Abstract
Individual cognitive-behavioral therapy (CBT) provides anxious youth with skills and experiences to increase “brave” behavior in the face of feared situations. This study addresses whether parental encouragement of bravery during an anxiety provoking and potentially avoidable naturalistic speech task (a) differs between parents of youth (ages 9–13) with anxiety disorders (N=47) and parents of healthy non-anxious controls (N=20); (b) influences response to treatment; and (c) changes during treatment for anxious youth randomized to receive CBT (N=30) or Child-Centered Therapy (CCT; a non-directive active comparison treatment; N=17). Parent-child dyads were videotaped during a discussion of whether or not the child should complete an optional speech task. Parents of anxious youth showed less encouragement of bravery than parents of controls. Encouragement of bravery increased from pre- to post-treatment for youth who received CBT but not CCT, and pre-treatment encouragement of bravery predicted a better response to treatment, particularly for youth receiving CBT.
Keywords: child anxiety, avoidance, approach, cognitive behavioral therapy, parenting, parent-child interaction
Cognitive-behavioral therapy (CBT) has consistently been shown to be an efficacious intervention for child anxiety (James, Soler, & Weatherall, 2005; Walkup, et al., 2008). Both family-focused (FCBT) and individual child-focused (ICBT) approaches have received empirical support (e.g., Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008), with little evidence of superiority of one approach over the other (for reviews see Barmish & Kendall, 2005; In-Albon & Schneider, 2007; Reynolds, Wilson, Austin, & Hooper, 2012). CBT interventions teach children skills for identifying and managing anxious affect and provide them with opportunities to practice these skills during in vivo exposures to feared situations. The extent to which parents encourage anxious children to approach anxiety-provoking situations outside of the clinic may be an important factor in treatment success, or a target for intervention and/or prevention approaches.
Parental support of brave behavior, defined in the present study as encouragement of approach behavior in the context of potential threat, has not been investigated as a potential factor in child anxiety treatment. This is surprising given that children with anxiety disorders often avoid situations that make them feel threatened and that could potentially increase their anxiety (Rapee, 2002). Anxious youth tend to be hyper-vigilant for threatening stimuli in the environment and often interpret ambiguous stimuli as threatening (Barrett, Rapee, Dadds, & Ryan, 1996; Dalgleish, et al., 2003; Taghavi, Moradi, Neshat-Doost, Yule, & Dalgleish, 2000). Furthermore, anxious children report lower levels of perceived self-efficacy in coping with anxiety-provoking situations (Kortlander, Kendall, & Panichelli-Mindel, 1997; Suveg & Zeman, 2004) and parents also report lower expectations of anxious children’s ability to cope with anxiety (Cobham, Dadds, & Spence, 1999; Kortlander, et al., 1997). It is possible that negative expectations among parents of anxious youth keep them from encouraging their children to complete tasks that they think will be too difficult for the youth to manage. Research using hypothetical vignettes has revealed that anxious children are more likely to nominate avoidant responses to ambiguous situations after discussing these situations with their families (Barrett, et al., 1996), suggesting that parenting behaviors may reinforce avoidance or fail to encourage bravery in anxious youth. However, this phenomenon has not been investigated using naturalistic or real-world anxiety-provoking stimuli.
In addition to contributing to the development of child anxiety, failure to encourage brave behavior could also interfere with successful treatment. In particular, support of brave behavior is theorized to play a role in facilitating out-of-session exposure tasks and the transfer of skills learned in the clinic to the child’s everyday world (Silverman & Kurtines, 1996). This “transfer of control” process involves a gradual shifting of knowledge and skills for managing anxiety from therapist to parent to child (Khanna & Kendall, 2009; Silverman & Kurtines, 1996). Khanna and Kendall (2009) found that therapists’ use of transfer of control strategies was associated with better post-treatment global functioing in FCBT. Khanna and Kendall (2009) also reported that therapists frequently used transfer of control strategies in communications with parents during the course of ICBT (although at a lower rate than FCBT). Parental support of brave behavior may therefore influence the success of the transfer of control process in ICBT, as well as FCBT.
Existing studies have not investigated the role of parental support of bravery in treatment response, but have yielded general support for the importance of family dynamics in response to family-based CBT. Studies relying on self or parent-report data have shown that lower family cohesion (Victor, Bernat, Bernstein, & Layne, 2007), higher family conflict (Crawford & Manassis, 2001), and higher parental rejection (Liber, et al., 2008) were associated with poorer response to FCBT. Two studies have used observational data to identify more specific parenting behaviors that may be associated with treatment response to FCBT. Wood, McLeod, Piacentini, and Sigman (2009) found that parental intrusiveness was a partial mediator of poorer treatment response to FCBT for early adolescents only. Creswell, Willetts, Murray, Singhal, and Cooper (2008) found that greater parental fearful expressions during children’s completion of a speech task were associated with poorer treatment response. This finding suggests that when parents convey anxiety to their children during a threatening situation, children do not do as well in treatment, providing potential support for our hypothesis that parental support of bravery will influence treatment response. However, there remains little data about parenting behaviors that interfere with or facilitate successful treatment response for youth engaged in ICBT. Although children are treated individually for approximately one hour per week in ICBT, they spend a great deal of time outside of the clinic with their parents, thus, parental behaviors have strong potential to exert influence over the ways in which they practice and incorporate skills learned in treatment into their everyday life.
