Abstract
Background
Tailoring care for patients and their families at the end-of-life is an important goal. This study examined factors associated with patient choices for level of care at the end of life.
Methods
Demographic data and level of care (full code, do not resuscitate, or withdrawal of life support) were collected on 1072 patients who died from January 1998 to June 2006 on a cardiac care unit. Logistic regression was used to identify factors associated with level of care.
Results
Of 15,402 patients admitted during the study, 1072 died, comprising the study sample. Median age of blacks was 64 years (IQR, 50, 74) and whites, 70 years (IQR, 62, 78). At the time of death the level of care differed significantly in blacks versus whites. 41.8% (n = 112) of blacks versus 26.7% (n = 194) of whites chose full code (p <.0001); 37.3% (n = 96) of blacks versus 43.9% (n = 317) whites chose DNR (p = .026); and 20.9% (n=54) of blacks versus 29.3% (n=210) of whites chose withdrawal of life support (p = .005). After controlling for age, sex, diagnosis, length of intensive care stay, and length of hospital stay, blacks were more likely than whites to choose full code status at the time of death (OR 1.91 [95% CI, 2.63 – 1.39], p <0.0001).
Conclusions
Blacks are 1.9 times as likely as others to choose full code at time of death. These results suggest the need to acknowledge cultural differences when providing end of life care.
Keywords: End of life, disparities, race, withdrawal of life support, do not resuscitate, full code
Introduction
An estimated one in five American deaths now occurs in an intensive care unit (ICU).(1-4) This shift in the last half-century to dying in-hospital contributes to the burgeoning cost of healthcare, to sub-optimal family access to patients in the dying process, and to a growing need for providers to address not only critical patient care needs, but concomitant needs of families in crisis. Perhaps one of the greatest needs generated by this shift to dying-in-hospital is the need for nurses and other care providers to gain a better understanding of patient preferences for care at the end-of-life.
One particularly unique aspect of dying-in-hospital is the increased use of hospital-based technology at the end of life, and the concomitant need to withdraw it. Predictably, a steadily increasing number of ICU patients die after end-of-life decisions such as foregoing cardiopulmonary resuscitation (“do not resuscitate,” or DNR) and withholding or withdrawing care.(5-8) In current studies an estimated 90% of ICU deaths are preceded by recommendations to limit therapy,(7) with over half of those deaths ending in withholding of additional support or withdrawal of existing supportive care.(8) From 1988 to present, withdrawal of life support in the ICU has increased by up to 50%, depending on hospital and geographical region.(5;6;8)
Thus, the practices of withholding and withdrawing life support have become increasingly prevalent; yet our understanding of cultural differences in how or when patients choose when or if to withdraw support is limited. Not only do decisions about level of care at end-of-life have profound cultural and spiritual implications, they may also significantly influence, and be influenced by, cost. In the most recent major analysis of end-of-life spending trends, Lubitz and Riley found that 10-12% of the total U.S. healthcare budget and 27% of the annual Medicare budget was spent on care at the end of life.(9;10) If family members struggle to bear the burden of such costs, the implications for end-of-life care may differ.
Therefore, while recent research on end-of-life care in the ICU has assessed trends in increased rates and costs (2;3;5-8;11-18) of withholding and withdrawal of life support, the understanding of patient preferences associated with various levels of care at the end of life remains limited. As a result, factors associated with the level of care at the time of death, and in particular, culturally sensitive preferences for care, merit further investigation. Therefore, using an exploratory, retrospective review of 1072 deaths occurring over an 8-year period in a cardiac intensive care unit (CCU) of a large academic medical center in North Carolina, we sought to identify factors that might be associated with each of three levels of care at the time of death, full code, do not resuscitate and withdrawal of life support. The research question was, “what patient-level factors are associated with level of care preferences at the end of life?”
Methods
Unit-specific end of life process
On the Duke Cardiac Care Unit, when patients are identified as having a low likelihood of recovery the health care team evaluates each patient and family in an established, systematic manner. A nurse who is specifically responsible for addressing end-of-life care issues assists in guiding the communication between the health care team, patients and families. During each conference, the family’s understanding of the patient status is assessed and possible options for care are discussed. If the patient is unable to express his wishes for the goal of car at the end of life, aggressive versus comfort care, the surrogate decision maker is encouraged to speak for the patient. The risks and benefits of various treatment plans are weighed for both aggressive and comfort care. Additional conferences are held on subsequent days to evaluate the patient’s progress and the ongoing appropriateness of the treatment plan. This affords the family an opportunity to assimilate information over time. As part of this care continuum a discussion may take place regarding the option for DNR status. When appropriate, a discussion of withdrawal of life support may be initiated by either the health care team or the family. The time frame between the first and final discussions varies according to the patient status and the needs of the family.
