Abstract
Intimate relationships have received increasing attention as a context for HIV transmission. We examined the relationships among perceptions that condoms interfere with intimacy, gay-related stigma, and unprotected/ protected anal intercourse. Participants included 245 single-identified men who have sex with men. Intimacy Interference was positively associated with number of unprotected anal intercourse acts, and this effect was stronger among participants who reported high levels of gay-related stigma. In contrast, Intimacy Interference was negatively associated with number of protected anal intercourse acts, and gay-related stigma was positively associated with this outcome with no evidence of interaction effects. The findings are explained in the context of rejection sensitivity theory, and implications for public health and clinical intervention are discussed.
Keywords: HIV prevention, sexual orientation, sexual risk taking, stigma
Introduction
Despite rigorous risk reduction campaigns and relatively stable HIV transmission rates in the United States, generally, men who have sex with men (MSM) are disproportionally affected by the epidemic and face rising rates of transmission (CDC, 2012a, 2012b). HIV prevention efforts among MSM have largely focused on the promotion of condom use, with decisions around the use of condoms being understood from a theoretical perspective, which emphasizes the awareness of transmission risk and the effectiveness of condoms in preventing transmission (Ajzen, 1991; Catania et al., 1990; Fisher and Fisher, 1992; Golub et al., 2012; Kalichman et al., 2008; Prochaska et al., 1994a).
In the face of ongoing prevention challenges, researchers have begun to take a more complex view of decisions around condom use, incorporating psychological and interpersonal factors. One important psychological factor associated with sexual health and risk taking for gay and bisexual men is the experience of stigma associated with sexual minority status (Coker, 2010; Hamilton, 2009; Meyer, 2003; Preston, 2007; Ramirez-Valles, 2010; Safren, 2011). Several mechanisms may contribute to the association between gay-related stigma (GRS) and sexual risk taking. For example, GRS is associated with increased rates of substance use (Coker, 2010; Hatzenbuehler, 2009), which has been associated with increased sexual risk (New York City Department of Health and Mental Hygiene, 2010). Alternatively, individuals reporting higher levels of GRS are more likely to report psychological characteristics that influence sexual risk-taking decisions and/or reduce their ability to be assertive about safer sex practices, including anxiety, depression, and social isolation (Frost et al., 2007; Hatzenbuehler, 2009; Pachankis, 2007).
Recent work has suggested that the interpersonal context of condom use, specifically the impact of condom use on the perception of intimacy with or closeness to one’s partner, is also a critical factor. In qualitative studies, MSM report that the use of condoms communicates mistrust or distance (Blechner, 2002; Shernoff, 2005; Smith et al., 2008), and some describe the receipt of semen as an intimately erotic act (Schilder et al., 2008). Golub et al. (2012) found that the perception that condoms interfere with intimacy was associated with the nonuse of condoms above and beyond the perception that condoms reduce risk, and the perception that condoms reduce the physical pleasure of sexual activity.
In thinking about the relationship between perceptions that condoms interfere with intimacy and GRS, we drew upon rejection sensitivity theory (Downey and Feldman, 1996; Pachankis, 2007; Pachankis et al., 2008). The experience of stigma may have an isolating effect. GRS connotes the rejection of the gay, lesbian, or bisexual individual by heterosexual society. Pachankis (2007; Pachankis et al., 2008) found that a history of rejection due to sexual orientation resulted in adoption of affective, cognitive, and behavioral strategies intended to reduce the likelihood of future rejection. For individuals who believe that the use of condoms may increase the likelihood of rejection or connote distance from a sexual partner, the nonuse of condoms may represent a mechanism by which to reduce the likelihood of such rejection. Therefore, rejection sensitivity theory would predict that the co-occurrence of high levels of GRS and strong perceptions that condoms interfere with intimacy may result in particularly high levels of HIV transmission risk. To date, no empirical data are available addressing this combination of psychological vulnerabilities.
The purpose of the current study is to examine the interaction between perceptions that condoms interfere with intimacy and GRS in the prediction of unprotected anal intercourse (UAI) and protected anal intercourse (PAI) among MSM. We anticipate that both the perception that condoms interfere with intimacy and GRS will be positively correlated with UAI. Furthermore, we anticipate an interaction effect such that the combination of strong perceptions that condoms interfere with intimacy and high levels of GRS will be associated with particularly high levels of UAI. In order to understand sexual expression more generally, this study also examines an analogous model in which GRS and the perception that condoms interfere with intimacy predict PAI. We anticipate that GRS and the perception that condoms interfere with intimacy would be negatively associated with the number of PAI acts.