There is also little information about how anxiety-related parenting behaviors change as a function of treatment, and existing data comes primarily from questionnaire measures. For example, Crawford and Manassis (2001) found decreases in mother and father reports of frustration with their child’s behaviors in FCBT. The extent to which parenting behaviors can be expected to change in ICBT is unclear. On the one hand, parents are not treated as co-clients and the majority of treatment time is spent one-on-one with the child. On the other hand, most individual child CBT approaches, such as the Coping Cat program used in the current study (Kendall & Hedtke, 2006a), do include some parental involvement (i.e., 2 parent sessions) as well as parental collaboration and consultation in exposure planning and homework. CBT may elicit change in parenting directly through this parent involvement in treatment. Additionally, over the course of therapy, parents may begin to modify their behavior in response to changes in their child’s responses to fear-provoking situations. For example, a parent may reduce protective behaviors after watching the child succeed at trying something “scary” on his/her own.” One study examined changes in child-reported family factors in both ICBT and FCBT (Silverman, Kurtines, Jaccard, & Pina, 2009). Results suggested that both ICBT and FCBT were associated with changes in children’s appraisals of positive and negative parenting behaviors, and these changes were associated with improvement in children’s anxious symptoms. These findings support the idea that parenting may change even in individual CBT, potentially as a function of change in children’s anxious behaviors. However, there is a need for direct observations of parenting behavior, which could provide more ecologically valid and objective information about specific parenting behaviors that may change over the course of treatment.
The present study utilized observational data on parenting during a naturalistic optional speech paradigm that was avoidable and potentially anxiety-provoking. We examined whether parents encouraged youth to approach this potentially avoidable anxiety-provoking scenario, and how differences in parental encouragement of bravery in response to this anxiety-provoking situation changed across treatment and related to treatment response. We hypothesized that parents of anxious youth, compared to parents of healthy controls, would be less likely to encourage bravery during the task. We also hypothesized that among the anxious youth, those whose parents were more encouraging of bravery would be most likely to respond positively to treatment. We further hypothesized that parental encouragement of bravery would increase over time with treatment.
Finally, by including a sample of youth treated with a comparison supportive therapy, we explored whether changes in parental encouragement of bravery across treatment and associations between encouragement of bravery and youths’ treatment response were specific to CBT or related to more general mechanisms of recovery. Recent clinical trials of child anxiety treatment have suggested that supportive and/or educational psychotherapies may be beneficial in treating anxiety symptoms for some children (Last, Hansen, & Franco, 1998; Silverman, et al., 1999), although other studies have shown greater effectiveness for CBT (Beidel, Turner, & Morris, 2000; Cohen, Deblinger, Mannarino, & Steer, 2004). It is critical to understand whether change in relevant parenting behaviors is specific to CBT or associated with non-specific aspects of therapy (e.g. attention, support). Because encouraging youth to overcome avoidance with brave approach-behavior is an explicit goal of CBT but not CCT, we expected change in parental encouragement of bravery in CBT but not CCT. Similarly, we expected parental encouragement of bravery to be more strongly associated with treatment response in CBT compared to CCT.
Method
Participants
Participants were 47 anxious youth (ANX) who were participating in a treatment study and 20 healthy controls (CON) with no history of mental health diagnoses. All youth participated in the study with a primary caregiver, defined as the individual who spent the most time in caregiving activities (63 mothers, 2 fathers, 1 grandmother, 1 step-mother; hereafter referred to as “parent” for simplicity). Youth (52% female) ranged in age from 9–13 years (M = 10.49, SD = 1.26). Participants were 88% Caucasian, 8% African-American, 1% Hispanic, and 3% Biracial. Anxious youth and healthy controls did not differ in age (F = .13, p = .718), gender (χ2 = .41, p = .437), race (χ2 = 5.46, p = .141), or family income (F = .05, p = .833). Healthy and anxious participants were recruited from the community through radio, television, and newspaper advertisements, and other University research studies. Anxious youth were also referred from pediatricians, school counselors, and University mental health clinics. Anxious youth were required to meet DSM-IV (American Psychiatric Association, 1994) criteria for current generalized anxiety disorder (GAD; N = 34), separation anxiety disorder (SAD; N = 12), and/or social phobia (SP; N = 10). Exclusion criteria for all participants included an IQ below 70 as assessed by the Wechsler Abbreviated Scale of Intelligence (Psychological Corporation, 1999), use of ongoing treatment with psychoactive medications, acute suicidality or risk for harm to self or others, and, because the larger study included a functional magnetic resonance imaging (fMRI) scan, presence of metal braces or other metal objects in their body. Specific exclusion criteria for healthy comparison youth included any current or lifetime DSM-IV diagnosis and having a parent with a current or lifetime DSM-IV diagnosis of an anxiety or mood disorder. Specific exclusion criteria for anxious participants included a current primary diagnosis of major depressive disorder (MDD), a current diagnosis of obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), conduct disorder, substance abuse or dependence, and ADHD combined type or predominantly hyperactive-impulsive type. Anxious youth were also excluded if they had a lifetime diagnosis of autism or Asperger’s syndrome, bipolar disorder, psychotic depression, schizophrenia, or schizoaffective disorder.
Procedures
Study procedures were approved by the University’s Institutional Review Board. Parents completed a brief phone screen and were scheduled for an intake assessment during which an independent evaluator administered a structured diagnostic interview to the child and his/her primary caregivers to confirm the diagnosis. Following the intake assessment, families of healthy youth and controls completed a baseline assessment that included behavioral observation tasks with the child and his or her primary caregiver. Anxious youth were randomized to 16 sessions of individual CBT (Kendall, 1994; Kendall, et al., 1997) or Child Centered Therapy (Cohen, et al., 2004), a non-directive active comparison therapy that was used to control for nonspecific components of treatment (e.g. attention and support). Restricted randomization was used to balance participants across conditions by age and gender, with a 2:1 ratio for assignment to CBT vs. CCT. Thirty were randomized to CBT and 17 were randomized to CCT. Following session 16, anxious youth completed a post-treatment assessment that included re-administration of behavioral observation tasks and psychiatric interviews. Although healthy controls also completed a 16 week assessement, only pre-treatment observational data were available for healthy controls (since we did not anticipate change in parenting over 16 weeks in healthy non-treated youth). As a result of occasional missed sessions, anxious youth completed between 13 and 16 sessions of treatment (M=15.85, SD = .55). One youth did not complete the post-treatment psychiatric interview, thus treatment response data were only available for 46 anxious youth. Both healthy youth and controls were compensated for completing assessments.