Patient population and data collection
Patients who died while in the Cardiac Care Unit (CCU) of Duke University Hospital from Jan 1, 1998 to June 30, 2006 were prospectively recorded in a registry that included all deaths. Descriptive data, including age, sex, self-described race, length of hospital and CCU stay, hospital and CCU admission diagnoses, cause of death, and level of care at time of death were recorded for 1072 subjects who died in the CCU. While our data collection included Asian, Black, Hispanic, Native American, White, other and unknown, the numbers in all categories other than black and white were too small to be statistically significant. For this reason we collapsed racial and ethnic categories into black, white and other. Level of care at the time of death was recorded as full code, referring to patients who received aggressive life-sustaining interventions; do not resuscitate (DNR) identifying those patients who received full aggressive ICU care interventions but did not desire cardiopulmonary resuscitative efforts, even if the alternative was death; and withdrawal of life support, denoting patients who had life-supporting therapies such as vasopressors and mechanical ventilation discontinued when survival without such therapy was unlikely and the expected outcome was death.
All registry entries were made as deaths occurred, either at the time of death or as close to the time of death as possible. Additional data were obtained if necessary from the medical record and through discussions with the care nurse, house officer and attending physician. The Institutional Review Board approved the project. All subjects included in the registry were deceased, risks were deemed minimal and consent was impractical, therefore a waiver of informed consent was obtained.
Analysis
We calculated descriptive statistics to assess the frequency and distribution of patient characteristics, including: sex, age (continuous), race (Asian, Black, Hispanic, Native American, Unknown or White), length of stay (continuous), diagnosis, ventilator status (on or off a ventilator), and level of care at the time of death (full code, DNR or withdrawal of life support). We evaluated differences in descriptive patient characteristics among the three groups of care, full code, DNR and withdrawal of life support, using ANOVA for normally distributed, continuous variables (age and length of stay) and chi-square for categorical variables. Univariable analyses were conducted to determine baseline characteristics that were associated with level of care at the time of death and those variables that were significant at an alpha of .05 were chosen to enter the multivariable model. We then conducted multivariable modeling using two-step sequential logistic regression to assess these variables in combination and their relationship to level of care at the end of life. First, a multivariable logistic regression model was used to examine the association of patient characteristics with a decision to undergo full code (yes or no). Then a second logistic regression model was used to evaluate predictors of the subsequent decision to choose withdrawal of life support as compared with DNR. The sequential approach was taken in order to obtain the most information on the contribution of individual variables (parameter weights) while accounting for interactions in the models and controlling for possible confounding variables. Timing of events was not a significant contributor in univariate analyses and therefore was not included in the multivariable models. An alpha of <0.05 was established for significance. Analyses were computed using SAS version 9.
Results
Characteristics of the Sample
Patient characteristics according to end-of-life resuscitation status are summarized in Table 1.a. Overall, patient age ranged from 17 – 101 years (median, 69.0 years), 47% were women, and 25% were black. The overall length of stay in the CCU ranged from 0 – 89 days (median 3.0 days). At the time of death, 50.2% of patients (n=525) were mechanically ventilated. The most common CCU admitting diagnoses were myocardial infarction (n=432), status post cardiac arrest (n=242), respiratory failure (n=64), sepsis (n=64), congestive heart failure (n=46), and arrhythmia (n=33). Of the total population, 32.4% were full code at the time of death, 40.9% were DNR and 26.7% of deaths were preceded by withdrawal of life support. Among all deaths, the number of days prior to death (length of stay) was shortest for patients who were full code status (median 1 day, IQR 0,3) and longest for patients who chose active withdrawal of life support (median 5 days, IQR 2,10) (Table 1a.). Men and women had equal distributions of each of the three end-of-life categories (Table 1.a). There was no significant difference in the proportion of men and women who died; however, women were older at the time of death than men with a higher proportion of men in the 4th to 7th decade of life, and a higher proportion of women in the 8th and 9th decades of life.
Table 1.