Methods
Participants and procedures
This article presents baseline data collected from MSM recruited in New York City for a randomized controlled trial testing the efficacy of a brief intervention designed to reduce substance use and sexual risk (Parsons et al., 2012a). Between September 2007 and September 2010, 315 participants completed a quantitative survey. Measures assessing attitudes toward condoms were assessed with reference to casual partners only; therefore, the analytic sample for the current study included only single-identified men (N = 245). To be eligible for the study, participants had to be men, at least 18 years of age, self-report a negative or unknown HIV serostatus, and report at least five instances of substance use (including cocaine, methamphetamine, gamma hydroxybutyrate, ecstasy, ketamine, or poppers), and at least one instance of UAI with a casual or serodiscordant main male partner in the last 3 months. Men completed baseline assessments consisting of psychosocial measures via audio computer-assisted self-interview (ACASI) software and an interviewer-administered time-line follow-back (TLFB) of recent (30-day) substance use and sexual behavior, as described in detail in the following. The Hunter College Institutional Review Board approved all procedures and measures in this study.
Men were recruited and screened actively inperson at local bars, clubs, bath-houses, and community events catering to gay men in the New York City area; actively online through websites and chat rooms catering to gay men or passively via recruitment cards, tear-off flyers, or posting ads on websites catering to gay men. Potential participants were then screened over the phone, provided additional information about the study, and scheduled for a baseline assessment. Study visits took place at the Center for HIV Educational Studies and Training. Participants were compensated US$40 for a 2-hour visit.
Measures
Demographic information
Participants reported their gender, race/ethnicity, age, education level, employment status, and sexual orientation.
Sexual behavior
Data related to sexual behavior were gathered as part of TLFB (Sobell and Sobell, 1996) interviews. Interviews covered the 30-day time period immediately preceding the assessment date. Participants were provided with a calendar. After indicating critical dates (birthdays, holidays, etc.), participants covered each day and indicated the number and type of anal sex acts that occurred. For each act, the participant also indicated whether a condom was used for the duration of the act. Composite scores were created representing the total number of receptive and insertive anal sex acts without a condom (UAI acts) and total number of receptive and insertive anal sex acts involving the use of condoms for protection (PAI acts) reported by each participant.
GRS
A modified version of the HIV stigma scale (Berger et al., 2001; Frost et al., 2007; Kelly et al., 2009) was used to evaluate participants’ level of GRS. Participants indicated their level of agreement with each item using a Likert-type scale from 1 (“strongly disagree”) to 4 (“strongly agree”). Example items included, “I have been hurt by how people reacted to learning I’m gay, bisexual, or transgendered.” and “People who know I’m gay, bisexual, or transgendered tend to ignore my good points.” Exploratory principal components analysis suggested that, as administered in the current sample, the 10 items constituted a single factor with high reliability (α = .93).
Intimacy Interference
The perception that condoms interfere with intimacy was assessed using the 4-item Intimacy Interference subscale of the Condom-Related Attitudes Scale (Golub et al., 2012). Two items (“How tempted would you be to have anal sex without a condom with a partner when you think he does not want to use a condom?” and “How tempted would you be to have anal sex without a condom with a partner when you really want to see or be with him again?”) were taken from a modified version of a measure of situational self-efficacy for safer sex (Grov et al., 2010; Redding and Rossi, 1999). Participants indicated the degree to which they would be tempted on a Likert-type scale from 1 (“not at all”) to 5 (“extremely). An additional two items (“having sex without a condom makes me feel more connected to my partner.” and “Not using a condom with a partner shows him that I trust him.”) were taken from the Decisional Balance for Unsafe Sex (Parsons et al, 2000; Prochaska et al., 1994b). Participants indicated how important each item was on a Likert-type scale from 1 (“not at all”) to 5 (“extremely”). The overall scale demonstrated adequate reliability (α= .73).
Data analysis
The number of sex acts constitutes a count variable. The use of ordinary least squares regression with such a variable may result in “inefficient, inconsistent, and biased estimates” of model parameters (Long, 1997: 217). Poisson and negative binomial models are appropriate for the prediction of count variables (Coxe et al., 2009; Long, 1997). Of these two, Poisson models are the more basic. They are predicated on the assumption that the mean of the Poisson distributed–dependent variables is equal to the variance. In the social sciences, many count variables have distributions with significant positive skew, resulting in overdispersion, wherein the variance exceeds the mean (Fridell et al., 2009). Negative binomial models are capable of modeling overdispersion and provide more accurate estimates of parameters in such cases (Coxe et al., 2009; Long, 1997). Both Poisson and negative binomial regressions use a log-link, in which the dependent variable is log-transformed. It is assumed that the predictors have a linear relationship to the log-transformed-dependent variable.
