Abstract
Objectives
Either dysphoria (sadness) or anhedonia (loss of interest in usually pleasurable activities) is required for a diagnosis of major depression. While major depression is a known risk factor for disability in older persons, few studies have examined the relationship between the 2 core symptoms of major depression and disability or mortality. Our objective was to examine the relationship between these two core symptoms and time to disability or death
Design
Longitudinal cohort study
Setting and Participants
We used the nationally representative Health and Retirement Study to examine this relationship in 11,353 persons over the age of 62 (mean = 74) followed for up to 13 years.
Measurements
Dysphoria and anhedonia were assessed with the Short Form Composite International Diagnostic Interview. Our outcome measure was time to either death or increased disability, defined as the new need for help in a basic activity of daily living. We adjusted for a validated disability risk index and other confounders.
Results
Compared to subjects without either dysphoria or anhedonia, the risk for disability or death was not elevated in elders with dysphoria without anhedonia (adjusted HR = 1.11, 95%CI = 0.91–1.36). The risk was elevated in those with anhedonia without dysphoria (HR = 1.30, 95%CI = 1.06–1.60) and those with both anhedonia and dysphoria (HR = 1.28, 95%CI = 1.13–1.46).
Conclusion
Our results highlight the need for clinicians to learn whether patients have lost interest in usually pleasurable activities, even if they deny sadness.
Keywords: Depression, anhedonia, activities of daily living, quality of life, health status
OBJECTIVE
Depression is a major source of suffering in older persons that markedly impairs quality of life1. Beyond its impact on quality of life, depression has consistently been shown to be a significant predictor of poor health outcomes in older persons, increasing the risk for disabilities that compromise the ability to live independently, as well as for death2–13.
The approach to depression diagnosis in the Diagnostic and Statistical Manual of Psychiatry (DSM-IV) requires the presence of at least 5 of 9 symptoms for a diagnosis of major depressive disorder14. However 2 of these symptoms, dysphoria and anhedonia, are core diagnostic requirements because a diagnosis of major depression cannot be made unless one of them is present. The importance of dysphoria and anhedonia is illustrated by the increasingly common use of screening tests in primary care that focus exclusively on these 2 symptoms15. Dysphoria, because it directly refers to feeling sad or blue, may best conform to what lay patients understand as depression. Anhedonia, which refers to a loss of interest in activities that are usually pleasurable, is probably less likely to be recognized by a lay patient as suggestive of a depressive disorder, and in an older patient may be inappropriately viewed as part of normal aging16.
While dysphoria and anhedonia are of equal importance in the DSM-IV diagnostic algorithm, it is not known if they are both important predictors of health outcomes. To address this issue, we compared the prognostic importance of dysphoria and anhedonia in a nationally representative sample of older persons who were administered a diagnostic interview for major depression. Specifically, we examined whether each symptom identified older persons who were at higher risk for developing new disabilities in the basic activities of daily living needed to live independently or death. This combined outcome of ADL disability or death is commonly used in the geriatric literature and often referred to as active life expectancy17. Active life expectancy is the amount of time an older patient will survive not dependent on caregivers for basic needs of daily living.
METHODS
Subjects
We used subjects enrolled in the Health and Retirement Study (HRS), an ongoing longitudinal study examining the changes in health and wealth with age.18,19 The current HRS represents the merger of several cohorts that represent various age ranges of the US population. This study leveraged the use of a lay-administered diagnostic interview that was given on a single occasion to participants in 3 of the HRS cohorts. We included subjects over the age of 62.
The HRS began with one cohort (original HRS) before merging additional cohorts. The original HRS, which started in 1992, was designed to be representative of persons between the ages 50–61. The depression interview was administered in 1996 and 1998. Of 3,559 HRS respondents who reached the age of 62 by 1996, 272 were not eligible because they had a surrogate respondent. Of the remaining eligible subjects, 129 did not complete an interview, leaving 3,158 study participants.
