Abstract
Background
Most patient chronic disease self-management interventions target single disease outcomes. We evaluated the effect of a tailored hypertension self-management intervention on the unintended targets of glycosylated hemoglobin (Hb A1c) and LDL cholesterol (LDL-C).
Methods
We examined 588 patients from the Veterans Study to Improve the Control of Hypertension (V-STITCH), a two year randomized controlled trial. Patients received either a hypertension self-management intervention delivered by a nurse over the telephone or usual care. Although the study focused on hypertension self-management, we compared changes in Hb A1c among a subgroup of 216 patients with diabetes and LDL-C among 528 patients with measurements during the study period. Changes in these lab values over time were compared between the two treatment groups using linear mixed-effects models.
Results
For the patients with diabetes, the hypertension self-management intervention resulted in a 0.46% reduction in Hb A1c over two years compared to usual care (95% CI: 0.04% to 0.89%; p=0.03). For LDL-C, the self-management intervention arm resulted in a reduction of 0.9mg/dl over two years compared to usual care (95% CI: -7.3mg/dl to 5.6mg/dl; p=0.79).
Conclusions
There was no evidence of a hypertension self-management intervention effect on LDL-C, but there was a modest effect of the intervention on the unintended target of Hb A1c. This effect was similar to that seen in self-management interventions specifically targeting diabetes management. Chronic disease self-management interventions may spill over into patients’ co-morbid diagnoses.
Keywords: Self-management, telemedicine, chronic disease, randomized controlled trial
Introduction
Cardiovascular disease (CVD) remains the leading cause of death in the U.S., accounting for over one third of deaths [1]. The modifiable risk factors of hypertension and hypercholesterolemia among the general population, and glycemic control among patients with diabetes synergistically contribute to a patient’s risk for cardiovascular events [2, 3]. These risk factors co-occur in the majority of affected individuals [4] and control of these risk factors in combination substantially reduce a patient’s risk for clinical events greater than any single risk factor alone [5]. In spite of the availability of effective therapy for diabetes, hypertension, and hypercholesterolemia, a study using the Third National Health and Nutrition Examination Survey (NHANES III) found that only 7.3% of patients with diabetes simultaneously achieve recommended goals of therapy for all three conditions [6]. Similarly, in the Veterans Affairs, only 4% of patients with diabetes achieve targets of simultaneous control of all three risk factors[7] and only 13% of patients with known CVD achieve target BP and cholesterol control [8].
The inability to achieve accepted targets of risk factor control likely arises from a complex interaction of patient and provider behaviors. Interventions that target self-management skills among patients with chronic diseases have been growing in popularity recently and have been suggested as an integral part of improving the quality of chronic disease care [9, 10]. A systematic review of chronic disease self-management programs in older adults reported modest, but clinically important reductions of Hb A1c (average reduction of 0.8%) and SBP (average reduction of 5mmHg)[11]. Counseling and behavioral interventions to improve LDL-C, however, have produced smaller benefits with mean reductions of less than 3mg/dl.[12] Most self-management interventions target a single chronic disease and focus on disease specific outcomes.[11, 13-18] The principles and methods of self-management support in chronic disease interventions are similar across disease states suggesting that the benefits of a self-management intervention may extend beyond the intended targets.[9] Therapeutic interventions that can improve multiple cardiovascular risk factors simultaneously would be particularly valuable in light of the growing prevalence of diabetes and hypertension and expanding indications for cholesterol lowering in high risk patients.
The Veterans’ Study to Improve the Control of Hypertension (V-STITCH) was a randomized controlled trial that tested a patient level self-management intervention delivered by a nurse over the phone and a provider level computer decision support system to optimize medication management [19]. The purpose of the present study is to evaluate the effect of the patient self-management intervention targeting patients’ blood pressure on the unintended targets of diabetes and cholesterol control.
Methods
Study Design
The Veterans Study to Improve the Control of Hypertension (VSTITCH) was a two-year cluster randomized control trial. The interventions occurred at two levels (provider and patient). Primary care providers were first randomized to either receive the computer decision support system focusing on hypertension medication management delivered at the point of care during patient visits or usual care without the decision support interface. Within each participating provider’s primary care panel, patients with hypertension were then randomized to either receive a nurse telephone self-management intervention (described in further detail below) or usual primary care. This two level randomization (patient and provider) was designed to create balance in both patient and provider characteristics for the two interventions being tested. The patients were the unit of analysis and the primary study outcome was blood pressure control defined by JNC 6 criteria which was the current guideline at the time of the study [20]. The primary study results are presented elsewhere [21]. There was no effect from the provider intervention on blood pressure control, nor was there a significant effect interaction between the patient and provider interventions. We therefore analyzed all patients receiving the telephone self-management intervention compared to all patients who did not receive this intervention, regardless of whether their provider received the computer decision support system.