In the current analysis, separate Poisson regression models were tested predicting UAI and PAI. For both outcomes, there was evidence of significant overdispersion (deviance/df = 6.93 and 8.46, respectively). Subsequent analyses specified a negative binomial distribution for these outcomes with maximum likelihood estimation of the dispersion parameter. Coxe et al. (2009) asserted that the traditional approach for testing moderation, initially specified by Aiken and West (1991), can be utilized in Poisson and negative binomial regression models. Therefore, for each outcome, an initial model was tested containing only the main effects of Intimacy Interference and GRS. A second model was then calculated containing an additional interaction term.
Results
Sample demographics
Participants included a total of 245 HIV-negative MSM who identified their relationship status as single. Demographic data on participants are presented in Table 1. Participants ranged in age from 18 to 65 years (M = 29.04 years, standard deviation (SD) = 7.11 years). Participants were relatively well distributed across categories of race/ethnicity and education. Over half the sample (54.7%) reported an annual income of less than US$30,000.
Table 1.
Demographic characteristics.
| N | Percentage | |
|---|---|---|
| Overall | 245 | |
| Self-identified sexual orientation | ||
| Bisexual | 18 | 7.3 |
| Gay | 227 | 92.7 |
| Race | ||
| White | 100 | 40.8 |
| Non-White | 145 | 59.2 |
| Education | ||
| <4-year college degree | 133 | 54.3 |
| 4-year college degree or more | 112 | 45.7 |
| Income | ||
| <US$29,999 | 134 | 54.7 |
| >US$30,000 | 111 | 45.3 |
| M(SD) | Range | |
| Sexual behavior | ||
| Number of UAI acts | 4.43(7.24) | 0–41 |
| AI acts involving a condom | 3.43(4.38) | 0–29 |
| Intimacy Interference | 1.51(1.00) | 0–4 |
| Gay-related stigma | 1.80(0.68) | 1–4 |
UAI: unprotected anal intercourse; SD: standard deviation.
Table 2 displays the bivariate relationships among demographic variables and variables used in regression models. Outcome variables (number of UAI acts and number of PAI acts) were positively skewed count distributions, predictor variables (GRS and Intimacy Interference) were normally distributed, and all demographic variables were dichotomized. The number of UAI and PAI acts were unrelated to any demographic variables.
Table 2.
Correlations among demographic and model variables (N = 245).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Age | . | ||||||
| 2. Race | .15* | . | |||||
| 3. Education | .20** | .32** | . | ||||
| 4. Income | .33** | .35** | .40** | . | |||
| 5. GRS | −.04 | −.19 | −.18** | −.18** | . | ||
| 6. Intimacy Interference | −.01 | −.09 | −.07 | −.02 | .14** | . | |
| 7. UAI acts | −.01 | .04 | −.03 | .05 | .08 | .25** | . |
| 8. PAI acts | −.06 | −.04 | .03 | .08 | .13* | −.09 | .08 |
GRS: gay-related stigma; UAI: unprotected anal intercourse; PAI: protected anal intercourse.
Bivariate relationships were evaluated using phi coefficients (between dichotomous variables), rho coefficients (between dichotomous and normally distributed variables), Pearson’s correlations (between normally distributed variables), Kendall’s tau (between nonnormally distributed; normally and nonnormally distributed; and dichotomous and nonnormally distributed variables).
p < .05;
p < .01.
Results of regression models
Associations with UAI acts
Table 3 contains the parameter estimates for these models. The model containing only main effects accounted for a significant amount of variability in the number of UAI acts; however, parameter estimates suggested that only Intimacy Interference significantly predicted the outcome. The addition of the moderation term resulted in a significant improvement in model fit as evidenced by a significant increase in the model log-likelihood. Parameter estimates suggested that higher levels of Intimacy Interference are associated with an increased number of UAI acts and that this effect is increased with increasing levels of GRS.
Table 3.