a. Demographic Characteristics According to End-of-life Status
| Patient characteristics | Full Code(n=344) | DNR* (n=442) | WOLS* (n=286) | Test of Difference (p) | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Continuous Variables | Median | (IQR) | Median | (IQR) | Median | (IQR) | ANOVA |
| Age (years) | 66.0 | 56, 75 | 72.0 | 63,79 | 66.5 | 57,75 | <.0001 |
|
| |||||||
| Length of Stay (days) | 1.0 | 0,3 | 3.0 | 1,10 | 5.0 | 2,10 | <.0001 |
|
| |||||||
| Categorical | n | (%) | N | (%) | n | (%) | χ2 |
|
| |||||||
| Gender | |||||||
| Men (% of men) | 190 | 33.6 | 232 | 41.1 | 143 | 25.3 | .421 |
| Women (% of women) | 154 | 30.4 | 210 | 41.4 | 143 | 28.2 | |
|
| |||||||
| Race (% of race) | |||||||
|
| |||||||
| Asian | 4 | 100 | 0 | 0 | 0 | 0 | ** |
|
| |||||||
| Black | 112 | 41.8 | 100 | 37.3 | 56 | 20.1 | <.0001 |
|
| |||||||
| Hispanic | 2 | 66.7 | 1 | 33.3 | 0 | 0 | ** |
|
| |||||||
| Native American | 10 | 34.5 | 12 | 41.4 | 7 | 24.1 | ** |
|
| |||||||
| Other | 2 | 100.0 | 0 | 0 | 0 | 0 | ** |
|
| |||||||
| Unknown | 20 | 50.0 | 10 | 25.0 | 10 | 25.0 | ** |
|
| |||||||
| White | 194 | 26.7 | 319 | 44.0 | 213 | 29.3 | <.0001 |
|
| |||||||
| Ventilator in place % of ventilated patients) | 274 | 49.4 | 219 | 39.5 | 62 | 11.2 | <.0001 |
|
| |||||||
| CCU Diagnosis (% of each diagnostic group) | .004 | ||||||
|
| |||||||
| Anoxia | 0 | 0 | 1 | 100.0 | 0 | 0 | |
|
| |||||||
| Arrhythmia | 16 | 45.7 | 18 | 51.4 | 1 | 2.9 | |
|
| |||||||
| Cardiogenic Shock | 8 | 36.4 | 8 | 36.4 | 6 | 27.3 | |
|
| |||||||
| Cardiomyopathy | 4 | 10.8 | 14 | 37.8 | 19 | 51.4 | |
|
| |||||||
| Heart Failure | 12 | 24.5 | 27 | 55.1 | 10 | 20.4 | |
|
| |||||||
| Post Cardiac Arrest | 85 | 34.0 | 78 | 31.2 | 87 | 34.8 | |
|
| |||||||
| Respiratory Failure | 16 | 23.9 | 29 | 43.3 | 22 | 34.3 | |
|
| |||||||
| Post Respiratory Arrest | 6 | 20.7 | 13 | 44.9 | 10 | 34.5 | |
|
| |||||||
| Pneumonia | 1 | 7.7 | 6 | 46.2 | 6 | 46.2 | |
|
| |||||||
| Sepsis | 19 | 28.8 | 31 | 47.0 | 16 | 24.2 | |
|
| |||||||
| Unstable Angina | 3 | 37.5 | 3 | 37.5 | 2 | 25.0 | |
|
| |||||||
| Valvular Disease | 2 | 28.6 | 2 | 28.6 | 3 | 42.9 | |
|
| |||||||
| Multisystem Organ Failure | 3 | 50.0 | 1 | 16.7 | 2 | 33.3 | |
|
| |||||||
| Pump Failure | 7 | 22.6 | 14 | 45.2 | 10 | 32.2 | |
|
| |||||||
| Other | 4 | 21.1 | 8 | 42.1 | 7 | 36.8 | |
|
| |||||||
| Heart Transplant Rejection | 1 | 50.0 | 0 | 0 | 1 | 50.0 | |
|
| |||||||
| Myocardial Infarction | 157 | 35.7 | 189 | 43.0 | 94 | 21.4 | |
|
| |||||||
| b. Demographic Characteristics by Race
| |||||||
| Patient characteristics | Black (n=268) | White (n=726) | Other (n=78) | Tests of Difference (p) | |||
|
| |||||||
| Continuous Variables | Median | (IQR) | Median | (IQR) | Median | (IQR) | ANOVA |
|
| |||||||
| Age (years) | 64 | 50,74 | 70 | 62,78 | 66 | 58,76 | <.0001 |
|
| |||||||
| Length of Stay (days) | 2 | 1,7 | 3 | 1,7 | 2 | 1,7 | .917 |
|
| |||||||
| Categorical | n | (%) | N | (%) | n | (%) | χ2 |
|
| |||||||
| Gender | .008 | ||||||
| Men (% of race) | 121 | 45.1 | 406 | 55.9 | 38 | 48.7 | |
| Women (% of race) | 147 | 54.8 | 329 | 45.3 | 40 | 51.2 | |
|
| |||||||
| Level of Care | |||||||