Participants
The study was conducted in the Durham VA Medical Center primary care clinics (3 sites). We enrolled patients from 32 primary care providers (23 general internists, 7 physician assistants and 2 registered nurse practitioners). To be eligible for the patient intervention, individuals had to be followed by one of the providers randomized to either the provider intervention or control group, had a diagnosis of hypertension by an outpatient diagnostic code (ICD 401.0, 401.1, or 401.9) on outpatient encounter forms, be enrolled in the Durham VAMC primary care clinics during the previous year, and had a filled prescription for hypertensive medication in the previous year. The research assistants sent letters and contacted 816 eligible patients by telephone prior to upcoming primary care appointments. Among these patients, 190 refused, and 38 were excluded for not meeting inclusion criteria (see [19] for more details). We enrolled 588 individuals (76% recruitment rate). Primary care providers were first randomized to receive or not receive the provider intervention. Patient randomization to the behavioral intervention occurred within each provider so that equal numbers of patients from each provider received the behavioral intervention or usual care. Study statisticians generated random assignment of interventions in blocks of 16 which were placed in sealed envelopes. At enrollment, the research assistants opened a sealed envelope to reveal the patients’ randomly assigned study arm. Patients enrolled in the study were followed for 24 months or until drop out. The study was approved by the Durham VAMC IRB; all patients provided written informed consent
For the present study, starting with the randomized sample of patients in V-STITCH, we created additional criteria to define appropriate cohorts of patients to evaluate the intervention effects on the outcomes of glycosolated hemoglobin (HbA1c) and low density lipoprotein cholesterol (LDL-C). First, to identify patients for inclusion in the analysis of HbA1c, we identified all study participants with a diagnosis of diabetes based either on self-report or based on an ICD-9 diagnosis code of 250.x at the time of enrollment. For the patients with diabetes enrolled in V-STITCH, we included all patients with laboratory measurements of HbA1c obtained from the Durham VAMC lab between 24 weeks prior to enrollment and 24 weeks after study completion. We obtained Hb A1c values for 216 patients (99% of all patients with diabetes in the parent study). Similarly, to identify a cohort of patients to include in analysis of LDL-C, we queried the Durham VAMC medical records to identify patients enrolled in the V-STITCH study with LDL-C measurements obtained within 24 weeks before enrollment and 24 weeks after study completion. Of the 588 patients enrolled in V-STITCH, 528 patients had LDL-C measurements during this window through the VAMC lab (90%).
Measures
The two outcomes of interest for the present study were glycemic control measured by Hb A1c, and fasting LDL cholesterol. All labs were obtained through the Durham VA Medical Center (DVAMC) clinical laboratory and abstracted from the electronic medical record. While some patients receive dual care outside of the VA, we did not record any outside lab measurements. All LDL-C measurements were calculated from a fasting lipid panel using the Friedewald method [22]. To describe the patient samples at the time of enrollment in the study, we defined the baseline HbA1c and LDL-C as the reading closest to enrollment that was within 24 weeks before or after this date.
Demographic information was collected by patient self-report at the time of enrollment: age, gender, race, marital status, education level, and financial status. Race was dichotomized as white or non-white. Highest level of education achieved was categorized as 0-9th grade, 10-12th grade, some college or vocational school, or college graduate. Patients who reported they had enough money to pay their bills only by cutting back on things or difficulty paying their bill no matter what was done were categorized as inadequate income [23]. Participants were asked if they currently exercise or participate in an active physical sport. Similarly, patients were asked to report their current smoking status. The Rapid Estimate of Adult Literacy in Medicine (REALM) was used to measure literacy [24]. Literacy was evaluated as a dichotomous variable with low literacy defined as REALM score, 0-60 (<9th grade level) and adequate literacy defined as REALM score 61-66 (≥9th grade level).