Results of negative binomial regression models.
| Exp(B) | 95% CI | Exp(B) | 95% CI | |
|---|---|---|---|---|
| UAI acts | ||||
| Intercept | 4.03** | 3.45, 4.71 | 3.80** | 3.24, 4.46 |
| Intimacy | 1.49** | 1.26, 1.77 | 1.52** | 1.28, 1.80 |
| Interference | ||||
| Gay-related stigma | 1.14 | 0.90, 1.45 | 1.09 | 0.86, 1.38 |
| Interaction | 1.32* | 1.04, 1.67 | ||
| Likelihood ratio χ2step(2) = 30.22** | Likelihood ratio χ2step(1) = 5.66* | |||
| Likelihood ratio χ2model(3) = 35.88** | ||||
| Test of simple slopes for UAI acts | ||||
| High gay-related stigma | 2.30** | 1.92, 2.76 | ||
| Low gay-related stigma | 1.37** | 1.13, 1.66 | ||
| PAI acts | ||||
| Intercept | 3.22** | 2.74, 3.78 | 4.25** | 2.76, 3.83 |
| Intimacy | 0.76** | 0.64, 0.91 | 0.76** | 0.64, 0.81 |
| Interference | ||||
| Gay-related stigma | 1.56** | 1.22, 1.98 | 1.58** | 1.24, 2.02 |
| Interaction | 0.94 | 0.76, 1.16 | ||
| Likelihood ratio χ2step(2) = 17.63** | Likelihood ratio χ2step(1) = 0.34 | |||
| Likelihood ratio χ2model(3) = 17.97** | ||||
UAI: unprotected anal intercourse; PAI: protected anal intercourse; CI: confidence interval.
p < .05;
p < .01.
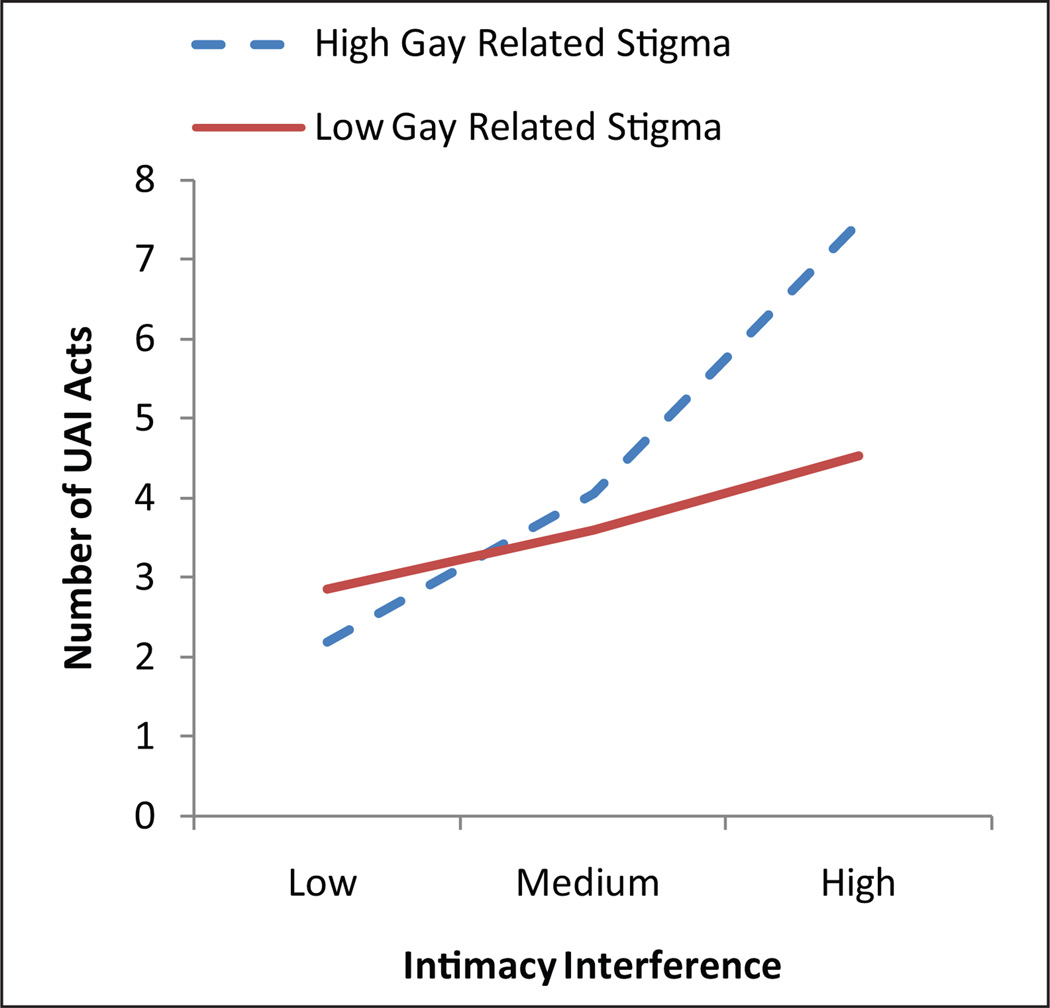
Tests of simple slopes
In order to gain a better understanding of the nature of the interaction effect, tests of simple slopes were conducted in a manner consistent with Aiken and West (1991). Values of high and low GRS were set at one SD above and below the mean. Values of Intimacy Interference were set at the mean (moderate), one SD below the mean (low), and one SD above the mean (high). While Intimacy Interference was significantly associated with increases in UAI at both low and high levels of GRS, the strength of this association was significantly greater at high levels of GRS (see Figure 1).