The second cohort was the Asset and Health Dynamics Among the Oldest Old study (AHEAD). The AHEAD was originated in 1993 and was representative of community-living elders over the age of 70. The depression interview was administered in 1995. Of the 6,900 AHEAD subjects interviewed in 1995, 871 were not eligible because they had a surrogate respondent. Of the remaining eligible subjects, 27 did not complete the depression interview, leaving a cohort of 6,002. In addition, 34 subjects belonging to the AHEAD study were interviewed in 1998, resulting in the final cohort of 6,036.
The third cohort was the Children of the Depression Age (CODA). CODA originated in 1998, and was representative of persons age 68 to 75. The depression interview was administered in 1998. Of the 2,303 CODA subjects, 129 were not eligible because they had a surrogate respondent. Of the remaining eligible subjects 15 did not complete the depression interview, leaving a final cohort of 2,159.
In total, 11,353 subjects over the age of 62 received the diagnostic interview and were eligible for this study.
Measures
Dysphoria and Anhedonia
Subjects were administered the Short Form Composite International Diagnostic Interview (CIDI-SF)20. The CIDI-SF used lay interviewers to approximate the DSM-IIIR criteria for major depression over the past year. The interview focuses on a detailed determination of whether at least one of the symptoms required for major depression, dysphoria or anhedonia, were of sufficient severity to meet diagnostic criteria. Once determining that either dysphoria or anhedonia are present, the interview then assesses whether other symptoms co-existed with dysphoria or anhedonia.
The CIDI-SF started with an assessment for dysphoria. First subjects were asked, “During the past 12 months, was there ever a time when you felt sad, blue, or depressed for two weeks or more in a row?” If subjects answered yes, they were then asked, “Please think of the two-week period during the past 12 months when these feelings were worst. During that time did the feelings of being sad, blue, or depressed usually last all day long, most of the day, about half the day, or less than half the day?” Subjects reporting half of the day or less were not considered to have severe enough dysphoria to meet diagnostic criteria. Subjects reporting dysphoria at least most of the day were then asked “During those two weeks, did you feel this way every day, almost every day, or less often than that?” Subjects reporting almost every day were classified as dysphoric, while those reporting less than half the day were classified as not dysphoric. Subjects who were dysphoric were then asked, “During those two weeks, did you lose interest in most things?” We classified subjects reporting “yes” as having dysphoria with anhedonia, and those reporting “no” as having dysphoria without anhedonia.
Subjects who did not have dysphoria were then administered a series of questions to determine if whether they had anhedonia over the past year. Similar to the question sequence for dysphoria, the anhedonia sequence required the presence of the symptom most of the day, nearly every day over a two week period. Subjects were first asked, “During the past 12 months, was there ever a time lasting two weeks or more when you lost interest in most things like hobbies, work, or activities that usually give you pleasure?” Subjects answering “yes” were then asked questions assessing whether anhedonia was present at least most of the day, almost every day over the two-week period. Subjects meeting these criteria were classified as having anhedonia without dysphoria. Subjects not meeting these criteria were classified as having neither dysphoria nor anhedonia.
It should be noted that the criteria for anhedonia differs in those with and without dysphoria. Among those with dysphoria, we can identify those who have co-existing anhedonia, but the criteria for pervasiveness are less stringent.
Outcome (Disability or Death)
Our primary outcome was the time to development of disability in at least one additional activity of daily living (ADL)21 or death. ADL are basic self-care activities that are essential to independent living. They were assessed by asking the subject if they needed the help of another person with one of six activities: walking across a room, getting dressed, taking a bath or shower, eating, getting in or out of bed, and using the toilet. Subjects whose baseline interview was in 1995 were asked about ADL outcomes in 1998, and every 2 years thereafter. All other subjects were asked about ADL outcomes every two years. If a subject was unable to be interviewed for a follow-up interview, information about ADL function was obtained from a family member. A subject was defined as having reached the disability outcome if they reported needing help on any ADL in which they were independent on the baseline interview. We combined this outcome with subjects who died. We did this because this combined outcome closely resembles the concept of active life expectancy, which is the amount of time an elder can expect to survive without the need for assistance without the need for help assistance from another person17. Of subjects reaching this outcome, 45% were classified based on interview evidence of disability, and 55% were classified based on death between interview waves.