Intervention
The nurse telephoned patients within one week of randomization and then every two months over 24 months to deliver the intervention for a total of 12 nurse calls. At each call, the nurse delivered scripted information drawn from the following nine educational and behavioral modules: hypertension knowledge; memory; social support; patient/provider communication; medication refill reminders; appointment compliance; health behaviors (diet, exercise, smoking alcohol use); health literacy aids; and medication side effects. The information has been described in further detail in a separate report [25]. To ensure that the intervention information was standardized, the nurse used a database application, which contained predetermined scripts and tailoring algorithms. There were no face-to-face meetings between the nurse and the patient. The majority of the patients in the intervention arm received all 12 phone calls (mean # of calls 11.0; median 12; range 3-12).
Patients enrolled in both the intervention arm and usual care received routine primary care throughout the study from the Durham VA Medical Center. Patients randomized to usual care did not receive any nurse calls and did not have access to the nurse. Patients enrolled in usual care, like intervention patients, were contacted at six and 24 months to complete 30-minute secondary outcome assessments.
2.6. Statistical Analyses
Two separate analyses were conducted: one for patients with diabetes using HbA1c as the dependent variable, and one for all patients with LDL-C as the dependent variable. Because these outcomes were collected during the course of routine primary care, each patient had a varying number of HbA1c and LDL assessments at varying intervals of time. Thus, it is not possible to examine specific lab values for all patients at set periods (e.g., 6, 12, and 24-months) as is commonly done in longitudinal randomized controlled trials. We used a linear mixed effects model because it is a method that accounts for this data structure, to analyze changes in HbA1c and LDL over time [26]. Using this method, all patient HbA1c or LDL-C measurements obtained during the study time interval contributed to the estimation of mean laboratory values during the two year study period.
Exploratory data analysis of HbA1c values indicated a linear trend over time in both the usual care and nurse telephone intervention groups, so time was defined as the number of weeks from baseline and treated as a linear, continuous variable in the mixed-effects model. The trend in the usual care arm was toward increasing HbA1c over time while the trend in the intervention arm was toward decreasing HbA1c over time. The fixed effects in the HbA1c model included intervention group (nurse behavior vs. usual care), time in weeks, and intervention group by time interaction. For analysis of the LDL-C outcome, exploratory data analysis indicated a quadratic trend over time, with the average LDL-C initially increasing in both groups and then declining. To appropriately model the shape of this outcome distribution, we included the fixed effects of intervention group (nurse behavioral vs. usual care), time in weeks, time2, intervention group-by-time interaction, and intervention group-by-time2 interaction. In both the A1c and LDL models, to account for the correlation between a patient’s repeated measurements over the 36 months, the model also included patient-level random effects in the form of a patient-level random intercept and slope. For both outcomes we report the estimated change in the lab value between study enrollment (t=0 weeks) and study completion (t=104 weeks). Models for A1c and LDL were estimated using PROC MIXED in SAS Version 9.1 (SAS Institute Inc, Cary NC).
Results
Results for patients with diabetes: Hb A1c
Of the 588 veterans enrolled in VSTITCH, there were 219 patients with diabetes (117 patients in usual care arm and 102 patients in the intervention group). Of these, 216 patients had HbA1c measurements available for analysis and were included in the analysis. The Figure shows the patient flow from patient enrollment in the parent V-STITCH study, with the two cohorts identified for analysis in the present study. Patient characteristics for the patient sample with diabetes are shown in Table 1. The majority of patients were male, obese, and currently married. There was a high prevalence of limited health literacy. There were no significant differences in any of the baseline patient characteristics between the two treatment arms (P >0.05 for all between group comparisons).
Figure. Patient Flow for Hb A1c and LDL Cholesterol analysis.
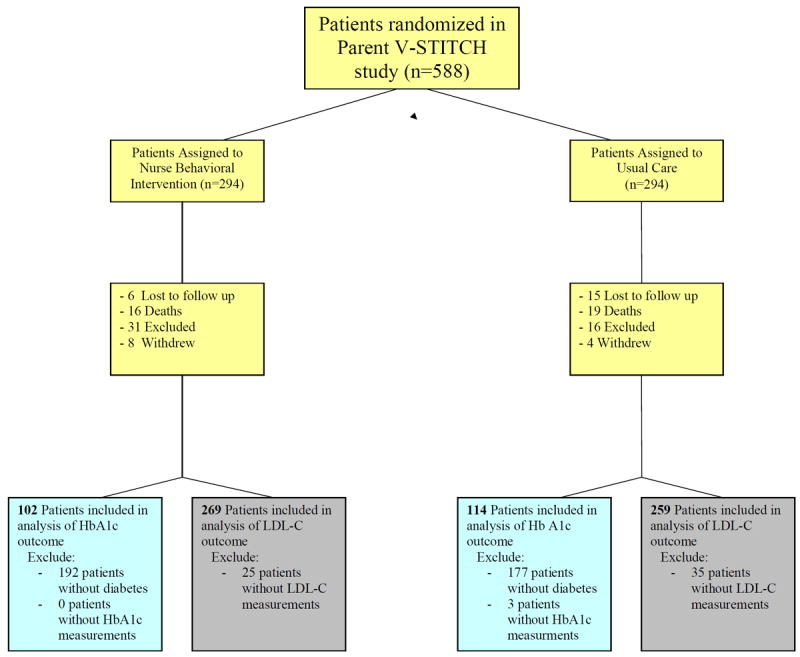
Table 1.