|
| |||||||
| Full code (% of race) | 112 | 41.7 | 194 | 26.7 | 38 | 48.7 | <0.0001 |
|
| |||||||
| DNR (% of race) | 96 | 35.8 | 317 | 43.6 | 22 | 28.2 | .006 |
|
| |||||||
| Withdrawal of life support (% of race) | 54 | 20.1 | 210 | 28.9 | 17 | 21.7 | .013 |
|
| |||||||
| Ventilator in place (% of race) | 154 | 57.4 | 355 | 48.8 | 46 | 58.9 | .024 |
|
| |||||||
| CCU Diagnosis (% of race) | .162 | ||||||
|
| |||||||
| Anoxia | 1 | 0.3 | 0 | 0.0 | 0 | 0.0 | ** |
|
| |||||||
| Arrhythmia | 6 | 2.2 | 27 | 3.7 | 2 | 2.5 | ** |
|
| |||||||
| Cardiogenic Shock | 3 | 1.1 | 19 | 2.6 | 0 | 0.0 | ** |
|
| |||||||
| Cardiomyopathy | 6 | 2.2 | 18 | 2.4 | 3 | 3.8 | ** |
|
| |||||||
| Heart Failure | 13 | 4.8 | 31 | 4.2 | 5 | 6.4 | ** |
|
| |||||||
| Post Cardiac Arrest | 80 | 28.9 | 157 | 21.6 | 13 | 16.6 | ** |
|
| |||||||
| Respiratory Failure | 14 | 5.2 | 48 | 6.6 | 5 | 6.4 | ** |
|
| |||||||
| Post Respiratory Arrest | 8 | 2.9 | 19 | 2.6 | 2 | 2.5 | ** |
|
| |||||||
| Pneumonia | 1 | 0.3 | 11 | 1.5 | 1 | 1.2 | ** |
|
| |||||||
| Sepsis | 17 | 6.3 | 45 | 6.1 | 4 | 5.1 | ** |
|
| |||||||
| Unstable Angina | 1 | 0.3 | 6 | 0.8 | 1 | 1.2 | ** |
|
| |||||||
| Valvular Disease | 2 | 0.7 | 5 | 0.6 | 0 | 0.0 | ** |
|
| |||||||
| Multisystem Organ Failure | 1 | 0.3 | 5 | 0.6 | 0 | 0.0 | ** |
|
| |||||||
| Pump Failure | 6 | 2.2 | 25 | 3.4 | 0 | 0.0 | ** |
|
| |||||||
| Other | 6 | 2.2 | 12 | 1.6 | 1 | 1.2 | ** |
|
| |||||||
| Heart Transplant Rejection | 2 | 0.7 | 0 | 0.0 | 0 | 0.0 | ** |
|
| |||||||
| Myocardial Infarction | 101 | 37.6 | 298 | 41.0 | 41 | 52.5 | .005 |
DNR = do not resuscitate; WOLS = withdrawal of life support
Cell counts with possible expected count of < 5 were not run.
Cells with expected counts of less than 5 were not run
Patient characteristics according to race are summarized in Table 1.b. Median age was younger among blacks (64.0 years) than whites (70.5 years). The number of days prior to death (length of stay) was similar in blacks and whites across each of the three levels of care at the time of death. The rate of unexpected death, based on a subjective assessment at the time of death by the care team, was similar in blacks and whites (8.6% and 8.3%, respectively; p = 0.164). Black patients were more likely to choose full code as compared to white patients (43% versus 27%), and were less likely to choose DNR (37 % versus 44%) or withdrawal of life support (21% versus 29%) (Figure 1).
Figure 1.
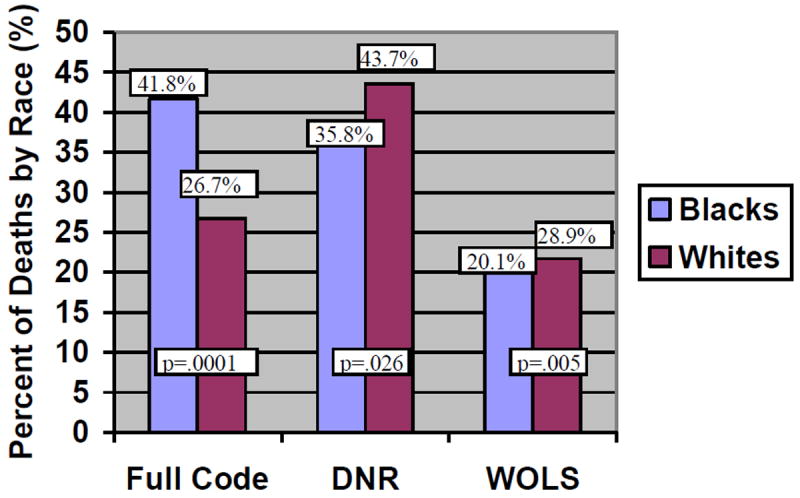
Level of Care at End of Life According to Race
*Chi Square test of difference used for group comparisons
Factors Associated With Full Code Status at the End-of-life
A univariable analysis of variable association with the full code status was first conducted to identify those variables that were significantly related to full code status, without controlling for others. Based on these findings, length of stay (Wald χ2= 42.4; O.R. 0.91 [CI,0.88-0.94], p < 0.0001), race (Wald χ2= 20.512; O.R. 1.97 [CI,1.47-2.64], p < 0.0001), and age (Wald χ2= 18.72; O.R. 0.98 [CI, 0.97-0.99], p < 0.0001) were highly associated with full code status, as were a number of admitting diagnoses.