Treatment was delivered by M.A. and doctoral level therapists. Both protocols followed manuals and included 14 sessions with the child and 2 parent sessions, as well as parental consultation throughout treatment. Therapists for both treatments were trained by experts in each protocol (PCK and AM), and participated in weekly supervision with expert therapists. Additionally, 20% of tapes were checked for treatment integrity and fidelity by the expert therapists throughout the study.
CBT treatment
CBT was delivered using the Coping Cat therapist manual (Kendall & Hedtke, 2006a) and child workbook (Kendall & Hedtke, 2006b). The first 8 sessions focused on anxiety-management skills such as identifying somatic cues of anxious arousal, identifying anxious “self-talk” and replacing it with coping “self-talk,” problem solving to cope with the anxiety-provoking situation, and using self-evaluation and self-reward. Behavioral techniques such as progressive muscle relaxation, coping modeling, and role play are emphasized. In the final 8 sessions, the therapist guides the child through a hierarchy of exposure tasks to increasingly anxiety-provoking situations. Throughout the program, children are encouraged to practice techniques at home through homework assignments. Sessions 4 and 9 are held with parents. During these sessions, therapists introduce parents to the CBT model and obtain information from parents about primary concerns and goals. Parents are not treated as co-clients, but are consultants to the child’s treatment and are asked to provide some collaboration and assistance in exposure planning and homework.
CCT treatment
Child-Centered Therapy (CCT; Cohen, et al., 2004; Cohen, Mannarino, & Knudsen, 2005) is a manualized nondirective, supportive psychotherapy based in humanistic approaches. CCT is founded on principles such as unconditional positive regard, empathy, and therapist genuineness. The techniques employed in CCT include acceptance responses, reflection, and nondirective problem-solving. The basic rationale for this treatment is that improvement in anxiety symptoms will occur through the child’s experience of unconditional positive regard in an empathic and supportive therapeutic relationship. CCT was developed to be analogous to typical supportive psychotherapy that anxious children and adolescents receive in the community. Cohen et al. (2004) found that although CBT was more effective than CCT in the treatment of children with PTSD, CCT was also associated with a significant decrease in PTSD symptoms at post-treatment. Child and parent satisfaction with treatment have been shown to be equivalent for CCT and CBT treatment (Cohen & Mannarino, 1998). As the original CCT manual (Cohen, et al., 2004) focused on anxious youth with PTSD, we adapted the manual to be suitable for youth with GAD, SAD, and/or SP.
Structured diagnostic interviews
On their first visit to the lab, each youth and his or her parent(s) were interviewed to determine the youth’s mental health history using the Schedule for Affective Disorders and Schizophrenia in School-Age Children—Present and Lifetime version (K-SADS-PL, Kaufman, Birmaher, Brent, & Rao, 1997). Parents and youth were interviewed separately, with Independent Evaluators (IE’s) integrating data from both informants to arrive at a final diagnosis. All interviews were carried out by trained BA- and MA-level IE’s. The results of the interview were presented at a consensus case conference with a child psychiatrist, who reviewed the findings and preliminary diagnosis and provided a final diagnosis based on DSM-IV (American Psychiatric Association, 1994) criteria. Inter-rater reliability was calculated for approximately 20% of interviews for all IE-rated measures. Reliability for anxiety diagnoses was high (kappa = .89).
Clinical Global Impression-Improvement Scale
Categorical response to treatment was assessed using post-treatment IE ratings on the Clinical Global Impression-Improvement Scale (CGI-I; Guy, 1976). The CGI-I yields a global rating of clinical improvement ranging from 1 (Very Much Improved) to 7 (Very Much Worse). A positive treatment outcome is defined as a CGI-I ≤ 2 (much improved or very much improved). A score of 1 or 2 reflects a clinically meaningful improvement in anxiety severity and functioning. Inter-rater reliability for the CGI-I score was high (ICC = .96).
Pediatric Anxiety Rating Scale
The dimensional primary outcome measure was post-treatment anxiety severity as rated by IE on the Pediatric Anxiety Rating Scale (RUPP Study Group, 2002). A total score was computed by summing seven items assessing anxiety severity, frequency, distress, avoidance, and interference during the previous week. Total scores on this scale range from 0 to 35. Inter-rater reliability for the PARS total score was high (ICC = .99).
Speech task
On the third pre-treatment assessment visit (the second visit was for an fMRI scan), children and their primary caregiver completed a 5 minute speech task that was videotaped for later coding. First, children were told that they must give a 1.5 minute speech in front of a video camera. Following Gar and Hudson (2008), the dyad was videotaped as the parent and child discussed and prepared for the speech together. This provided a naturalistic opportunity to assess aspects of parenting relevant to coping with an anxiety-provoking task. A second optional speech was then introduced by the experimenter (see Cobham, et al., 1999). The purpose of the optional speech was to introduce a new stressor that could potentially be avoided, and then observe whether the parent encourages brave behavior. Parents were asked to help the child decide whether or not to participate in the second optional speech and this discussion was also videotaped. Participants gave the required (and optional) speech, if chosen, following the discussion with their parent.
Children were told they would be giving the speech in front of a video camera. We attempted to ensure that the task would be mildly anxiety-provoking for the majority of youth by telling them that their performance skills would be assessed and compared to other children’s skills and by providing speech topics that would be feasible but challenging. Children were asked to rank three potential speech topics in order of how much they would want to speak on that topic. The topics at the pre-treatment assessment were: “Talk about something you have learned from reading a book”, “Talk about something you learned recently in science”, or “Talk about something that you think is wrong with our government and how you would fix it”. The topics at the post-treatment assessment were: “Talk about another country or culture that you know about”, “Talk about a famous person in history”, or “Talk about something that you think is wrong with your school and how you would fix it.” Children were always assigned the topic they ranked as #1 for the first speech, and #2 for the 2nd optional speech. Sixty percent of children chose not to complete the optional speech, and rates did not differ between anxious youth and controls (χ2 = 1.13, p = .567), suggesting that the task was relatively anxiety provoking for the majority of youth.
