Abstract
Background:
General anesthesia (GA) is the most frequently used technique for lumbar spine disc surgery. The aim of this study was to compare the intraoperative variables and postoperative outcome after GA and combined general/epidural anesthesia (CEG) in patients undergoing elective lumbar spine disk surgery.
Methods:
Eighty patients who underwent one or two level of laminectomy/discectomy during a 2 year period were enrolled in this randomized controlled trial (RCT). They were randomly selected to undergo GA or CEG. The data recorded during surgery were: The patients’ heart rate (HR), mean arterial blood pressure (MABP), amount of blood loss, and the medication used during anesthesia. The severity of pain score, total analgesic consumption, and complications were recorded in the postoperative period.
Results:
The MABP, HR, blood loss, and anesthetic medication were significantly lower in CEG group in comparison with that of GA group. In the postoperative period, the pain score and total analgesic requirement was lower in the CEG group and less complication were encountered in this group.
Conclusion:
The results of this study revealed that CEG have some advantages over GA in reducing the blood loss and anesthetic medication during the operation and it is also more effective in control of pain with fewer complications during the postoperative period.
Keywords: Bupivacaine, combined epidural/general anesthesia, fentanyl, laminectomy, pain
INTRODUCTION
Lumbar laminectomy and discectomy is most commonly performed under general anesthesia (GA). This technique can be accompanied by several perioperative morbidities including blood loss, postoperative pain, nausea, vomiting, and prolonged postanesthesia recovery period.[7] Patient's satisfaction and the ability to carry out prolonged operations in prone position without airway compromise are the main advantages of using GA.[2]
Techniques of regional anesthesia (RA) alone or epidural anesthesia (EA), may reduce the amount of blood loss, which is an effect of decreased peripheral venous pressure after RA and may also lower the incidence of pulmonary complications.[10,12]
This prospective study was conducted to compare the anesthetic, analgesic, and postoperative side effects of GA versus combined epidural/general anesthesia (CEG) in patients undergoing laminectomy for one or two level disc disease. We hypothesized that the CEG would be more suitable and effective, with less blood loss and less amount of anesthetic medications and it would provide more satisfactory postoperative analgesia after lumbar laminectomy.
MATERIALS AND METHODS
After the project was approved by the institutional review board and written-informed consent prepared for the patients being enrolled for elective lumbar laminectomy/discectomy, 80 patients undergoing lumbar one or two level laminectomy/discectomy for the first time were enrolled. The exclusion criteria were, contraindications for EA, that is, patient refusal, local infection, bleeding diathesis. Patients were randomly allocated into GA or CEG groups using sealed envelopes method with 40 patients in each group. A single anesthesiologist handled all the anesthesia procedures. The patients receiving EA were given a single injection of 18 ml bupivacaine 0.25% (45 mg) plus100 μg of fentanyl (2 ml) in 18 ml of distilled water. The injection performed at the same level or one level below of the surgery in sitting position, using18-gauge Tuohy needle. All patients receiving GA were induced with Thiopental (4-5 mg/kg), fentanyl (2 μg/kg), midazolam (0.05 mg/kg), and atracurium (0.5 mg/kg). For maintaining the anesthesia, combination of N2O/O2 Isoflurane and fentanyl 1 μg/kg/hour was used. The percent of Isoflurane was changed on the basis of bispectral index score (BIS) 40-60.[13] All the patients were operated in prone position. The heart rate (HR), systolic, diastolic, mean arterial blood pressure (MABP), oxygen saturation, and depth of anesthesia were monitored using BIS index throughout the surgery. All the surgeries were carried out by a single surgeon. The age, sex, height, weight, and American society of anesthesiologists physical status (ASA) were recorded.
Hypotension or bradycardia was defined as HR <60, and MABP <65 mmHg and treated with atropine or ephedrine 5 mg IV.
Blood loss was measured in routine manner by calculating the volume of blood suctioned from the surgical field and blood collected by sponges. The volume of blood transfusion was calculated by enumerating the blood bags injected during the operation. The percentile of Isoflurane used for GA was also recorded.