Patient Characteristics for Diabetic Outcomes
| Characteristics | Behavioral Intervention (n=102) | Usual Care (n=114) |
|---|---|---|
| Age - Mean (SD) | 63.8 (10.8) | 64.3 (10.8) |
|
| ||
| Mean BMI (SD) | 31 (5) | 32 (6) |
|
| ||
| Male | 98% | 99% |
|
| ||
| Married | 66% | 71% |
|
| ||
| High school or less | 53% | 56% |
|
| ||
| Literacy <9th grade | 42% | 41% |
|
| ||
| Currently Employed | 14% | 24% |
|
| ||
| Inadequate income | 23% | 18% |
|
| ||
| Self-reported Race | ||
| White | 55% | 56% |
| African-American | 42% | 43% |
| Other | 3% | 1% |
|
| ||
| Health Behaviors | ||
| No Exercise | 44% | 43% |
| Currently smoke | 25% | 16% |
|
| ||
| Baseline Clinical Variables | ||
| Mean HbA1c, % (SD) | 7.5 (1.2) | 7.1 (1.2) |
| Mean Systolic BP, mmHg (SD) | 138.5 (17.9) | 139.1 (20.0) |
| Mean Diastolic BP, mmHg (SD) | 73.2 (12.3) | 74.1 (12.1) |
No significant between group differences for all variables (P>0.05)
Changes in Hb A1c over the course of intervention period are presented in Table 3. The mean Hb A1c decreased by 0.28% in the intervention arm (95% CI: -0.59 to + 0.04), but increased by 0.18% in the usual care arm (95% CI: -0.11 to +0.47). Based on the linear mixed-effects model, the estimated mean reduction in HbA1c over 2 years in the intervention compared to usual care group was 0.46% (95% CI: 0.04% to 0.89%; p=0.03).
Table 3.
Two year changes in glycemic and lipid control.
| Mean Change over 24 month a | Mean Difference in Behavioral Arm compared to Usual Care (95% CI) | |||
|---|---|---|---|---|
|
| ||||
| Behavioral Intervention | Usual Care | Behavioral Intervention-Usual Care | p-value | |
| Hb A1c, % | -0.28 (-0.59 to -0.04) | +0.18 (-0.11 to +0.47) | -0.46 (-0.03 to -0.89) | 0.03 |
| LDL-C, mg/dl | -4.3 (-8.9 to +0.3) | -5.2 (-9.7 to -0.6) | +0.9 (-5.6 to +7.3) | 0.79 |
negative values represent overall reduction in lab value; positive values represent mean increase
Predicted values based on linear mixed effects model
Results for patients with available cholesterol measurements: LDL-C
Of the 588 patients enrolled in VSTITCH, 528 patients had LDL-C measurements within the defined time period and were included in the analysis (269 patients in the behavioral intervention and 259 in usual care). Patient characteristics are shown in table 2 and are similar to the cohort examined for analysis of HbA1c outcome. There was no significant difference between the intervention and usual care for any baseline characteristics (p>0.05 for all between group comparisons).
Table 2.
Patient Characteristics for LDL Outcomes
| Characteristics | Behavioral Intervention (n=269) | Usual Care (n=259) |
|---|---|---|
| Age - Mean (SD) | 63.0 (11.1) | 63.6 (10.9) |
|
| ||
| BMI (SD) | 30.4 (5.5) | 30.3 (5.7) |
|
| ||
| Male gender | 98% | 98% |
|
| ||
| Married (%) | 69% | 70% |
|
| ||
| High school or less (%) | 49% | 52% |
|
| ||
| Literacy <9th grade (%) | 38% | 41% |
|
| ||
| Employed (%) | 26% | 32% |
|
| ||
| Inadequate income (%) | 23% | 19% |
|
| ||
| Self-reported Race | ||
| White | 56% | 60% |
| African American | 42% | 37% |
| Other | 2% | 3% |
|
| ||
| Health Behaviors | ||
| No Exercise | 48% | 41% |
| Currently smoke | 29% | 21% |
|
| ||
| Baseline Disease Control | ||
| LDL-cholesterol, mg/dl (SD) | 112 (32) | 107 (33) |
| Mean Systolic BP, mmHg (SD) | 138.7 (16.9) | 139.1 (17.9) |
| Mean Diastolic BP, mmHg (SD) | 75.8 (11.7) | 76.2 (11.2) |
No significant differences between groups: P>0.05 for all comparisons.