Maternal encouragement to complete the task (regardless of actual decision outcome) was coded using an event-based coding system developed for this study, in which observers code second-by second speaker content from the video-recorded interactions. “Encouragement of bravery” was coded when a mother encouraged the child to do the optional speech or reinforced the child’s inclination to do so. Examples included statements suggesting that the child do the speech, telling the child that they think they will do well or are good at giving speeches, providing reasons not to worry about the speech or why it should be easy, or providing advice about how to approach the speech to make it easier or to manage associated anxiety. A rate per minute (RPM) variable was calculated to reflect the frequency of encouragement statements per minute throughout the interaction. Coding was conducted by extensively trained and experienced research staff who were blind to group and condition. Approximately 20% of the interactions were coded by a second observer to examine inter-rater reliability. Kappas for maternal behavior were approximately .60. Kappa is a conservative measure, which corrects for chance agreement. Kappas of .60 reflect an adequate level of agreement for frequency rates (Fleiss, 1981).
Analytic Plan
(1) Pre-treatment differences in parental encouragement between parents of all anxious youth and healthy controls were assessed using independent samples t-tests. (2) Changes in parental encouragement from pre- to post-treatment among anxious youth only (since controls did not receive treatment) were examined using a 2 (treatment condition: CBT, CCT) × 2 (time: pretest, posttest) mixed model ANOVA with parental encouragement as the dependent variable. The interaction with treatment type was included to test the hypothesis that greater change would be observed in the families of youth who received CBT compared to CCT. (3) Associations between parental encouragement and treatment response were examined using linear and logistic regression. Hierarchical linear regression was used to examine how pre-treatment parental encouragement predicted post-treatment PARS total scores, controlling for pre-treatment PARS total scores. Pre-treatment PARS score and pre-treatment parental encouragement were entered on the first step and treatment group and the interaction between treatment group and pre-treatment parental encouragement were entered on the second step. Binary logistic regression was used to examine whether pre-treatment parental encouragement predicted categorical treatment response at post-treatment using the CGI-I. Although we originally planned to include an interaction with treatment type in the logistic regression for treatment response, preliminary analyses indicated that only 10 youth (22%) across both treatments (4 CBT/6 CCT) were classified as non-responders on the CGI-I, therefore we did not have sufficient power to examine differences in the association between parenting behaviors and categorical treatment response by treatment type. Youth randomized to both CBT and CCT were included in the categorical logistic regression analysis.
Results
Preliminary Analyses
Intercorrelations among key variables are presented in Table 1. A one-way ANOVA indicated that there were no significant differences in pre-treatment anxiety severity on the PARS between youth randomized to CBT (M = 20.48, SD = 4.43) vs. CCT (M = 20.35, SD = 4.97), but, as expected, these groups differed significantly from controls (M = 1.26, SD = 2.40; F(2,64) = 146.08, p < .0005; d = 3.07). Descriptive statistics for anxious youth treated with CBT and CCT are shown in Table 2. Youth treated with CBT (M = 7.25, SD = 5.49) were rated lower at post-treatment on the PARS compared to youth treated with CCT (M = 11.06, SD = 7.24), although this difference was only significant at the trend level (t = 1.97, p = .055, d = .59). Similarly, more CBT youth were classified as treatment responders on the CGI-I (86%) compared to CCT youth (65%), but again the difference was not statistically significant beyond the trend level (χ2 = 2.91, p = .088, r = .25). The majority of youth in both treatments no longer retained a diagnosis of GAD, SAD, or SP at post-treatment (87% for CBT and 76% for CCT; χ2= .80, p = .371, r = .13).
Table 1.
Bivariate Intercorrelations between Key Variables
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Pre-Tx Encouragement of Bravery (RPM) | -- | .01 | −.35** | −.43*** |
| 2. Post-Tx Encouragement of Bravery (RPM) | -- | -- | .01 | −.11 |
| 3. Pre-Tx PARS | -- | -- | -- | .61*** |
| 4. Post-Tx PARS | -- | -- | -- | -- |
Note: Pre-Tx = pre-treatment; Post-Tx = post-treatment; RPM= rate per minute; PARS = Pediatric Anxiety Rating Scale.
p < .01.
p < .001.
Table 2.
Descriptive Statistics for Key Variables in Anxious Sample.
| Variable | Min | Max | CBT | CCT | t/χ2 | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | ||||
| Pre-Tx Encouragement of Bravery (RPM) | .00 | 4.70 | 1.91 | 1.13 | 1.80 | .99 | −.35 |
| Post-Tx Encouragement of Bravery (RPM) | .21 | 4.62 | 2.57 | 1.00 | 1.43 | 1.03 | −3.68*** |
| Pre-Tx PARS | 9.00 | 29.00 | 20.48 | 4.43 | 20.35 | 4.97 | −.09 |
| Post-Tx PARS | 0.00 | 21.00 | 7.25 | 5.49 | 11.06 | 7.24 | 1.97+ |
| Post-Tx CGI-I (% responder) | 86% | 65% | 2.91+ | ||||
Note: CBT = Cognitive Behavioral Therapy; CCT = Child Centered Therapy; Pre-Tx = pre-treatment; Post-Tx = post-treatment; RPM= rate per minute; PARS = Pediatric Anxiety Rating Scale; CGI-I = Clinical Global Impressions - Improvement Scale.
p < .001.
p < .10.
(1) Group Differences in Parental Behavior During Speech Task
Our first goal was to examine whether parents of anxious youth differed from parents of controls in encouragement of bravery. As hypothesized, parents of anxious youth had lower rates per minute of encouragement to complete the optional speech (MANX = 1.87, SD = 1.07) compared to healthy controls (MCON = 2.44, SD = .91; t(65) = −2.05, p = .044; d = −.57).
