Abstract
Objectives
The aim of this study was to review the epidemiologic data of rubella and congenital rubella syndrome (CRS) supplied by surveillance systems from 2001 to 2009 and to propose measures to improve the quality of the surveillance system in the Republic of Korea.
Methods
The epidemiological data for rubella and CRS cases reported to the Korea Centers for Disease Control and Prevention from 2001 to 2009 were retrospectively reviewed, and insurance reimbursement data from the Korea National Health Insurance Review Agency were collected for comparison.
Results
The number of yearly reported rubella cases to the Korea Centers for Disease Control and Prevention from 2001 to 2009 was 128, 24, 8, 24, 15, 12, 35, 30, and 36, respectively. The occurrence of rubella shifted to a slightly higher age group during the 9-year period, i.e. from 0–9 years to 10–19 years. Among the 309 reported rubella cases, three were confirmed cases of CRS. In addition, according to data sourced from Health Insurance Review Agency, 24, 19, 19, 9, and 5 CRS cases were reported for medical insurance reimbursement from 2005 to 2009, respectively.
Conclusion
According to available surveillance data, the reported cases of rubella and CRS were not high, but a more detailed surveillance with emphasis on susceptible women of childbearing age is necessary for better monitoring and control of rubella and CRS in the Republic of Korea.
Key words: congenital rubella syndrome, monitor, rubella, surveillance
1. Introduction
Rubella, a mild febrile viral exanthematous disease, is an important public health concern because of its association with congenital rubella syndrome (CRS), which can result in miscarriage, stillbirth, and multiple birth defects including deafness, blindness, heart disease, and mental retardation.1 Although rubella itself is a well-controlled disease that is preventable through vaccination in some nations,2,3 widespread epidemics of the disease and significant morbidity and mortality from CRS still exist in other parts of the world.4,5
Since its introduction in the 1960s, vaccination against rubella was a significant factor in the prevention of rubella and CRS. Two different strategies have been used to control rubella and CRS: in the United States, all infants from 12 to 15 months of age are vaccinated,6 whereas in the United Kingdom, susceptible women of childbearing age are vaccinated.7 Both strategies were partially successful, which prompted the strategies to be revised to include vaccination of both populations (i.e. 12–15-month-old infants and susceptible women of childbearing age) by means of a universal dual vaccination strategy.8 On the other hand, a comprehensive two-dose measles-mumps-rubella (MMR) vaccination program along with national surveillance and high vaccination coverage, as implemented in Finland, has led to success in the elimination of rubella and CRS in that country.9
In the Republic of Korea, the vaccine for rubella was first introduced in a monovalent form in 1978 and became standard in 1982 when the MMR combination vaccine was introduced. The MMR vaccine was recommended for all infants aged 15 months, but the actual vaccine coverage rate was not known. In 1997, a second dose of MMR was added to the schedule for children aged 4–6 years, in addition to the dose received at 12–15 months. However, because of insufficient policies to promote the second-dose coverage, the two-dose MMR vaccine coverage rate was low at 39% in 200110 and thus resulted in a large nationwide outbreak of measles in 2000–2001.
Before 2000, when the Prevention of Contagious Diseases Act was implemented, the reported case of rubella in the Republic of Korea was rare, and only a minor outbreak in Seoul in 1963 was recorded.11 In the mid-1990s, a rubella outbreak among the adolescent population led to a change in policy from universal vaccination of infants to selective vaccination of all adolescent girls in tenth grade of high school.12 Before the institution of vaccination to adolescent girls, a cost-benefit analysis study has revealed that both rubella vaccination policies were found to be cost-effective, but vaccination to adolescent girls were more effective than vaccination to infants of both sexes.12 However, a large outbreak of measles in 2000 and 2001 prompted the government to implement a Five-Year Measles Elimination Program, which involved a nationwide measles-rubella catch-up vaccination program targeting the population aged from 8 to 16 years.10 This campaign eliminated the selective vaccination program that targeted adolescent females, and a universal vaccination of all infants from 12 to 15 months of age and children from 4 to 6 years of age was implemented.13
Meanwhile, a surveillance system for rubella and CRS in conjunction with nine other vaccine-preventable diseases (i.e. diphtheria, pertussis, tetanus, measles, mumps, polio, hepatitis B, Japanese encephalitis, and chickenpox) has been implemented since 2001, and all cases of suspected rubella are requested to be reported immediately to the Korea Centers for Disease Control and Prevention (KCDC).