Changes in LDL-C over the course of intervention period are presented in Table 3. While LDL-C decreased over the 2 year study period in both groups, there was no significant between group difference in this outcome with an estimated mean difference of 0.9mg/dl LDL-C lowering in the usual care group compared to the behavioral intervention (95% CI: -7.3 to 5.6; p=0.79).
Discussion
In a randomized controlled trial of a nurse administered tailored behavioral intervention to improve blood pressure control, we evaluated the effect of the intervention on the unintended targets of diabetes and cholesterol control over two years. There was a modest difference in glycemic control between intervention and usual care patients that was statistically significant. LDL-C improved in both the intervention and usual care groups over the two year study period and there was no evidence of an intervention effect on this outcome.
Although hypertension, diabetes, and dyslipidemia are pathophysiologically distinct, from the patient perspective they are similar in the self-management requirements for successful disease control. All three are usually asymptomatic which has been reported as a barrier to effective self-management [27]. The benefits of treatment are based on avoiding long-term future vascular events and patients often lack accurate risk perception [28, 29]. Patients can significantly improve disease control of all three through diet and lifestyle changes, however such changes are often difficult to maintain [30]. In addition, approximately 20-50% of patients are non-adherent to chronic medications and suffer worse health outcomes as a result [31]. In spite of these similar self-management challenges, self-management interventions for hypertension, diabetes, or cholesterol typically focus on single disease-specific outcomes. Indeed, the present study is taken from a trial focused on changing patient behavior specifically within the context of hypertension without focus on related cardiovascular risk factors. Because the patient behaviors required for effective hypertension care overlap with other cardiovascular risk factors, there is reason to believe that an intervention’s effect may ‘spill over’ to other related conditions.
The findings of this study should be considered in light of prior self-management interventions directly targeting glycemic control or cholesterol. One useful way to compare the magnitude of intervention effects across studies is through standardized effect sizes. This measure divides the intervention effect by the standard deviation of the outcome variable. For the outcome of Hb A1c, the effects of self-management interventions are typically modest. Among older adults, Chodosh and colleagues reported that self-management interventions produced a mean effect size of -0.36 on the outcome of Hb A1c (approx 0.81% reduction) [11]. This is comparable to the estimated effect size of the present intervention which is approximately -0.38 (-0.46 divided by the baseline standard deviation of 1.2). Among behavioral interventions targeting cholesterol in addition to other risk factors, the mean reduction in cholesterol is often much smaller with effect sizes of <0.1 (or <3mg/dl) [12]. This suggests that the effects of self-management interventions on cholesterol may be small even when this is the targeted outcome. Although the interpretation of these effect sizes may be limited by significant heterogeneity in the definitions for self-management interventions [17], it is interesting to note that our findings of indirect intervention effects on Hb A1c and LDL-C are similar to that of studies targeting these outcomes.
There are a few limitations of this study that should be considered when interpreting the results. First, our patient sample was almost entirely male and these findings may not generalize to female populations. Second, all patients were willing to participate in a hypertension improvement randomized controlled trial and may be more motivated than other patients with hypertension. Finally, Hb A1c and LDL-C were not collected as part of the study protocol and we relied on the measurement of these outcomes in the course of routine clinical care. Because of the variable measurement of the outcome over time a linear mixed effects model was used to estimate average change in lab parameters over time.
It is also important to note that we evaluated the intervention’s effect on Hb A1c and LDL-C over a two year period. Most self-management interventions for chronic disease last 6 months or less and there appears to be a deterioration of intervention effects over longer time periods [17, 32]. Norris and colleagues reported that the effect of diabetes self-management intervention often diminishes over time [32]. By choosing the longer timeframe we were able to evaluate lasting changes in disease control, although we were not able to determine if these changes persisted after completion of the intervention. The difficulty in maintaining behavioral change is one of the greatest challenges in chronic disease management and further research is needed to determine if lasting changes in disease control can be sustained.