Figure 1. Number of UAI acts.
UAI: unprotected anal intercourse.
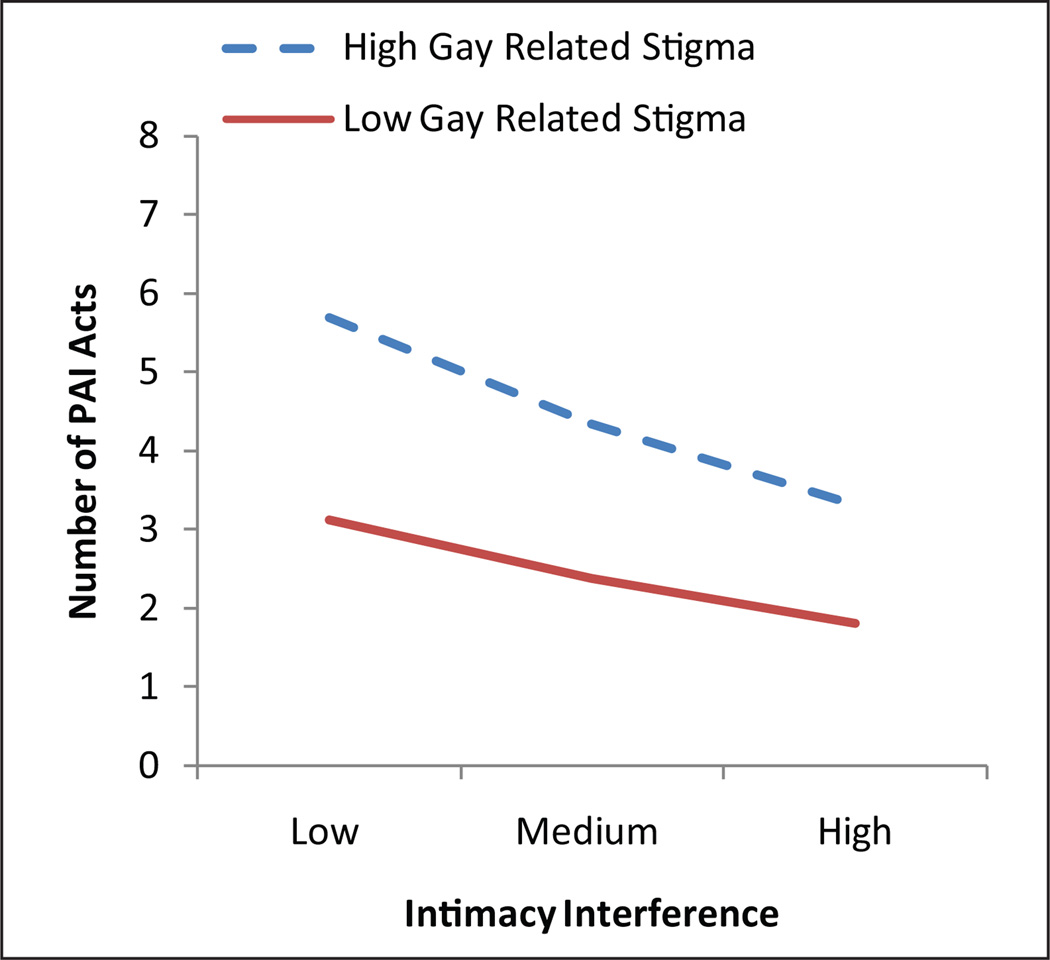
Associations with PAI acts
Table 3 contains the parameter estimates for these models. The model containing only main effects accounted for a significant amount of variability in the number of PAI acts. Parameter estimates suggested that both Intimacy Interference and GRS significantly predicted the outcome. Increasing levels of GRS were associated with a greater number of PAI acts. In contrast, increasing levels of Intimacy Interference were associated with a lower number of PAI acts. The interaction between Intimacy Interference and GRS was not significant (see Figure 2).