After extubation, the patients were transferred to the postanesthesia care unit (PACU) where an anesthetist and a nurse unaware of the study protocol observed the patients. Pain scores were evaluated by a blinded observer anesthesiologist at the time of arrival in the PACU, and 10, 20, and 30 minutes thereafter using visual analogue scale (VAS) (0-10 cm: 0 = no pain, 10 = the worst pain possible). Postoperative pain score (VAS score), the first time and dosage of analgesic given and total analgesic requirement for the first 24 hours were recorded. Rescue analgesia with injection of morphine 2 mg was given intravenously to a maximum total dose of 10 mg when pain score exceeded 4. Any complication such as nausea, vomiting, and catheter-related bladder discomforts (CRBD) occurring in the PACU were also recorded.
Statistical analysis
To analyze the effect of different binary values of variants x2 test was used. Simple linear regression test was used for analysis of multiple effective variants. Repeated data were analyzed using repeated measure analysis of variance (ANOVA). All statistical analysis were done using SPSS (version 17 Chicago, IL) and statistical significance was defined as P < 0.05.
RESULTS
Eighty patients were enrolled in this study with rather similar demographic characteristics in both groups [Table 1]. The age range varied from 24 to 66 years with a mean age of 45.0 years. The mean intraoperative blood pressure and HR was significantly higher in the GA group as compared with the CEG group [Figures 1 and 2]. In the CEG group and at the beginning of surgery, there were hypotension and bradycardia in 25% of patients, which needed atropine or ephedrine injection.
Table 1.
Patient characteristics in the two groups
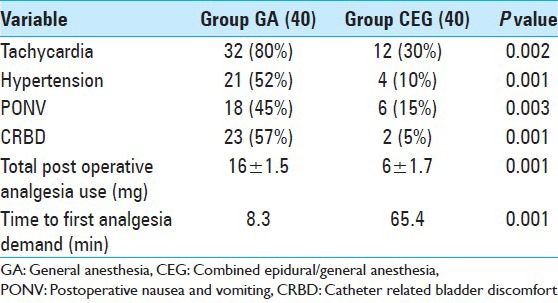
Figure 1.
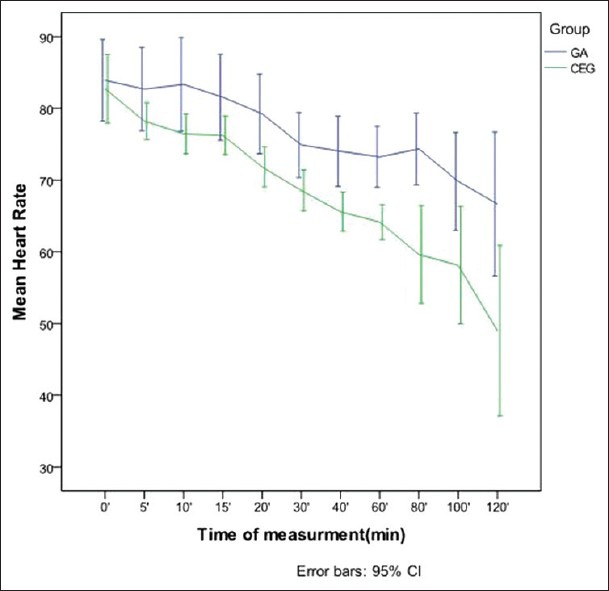
Intraoperative heart rate data (P> 0.05)
Figure 2.