In addition to measuring active life expectancy, there is also an important methodologic rationale for combining ADL disability and death into a single outcome measure. Since HRS only interviews subjects every two years, a substantial number of elders who die in HRS do not report disability in the interview that preceded their death. However, other longitudinal studies of elders suggest that the vast majority of older persons have a period of ADL disability before death22. Censoring subjects who die without reporting disability would result in significant bias because the most of these decedents would have reported ADL disability if the HRS interview had been obtained closer to death.
Confounders
We considered additional measures that were potential confounders of the relationship between depressed mood, anhedonia, and disability. Our primary measures were the components of a disability-prediction index we previously validated using the AHEAD portion of this cohort23. We used this index to adjust for the differences in baseline risk of developing disability. The index considered demographic characteristics, health habits, disease diagnoses, and functional status for inclusion. The final index had the following 9 items: age older than 80, diabetes, difficulty walking several blocks, difficulty bathing or dressing, need for help with personal finances, difficulty lifting 10 pounds, inability to name the vice president, history of falling, and low body mass index (BMI). Because this index did not consider gender, race, marital status, and measures of socioeconomic status (SES) for inclusion, we also adjusted for these variables.
Analysis
Demographics, SES and health characteristics at baseline were compared between four depression groups using chi-square test for categorical variables and ANOVA or Kruskal-Wallis tests for continuous variables.
To describe the time to development of disability in the 4 groups, we created Kaplan-Meier curves. To compare unadjusted and adjusted rates of the disability outcome, we use proportional hazards Cox models with delayed entry, which compared the group with just dysphoria, just anhedonia, and both anhedonia and dysphoria to the group with neither dysphoria nor anhedonia. Age at the time of disability or death was used as time scale, because in older populations age has a greater effect on the hazard than time since last interview. To adjust for possible confounders, we adjusted for the score on the disability risk index, as well as age, race, marital status, and total net worth.
Information on history of falls in the previous two years was not collected in 1996 interview, leading to a large amount of missing data for this variable. Since those values are considered to be missing at random, we used multiple imputation procedures to impute missing values for the covariates24.
We conducted an additional exploratory analysis to determine whether subjects with dysphoria or anhedonia who also met criteria for major depression were more likely to develop ADL disability or death. We defined major depression as reporting at least 4 of the 8 symptoms assessed by the CIDI-SF.
All reported analyses were weighted for the differential probability of selection and take into account the complex design of HRS. Statistical analyses were done by using Stata software, version 10.1 (StataCorp, College Station, TX), and SAS software, version 9.2 (SAS Institute, Cary, North Carolina). The use of imputation and the complex survey design of the HRS results in noninteger values for degrees of freedom for some of our analyses.
RESULTS
Characteristics of Subjects
The mean age of subjects was 74 and 59% were women (Table 1). 568 (5.0%) subjects met criteria for dysphoria during the prior year. Of these, 396 (70%) also reported anhedonia, while 1742 (30%) did not report anhedonia. Of the 10,785 subjects who did not report dysphoria 152 (1.4%) reported anhedonia. The Pearson correlation coefficient between dysphoria and anhedonia was 0.69 (z = 41.7, p<0.001)
Table 1.