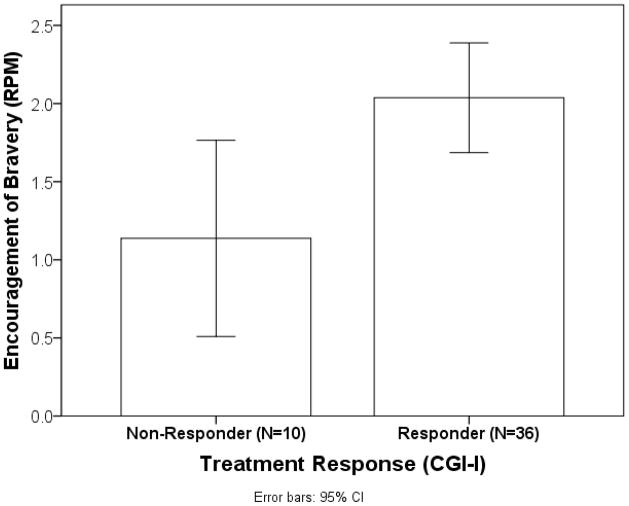
(2) Change in Parental Behavior Following Treatment
Our second goal was to examine whether parental behavior on this task changed following children’s treatment. For encouragement of bravery, there was no main effect of time (pre. Vs post; F(1,45) = .68, p = .415) but, as hypothesized, there was a significant time by treatment type interaction (F(1,45) = 6.15, p = .017; d = 1.14). As shown in Figure 1, rates per minute of encouragement increased from pre- to post-treatment for parents of youth who received CBT but not CCT.
Figure 1.
Change in rate per minute (RPM) of parental encouragement of bravery during speech task from pre- to post-treatment by for CBT vs. CCT
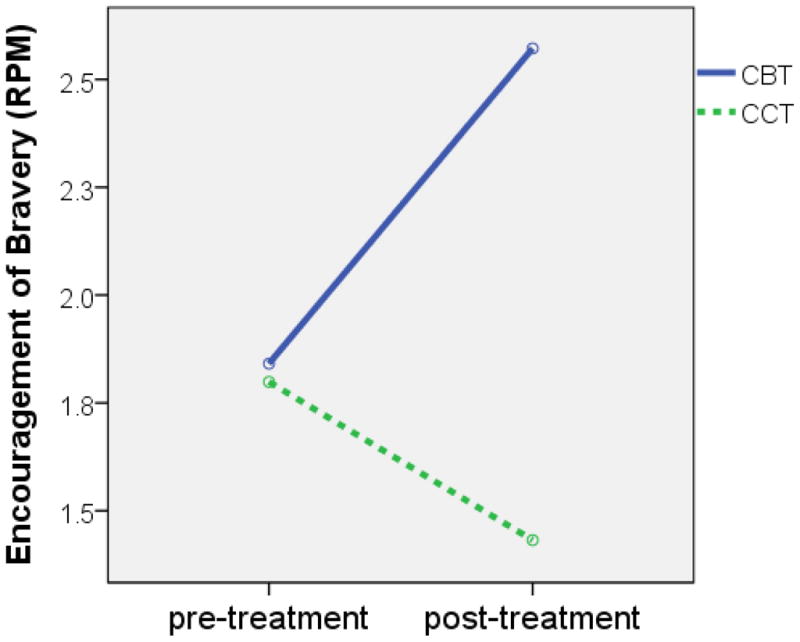
(3) Association of Parental Behavior with Treatment Response
Our third goal was to examine whether parental encouragement was associated with response to treatment. In the hierarchical linear regression predicting continuous treatment response (see Table 3), there was a main effect of encouragement of bravery on the first step (B= −.36, p = .026) that was qualified by an interaction with treatment group on the second step (B= −1.82, p < .001; ΔR2 =.34, p < .001). Post-hoc analyses indicated that pre-treatment encouragement to complete the optional speech was a significant predictor of post-treatment PARS severity (above and beyond pre-treatment severity) for youth treated with CBT (B = −.47, p = .023) but not CCT (B = −.21, p = .445). In the logistic regression predicting categorical treatment response, pre-treatment encouragement of bravery was a significant predictor of treatment response (B = 1.03, p = .024, odds ratio [OR] = 2.80), with youth whose mothers encouraged them more to complete the optional speech at pre-treatment more likely to be classified as treatment responders (see Figure 2).
Table 3.
Summary of Hierarchical Regression Analysis for Variables Predicting Post-Treatment Anxiety Severity (PARS).
| Variable | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE B | β | B | SE B | β | |
| Pre-treatment PARS | .21 | .22 | .15 | .19 | .17 | .14 |
| Encouragement of Bravery | −2.34 | 1.01 | −.36* | 8.82 | 2.63 | 1.37** |
| Treatment (CBT vs. CCT) | 1.07 | 1.62 | .08 | |||
| Encouragement of Bravery × Treatment | −5.54 | 1.25 | −1.82*** | |||
| R2 | .20 | .34 | ||||
| F for change in R2 | 4.91* | 13.50*** | ||||
Note: PARS = Pediatric Anxiety Rating Scale; CBT = Cognitive Behavioral Therapy; CCT = Child Centered Therapy.
p < .05.
p < .01.
p < .001.
Figure 2.
Differences in rate per minute (RPM) of parental encouragement of bravery during speech task for treatment responders and non-responders (based on CGI-I).