The World Health Organization (WHO) has recommended that countries that implement the rubella vaccine should conduct surveillance for rubella and CRS as a part of the measles surveillance system.14 The minimum requirements for the surveillance system include monthly routine reporting of suspected CRS cases with zero reporting, monthly routine reporting of suspected rubella cases, investigation of all febrile rash illnesses in pregnant women, and testing for rubella-specific immunoglobulin M (IgM) antibodies in any suspected rubella outbreaks.15 Recently, the Republic of Korea has experienced a series of measles outbreaks, which prompted attention to improve the surveillance system for measles. In conjunction with measles, the need to re-evaluate the surveillance for monitoring rubella and CRS has been raised. The aim of this study was to review the reported cases of rubella and CRS supplied by the surveillance system from 2001 to 2009 and to propose measures to improve the quality of the surveillance system in the Republic of Korea.
2. Methods
The epidemiological data for rubella and CRS cases under the Prevention of Contagious Diseases Act16 were reported to the KCDC from 2001 to 2009. A suspected rubella case was defined as any patient presenting clinical symptoms of rubella; a confirmed rubella case was defined as any patient presenting clinical symptoms of rubella with laboratory confirmation [i.e. a positive blood test for rubella-specific IgM, 4-fold increase in immunoglobulin G (IgG) in paired serum samples, or virus isolation]. A suspected CRS case was defined as any infant with clinical symptoms of CRS; a confirmed CRS case was defined as any infant in whom clinical symptoms of CRS were presented with laboratory confirmation (i.e. the presence of positive rubella-specific IgM or isolation of virus).17 For each case, a thorough investigation by an epidemic intelligence service officer was provided, including recording the date of disease onset and patient sex, age, symptoms, vaccination status, and recent travel history.
The Korean Health Insurance Review Agency (HIRA) collects detailed data from Korean citizens regarding medical care and expenses as well as the amount to be paid as insurance. The agency consolidates available nationwide statistical and medical records. We obtained data regarding CRS cases in patients aged less that 1 year from 2005 to 2009 from the HIRA.
In the Republic of Korea, the 2001 Five-Year Measles Elimination Program established a laboratory surveillance that mandates all specimens submitted to the KCDC for measles testing to be routinely tested for rubella IgM and IgG.10 Any cases of suspected measles identified as rubella after laboratory testing were transferred to the rubella surveillance system.
3. Results
Before the implementation of the Prevention of Contagious Diseases Act in 2000,16 which mandated that all health care personnel report suspected cases of rubella and CRS to the government, reported cases of rubella and CRS were scarce. In 2001, after continued outbreaks of measles, the Five-Year Measles Elimination Program introduced a two-dose MMR vaccination for children aged 12–15 months and 4–6 years.10 As a result, the reported case of rubella was declined from 128 cases in 2001 down to a record low of only eight cases in 2003. For the years 2002, 2003, 2004, 2005, and 2006, the number of cases of rubella reported was 24, 24, 15, 12, and 18, respectively. The reported cases were slightly higher in 2007, 2008, and 2009, when 35, 30, and 36 cases were reported, respectively.
The highest reported cases were observed in the age groups of 0–9 and 10–19 years, which were 58 and 59 in 2001, respectively (Table 1). These reported cases were decreased to 10 and 9 in 2002 and to four and two in 2003, respectively, after the implementation of the two-dose MMR vaccination policy. In 2004, the highest reported cases were detected in the age group representing below 10 years (11/15, 73.3%), which decreased to 58.3% in 2005, 38.9% in 2006, 28.6% in 2007, 43.3% in 2008, and 36.1% in 2009 (Figure 1). Conversely, the reported cases between the ages 10 years and 19 years increased from 8.3% in 2005 to 27.8% in 2006, 22.9% in 2007, 33.3% in 2008, and 38.9% in 2009 (Figure 2). From 2001 to 2009, no documented outbreak of rubella was reported.
Table 1.
Annual reported cases of rubella, by age
| Years | 0–9 | 10–19 | 20–29 | 30–39 | 40–49 | ≥50 | Total cases |
|---|---|---|---|---|---|---|---|
| 2001 | 58 | 59 | 5 | 5 | 0 | 1 | 128 |
| 2002 | 10 | 9 | 3 | 1 | 0 | 1 | 24 |
| 2003 | 4 | 2 | 1 | 1 | 0 | 0 | 8 |
| 2004 | 11 | 2 | 1 | 1 | 0 | 0 | 15 |
| 2005 | 7 | 1 | 0 | 2 | 2 | 0 | 12 |
| 2006 | 7 | 5 | 5 | 1 | 0 | 0 | 18 |
| 2007 | 10 | 8 | 10 | 6 | 1 | 0 | 35 |
| 2008 | 13 | 10 | 4 | 3 | 0 | 0 | 30 |
| 2009 | 13 | 14 | 6 | 2 | 1 | 0 | 36 |
Figure 1.