Baseline Characteristics Subjects (N = 11,353)
| No Dysphoria, No Anhedonia (n = 10633) | Dysphoria without Anhedonia (n = 172) | Anhedonia without dysphoria (n = 152) | Dysphoria with Anhedonia (n = 396) | ||||
|---|---|---|---|---|---|---|---|
| Characteristic | N (%) | N (%) | N (%) | N (%) | Test Statistics (DF) | p-value | |
|
| |||||||
| Demographics | Age, mean ± SD | 73.5 ± 7.4 | 72.0 ± 7.5 | 72.5 ± 7.1 | 72.2 ± 7.1 | F(3,50) = 0.80 | <0.001 |
| Male | 4494 (41.9%) | 37 (21.2%) | 63 (39.2%) | 111 (27.0%) | Χ2 (3) = 57.7 | <0.001 | |
| Race | |||||||
| White | 8554 (86.3%) | 139 (85.1%) | 119 (85.3%) | 299 (82.6%) | |||
| Black | 1306 (8.2%) | 17 (7.1%) | 22 (8.5%) | 56 (9.3%) | Χ2 (6) = 7.9 | 0.245 | |
| Hispanic or Other | 772 (5.5%) | 16 (7.8%) | 11 (6.2%) | 41 (8.1%) | |||
| Married | 6552 (60.1%) | 93 (49.6%) | 83 (51.8%) | 166 (40.5%) | Χ2 (3) = 75.0 | <0.001 | |
|
| |||||||
| Socio-economic status | Education Less Than High School | 3519 (31.7%) | 58 (31.9%) | 62 (41.0%) | 186 (43.3%) | Χ2 (3) = 22.2 | <0.001 |
| Net Worth, median (IQR)* | 135K (48K–306K) |
122K (36K–253K) |
88K (20K–227K) |
55K (9K–195K) |
Χ2 (3) = 96.4 | <0.001 | |
|
| |||||||
| Comorbidities | Hypertension | 4934 (46.1%) | 76 (46.7%) | 83 (54.2%) | 228 (57.4%) | Χ2 (3) = 24.3 | <0.001 |
| Diabetes | 1466 (13.0%) | 21 (11.1%) | 29 (17.0%) | 87 (21.3%) | Χ2 (3) = 21.2 | <0.001 | |
| Cancer | 1313 (12.9%) | 20 (11.6%) | 21 (13.8%) | 46 (12.7%) | Χ2 (3) = 0.3 | 0.961 | |
| Chronic Lung Disease | 803 (7.9%) | 13 (7.7%) | 26 (17.1%) | 77 (18.7%) | Χ2 (3) = 55.9 | <0.001 | |
| Heart Condition | 2634 (25.7%) | 46 (27.3%) | 59 (39.5%) | 174 (43.2%) | Χ2 (3) = 63.5 | <0.001 | |
| Stroke | 787 (7.7%) | 20 (13.8%) | 15 (10.3%) | 56 (14.7%) | Χ2 (3) = 22.6 | <0.001 | |
|
| |||||||
| Other Health | Current Smoker | 1201 (10.8%) | 24 (13.6%) | 23 (12.7%) | 78 (18.9%) | Χ2 (3) = 28.3 | <0.001 |
| Currently Drinks Alcohol | 4928 (47.1%) | 66 (42.4%) | 63 (41.8%) | 131 (32.6%) | Χ2 (3) = 30.5 | <0.001 | |
| Body mass index mean ± sd | 26.0 ± 4.7 | 26.7 ± 4.8 | 26.4 ± 5.3 | 26.4 ± 5.7 | F(3,50) = 2.22 | 0.098 | |
| Vigorous Activity 3x/week | 4362 (40.6%) | 64 (36.5%) | 34 (22.5%) | 109 (27.7%) | Χ2 (3) = 44.4 | <0.001 | |
|
| |||||||
| ADL Function | Independent in all | 9965 (94.0%) | 157 (92.1%) | 121 (80.4%) | 326 (82.9%) | Χ2 (3) = 83.1 | <0.001 |
| Dependent in one or more | 638 (6.0%) | 15 (7.9%) | 30 (19.6%) | 69 (17.1%) | |||
IQR = Interquartile range
There were significant differences across the various symptom categories. Compared to those with neither dysphoria or anhedonia, women were more like to have dysphoria. There was no gender difference for anhedonia. Across most of the socioeconomic, disease, and functional status risk factors, subjects who had both dysphoria and anhedonia, and subjects with anhedonia without dysphoria had considerably worse risk profiles than subjects with neither dysphoria nor anhedonia. However, subjects with dysphoria without anhedonia were often more similar to the subjects with neither symptom.