Discussion
Findings from the present study suggest that the extent to which parents encourage youth to approach potentially anxiety- provoking situations is an important factor in both the phenomenology and treatment of child anxiety. As hypothesized, parents of anxious youth were less likely to encourage brave behavior during a discussion of whether or not to complete an optional speech than the parents of the healthy controls. These findings are consistent with the notion that parents of anxious youth may facilitate or reinforce avoidance by forgoing opportunities to push their children to do things that may be anxiety-provoking. Failure to encourage brave behavior in anxious situations could stem from a desire to protect the child from potential negative outcomes, such as distress or failure. This notion is consistent with research showing that parents of anxious youth have more negative expectations about their children’s ability to successfully accomplish an anxiety-provoking task (Cobham, et al., 1999; Kortlander, et al., 1997). Parents of anxious youth may also find it personally distressing to observe their child during anxiety provoking situations, particularly since many parents of anxious youth have their own personal history of anxiety disorder (Last, Hersen, Kazdin, Francis, & et al., 1987). Parenting interventions aimed at increasing approach-oriented parenting among parents of youth at high risk for anxiety or with emerging anxious symptoms could be helpful in the prevention and early intervention of child anxiety.
This study focused on a single specific parenting behavior selected because of its theoretical importance for the development and treatment of child anxiety. This differs from the majority of parenting research in the child anxiety literature, which has focused on the related but broader constructs of overprotective parenting, warmth, and autonomy granting. This literature suggests higher levels of overprotective parenting and lower levels of autonomy granting in parents of anxious youth compared to controls (Gar & Hudson, 2008; Hudson, Comer, & Kendall, 2008; Rapee, Schniering, & Hudson, 2009; Jeffrey J. Wood, McLeod, Sigman, Hwang, & Chu, 2003). A meta-analysis of this literature (McLeod, Wood, & Weisz, 2007) showed that global measures of parenting did not explain a large portion of the variance in child anxiety, but the autonomy-granting sub-dimension of parenting was most strongly related to children’s anxious symptoms. Autonomy granting and encouragement of bravery, although different constructs, both convey the parent’s willingness to tolerate and allow the child to make mistakes and experience distress, as well as a respect for the child’s ability (i.e. to make independent decisions or accomplish difficult tasks). These messages likely help anxious youth to develop confidence and gain experience in conquering their fears.
It is important to note that children’s own behaviors probably play an important role in parents’ tendencies to encourage bravery. For example, children who are more anxious may be less likely to elicit or generate encouragement from their parents as a result of transactional processes. For example, when an anxious child cries, screams, or becomes extremely sullen or difficult to manage when a parent pushes them, but ceases these behaviors when the parent ceases pushing, the child is negatively reinforcing the parent’s tendency to avoid pushing for brave behavior. Although little research has addressed this question, a recent study demonstrated that mothers of anxious children asked to help unrelated children prepare for a speech task were more involved and more negative when interacting with anxious compared to non-anxious children (Hudson, Doyle, & Gar, 2009). Another study of preschool aged children showed that children’s anxious behaviors during peer interactions predicted paternal overprotective parenting one year later (McShane & Hastings, 2009). These findings suggest that child effects on anxiety related parenting behaviors are likely. Parents may also be less likely to encourage brave behavior when they are anxious themselves, either through decreased modeling of brave behavior (Whaley, Pinto, & Sigman, 1999) and/or parental discomfort with child distress (Turner, Beidel, Roberson-Nay, & Tervo, 2003). For these reasons, it may be useful to further investigate child effects on parental encouragement of bravery and contributions of parents’ own anxious symptoms or diagnoses.
A particularly encouraging finding was that parenting behavior was amenable to change in child-focused individual CBT. This is one of the first studies to utilize observational data to examine how parenting changes in CBT, particularly in ICBT. Findings are consistent with one existing study which found that child-reported positive and negative parenting improves in both individual and family-based CBT (Silverman, et al., 2009). The present study adds support to the idea that child-focused CBT may result in parenting change by demonstrating change in a specific theoretically-relevant aspect of parenting measured observationally pre- and post-treatment in a naturalistic context. Furthermore, we found that change in encouragement of bravery occurred in CBT but not in a comparison supportive treatment. Because both treatments included similar levels of in-session parent contact, this change may be linked to CBT techniques such as in vivo exposure and weekly homework. CBT therapists actively model and encourage brave behaviors in anxious youth and arrange exposure tasks to feared stimuli in the session and through homework assignments. Parents may model these behaviors initially demonstrated by the therapist. Parents may also respond to increases in mastery and self efficacy from the children themselves as they progress through CBT treatment. Additional research will be needed to clarify the specific mechanisms through which CBT treatment increases parental encouragement to approach anxiety-provoking situations.
It was noteworthy that change in parenting was observed using an individual, child-focused CBT. Although sessions were conducted primarily with the child alone, the treatment included two parent sessions during which therapists introduced parents to the CBT model and encouraged parents to coach their children in facing their fears outside of the clinic. Therapists also engaged parents in planning of exposures and assisting with homework completion. Although our findings suggest that parental change can occur in CBT with this relatively limited parental involvement, it will be important to investigate whether it is possible to achieve greater change in treatments that more directly target parental support for children’s brave behaviors. For example, treatments that focus explicitly on training parents to help their children tackle their fears might be more effective at generating parental change. Alternatively, if levels of parental change are comparable across individual and family-based approaches, individual approaches may be more cost-effective.
We also found that children whose parents were more encouraging of bravery did better in treatment than children whose parents were less encouraging. Although several studies have shown that the family environment has the potential to influence treatment response in FCBT approaches (Crawford & Manassis, 2001; Liber, et al., 2008; Victor, et al., 2007), this is one of the first studies to demonstrate that parenting facilitates successful individual treatment response even when parenting is not explicitly addressed in treatment. Presumably, parents who are more comfortable encouraging their children to approach feared situations will be more likely to encourage children to practice coping skills out of session, and to facilitate home-based exposure practices. In contrast, parents who are not comfortable encouraging their children to do things that may make them anxious, may either convey a lack of confidence in their children’s ability to cope with anxiety, or may simply fail to set up opportunities for practice. Parental encouragement of brave behaviors may also contribute to the strengthening of neural networks underlying behavioral activation and approach motivation (Gray, 1982) in ways that could tip the balance of children’s behavior away from avoidance toward bolder approaches.