In conclusion, there was some evidence that a telephone administered nurse behavioral intervention targeting blood pressure control may have a modest ‘spill over’ effect on diabetes control at two years; however the intervention had no significant effect on LDL-cholesterol. While self-management interventions often have modest effects on their intended target of disease control, the self-management requirements for disease control are similar for many chronic diseases. Given the growing prevalence of multimorbidity and the synergistic relationship between cardiovascular risk factors, interventions that can simultaneously target multiple determinants of risk may be particularly valuable in optimizing patient outcomes.
Acknowledgments
This research is supported by the Department of Veterans Affairs, Veterans Health Administration, HSR&D Service, investigator initiative grant 20-034. The first author was supported by Grant Number KL2 RR024127 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR, NIH, or Department of Veterans Affairs. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asap.
Footnotes
This work was presented in part as a poster at the Society of General Internal Medicine Annual Meeting in Pittsburgh, PA on April 9th, 2008.
References
- 1.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Jackson R, Lawes CM, Bennett DA, Milne RJ, Rodgers A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet. 2005;365(9457):434–41. doi: 10.1016/S0140-6736(05)17833-7. [DOI] [PubMed] [Google Scholar]
- 3.Law MR, Wald NJ. Risk factor thresholds: their existence under scrutiny. Bmj. 2002;324(7353):1570–6. doi: 10.1136/bmj.324.7353.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selby JV, Peng T, Karter AJ, et al. High rates of co-occurrence of hypertension, elevated low-density lipoprotein cholesterol, and diabetes mellitus in a large managed care population. Am J Manag Care. 2004;10(2 Pt 2):163–70. [PubMed] [Google Scholar]
- 5.Goede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91. doi: 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]
- 6.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. Jama. 2004;291(3):335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 7.Jackson GL, Edelman D, Weinberger M. Simultaneous control of intermediate diabetes outcomes among Veterans Affairs primary care patients. J Gen Intern Med. 2006;21(10):1050–6. doi: 10.1111/j.1525-1497.2006.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Therapeutic goal attainment in patients with hypertension and dyslipidemia. Med Care. 2006;44(1):39–46. doi: 10.1097/01.mlr.0000188982.25397.37. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. Jama. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st centry. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 11.Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143(6):427–38. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ebrahim S, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev. 2006;(4) doi: 10.1002/14651858.CD001561.pub2. CD001561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363(9421):1589–97. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- 14.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care?: Systematic review of randomized controlled trials. Arch Intern Med. 2004;164(7):722–732. doi: 10.1001/archinte.164.7.722. [DOI] [PubMed] [Google Scholar]
- 15.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 16.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 17.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164(15):1641–9. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 18.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–37. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 19.Bosworth HB, Olsen MK, Goldstein MK, et al. The veterans’ study to improve the control of hypertension (V-STITCH): design and methodology. Contemp Clin Trials. 2005;26(2):155–68. doi: 10.1016/j.cct.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 20.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157(21):2413–46. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 21.Bosworth H, Olsen MK, Dudley T, Orr M, Goldstein MK, Datta SK, McCant F, Gentry, Simel DL, Oddone EZ. The Veterans’ Study to Improve The Control of Hypertension (V-STITCH): A Patient and Provider Intervention to Improve Blood Pressure Control; 25th HSR&D National meeting; Washington, DC. 2007. [Google Scholar]
- 22.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 23.Bosworth HB, Bastian LA, Kuchibhatla MN, et al. Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med. 2001;63(4):603–8. doi: 10.1097/00006842-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Davis T, Long SW, Jackson RH, et al. Rapid Estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine. 1993;25:391–395. [PubMed] [Google Scholar]
- 25.Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005;57(1):5–14. doi: 10.1016/j.pec.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of Longitudinal Data. 2. New York: Oxford University Press; 2002. [Google Scholar]
- 27.Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Educ Couns. 2005;57(3):300–7. doi: 10.1016/j.pec.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Powers BJ, Oddone EZ, Grubber JM, Olsen MK, Bosworth HB. Perceived and actual stroke risk among men with hypertension. J Clin Hypertens (Greenwich) 2008;10(4):287–94. doi: 10.1111/j.1751-7176.2008.07797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Avis NE, Smith KW, McKinlay JB. Accuracy of perceptions of heart attack risk: what influences perceptions and can they be changed? Am J Public Health. 1989;79(12):1608–12. doi: 10.2105/ajph.79.12.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147(1):41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- 31.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40(9):794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]