Next, a multivariable model, the factors significantly associated with full code status after adjusting for other variables that may have influenced level of care at the time of death included: length of stay, race, age, and presence of a lethal arrhythmia on admission to the CCU (Table 2). While length of stay and age were important contributors to the model (Wald statistic, 38.58 for length of stay and 14.46 for age), and were both statistically significant (p < .0001), the relationship with full code status was similar for race (Wald statistic 22.96, OR 1.91 for black versus white).
Table 2.
Predictors of Full Code Status in Cardiac Care Unit Patients at the End-of-life
| Predictor | Full Code (n=1072)a | |||
|---|---|---|---|---|
| Variables | Wald | OR | 95% (CI) | p-value |
| Gender (female vs. male) | 2.49 | 0.80 | 0.61, 1.06 | .12 |
| Age (every 10 yrs) | 14.46 | 0.82 | 0.74, 0.89 | <.0001 |
| Race | ||||
| Black vs. White | 22.96 | 1.91 | 1.39, 2.63 | <.0001 |
| Black vs. Other | 5.91 | 1.35 | 0.43, 1.28 | .02 |
| Length of Stay (per day) | 38.58 | 0.91 | 0.88, 0.94 | <.0001 |
| Diagnosis | ||||
| Arrhythmia | 5.10 | 1.70 | 0.82, 3.53 | .01 |
| Cardiac Arrest | 0.14 | 0.76 | 0.54, 1.08 | .71 |
| Cardiomyopathy | 2.49 | 0.31 | 0.10, 0.94 | .12 |
| Chronic Heart Failure | 0.42 | 0.56 | 0.27, 1.15 | .58 |
| Other | 0.23 | 0.63 | 0.42, 0.94 | .63 |
| Respiratory arrest | 0.01 | 0.68 | 0.36, 1.28 | .91 |
| Pump failure | 1.88 | 1.98 | 0.38, 10.21 | .17 |
| Sepsis | 1.45 | 0.22 | 0.028, 1.80 | .23 |
c-statistic = .72
For length of stay, each incremental day of CCU stay decreased the likelihood of being full code status by only 9% (O.R. 0.91 [95% CI, 0.88-0.94], p < .0001). For age, each incremental decade of life decreased the likelihood of being full code status by 18% (O.R. 0.82 [95% CI, 0.74-0.90], p < .0001). By contrast, blacks were almost twice as likely (O.R. 1.91) as whites and others to choose full code status, even after controlling for other variables that may have influenced the relationship, such as length of stay in the CCU, age and diagnosis on admission.
In the second step of the sequential logistic regression analysis, factors associated with withdrawal from life support were evaluated (Table 3). Again, race was a significant, independent contributor, with blacks half as likely to choose withdrawal of life support as compared to whites (OR 0.54 [95% CI, 0.38 – 0.78], p = 0.006). Other variables associated with level of care at end-of-life remained important predictors of withdrawal of support, including age, length of stay and diagnosis.
Table 3.
Factors Associated With Withdrawal of Life Support as Compared to DNR
| Predictor | Withdrawal of Life Support (n = 728)a | |||
|---|---|---|---|---|
| Variables | Wald | OR | 95% (CI) | p-value |
| Gender Female vs male | 2.80 | 1.28 | 0.96, 1.70 | .09 |
| Age per 10 yrs | 4.80 | 0.90 | 0.80, 0.99 | .03 |
| Race | ||||
| Black vs. White | 7.71 | 0.54 | 0.38, 0.78 | .01 |
| Black vs. Other | 0.15 | 0.83 | 0.44, 1.57 | .70 |
| Length of Stay (per day) | 19.43 | 1.047 | 1.02, 1.05 | <.0001 |
| Diagnosis | ||||
| Arrhythmia | 6.35 | 0.11 | 0.02, 0.84 | .01 |
| Cardiac Arrest | 8.33 | 2.11 | 1.47, 3.02 | .004 |
| Cardiomyopathy | 0.51 | 1.52 | 0.64, 3.62 | .47 |
| Chronic heart failure | 0.52 | 0.86 | 0.41, 1.84 | .47 |
| Other | 1.52 | 1.50 | 1.00, 2.23 | .22 |
| Respiratory arrest | 1.05 | 1.53 | 0.86, 2.71 | .31 |
| Pump failure | 0.16 | 1.54 | 0.27, 8.76 | .69 |
| Sepsis | 0.53 | 2.68 | 0.86, 8.36 | .10 |
c statistic = .67
Discussion
Findings in this study suggest that preferences for care at the end-of-life differ significantly according to race, and also, though to a lesser extent, according to length of stay and age. Blacks are more likely to choose full code status over DNR or withdrawal of life support, as compared to whites. Similar findings regarding racial differences in preferences for end of life care have been reported in other settings, such as primary care,(19) nursing homes (20) and hospice.(21) These prior studies suggest that blacks are less likely to complete advance directives or to pursue hospice and related types of palliative care at the end of life. Our findings show that, similar to nursing homes and hospice settings, in a critical care setting blacks are also less likely to limit aggressive care, and significantly more likely to choose full code, as compared to others.