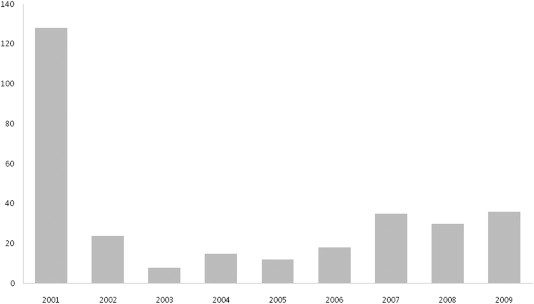
Annual reported cases of rubella reported in the Republic of Korea, 2001–2009.
Figure 2.
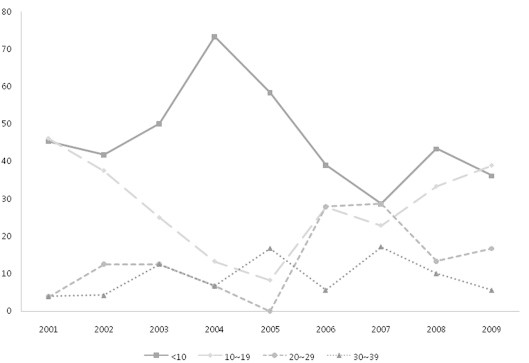
Percentages of age-specific reported cases of rubella.
The reported case of rubella among women aged 15–44 years was 6 in 2006, 16 in 2007, 3 in 2008, and 5 in 2009. The reported case of CRS was one in 2008 and two in 2009. Among the three confirmed CRS cases, the first case was of a male, who had cataract and a kidney anomaly in infancy and whose mother had gestational diabetes mellitus. The second case was of a prematurely born female with cataract and chorioretinitis. The third case was of a male, who was born prematurely at 29 weeks of gestational age with a birth weight of 1000 g, with ear anomalies and a ventricular septal defect (Table 2). The latter two cases were admitted to the neonatal intensive care unit, and outcomes were not described.
Table 2.
Reported cases of rubella among women aged 15–44 years, number of reported therapeutic abortions performed because of rubella infection in pregnant women, and the reported cases of congenital rubella syndrome
| Years | Reported rubella among women aged 15–44 yr | Number of therapeutic abortions | Reported CRS |
|---|---|---|---|
| 2006 | 6 | 1 | 0 |
| 2007 | 16 | 5 | 0 |
| 2008 | 3 | 0 | 1 |
| 2009 | 5 | 2 | 2 |
CRS = congenital rubella syndrome.
According to the data from HIRA, the number of CRS cases reported for reimbursement from 2005 to 2009 was 24, 19, 19, 9, and 5, respectively (Table 3).
Table 3.
Reported cases of congenital rubella syndrome from data retrieved from the Korean Health Insurance Review Agency, 2005–2009
| Years | 2005 | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|---|
| Male | 12 | 6 | 10 | 4 | 2 |
| Female | 12 | 13 | 9 | 5 | 3 |
| Total | 24 | 19 | 19 | 9 | 5 |
4. Discussion
The reported cases of rubella has declined from 128 cases in 2001 to 36 cases in 2009, probably because of the comprehensively increased vaccine coverage rate from 84% of first dose of MMR in 199918 to nearly 99% in 2009.19 However, the actual trend of rubella incidence remains unknown because of insufficient information reported before 2001. In addition, it is possible that the reported rubella cases in 2001 could be over-estimated because of large outbreak of measles, which led to actively capture under-diagnosed rubella cases and more reporting of suspected cases. Because of limited data before year 2000, the present study does not provide evidence that the Five-Year Measles Elimination Program, which resulted in mass vaccination of more than 5 million susceptible populations and a mandated second dose of MMR vaccination to children aged 4–6 years,10 has reduced the actual incidence of rubella in conjunction with measles in the Republic of Korea.
Before the present study, there were only few reported cases of CRS in the Republic of Korea.20 Despite a reduction of 71.9% of rubella cases between 2001 and 2009, three cases of confirmed CRS occurred in 2008 and 2009. The reported CRS cases were confirmed by clinical criteria as well as positive laboratory results. However, information regarding the case patients and their mothers, including birth weight, gestational age, and prenatal courses, was not complete. Follow-up outcome status was not recorded. The present study suggests a lack of validity of the rubella surveillance system currently implemented in the Republic of Korea.