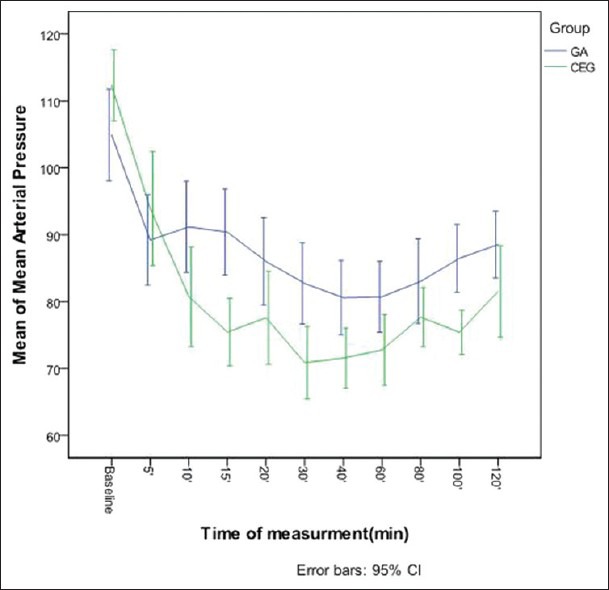
Intraoperative mean arterial pressure data (P = 0.004)
The mean intraoperative blood loss was significantly lower in the CEG group in comparison with that of GA group (P = 0.002). This significance was present after controlling for other variables (age, sex, weight) in linear regression analysis (b = −121.147, P = 0.047). In addition, less allogeneic blood was transfused in the CGA group than in the GA group (0.12 blood units transfused vs. 0.72 blood units; P = 0.006).
The mean percent of anesthetic agent (Isoflurane) that was used during surgery in the CGA group was significantly lower in comparison with that of the GA group (0.67 ± 0.15 vs. 1.23 ± 0.25 P < 0.001).
During the postoperative period, there were no major cardiopulmonary complications in either group, whereas at PACU admission, tachycardia, hypertension, nausea, vomiting, and CRBD were more frequent in those undergoing GA [Table 2].
Table 2.
Postoperative outcomes in the two groups
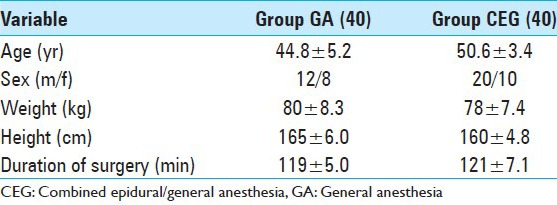
In the PACU, the mean pain scores [Figure 3] in CEG group was significantly lower in comparison with that of GA group (P < 0.01) and analgesic requirements (GA: 72.3%, CEG: 18.6%, P < 0.001) were higher in the GA group [Table 2]. Time to first rescue analgesia in the postoperative period was significantly longer in CEG group (P = 0.001) [Table 2]. The total amount of morphine used during the 24 hours of study was significantly higher in the GA group than in the CEG group (P = 0.001) [Table 2].
Figure 3.
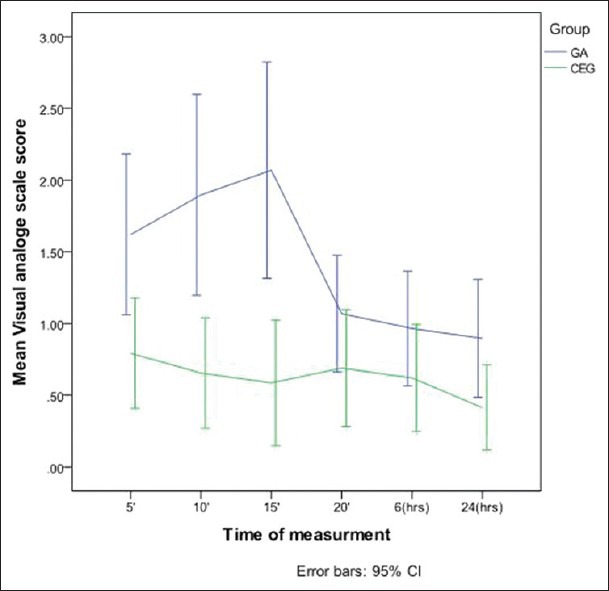
The mean of visual analog scale scores after surgery
DISCUSSION
In spinal surgery, GA and various forms of RA, either spinal anesthesia (SA) or EA have been in use for decades as successful alternatives. A good anesthetic technique should have both rapid onset and reversal of effects. It should provide desirable intraoperative hemodynamic conditions and, if possible, contribute to reduced demand for blood transfusion. Moreover, it should permit the earliest possible discharge from the PACU and minimize the common postoperative problems such as pain, analgesics consumption, nausea, and vomiting.[11] Reduced intraoperative hypertensive episodes, decreased blood loss, and less postoperative pain and nausea are among the many reported advantages of SA and EA compared with GA in patients undergoing lumbar laminectomy.
