative psychological impact of cancer. Quality of Life Research. 2004;13(9):1503. [Google Scholar]
- 44.S. A. S. Institute Inc . SAS/STAT, Version 9.1. Cary; NC: 2003. [Google Scholar]
- 45.Kaiser HF. The application of electronic computers to factor analysis. Educational and Psychological Measurement. 1960;20:141–151. [Google Scholar]
- 46.Cattell RB. The screen test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 47.Hatcher L. A step-by-step approach to using the SAS system for factor analysis and structure equation modeling. SAS Institute Inc; Cary, NC: 1994. [Google Scholar]
- 48.Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 49.Chen FF, West SG, Sousa KH. A comparison of bifactor and second-order models of quality of life. Multivariate Behavioral Research. 2006;41(2):189–225. doi: 10.1207/s15327906mbr4102_5. [DOI] [PubMed] [Google Scholar]
- 50.Lai JS, Crane PK, Cella D. Factor analysis techniques for assessing sufficient unidimensionality of cancer related fatigue. Quality of Life Research. 2006;15(7):1179–1190. doi: 10.1007/s11136-006-0060-6. [DOI] [PubMed] [Google Scholar]
- 51.McDonald RP. Test theory: A unified treatment. Lawrence Earlbaum Associates, Inc; Mahwah, NJ: 1999. [Google Scholar]
- 52.Stanton AL, Snider PR. Coping with a breast cancer diagnosis: A prospective study. Health Psychology. 1993;12(1):16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- 53.Vinokur AD, et al. Physical and psychosocial functioning and adjustment to breast cancer: Long term follow-up of a screening population. Cancer. 1989;63(2):394–405. doi: 10.1002/1097-0142(19890115)63:2<394::aid-cncr2820630233>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 54.Stanton AL, et al. Promoting adjustment after treatment for cancer. Cancer. 2005;104(11 Suppl):2608–2613. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- 55.Cassileth BR, et al. Psychosocial status in chronic illness. A comparative analysis of six diagnostic groups. The New England Journal of Medicine. 1984;311(8):506–511. doi: 10.1056/NEJM198408233110805. [DOI] [PubMed] [Google Scholar]
- 56.Ganz PA, et al. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. Journal of Clinical Oncology. 1998;16(2):501–514. doi: 10.1200/JCO.1998.16.2.501. [DOI] [PubMed] [Google Scholar]
- 57.Fife BL. The conceptualization of meaning in illness. Social Science and Medicine. 1994;38(2):309–316. doi: 10.1016/0277-9536(94)90400-6. [DOI] [PubMed] [Google Scholar]
- 58.Langeveld NE, et al. Quality of life, self-esteem and worries in young adult survivors of childhood cancer. Psycho-Oncology. 2004;13(12):867–881. doi: 10.1002/pon.800. [DOI] [PubMed] [Google Scholar]
- 59.Taïeb O, et al. Posttraumatic stress symptoms after childhood cancer. European Child and Adolescent Psychiatry. 2003;12(6):255–264. doi: 10.1007/s00787-003-0352-0. [DOI] [PubMed] [Google Scholar]
- 60.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth: Research and practice. Lawrence Erlbaum Associates, Inc; Mahwah: 2006. pp. 138–175. [Google Scholar]
- 61.Soni MK, Cella D. Quality of life and symptom measures in oncology: An overview. The American Journal of Managed Care. 2002;8(18 Suppl):S560–S573. [PubMed] [Google Scholar]
- 62.Hahn EA, Cella D. Health outcomes assessment in vulnerable populations: Measurement challenges and recommendations. Archives of Physical Medicine and Rehabilitation. 2003;84(Suppl 2):S35–S42. doi: 10.1053/apmr.2003.50245. [DOI] [PubMed] [Google Scholar]
- 63.Cella D, Chang CH. A discussion of item response theory (IRT) and its applications in health status assessment. Medical Care. 2000;38(9 Suppl):1166–1172. doi: 10.1097/00005650-200009002-00010. [DOI] [PubMed] [Google Scholar]
- 64.Cella D, Chang CH, Heinemann AW. Item Response Theory (IRT): Applications in quality of life measurement, analysis, and interpretation. In: Mesbah M, Cole B, Lee MLT, editors. Statistical methods for quality of life studies: Design, measurements, and analysis. Kluwer Academic Publishers; Boston, MA: 2002. pp. 169–186. [Google Scholar]
- 65.Gershon R, et al. Item response theory and health-related quality of life in cancer. Expert Review of Pharmaco-economics & Outcomes Research. 2003;3(6):783–791. doi: 10.1586/14737167.3.6.783. [DOI] [PubMed] [Google Scholar]