There was some evidence that encouragement of bravery was specifically related to CBT treatment response, as parental encouragement was more strongly associated with post-treatment anxiety severity for youth treated with CBT compared to CCT. CBT is presumed to operate by producing behavioral and cognitive change as a function of mastery in gradual exposure to feared stimuli (Hudson, 2005). Thus, it makes sense that parenting behaviors that facilitate mastery in feared situations could play a specific role in treatment outcome. In contrast, CCT is presumed to work by establishing a trusting therapeutic relationship that is self-affirming, empowering, and validating (Cohen, et al., 2004). There may be other parenting behaviors, such as parental warmth and validation, that might be expected to change in CCT treatment, and these should be investigated further.
Potential limitations of the study should be noted. We defined encouragement of bravery as encouragement of approach behaviors in the context of potential threat. However, it is possible that not all youth would require “bravery” to complete the task, as they may not have experienced it as anxiety-provoking. Although high rates of declining to complete the optional speech (60%), and clinical observations, suggested that the majority of youth found the task to be anxiety-provoking, we did not collect objective data on anxiety levels in response to the optional speech. Additionally, parents might have encouraged, or failed to encourage, youth to complete the task for reasons other than encouraging bravery, such as the desire to please the experimenter or the desire to leave the lab sooner. Another limitation of the study is its exclusive focus on primary caregivers (the mother for 94% of dyads). Recent data suggests that fathers’ behaviors, such as rough and tumble play, can play an important protective role in child anxiety (Bogels & Phares, 2008). It is possible that fathers may be more likely to encourage approach behaviors than mothers, and that paternal behavior may interact with maternal behavior in influencing children’s avoidance tendencies. Focusing on how fathers help children cope with anxiety provoking situations is an important area for future research. Another limitation is the sample size, which limited our ability to examine moderator variables. Furthermore, positive treatment response was particularly high in this sample. Although there was sufficient variability in continuous post-treatment severity ratings, there was a relatively small number of youth classified as categorical non-responders based on independent evaluator ratings of global improvement. For this reason, we did not have sufficient power to compare predictors of categorical treatment response for CBT vs. CCT.
Despite these limitations, this study also had several strengths. A key strength is the inclusion of observational data during an ecologically valid laboratory stressor. The use of a clinically diagnosed sample of anxious youth and the ability to look at changes in parenting behaviors in response to two manualized and randomized psychotherapy treatments were also notable strengths. Specifically, this is one of the first investigations to examine how parenting changes in response to individual CBT treatment. It is also the first study of which we are aware that compares family-based predictors of treatment response or change across treatment in CBT with an active comparison treatment. Findings suggest that parental encouragement of brave behavior in anxiety-provoking contexts is an important target that could be maximized in CBT preventive and intervention approaches for improving the social and emotional functioning of anxious youth.
Highlights.
Parents of anxious youth are less likely to encourage bravery during a speech.
Parental encouragement of bravery increases with CBT treatment.
Parental encouragement of bravery does not increase with supportive treatment.
Anxious youth do better in treatment when their parents encourage bravery.
Encouragement of bravery is important in the development and treatment of anxiety.
Acknowledgments
We are grateful to the participants and their families. We are also grateful to Craig Leve, Marc Zollinger and MaryAnn Roberts for their assistance in coding and processing this data, Kelly O’Neil and Jennifer Podell for their contributions to clinical supervision, and Emily Yarrison, Rachel Kolko, Jennifer Jakubcak, and Marcie Walker for research assistance and data management. This research was supported by National Institute of Mental Health grant P50 MH080215 (Neal D. Ryan, P.I., Jennifer S. Silk, Project Director). Support for research participant recruitment was also provided by the Clinical and Translational Science Institute at the University of Pittsburgh (NIH/NCRR/CTSA Grant UL1 RR024153).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychological Association, A. P. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C: Author; 1994. [Google Scholar]
- Barmish AJ, Kendall PC. Should parents be co-clients in cognitive-behavioral therapy for anxious youth? Journal of Clinical Child and Adolescent Psychology. 2005;34:569–581. doi: 10.1207/s15374424jccp3403_12. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Rapee RM, Dadds MM, Ryan SM. Family enhancement of cognitive style in anxious and aggressive children. Journal of Abnormal Child Psychology. 1996;24:187–203. doi: 10.1007/BF01441484. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. Journal of Consulting & Clinical Psychology. 2000;68:1072–1080. [PubMed] [Google Scholar]
- Bogels S, Phares V. Fathers’ role in the etiology, prevention and treatment of child anxiety: a review and new model. Clinical Psychology Review. 2008;28:539–558. doi: 10.1016/j.cpr.2007.07.011. [DOI] [PubMed] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH. Anxious children and their parents: What do they expect? Journal of Clinical Child Psychology. 1999;28:220–231. doi: 10.1207/s15374424jccp2802_9. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Interventions for sexually abused children: Initial treatment outcome findings. Child Maltreatment. 1998;3:17–26. [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse & Neglect. 2005;29:135–145. doi: 10.1016/j.chiabu.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Corporation, P. Wechsler Abbreviated Scale of Intelligence (WASI) manual. San Antonio, TX: Author; 1999. [Google Scholar]
- Crawford A, Manassis K. Familial predictors of treatment outcome in childhood anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:1182–1189. doi: 10.1097/00004583-200110000-00012. [DOI] [PubMed] [Google Scholar]