Disabilty or Death
Overall, 6,537 (59%) subjects developed disability or death before the end of the follow-up period. Compared to subjects with neither dysphoria nor anhedonia, subjects with dysphoria and anhedonia (HR = 1.54, 95% CI 1.35–1.76) and subjects with anhedonia without dysphoria (HR 1.57, 95% CI 1.28–1.92) were more likely to develop new ADL disabilities or death. Subjects with dysphoria without anhedonia were not more likely to develop disability or death (HR 1.11, 95% CI 0.91–1.36) (Figure, Table 2).
Figure. Age of Increased Disability in Activities of Daily Living Disability or Death.
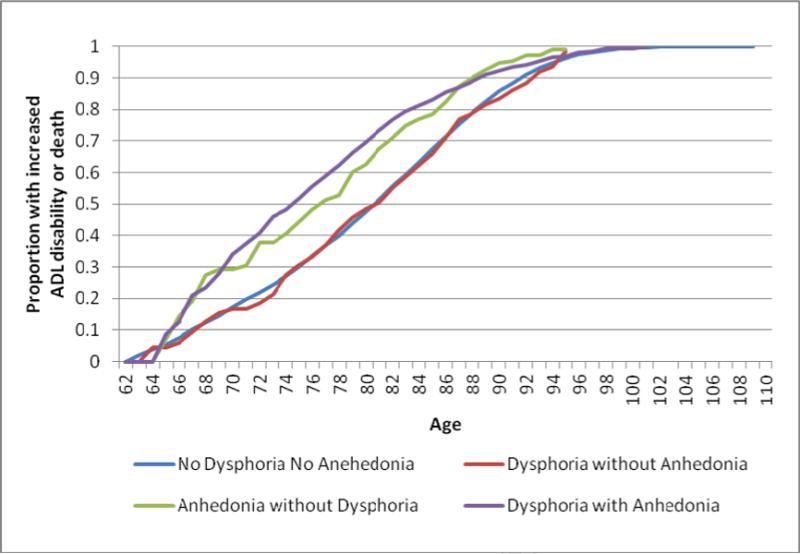
The figure describes age at the time of onset of increased disability or death for each of the symptom groups. The figure was created using a discrete hazard model with subject age as the time axis.
Table 2.
Risk of ADL Dependence or Death across Symptom Groups (N = 11,353)
| No Dysphoria No Anhedonia (n = 10633) | Dysphoria without Anhedonia (n = 172) | Anhedonia without dysphoria (n = 152) | Dysphoria with Anhedonia (n = 396) | ||
|---|---|---|---|---|---|
| Characteristic | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | Wald Statistics (DF) |
| Unadjusted | 1 | 1.11 (0.91, 1.36) |
1.57 (1.28, 1.92) |
1.54 (1.35, 1.76) |
F(3, 50.1) = 24.7 p<0.001 |
| Adjusted for Disability Risk Index | 1 | 1.06 (0.86, 1.30) |
1.31 (1.08, 1.60) |
1.27 (1.12, 1.44) |
F(3, 50.1) = 8.51 P<0.001 |
| Adjusted for Demographics (gender, race, marital status) | 1 | 1.15 (0.94, 1.41) |
1.54 (1.24, 1.92) |
1.54 (1.34, 1.77) |
F(3, 50.1) = 21.5 P<0.001 |
| Adjusted for Net Worth | 1 | 1.10 (0.90, 1.36) |
1.56 (1.27, 1.92) |
1.52 (1.33, 1.74) |
F(3, 50.1) = 22.4 P<0.001 |
| Adjusted for Disability Risk Index, Demographics and Net Worth | 1 | 1.11 (0.91, 1.36) |
1.30 (1.06, 1.60) |
1.28 (1.13, 1.46) |
F(3, 50.1) = 8.9 P<0.001 |
Degrees of Freedom adjusted for multiple imputation procedures (CITE Li)
After adjustment for the disability risk index, gender, race, marital status, and net worth reduced these associations, but they remained significant (Table 2). For subjects with both dysphoria and anhedonia, HR = 1.28, 95% CI 1.13–1.46. For subjects with anhedonia without dysphoria, HR = 1.30, 95% CI 1.06–1.60).