Race and Level of Care at the End-of-life
Although blacks reportedly receive fewer invasive interventions at the time of diagnosis, particularly interventional procedures such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG),(22-26) the data from our study suggest that near the end-of-life blacks more frequently chose aggressive supportive care. Similarly, a nationwide study of 10,122 deaths found that blacks were more likely to die in a hospital than whites (70.4% vs. 55.1%). These findings are consistent with our data, and suggest that black race is associated with more aggressive end-of-life care. Similar to our study, in the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) study, 30% of white patients did not want cardiopulmonary resuscitation (CPR) compared with 19% of non-white patients (RR 1.62; 95% CI: 1.3-2.1).(27)
Length of Stay and Level of Care at the End-of-Life
Length of stay was also significantly associated with level of care; however the timing of death increased across the care groups, with full codes being shortest and withdrawal of support being the longest (Table 1.a.). The median length of stay prior to death for patients who were full code was one day, for DNR status the median time to death was three days, and for withdrawal of life support five days. The relationship was not unexpected since the situations surrounding full code often leave little time for lengthy discussions and require rapid decision-making. Other studies evaluating length of stay as it relates to withdrawal of life support are few, and we found only one published study evaluating this relationship in an intensive care setting.(18) Consistent with our reflections on this finding, Wunsch and colleagues found that, on average, the length of stay in patients who choose withdrawal of life support is longer, due in part to the families’ need to process the situation and the finality of the end of life.(18)
Age, Sex and Level of Care at the End-of-life
Age was also associated with level of care at the end-of-life. As age increased, full code orders were less common than either DNR or withdrawal of life support. These findings are consistent with the SUPPORT study, which interviewed 1650 patients on resuscitation preferences,(26;27) finding that patients who did not want cardiopulmonary resuscitation (CPR) were older (mean 65.6 vs. 60.3 years, p<.001); 36.7% of patients who had “do not resuscitate status” and did not want CPR were 70–79 years of age.
A six-year difference in the median age of blacks versus whites was observed, with blacks being younger than whites. The younger age of blacks at the time of death may have contributed to choosing a more aggressive approach to care at the end-of-life. However, it is important to note that the life expectancy among blacks in the U.S. is 5 years lower, on average, as compared to whites (69 years on average for black men, as compared to 75.3 among white men)(28); suggesting that the patients in our study are consistent with national population with regard to age at the time of death.(29)
In our analysis, the proportions of levels of care at the time of death were similar among men and women, and sex was not significantly associated with level of care in multivariable modeling. Similarly, in the literature, patient sex has not been independently associated with level of care at the time of death.(5;18) However, women in most studies are older at the time of death than men, as was true in our study.(2;30)
Implications for Practice
Our study was not designed to determine the specific factors underpinning the observed association of race with end-of-life decisions. Literature suggests three major reasons, including spirituality, distrust of the healthcare delivery system and the collective community that influence end-of-life decisions making among blacks. Because spirituality is widely reported to be a fundamental tool for coping with the experience of death, particularly among blacks (31;32), the results of our study may not be surprising. Understanding the nature and importance of black spirituality may allow us to assist black patients and families through the death and dying process in a manner that is harmonious with their culture.
Distrust of the healthcare delivery system may also be an important factor in decision-making at the end-of-life among blacks. The historical root of distrust stems from generations of perceptions of unequally rendered services, abuses in medical experimentation, and economic injustice.(33) Such perceptions have led to a general loss of credibility of health care providers and institutions.
A third factor that may influence decision-making by blacks at the end-of-life is the collective community.(31) Black culture places a strong value on the “collective” or family, friends and the faith community. Honoring members of this community, especially family, is a central focus of the “collective” culture and decisions made without consensus of the community is considered disrespectful. Arranging for inclusion of family members, faith community and clergy in discussions and decision-making is an important way to assist black patients at the end-of-life.
Other possible reasons for differences in end of life choices include our approach in discussing end-of-life; the patient and family understanding of the choices at end-of-life; patient and family circumstances or previous experience with end-of-life decision-making; or differences in beliefs regarding appropriate care at end-of-life. Although our standard unit approach is consistent for all patients, the specific course that discussions take is unique and tailored to meet the needs of the individual patient and family. Tailoring that occurred in the context of care to address the specific needs of the patient and family included varying the actual time-line for decision-making; addressing families’ past experience with hospitalized family members, illness and death; and using effective communication techniques to work closely with individual family dynamics. Each of these variations may influence the tailored approach taken in planning the continuum of care at the end-of-life.