Figure 2. Number of PAI acts.
PAI: protected anal intercourse.
Discussion
The current study represents a meaningful extension in understanding the psychological context that frames condom-use behavior. Contrary to hypotheses, we did not observe a main effect of GRS on UAI; however, GRS enhanced the association between the perception that condoms reduce intimacy and UAI. This model is similar to Hamilton (2009) who found that group norms condoning sexual risk were associated with risk taking but only for individuals who experienced high levels of minority stress. These effects can be understood in terms of rejection sensitivity theory, which implies a possible process wherein an individual experiences stigma as a form of rejection (Downey and Feldman, 1996; Pachankis, 2007; Pachankis et al., 2008). Following such rejection, for those who believe that the nonuse of condoms communicates intimacy and enhances trust, the nonuse of condoms then becomes a behavioral mechanism for reducing future rejection. While conclusions about causality are limited due to the cross-sectional nature of these data, the pattern of associations suggests that the combination of stigma and the perception that condoms serve as a barrier to intimacy constitutes a psychological vulnerability strongly associated with UAI and supports the potential usefulness of rejection sensitivity theory in explaining these relationships.
These findings suggest that stigma and Intimacy Interference are associated not only with UAI but also with engagement in safer PAI. People who believe not using a condom enhances intimacy and connotes trust are not only having more UAI, they are having less PAI. In contrast, while stigma was associated with UAI only in the presence of the belief that condoms reduce intimacy, higher levels of stigma were associated with a higher number of PAI acts. This is perhaps best understood in the context of the metropolitan area in which these data were collected. The New York City metro provides substantial opportunity for men to access the gay community, which may weaken the direct link between stigma and risky sexual behavior (Ramirez-Valles, 2002, 2010). Alternatively, men who are more sexually active may be more publicly engaged in ways that increase potential exposure to, or awareness of, stigmatizing experiences.
These findings have implications for researchers interested in the impact of stigma on sexual health behaviors as well as HIV prevention efforts and clinical interventions with individual gay and bisexual men. They suggest that a full understanding of the influence of stigma on condom-use decisions requires information about the perceived relational implications of condom use. Specifically, prevention strategies among MSM may consider assessing perceptions that condoms reduce intimacy and testing the effects of relational strategies that enhance experiences of intimacy among male partners while maintaining sexual safety. In the context of clinical interventions, therapists should be sensitive to the fact that experiences of stigma may not be uniformly associated with risk. These data suggest that viewing the nonuse of condoms as a mechanism for communicating closeness constitutes a psychological vulnerability in combination with stigma.
These data are subject to several limitations. First, we examined only single-identified men. Main partner relationships have recently been identified as a major source of new HIV infections (Goodreau et al., 2012; Sullivan et al., 2009). Perceptions of relational implications of condom use may operate differently within main partner relationships. Future research should investigate the role of Intimacy Interference in sexual risk decisions among main partners. Such work would require the development of scales assessing the interpersonal significance of condom use between main partners. Such work should also take into account sexual agreements between partners, as recent work suggests such arrangements are meaningfully related to psychological functioning and sexual risk behavior (Hoff and Beougher, 2010; Parsons et al., 2013) despite the absence of associations with indicators of sexual relationship quality (Parsons et al., 2012b). Second, this study utilized data from self-identified HIV-negative men. MSM diagnosed with HIV face additional challenges in the form of HIV-associated stigma (Bunn et al., 2007; Derlega et al., 2010; Nyblade, 2006) and the negotiation of status disclosure to sexual partners (Bird and Voisin, 2011). The use of harm reduction strategies, such as serosorting (Golub et al., 2009) in lieu of condoms, may alter the salience of Intimacy Interference in meaningful ways. Future studies should investigate perceived relational implications of condom use among HIV-positive men.
Third, the Intimacy Interference scale was not originally designed specifically to measure this construct. It is possible that participants were subject to demand characteristics that introduced additional error variance and decreased scale reliability—and thereby the ability to detect meaningful associations with other constructs such as those demonstrated here. Finally, because of the nature of the study from which these data are drawn, participants are high-risk, active substance users living in an urban setting and may not generalize to other populations of MSM. However, this population is considered at highest risk for HIV infection (CDC, 2011a, 2012b) and can be argued to be those most in need of innovative intervention strategies.