Results were similar when we restricted our outcome to death. Subjects with dysphoria and anhedonia (HR = 1.23, 95% CI = 1.07–1.42) and with anhedonia without dysphoria (HR = 1.33, 95% CI = 1.06–1.66) were at increased risk for death. Subjects with dysphoria, but not anhedonia were not at increased risk for death (HR = 1.05, 95% CI = 0.83–1.33) (F(3, 50.1) = 5.97, p = 0.002).
Among those with dysphoria or anhedonia, we did not find an increased risk of disability or death in those who also had major depression (Adjusted HR = 1.01, 95% CI 0.78–1.30, t (49) = 0.05, p = 0.958) for those with anhedonia and major depression, HR = 1.16, 95% CI 0.90–1.50, t(48) = 1.18, p = 0.238 for those with dysphoria and major depression).
CONCLUSIONS
Diagnostic criteria for a current diagnosis of major depression require a person to have pervasive symptoms of either dysphoria or anhedonia14. Using a nationally-representative cohort, we determined which subjects met diagnostic criteria for each of the symptoms during the past year and then assessed whether these symptoms placed subjects at higher risk for subsequent disability or death. We found that older persons without dysphoria but with anhedonia were at higher risk. However, we were not able to prove that persons with dysphoria without anhedonia were at higher risk. These results provide an empiric justification for the major depression diagnostic criteria that consider both anhedonia and dysphoria as part of the core diagnostic criteria, requiring one of these symptoms for a diagnosis.
Our results support the contention that a patient’s loss of interest in activities that usually give pleasure is a clinically important symptom that independently predicts a higher-risk disability or death. Our combined outcome of disability with basic ADLs or death is often referred to as active life expectancy because the need for help with basic ADLs usually signals the loss of an older person’s ability to live independently without assistance17. Because rates of this outcome are high in older persons, the adjusted risk of 30% conferred by anhedonia would translate into substantial increased risk of disability and death. This supports the contention made in many clinical texts suggesting anhedonia plays an increasingly important role in the presentation of late life depression25.
With advancing age, older persons in clinical settings may be less likely to endorse symptoms of dysphoria, making it particularly important for clinicians to also screen for anhedonia1,26,27.
However, if the popular view of depression is primarily linked to sadness or personal reports of “feeling depressed,” it is less likely persons with anhedonia will be identified. Further, if loss of interest in usual activities is identified, it may not routinely be recognized as a component of depressive illness. Public health efforts to improve recognition and treatment of depression need to consider approaches that help patients and clinicians view loss of interest in usual activities as a serious symptom in need of attention that is as much part of depression as sadness. These efforts may need to address the use of the clinical term “anhedonia” to describe this symptom. The use of a linguistically complex and obscure word to describe a clinical problem of such importance likely contributes to under-recognition by clinicians and patients.
There are several reasons anhedonia may identify adverse outcomes in older persons. Perhaps most important is that it identifies elders in whom depression has had a clinically important impact by leading to the discontinuation usual activities. Elders who have dysphoria without anhedonia may be better adapting to depression. Loss of interest in usual activities may lead to less physical activity and greater social isolation, both of which increase the risk for ADL disability12,28,29. Anhedonia may lead to a self-reinforcing cascade of events resulting in continually worsening depression and functioning.
There are also mechanistic reasons why anhedonia may confer a higher risk for disability or death. For example the vascular depression hypothesis suggests that late-life depression may be induced by atherosclerotic vascular disease in the brain30. Further, vascular disease may be more strongly correlated with anhedonia than dysphoria31. In addition, anhedonia may be a preclinical marker of dementia32,33. Therefore, anhedonia may be a stronger predictor of disability and death because it is marker for comorbid conditions associated with these outcomes.