Rubella elimination plans are established in most countries in the measles elimination phase. In 2000, the WHO recommended joint surveillance for suspected measles and rubella as febrile exanthematous illness surveillance.21 There is special emphasis regarding focused surveillance for infants less than 1 year of age with heart disease, cataracts, or deafness because such illness may provide an opportunity to accumulate information on the CRS disease burden.15 Currently, the precise incidence of congenital heart disease22,23 (0.89%–1.27%), infantile cataract,24 and congenital deafness25 has not yet been postulated at the nationwide level in the Republic of Korea. In addition to nationwide epidemiology studies of these three conditions, detailed communications between infection specialists, neonatologists, ophthalmologists, cardiologists, and hearing specialists will be required to conduct an active surveillance of CRS.
Currently, the RA 27/3 strain of rubella is the only vaccine strain available in the Republic of Korea.26 An immunogenicity analysis of the vaccine revealed the seroconversion rate of the antibody to be nearly 100%;27 thus the vaccine itself is not a mere problem in the control of rubella and CRS in the Republic of Korea. In 2007, it was reported that the estimated MMR vaccine coverage rate in the Republic of Korea was 93.2% for the first dose, but there was low second dose vaccine coverage: 24.2%, 42.3%, and 59.0% for children aged 4, 5, and 6 years, respectively.28 The considerably higher proportion of children who remain unvaccinated despite the mandatory two-dose MMR vaccine established since 2001 remains a concern. In addition, the level of susceptible childbearing age women should be vigilantly monitored and the surveillance system needs to account for such monitoring. According to a recent study conducted by the Korea Food and Drug Administration in 2009 (unpublished data), the seropositivity rate of rubella IgG was 100.0% among females aged 2–24 years, 90.0% in 25- to 26-year-old women, and 97.8% in 27- to 30-year-old women. Women with negative rubella IgG are at risk of rubella infection and at higher risk for CRS when exposed to the virus during pregnancy.
Recently, the increasing portion of immigration of women of childbearing age from developed countries may pose a higher risk of rubella virus transmission and CRS. Therefore, identifying all cases of rubella that occur in the Republic of Korea as well as monitoring women of childbearing age and foreign-born persons will be essential in improving surveillance for CRS.
As stated by the WHO, the primary purpose of a rubella vaccination is to prevent the occurrence of CRS.15 The surveillance system to detect and control rubella should reflect this objective. The discrepancy of reported cases of CRS among data from the KCDC and HIRA may suggest that the CRS surveillance system currently operating in the Republic of Korea is inadequate.
In conclusion, the present study questions the validity and ultimately the utility of the current rubella and CRS monitoring system in place in the Republic of Korea. A more detailed surveillance with greater emphasis on susceptible women of childbearing age may provide a more reliable system for monitoring and controlling both rubella and CRS in the Republic of Korea.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Freij B.J., South M.A., Sever J.L. Maternal rubella and the congenital rubella syndrome. Clin Perinatol. 1988;15:247–257. [PubMed] [Google Scholar]
- 2.Dayan G.H., Castillo-Solorzano C., Nava M. Efforts at rubella elimination in the United States: the impact of hemispheric rubella control. Clin Infect Dis. 2006;43(Suppl 3):S158–S163. doi: 10.1086/505949. [DOI] [PubMed] [Google Scholar]
- 3.Martin R., Deshevoi S., Buddha N., Jankovic D. Approaching measles and rubella elimination in the European region—need to sustain the gains. Euro Surveill. 2009;14:1–3. [PubMed] [Google Scholar]
- 4.Muscat M., Falkenhorst G., Bang H. Decline in measles in WHO European Region but rubella remains high. Euro Surveill. 2005;10:E050324.3. doi: 10.2807/esw.10.12.02669-en. [DOI] [PubMed] [Google Scholar]