GA is the method of choice for spinal procedures according to some authors.[8] This concept either may be related to the lack of familiarity with the use of RA in such procedures or may reflect the uncertainty concerning the potential risks and complications incurred when spinal operations are carried out.
The CEG is an efficient technique that offers many advantages for the patient undergoing lumbar spine surgery.[14] CEG with using a deliberate hypotension led to a significant reduction of blood loss (35% reduction of bleeding) and more satisfactions of the patient and surgeon as in our study.
Demirel et al. randomized 60 patients undergoing discectomy or laminectomy into two groups, which received either GA or EA. The latter, was considered superior to GA with fewer episodes of hypertension and less blood loss.[6]
Patients undergoing lumbar laminectomy, usually experience severe pain postoperatively. Several studies have evaluated the use of epidural injections for postoperative analgesia after lumbar laminectomy and found that this technique was superior to IM or IV injection of analgesic medications using patient control analgesia systems.[3] Bourke et al.[4] stated that the patients who received epidural morphine for laminectomy under GA reported less pain on the VAS score. They were evaluated as having less pain by their nurses, and they required less opioid analgesic pain medication in the immediate postoperative period. We were used to such technique previously and that was an initiation for developing this randomized controlled trial (RCT) also.
Cherng et al.[5] showed that epidural fentanyl accelerates the onset time of sensory and motor blockades during the epidural ropivacaine anesthesia. They suggest that fentanyl might stop the nerve conduction in spinal roots. In the present study, it is well demonstrated that induced hypotension, with lower amount of blood loss, less amount of anesthetic medications used during surgery, lower prevalence of tachycardia and hypertension in the recovery room, less pain leading in the lower demand of the patient for analgesics during the recovery period were reported in patients undergoing CEG, significantly [Tables 1 and 2]. In our study, we used epidural fentanyl injection, as a supplement for RA. Fentanyl can enhance sensory and motor blockades in EA, due to its rapid onset of action in spinal roots and dorsal ganglia.[9] The high incidence of hypotension in CEG may be due to the addition of fentanyl to local anesthetic.
CRBD is common in patients awakening from anesthesia who have had urinary catheterization during operation and often complain an urge to void or discomfort in the suprapubic region in the postoperative period.[1] The urinary bladder receives cholinergic innervations by the pelvic nerves and adrenergic innervations by the hypogastric nerve. In our study, blocking the pelvic nerve plexuses by local anesthetics in CEG group could lower the incidence of CRBD in recovery room significantly.
Limitations of this study
The main limitation of this study would be the small number of the cases included in this preliminary report and it will be tried to continue on the trial in further research protocols.
CONCLUSION
Addition of EA can lower the need for the anesthetic agents during CEG and lower the blood loss during lumbar laminectomy and discectomy and the intensity of pain score after these surgeries.
ACKNOWLEDGMENT
The authors acknowledge the support of the Research and Development Center of Sina Hospital for their technical assistance.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/105/116683
Disclaimer: The authors of this article has no conflict of interest to disclose, and has adhered to SNI's policies regarding human/animal rights, and informed consent. Advertisers in SNI did not ask for, nor did they receive access to this article prior to publication
Contributor Information
Mohammad Reza Khajavi, Email: khajavim@tums.ac.ir.
Mohammad Amir Asadian, Email: asadian.ma@gmail.com.
Farsad Imani, Email: imanifar@tums.ac.ir.
Farhad Etezadi, Email: etezadi@tums.ac.ir.
Reza Shariat Moharari, Email: moharari@tums.ac.ir.
Abbas Amirjamshidi, Email: abamirjamshidi@yahoo.com.