Our study builds on an extensive literature demonstrating that depression, whether measured by a diagnostic algorithm or a screening symptom scale, is strongly associated with disability in older persons2–13. Further, several studies have shown that persons with high levels of depressive symptoms, but not meeting diagnostic criteria for major depression are at substantially increased risk for poor health outcomes1,26,27. Similar work has shown that subthreshold depression at levels below commonly used clinical thresholds is associated with functional limitations34,35. For example, Gallo showed that older persons without dysphoria, but with other complexes of depressive symptoms were at much higher risk of disability and death27. Our study adds to this literature with its focused comparison of anhedonia with dysphoria. To the best of our knowledge, this is the first population-based study to show that older persons without dysphoria but with anhedonia are at higher risk for disability or death.
Strengths of our study include a nationally-representative sample and a diagnostic algorithm for dysphoria and anhedonia. Our study also has several limitations. First, the CIDI algorithm for dysphoria and anhedonia is very restrictive. This resulted in a small number of cases, which limited our studies power despite its large sample size. Second, dysphoria and anhedonia were examined at one point in time and subjects were asked all about the symptoms over the past year. However, depression is an episodic illness with periods of recovery and remission1. Assessment at multiple time points or a longer time interval would have identified more cases. The likely inclusion of persons with a past history of dysphoria or anhedonia in the control subjects makes our risk estimates conservative. Finally, the CIDI interview only conducts a full assessment for anhedonia in those who do not meet criteria for dysphoria. In those who met criteria for dysphoria, much less restrictive criteria for anhedonia were applied. As a result, our study is not well-suited towards directly comparing the impact of dysphoria and anhedonia. Therefore, our study should not be interpreted as indicating that anhedonia is associated with worse outcomes than dysphoria.
In conclusion, this nationally-representative study demonstrates that persons without dysphoria but with anhedonia are at greater risk for disability or death. Our results highlight the need for clinicians to learn whether patients have lost interest in usually pleasurable activities, even if they deny sadness. In addition, public education efforts that equate loss of interest in pleasurable activities as part of depressive illness may be helpful.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest and Source of Funding: There are no conflicts of interest. Supported by Grants R01AG028481 and K24AG029812 from the National Institute on Aging. The Health and Retirement Study is funded by the National Institute on Aging.
References
- 1.Blazer DG. Depression in late life: review and commentary. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003;58(3):M249. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 2.Blazer DG, Hybels CF, Pieper CF. The association of depression and mortality in elderly persons: a case for multiple, independent pathways. J Gerontol A Biol Sci Med Sci Aug. 2001;56(8):M505–509. doi: 10.1093/gerona/56.8.m505. [DOI] [PubMed] [Google Scholar]
- 3.Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. Jama. 1990;264(19):2524–2528. [PubMed] [Google Scholar]
- 4.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry Spring. 2001;9(2):102–112. [PubMed] [Google Scholar]
- 5.Callahan CM, Kroenke K, Counsell SR, et al. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc Mar. 2005;53(3):367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 6.Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126(6):417–425. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE, Kahana E, Chin MH, Palmer RM, Fortinsky RH, Landefeld CS. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130(7):563–569. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 8.Covinsky KE, Yaffe K, Lindquist K, Cherkasova E, Yelin E, Blazer DG. Depressive symptoms in middle age and the development of later-life functional limitations: the long-term effect of depressive symptoms. J Am Geriatr Soc Mar. 2010;58(3):551–556. doi: 10.1111/j.1532-5415.2010.02723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cronin-Stubbs D, de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Arch Intern Med. 2000 Nov 13;160(20):3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- 10.Gurland B, Wilder DE, Berkman C. Depression and disability in the elderly: reciprocal relations and changes with age. International Journal of Geriatric Psychiatry. 1988;3:163–179. [Google Scholar]
- 11.Mehta KM, Yaffe K, Covinsky KE. Cognitive impairment, depressive symptoms, and functional decline in older people. J Am Geriatr Soc Jun. 2002;50(6):1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008 Nov 26;300(20):2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yaffe K, Edwards ER, Covinsky KE, Lui LY, Eng C. Depressive symptoms and risk of mortality in frail, community-living elderly persons. Am J Geriatr Psychiatry Sep–Oct. 2003;11(5):561–567. [PubMed] [Google Scholar]
- 14.Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Assoc; 1994. pp. 320–327. [Google Scholar]
- 15.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med Jul. 1997;12(7):439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarkisian CA, Hays RD, Berry SH, Mangione CM. Expectations regarding aging among older adults and physicians who care for older adults. Med Care Sep. 2001;39(9):1025–1036. doi: 10.1097/00005650-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Katz S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983 Nov 17;309(20):1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- 18.Health and Retirement Study Website. 2010 http://www.umich.edu/~hrswwwAccessed August 1, 2010.