The results of the current study offer valuable insights into the salience of relational variables in the negotiation of condom use. The association between perceptions that condoms interfere with intimacy and sexual risk taking was stronger among MSM who reported high levels of GRS, consistent with rejection sensitivity theory (Downey and Feldman,1996). The findings support previous research that the perception that condoms impede intimacy is a significant predictor of sexual risk (Golub et al., 2012). More research is necessary to understand the complex, relational process that is implicated in the decision to use condoms among MSM. However, the results of the current study suggest that addressing both experiences of stigma and the interpersonal meaning of condom use may represent an avenue for reducing the transmission of HIV.
Acknowledgements
The authors gratefully acknowledge Dr. Corina L. Weinberger, the Project Director, and the contributions of the Young Men’s Health Project team— Michael Adams, Anthony Bamonte, Kristi Gamarel, Christian Grov, Chris Hietikko, Catherine Holder, John Pachankis, Mark Pawson, Jonathan Rendina, Kevin Robin, Anthony Surace, Julia Tomassilli, Jaye Walker, Brooke Wells, and the CHEST recruitment team. We would also like to thank Richard Jenkins for his support of the project.
Funding
The Young Men’s Health Project was supported by a grant from the National Institute on Drug Abuse (NIDA) (R01-DA020366, Jeffrey T. Parsons, Principal Investigator).
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: SAGE; 1991. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:170–211. [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing & Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bird JDP, Voisin DR. A conceptual model of HIV disclosure in casual sexual encounters among men who have sex with men. Journal of Health Psychology. 2011;16(2):365–373. doi: 10.1177/1359105310379064. [DOI] [PubMed] [Google Scholar]
- Blechner MJ. Intimacy, pleasure, risk, and safety: Discussion of Cheuvront’s high-risk sexual behavior in the treatment of HIV-negative patients. Journal of Gay & Lesbian Psychotherapy. 2002;6(3):27–33. [Google Scholar]
- Bunn JY, Solomon SE, Miller C, et al. Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Education and Prevention. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. [Accessed 27 Oct 2011];Substance use and sexual health among men who have sex with men, injection drug users, and high-risk heterosexuals: Results from the national HIV behavioral surveillance study in New York City. 2010 http://www.nyc.gov/html/doh/downloads/pdf/dires/nhbs-sex-rsk-and-substance-use-jun2010.pdf.
- CDC. HIV among youth. 2011a Available at: http://www.cdc.gov/hiv/youth/pdf/youth.pdf.
- CDC. HIV and AIDS among gay and bisexual men. 2011b Available at: http://archives.jrn.columbia.edu/coveringed/nchhstp/newsroom/docs/FastFacts-MSM-FINAL508COMP.pdf.
- CDC. HIV in the United States: An overview. 2012a Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/pdf/HIV_overview_2012.pdf.
- CDC. New HIV infections in the United States. 2012b Available at: http://www.cdc.gov/nchhstp/newsroom/docs/2012/hiv-infections-2007-2010.pdf.