- Creswell C, Willetts L, Murray L, Singhal M, Cooper P. Treatment of child anxiety: an exploratory study of the role of maternal anxiety and behaviours in treatment outcome. Clinical Psychology & Psychotherapy. 2008;15:38–44. doi: 10.1002/cpp.559. [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Taghavi R, Neshat-Doost H, Moradi A, Canterbury R, Yule W. Patterns of processing bias for emotional information across clinical disorders: A comparison of attention, memory, and prospective cognition in children and adolescents with depression, generalized anxiety, and posttraumatic stress disorder. Journal of Clinical Child and Adolescent Psychology. 2003;32:10–21. doi: 10.1207/S15374424JCCP3201_02. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. Statistical Methods for Rates and Proportions. 2. New York: Wiley; 1981. [Google Scholar]
- Gar NS, Hudson JL. An examination of the interactions between mothers and children with anxiety disorders. Behaviour Research and Therapy. 2008;46:1266–1274. doi: 10.1016/j.brat.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Gray JA. The Neuropsychology of Anxiety: an Enquiry into the Functions of the Septo-Hippocampal System. Oxford: Clarendon Press/Oxford University Press; 1982. [Google Scholar]
- Guy W. The Clinical Global Impression Scale. Rockville, MD: U.S. Department of Health, Education, and Welfare Public Health Service, Alcohol, Drug Abuse, Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research; 1976. [Google Scholar]
- Hudson JL. Mechanisms of change in cognitive behavioral therapy for anxious youth. Clinical Psychology: Science and Practice. 2005;12:161–165. [Google Scholar]
- Hudson JL, Comer JS, Kendall PC. Parental responses to positive and negative emotions in anxious and nonanxious children. Journal of Clinical Child and Adolescent Psychology. 2008;37:303–313. doi: 10.1080/15374410801955839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, Doyle AM, Gar N. Child and maternal influence on parenting behavior in clinically anxious children. Journal of Clinical Child and Adolescent Psychology. 2009;38:256–262. doi: 10.1080/15374410802698438. [DOI] [PubMed] [Google Scholar]
- In-Albon T, Schneider S. Psychotherapy of childhood anxiety disorders: A meta-analysis. Psychotherapy and Psychosomatics. 2007;76:15–24. doi: 10.1159/000096361. [DOI] [PubMed] [Google Scholar]
- James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews. 2005:4. doi: 10.1002/14651858.CD004690.pub2. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children- (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kendall PC. Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 1994;62:100–110. doi: 10.1037//0022-006x.62.1.100. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clincal trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke K. Cognitive-Behavioral Therapy for Anxious Children: Therapist Manual. Ardmore, PA: Workbook Publishing; 2006a. [Google Scholar]
- Kendall PC, Hedtke K. The Coping Cat Workbook. Ardmore, PA: Workbook Publishing; 2006b. [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Khanna MS, Kendall PC. Exploring the role of parent training in the treatment of childhood anxiety. Journal of Consulting & Clinical Psychology. 2009;77:981–986. doi: 10.1037/a0016920. [DOI] [PubMed] [Google Scholar]
- Kortlander E, Kendall PC, Panichelli-Mindel SM. Maternal expectations and attributions about coping in anxious children. Journal of Anxiety Disorders. 1997;11:297–315. doi: 10.1016/s0887-6185(97)00012-1. [DOI] [PubMed] [Google Scholar]
- Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:404–411. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- Last CG, Hersen M, Kazdin AE, Francis G, et al. Psychiatric illness in the mothers of anxious children. American Journal of Psychiatry. 1987;144:1580–1583. doi: 10.1176/ajp.144.12.1580. [DOI] [PubMed] [Google Scholar]
- Liber JM, van Widenfelt BM, Goedhart AW, Utens EMWJ, van der Leeden AJM, Markus MT, et al. Parenting and parental anxiety and depression as predictors of treatment outcome for childhood anxiety disorders: has the Role of fathers been underestimated? Journal of Clinical Child & Adolescent Psychology. 2008;37:747–758. doi: 10.1080/15374410802359692. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007;27:155–172. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- McShane KE, Hastings PD. The new friends vignettes: Measuring parental psychological control that confers risk for anxious adjustment in preschoolers. International Journal of Behavioral Development. 2009;33:481–495. [Google Scholar]
- Rapee RM. The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety? Biological Psychiatry. 2002;52:947–957. doi: 10.1016/s0006-3223(02)01572-x. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology. 2009;5:311–341. doi: 10.1146/annurev.clinpsy.032408.153628. [DOI] [PubMed] [Google Scholar]
- Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for anxiety in children and adolescents: A meta-analytic review. Clinical Psychology Review. 2012;32:251–262. doi: 10.1016/j.cpr.2012.01.005. [DOI] [PubMed] [Google Scholar]
- RUPP Study Group. The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM. Transfer of control: A psychosocial intervention model for internalizing disorders in youth. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association; 1996. pp. 97–119. [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:675–687. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology. 2009;77:474. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suveg C, Zeman J. Emotion regulation in children with anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33:750–759. doi: 10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- Taghavi MR, Moradi AR, Neshat-Doost HT, Yule W, Dalgleish T. Interpretation of ambiguous emotional information in clinically anxious children and adolescents. Cognition & Emotion. 2000;14:809–822. [Google Scholar]
- Turner SM, Beidel DC, Roberson-Nay R, Tervo K. Parenting behaviors in parents with anxiety disorders. Behaviour Research and Therapy. 2003;41:541–554. doi: 10.1016/s0005-7967(02)00028-1. [DOI] [PubMed] [Google Scholar]
- Victor AM, Bernat DH, Bernstein GA, Layne AE. Effects of parent and family characteristics on treatment outcome of anxious children. Journal of Anxiety Disorders. 2007;21:835–848. doi: 10.1016/j.janxdis.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley SE, Pinto A, Sigman M. Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology. 1999;67:826–836. doi: 10.1037//0022-006x.67.6.826. [DOI] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Piacentini JC, Sigman M. One-year follow-up of family versus child CBT for anxiety disorders: Exploring the roles of child age and parental intrusiveness. Child Psychiatry and Human Development. 2009;40:301–316. doi: 10.1007/s10578-009-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Sigman M, Hwang WC, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003;44:134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]