- 19.Juster F, Suzman R. An overview of the health and retirement study. J Human Resources. 1995;30:S8–S56. [Google Scholar]
- 20.Kessler RC. The World Health Organization International Consortium in Psychiatric Epidemiology (ICPE): initial work and future directions — the NAPE Lecture 1998. Nordic Association for Psychiatric Epidemiology. Acta Psychiatr Scand Jan. 1999;99(1):2–9. doi: 10.1111/j.1600-0447.1999.tb05378.x. [DOI] [PubMed] [Google Scholar]
- 21.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standarized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 22.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. Jama. 2003 May 14;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 23.Covinsky KE, Hilton J, Lindquist K, Dudley RA. Development and validation of an index to predict activity of daily living dependence in community-dwelling elders. Med Care Feb. 2006;44(2):149–157. doi: 10.1097/01.mlr.0000196955.99704.64. [DOI] [PubMed] [Google Scholar]
- 24.Little R, Rubin D. Statistical Analysis with Missing Data. 2. Hoboken: Whiley-InterScience; 2002. [Google Scholar]
- 25.Koenig H, Blazer D. Depression, Anxiety, and other Mood Disorders. In: Cassl C, Leipzig R, Cohen H, Larson E, Meier D, editors. Geriatric Medicine: An evidence based approach. 4. New York: Springer; 2006. pp. 1163–1185. [Google Scholar]
- 26.Gallo JJ, Rabins PV, Anthony JC. Sadness in older persons: 13-year follow-up of a community sample in Baltimore, Maryland. Psychological Medicine. 1999;29(2):341–350. doi: 10.1017/s0033291798008083. [DOI] [PubMed] [Google Scholar]
- 27.Gallo JJ, Rabins PV, Lyketsos CG, Tien AY, Anthony JC. Depression without sadness: functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc May. 1997;45(5):570–578. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- 28.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med. 1992;117(12):1003–1009. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 29.Seeman TE, Bruce ML, McAvay GJ. Social network characteristics and onset of ADL disability: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci Jul. 1996;51(4):S191–200. doi: 10.1093/geronb/51b.4.s191. [DOI] [PubMed] [Google Scholar]
- 30.Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression’ hypothesis. Archives of general psychiatry. 1997;54(10):915. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- 31.Krishnan KR, Hays JC, Blazer DG. MRI-defined vascular depression. American Journal of Psychiatry. 1997;154(4):497. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- 32.Keedwell PA, Andrew C, Williams SCR, Brammer MJ, Phillips ML. The neural correlates of anhedonia in major depressive disorder. Biological Psychiatry. 2005;58(11):843–853. doi: 10.1016/j.biopsych.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 33.Lampe IK, Kahn RS, Heeren TJ. Apathy, anhedonia, and psychomotor retardation in elderly psychiatric patients and healthy elderly individuals. Journal of geriatric psychiatry and neurology. 2001;14(1):11. doi: 10.1177/089198870101400104. [DOI] [PubMed] [Google Scholar]
- 34.Hybels CF, Blazer DG, Pieper CF. Toward a threshold for subthreshold depression: an analysis of correlates of depression by severity of symptoms using data from an elderly community sample. Gerontologist Jun. 2001;41(3):357–365. doi: 10.1093/geront/41.3.357. [DOI] [PubMed] [Google Scholar]
- 35.Hybels CF, Pieper CF, Blazer DG. The complex relationship between depressive symptoms and functional limitations in community-dwelling older adults: the impact of subthreshold depression. Psychol Med Oct. 2009;39(10):1677–1688. doi: 10.1017/S0033291709005650. [DOI] [PMC free article] [PubMed] [Google Scholar]