REFERENCES
- 1.Agarwal A, Gupta D, Kumar M, Dhiraaj S, Tandon M, Singh PK. Ketamine for treatment of catheter related bladder discomfort: A prospective, randomized, placebo controlled and double blind study. Br J Anaesth. 2006;96:587–9. doi: 10.1093/bja/ael048. [DOI] [PubMed] [Google Scholar]
- 2.Attari M, Mirhosseini A, Honarmand A, Safavi M. Spinal anesthesia versus general anesthesia for elective lumbar spine surgery: A randomized clinical trial. J Res Med Sci. 2011;164:524–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Bonhomme V, Doll A, Dewandre PY, Brichant JF, Ghassempour K, Hans P. Epidural administration of low-dose morphine combined with clonidine for postoperative analgesia after lumbar disc surgery. J Neurosurg Anesthesiol. 2002;14:1–6. doi: 10.1097/00008506-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bourke DL, Spatz E, Motara R, Ordia JI, Reed J, Hlavacek JM. Epidural opioids during laminectomy surgery for postoperative pain. J Clin Anesth. 1992;4:277–81. doi: 10.1016/0952-8180(92)90128-n. [DOI] [PubMed] [Google Scholar]
- 5.Cherng CH, Yang CP, Wong CS. Epidural Fentanyl speeds the onset of sensory and motor blocks during epidural Ropivacaine anesthesia. AnesthAnalg. 2005;101:1834–7. doi: 10.1213/01.ANE.0000184131.06529.35. [DOI] [PubMed] [Google Scholar]
- 6.Demirel CB, Kalayci M, Ozkocak I, Altunkaya H, Ozer Y, Acikgoz B. A prospective randomized study comparing perioperative outcome variables after epidural or general anesthesia for lumbar disc surgery. J Neurosurg Anesthesiol. 2003;15:185–92. doi: 10.1097/00008506-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Gulur P, Nishimori M, Ballantyne JC. Regional anaesthesia versus general anaesthesia, morbidity and mortality. Best Pract Res Clin Anaesthesiol. 2006;20:249–63. doi: 10.1016/j.bpa.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Jellish WS, Thalji Z, Stevenson K, Shea J. A prospective randomized study comparing short and intermediate term perioperative outcome variables after spinal or general anesthesia for lumbar disk and laminectomy surgery. Anesth Analg. 1996;83:559–64. doi: 10.1097/00000539-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Moharari RS, Sadeghi J, Khajavi MR, Davari ME, Mojtahedzadeh M. Fentanyl supplement expedites the onset time of sensory and motor blocking in interscalenelidocaine anesthesia. Daru. 2010;18:298–302. [PMC free article] [PubMed] [Google Scholar]
- 10.Papadopoulos EC, Girardi FP, Sama A, Pappou IP, Urban MK, Cammisa FP., Jr Lumbar microdiscectomy under epidural anesthesia: A comparison study. Spine J. 2006;6:561–4. doi: 10.1016/j.spinee.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Riegel B, Alibert F, Becq MC, Duckert I, Krivosic-Horber R. Lumbar disc herniation with surgical option: General versus local anesthesia. Agressologie. 1994;34:33–7. [PubMed] [Google Scholar]
- 12.Sadrolsadat SH, Mahdavi AR, Moharari RS, Khajavi MR, Khashayar P, Najafi A, et al. A prospective randomized trial comparing the technique of spinal and general anesthesia for lumbar disk surgery: A study of 100 cases. Surg Neurol. 2009;71:60–5. doi: 10.1016/j.surneu.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Shariat Moharari R, Samadi A, Imani F, Panah Khahi M, Khashayar P, Meysamie A, et al. The effect of epidural Bupivacaine on Bis levels in the awake phase and on the maintenance doses of Propofol and Fentanyl during general anesthesia. Anesth Pain. 2013;2:149–53. doi: 10.5812/aapm.5461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.William F, Urme Y. Combined regional and general anesthesia for orthopedic spine fusion surgery. Tech Reg Anesth Pain Manag. 2000;4:101–5. [Google Scholar]