- 5.Chandy S., Abraham A.M., Jana A.K. Congenital rubella syndrome and rubella in Vellore, South India. Epidemiol Infect. 2010:1–5. doi: 10.1017/S0950268810001755. [DOI] [PubMed] [Google Scholar]
- 6.Preblud S.R., Serdula M.K., Frank J.A., Jr. Rubella vaccination in the United States: a ten-year review. Epidemiol Rev. 1980;2:171–194. doi: 10.1093/oxfordjournals.epirev.a036221. [DOI] [PubMed] [Google Scholar]
- 7.Dudgeon J.A. Selective immunization: protection of the individual. Rev Infect Dis. 1985;7(Suppl 1):S185–S190. doi: 10.1093/clinids/7.supplement_1.s185. [DOI] [PubMed] [Google Scholar]
- 8.Watson J.C., Hadler S.C., Dykewicz C.A. Measles, mumps, and rubella-vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1998;47:1–57. [PubMed] [Google Scholar]
- 9.Peltola H., Heinonen O.P., Valle M. The elimination of indigenous measles, mumps, and rubella from Finland by a 12-year, two-dose vaccination program. N Engl J Med. 1994;331:1397–1402. doi: 10.1056/NEJM199411243312101. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Elimination of measles—South Korea, 2001–2006. MMWR Morb Mortal Wkly Rep. 2007;56:304–307. [PubMed] [Google Scholar]
- 11.Shin Y.K., Cheon H.W., Lee K.H. Mumps and rubella-specific IgG levels of term pregnant women and their neonates. J Korean Pediatr Soc. 1998;41:47–52. [Google Scholar]
- 12.Shin Y.J., Choi B.Y., Park H.B. Cost-benefit analysis on rubella vaccination policy. Korean J Prev Med. 1994;27:337–365. [Google Scholar]
- 13.The Korean Pediatric Society . General recommendation on immunization. In: Lee H.J., editor. Immunization guideline. 6th edn. The Korean Pediatric Society; Seoul: 2008. pp. 14–26. [Google Scholar]
- 14.Muller C.P., Kremer J.R., Best J.M. Reducing global disease burden of measles and rubella: report of the WHO Steering Committee on research related to measles and rubella vaccines and vaccination, 2005. Vaccine. 2007;25:1–9. doi: 10.1016/j.vaccine.2006.07.039. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organizations, Department of Vaccines and Biologicals; Geneva, Switzerland: 2003. WHO-Recommended Guideline for Surveillance of Vaccine-Preventable Diseases. [Google Scholar]
- 16.Ministry of Health . Korean Centers for Disease Control and Prevention; Seoul: 2009. Prevention of Contagious Disease Act. [Google Scholar]
- 17.Rubella prevention Recommendations of the Immunization Practices Advisory Committee (ACIP) MMWR Recomm Rep. 1990;39:1–18. [PubMed] [Google Scholar]
- 18.Jeong Y.W., Park B.H., Kim K.H. Timeliness of MMR vaccination and barriers to vaccination in preschool children. Epidemiol Infect. 2010:1–10. doi: 10.1017/S0950268810000889. [DOI] [PubMed] [Google Scholar]
- 19.Yoon K.C., Moon K.H., Joo C.U. A case of congenital rubella syndrome. J Korean Soc Neonatol. 1998;5:108–111. [Google Scholar]
- 20.World Health Organizations, Department of Vaccines and Biologicals; Geneva, Switzerland: 2000. Report of a Meeting on Preventing Congenital Rubella Syndrome: Immunization Strategies, Surveillance Needs. [Google Scholar]
- 21.Jang S.H., Kim J.H., Yeom J.S. Incidence of congenital heart disease in the western part of Gyeongnam Province in Korea. Korean J Pediatr. 2008;51:848–855. [Google Scholar]
- 22.Lee J.H., Shim G.H., Shin K.S. Congenital heart disease in Jeju: postnatal incidence and clinical features. Korean J Pediatr. 2004;47:294–303. [Google Scholar]
- 23.Kim D.H., Kim J.H., Kim S.J., Yu Y.S. Clinical results of secondary intraocular lens implantation in bilateral congenital cataract. J Korean Ophthalmol Soc. 2008;49:1752–1758. [Google Scholar]
- 24.Hn K. Audiologic survey of deaf school children. Korean J Otolaryngol. 1973;16:275–287. [Google Scholar]
- 25.Oh S.H. Active immunization. Hanyang Med Rev. 2008;28:4–15. [Google Scholar]
- 26.Ahn S.I., Chung M.K., Yoo J.S. The Safety and Immunogenicity of a Trivalent, Live, Attenuated MMR Vaccine, PriorixTM. Korean J Pediatr. 2005;48:960–968. [Google Scholar]
- 27.Lee HJ, Kim KH, Chun BC. Vaccine coverage rate in Korean children. In: Congress of Korean Society of Pediatrics, 2007.
- 28.Corcoran C., Hardie D.R. Seroprevalence of rubella antibodies among antenatal patients in the Western Cape. S Afr Med J. 2005;95:688–690. [PubMed] [Google Scholar]