Limitations
Because data were collected in a cardiac intensive care unit, and only on patients who died, the results may be specific to this patient population. Our findings may be a reflection of cultural differences in the southeastern United States, and may not be generalizable to other regions of the United States. A third limitation is the inability to evaluate the degree to which findings may be confounded by educational or socio-economic factors. While we recognize the importance of the relationship between socio-economic status (SES) and end of life preferences (34), we did not collect individual-level socioeconomic data in this study. However, we know that of all cardiac patients cared for at Duke University Hospital, 35% are black and 58% are white, and that this is a proportionally accurate representation of Durham County.(35) Of those Durham county residents, a higher percentage of blacks are at poverty level (20% of blacks and 8.5% of whites, respectively), and are unemployed (8.9% of blacks and 2.7% of whites, respectively).(35) These data suggest that black patients represented in this study were likely to be disproportionately socio-economically disadvantaged as compared to whites. If so, as suggested by Volandes and colleagues, this disadvantage may affect their health literacy levels and be reflected in their choices for care at the end-of-life.(34)
In addition, patients whose end-of-life care began in the cardiac care unit but ended in another unit were not captured in this dataset. It is also possible that patients who died prior to having the opportunity to complete an advanced directive could result in the appearance of lower DNR rates at the time of death. However, we do not suspect any systematic bias related to age, sex or race in transfer of these patients from the CCU, nor do we expect differential patterns of death by race that would materially change our results.
Conclusions
In the cardiac intensive care setting where terminal disease is common, we have found that race has a significant association with level of care at the end of life. When controlling for other variables including age, gender, length of stay and admitting diagnosis, blacks were more likely than whites to choose a status of full code. Sensitivity to this difference may be important to providing better end-of-life care.
Acknowledgments
Funded in part by a Clinical Practice Grant from the American Association of Critical Care Nurses (AACN).
Reference List
- 1.Flory J, Yinong YX, Gurol I, Levinsky N, Ash A, Emanuel E. Place of death: U.S. trends since 1980. Health Aff (Millwood) 2004 May;23(3):194–200. doi: 10.1377/hlthaff.23.3.194. [DOI] [PubMed] [Google Scholar]
- 2.Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004 Mar;32(3):638–43. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 3.Solloway M, LaFrance S, Bakitas M, Gerken M. A chart review of seven hundred eighty-two deaths in hospitals, nursing homes, and hospice/home care. J Palliat Med. 2005 Aug;8(4):789–96. doi: 10.1089/jpm.2005.8.789. [DOI] [PubMed] [Google Scholar]
- 4.Weitzen S, Teno JM, Fennell M, Mor V. Factors associated with site of death: a national study of where people die. Med Care. 2003 Feb;41(2):323–35. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- 5.Azoulay E, Pochard F, Garrouste-Org Moreau D, Montesino L, Adrie C, et al. Decisions to forgo life-sustaining therapy in ICU patients independently predict hospital death. Intensive Care Med. 2003 Nov;29(11):1895–901. doi: 10.1007/s00134-003-1989-3. [DOI] [PubMed] [Google Scholar]
- 6.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998 Oct;158(4):1163–7. doi: 10.1164/ajrccm.158.4.9801108. [DOI] [PubMed] [Google Scholar]
- 7.Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med. 1997 Jan;155(1):15–20. doi: 10.1164/ajrccm.155.1.9001282. [DOI] [PubMed] [Google Scholar]
- 8.McLean RF, Tarshis J, Mazer CD, Szalai JP. Death in two Canadian intensive care units: institutional difference and changes over time. Crit Care Med. 2000 Jan;28(1):100–3. doi: 10.1097/00003246-200001000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993 Apr 15;328(15):1092–6. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- 10.Hogan C, Lunney J, Gabel J, Lynn J. Medicare beneficiaries’ costs of care in the last year of life. Health Aff (Millwood) 2001 Jul;20(4):188–95. doi: 10.1377/hlthaff.20.4.188. [DOI] [PubMed] [Google Scholar]
- 11.Bacchetta MD, Eachempati SR, Fins JJ, Hydo L, Barie PS. Factors influencing DNR decision-making in a surgical ICU. J Am Coll Surg. 2006 Jun;202(6):995–1000. doi: 10.1016/j.jamcollsurg.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 12.Hall RI, Rocker GM, Murray D. Simple changes can improve conduct of end-of-life care in the intensive care unit. Can J Anaesth. 2004 Jun;51(6):631–6. doi: 10.1007/BF03018408. [DOI] [PubMed] [Google Scholar]