- Coker TR. The health and health care of lesbian, gay, and bisexual adolescents. Annual Review of Public Health. 2010;31(1):457–477. doi: 10.1146/annurev.publhealth.012809.103636. [DOI] [PubMed] [Google Scholar]
- Coxe S, West SG, Aiken LS. The analysis of count data: A gentle introduction to Poisson regression and its alternatives. Journal of Personality Assessment. 2009;91(2):121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- Derlega VJ, Winstead BA, Gamble KA, et al. Inmates with HIV, stigma, and disclosure decision-making. Journal of Health Psychology. 2010;15(2):258–268. doi: 10.1177/1359105309348806. [DOI] [PubMed] [Google Scholar]
- Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology. 1996;70:1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fridell L, Faggiani D, Taylor B, et al. The impact of agency context, policies, and practices on violence against police. Journal of Criminal Justice. 2009;37:542–552. [Google Scholar]
- Frost DM, Parsons JT, Nanín JE. Stigma, concealment and symptoms of depression as explanations for sexually transmitted infections among gay men. Journal of Health Psychology. 2007;12:636–640. doi: 10.1177/1359105307078170. [DOI] [PubMed] [Google Scholar]
- Golub SA, Starks TJ, Payton G, et al. The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS and Behavior. 2012;16(3):626–632. doi: 10.1007/s10461-011-9972-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Tomassilli JC, Parsons JT. Partner serostatus and disclosure stigma: Implications for physical and mental health outcomes among HIV-positive adults. AIDS and Behavior. 2009;13:1233–1240. doi: 10.1007/s10461-008-9466-1. [DOI] [PubMed] [Google Scholar]
- Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior. 2010;39(4):940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton CJ. Minority stress, masculinity, and social norms predicting gay men’s health risk behaviors. Journal of Counseling Psychology. 2009;56(1):132–141. [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CC, Beougher SC. Sexual agreements among gay male couples. Archives of Sexual Behavior. 2010;39:774–787. doi: 10.1007/s10508-008-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Picciano JF, Roffman RA. Motivation to reduce HIV risk behaviors in the context of the Information, Motivation, and Behavioral Skills (IMB) model of HIV prevention. Journal of Health Psychology. 2008;13:680–689. doi: 10.1177/1359105307082456. [DOI] [PubMed] [Google Scholar]
- Kelly BC, Bimbi DS, Izienicki H, et al. Stress and coping among HIV-positive barebackers. AIDS and Behavior. 2009;13(4):792–797. doi: 10.1007/s10461-009-9586-2. [DOI] [PubMed] [Google Scholar]
- Long JS. Regression Models for Categorical and Limited Dependent Variables. Vol. 7. Thousand Oaks, CA: SAGE; 1997. [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade LC. Measuring HIV stigma: Existing knowledge and gaps. Psychology, Health & Medicine. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Pachankis JE. The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychological Bulletin. 2007;133(2):328–345. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Goldfried MR, Ramrattan ME. Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. Journal of Consulting and Clinical Psychology. 2008;76(2):306–317. doi: 10.1037/0022-006X.76.2.306. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Bimbi DS, et al. Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. Journal of Adolescence. 2000;23:377–397. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, et al. Predictors of day-level sexual risk for young gay and bisexual men. AIDS and Behavior. 2012a doi: 10.1007/s10461-012-0206-1. Epub ahead of print 22 May 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Starks TJ, Dubois S, et al. Alternatives to monogamy among gay male couples in a community survey: Implications for mental health and sexual risk. Archives of Sexual Behavior. 2013;42(2):303–312. doi: 10.1007/s10508-011-9885-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Starks TJ, Gamarel KE, et al. (Non)monogamy and sexual relationship quality among same-sex male couples. Journal of Family Psychology. 2012b;26(5):669–677. doi: 10.1037/a0029561. [DOI] [PubMed] [Google Scholar]
- Preston DB. The relationship of stigma to the sexual risk behavior of rural men who have sex with men. AIDS Education and Prevention. 2007;19(3):218–230. doi: 10.1521/aeap.2007.19.3.218. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Harlow LL, et al. The transtheoretical model of change and HIV prevention: A review. Health Education & Behavior. 1994a;21(4):471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994b;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J. The protective effects of community involvement for HIV risk behavior: A conceptual framework. Health Education Research. 2002;17(4):389–403. doi: 10.1093/her/17.4.389. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J. Social integration and health: Community involvement, stigmatized identities, and sexual risk in Latino sexual minorities. Journal of Health and Social Behavior. 2010;51(1):30–47. doi: 10.1177/0022146509361176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redding CA, Rossi JS. Testing a model of situational self-efficacy for safer sex among college students: Stage of change and gender-based differences. Psychology and Health. 1999;14(3):467–486. [Google Scholar]
- Safren SA. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior. 2011;15(Suppl. 1):30–34. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilder AJ, Orchard TR, Bruchner CS, et al. It’s like the treasure: Beliefs associated with semen among young HIV-positive and HIV-negative gay men. Culture, Health & Sexuality. 2008;10(7):667–679. doi: 10.1080/13691050802183899. [DOI] [PubMed] [Google Scholar]
- Shernoff M. Condomless sex: Considerations for psychotherapy with individual gay men and male couples having unsafe sex. Journal of Gay & Lesbian Psychotherapy. 2005;9(3):149–169. [Google Scholar]
- Smith MD, Grov C, Seal DW. Agency-based male sex work: A descriptive focus on physical, personal, and social space. The Journal of Men’s Studies. 2008;16(2):193–210. doi: 10.3149/jms.1602.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: User’s Guide. Toronto, ON, Canada: Alcohol Research Foundation; 1996. [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]