- 13.Holzapfel L, Demingeon G, Piralla B, Biot L, Nallet B. A four-step protocol for limitation of treatment in terminal care. An observational study in 475 intensive care unit patients. Intensive Care Med. 2002 Sep;28(9):1309–15. doi: 10.1007/s00134-002-1370-y. [DOI] [PubMed] [Google Scholar]
- 14.Jayes RL, Zimmerman JE, Wagner DP, Draper EA, Knaus WA. Do-not-resuscitate orders in intensive care units. Current practices and recent changes. JAMA. 1993 Nov 10;270(18):2213–7. [PubMed] [Google Scholar]
- 15.Knaus WA, Wagner DP, Zimmerman JE, Draper EA. Variations in mortality and length of stay in intensive care units. Ann Intern Med. 1993 May 15;118(10):753–61. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- 16.Lindgren VA, Barnett SD, Bloom RL. Who is dying in our critical care units? A single center’s experience. J Nurs Care Qual. 2006 Jan;21(1):78–85. doi: 10.1097/00001786-200601000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Rady MY, Johnson DJ. Admission to intensive care unit at the end-of-life: is it an informed decision? Palliat Med. 2004 Dec;18(8):705–11. doi: 10.1191/0269216304pm959oa. [DOI] [PubMed] [Google Scholar]
- 18.Wunsch H, Harrison DA, Harvey S, Rowan K. End-of-life decisions: a cohort study of the withdrawal of all active treatment in intensive care units in the United Kingdom. Intensive Care Med. 2005 Jun;31(6):823–31. doi: 10.1007/s00134-005-2644-y. [DOI] [PubMed] [Google Scholar]
- 19.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008 Oct;56(10):1953–8. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Messinger-Rapport BJ, Kamel HK. Predictors of do not resuscitate orders in the nursing home. J Am Med Dir Assoc. 2005 Jan;6(1):18–21. doi: 10.1016/j.jamda.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Johnson KS, Kuchibhatla M, Tanis D, Tulsky JA. Racial differences in hospice revocation to pursue aggressive care. Arch Intern Med. 2008 Jan 28;168(2):218–24. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]
- 22.Welch LC, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005 Jul;53(7):1145–53. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 23.Peterson ED, Lansky AJ, Anstrom KJ, Muhlbaier LH, Popma JJ, Satler LF, et al. Evolving trends in interventional device use and outcomes: results from the National Cardiovascular Network Database. Am Heart J. 2000 Feb;139(2 Pt 1):198–207. doi: 10.1067/mhj.2000.103848. [DOI] [PubMed] [Google Scholar]
- 24.East MA, Peterson ED. Understanding racial differences in cardiovascular care and outcomes: issues for the new millennium. Am Heart J. 2000 May;139(5):764–6. doi: 10.1016/s0002-8703(00)90004-8. [DOI] [PubMed] [Google Scholar]
- 25.Rao SV, Shaw RE, Brindis RG, Klein LW, Weintraub WS, Krone RJ, et al. Patterns and outcomes of drug-eluting coronary stent use in clinical practice. Am Heart J. 2006 Aug;152(2):321–6. doi: 10.1016/j.ahj.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Borum ML, Lynn J, Zhong Z. The effects of patient race on outcomes in seriously ill patients in SUPPORT: an overview of economic impact, medical intervention, and end-of-life decisions. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000 May;48(5 Suppl):S194–S198. doi: 10.1111/j.1532-5415.2000.tb03132.x. [DOI] [PubMed] [Google Scholar]
- 27.A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995 Nov 22;274(20):1591–8. [PubMed] [Google Scholar]
- 28.Harper S, Lynch J, Burris S, Davey SG. Trends in the black-white life expectancy gap in the United States, 1983-2003. JAMA. 2007 Mar 21;297(11):1224–32. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 29.American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Dallas, Tex.: American Heart Association; 2004. [Google Scholar]
- 30.Arias E. United States life tables, 2004. Natl Vital Stat Rep. 2007 Dec 28;56(9):1–39. [PubMed] [Google Scholar]
- 31.Johnson KS, Elbert-Avila KI, Tulsky JA. The influence of spiritual beliefs and practices on the treatment preferences of African Americans: a review of the literature. J Am Geriatr Soc. 2005 Apr;53(4):711–9. doi: 10.1111/j.1532-5415.2005.53224.x. [DOI] [PubMed] [Google Scholar]
- 32.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004 Apr;7(2):247–56. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 33.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. JAMA. 2000 Nov 15;284(19):2518–21. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 34.Volandes AE, Paasche-Orlow M, Gillick MR, Cook EF, Shaykevich S, Abbo ED, et al. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008 Jun;11(5):754–62. doi: 10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- 35.Regenstein M, Lara A, Trott J, Cyprien S. A Preview of Heart Care in Durham, North Carolina: Implications for African American and Latino Residents. For the Robert Wood Johnson Foundation, CV Bulletin, and the George Washington University Department of Health Policy; 2006. [Google Scholar]


