Abstract
Purpose
Epilepsy is a common childhood neurologic disorder, affecting 0.5 to1% of children. Increased mortality occurs due to progression of underlying disease, seizure-related accidents, suicide, status epilepticus, aspiration during seizures, and sudden unexplained death in epilepsy (SUDEP). Previous studies show mortality rates of 2.7 to 6.9 per 1000 person-years (Berg et al., 2004, Sillanpaa & Shinnar, 2010). Potential risk factors include poor seizure control, intractable epilepsy, status epilepticus, tonic-clonic seizures, mental retardation, and remote symptomatic cause of epilepsy (Berg et al., 2004, Sillanpaa & Shinnar, 2010, Walczak et al., 2001). Few population-based studies of mortality and SUDEP in childhood-onset epilepsy have been published. The purpose of this study is to report mortality and SUDEP from a 30 year population-based cohort of children with epilepsy.
Methods
The Medical Diagnostic Index of the Rochester Epidemiology Project was searched for all codes related to seizure and convulsion in children living in Olmsted County, Minnesota and of ages birth through 17 years from 1980 through 2009. The medical records of these children were reviewed to identify all those with new-onset epilepsy, and to abstract other baseline and follow-up information. Potential risk factors including seizure type, epilepsy syndrome, history of status epilepticus, the presence and severity of neurologic impairment, and epilepsy outcome was reviewed. Epilepsy outcome was characterized by seizure frequency, number of anti-seizure medications (AEDs) used, and number of AEDs failed due to lack of efficacy, and epilepsy intractability at 1, 2, 3, 5, 10, 15, and 20 years after epilepsy onset. We followed all children through their most recent visit to determine vital status, cause of death, and whether autopsy was performed.
Key Findings
From 1980 to 2009, there were 467 children age birth through 17 years diagnosed with epilepsy while residents of Olmsted County, MN and had follow-up beyond the time of epilepsy diagnosis. Children were followed for a median of 7.87 years after the time of diagnosis (range 0.04–29.49 years) for a total of 4558.5 person-years. Sixteen (3.4%) of the children died, or 3.51 deaths per 1000 person-years. Two deaths were epilepsy-related (12.5%) for a rate of 0.44 per 1000 person years. One of these children died of probable SUDEP and one died of aspiration during a seizure. The remaining 14 deaths (87.5%) were due to other complications of underlying disease. Several risk factors for mortality were found, including abnormal cognition, abnormal neurologic exam, structural/metabolic etiology for epilepsy, and poorly controlled epilepsy.
Background
Epilepsy is a common neurologic disorder in childhood, affecting 0.5 to 1% of children (Shinnar & Pellock, 2002). Increased mortality is seen in those with epilepsy due to progression of underlying disease, seizure-related accidents, suicide, status epilepticus, aspiration during seizures, and sudden unexplained death in epilepsy (SUDEP)(Ficker, 2000). The standardized mortality ratio (SMR) in adults with epilepsy has been reported to be 2.5 to 3.6 when compared to the general population, suggesting adults with epilepsy have significantly higher mortality rates (Cockerell et al., 1994, Nilsson et al., 1997).
SUDEP is a common cause of death in adults with epilepsy, accounting for 2% to 18% of deaths in patients with epilepsy, with an incidence of 0.35 to 1.5 deaths per 1000 person years (Annegers & Coan, 1999, Ficker et al., 1998, Vlooswijk et al., 2007, Walczak et al., 2001). A previous population-based study of SUDEP in all patients with epilepsy in Rochester, MN reported the incidence of SUDEP to be 0.35 deaths per 1000 person years with a standardized mortality ratio of 23.7 when compared to the general population. Although SUDEP was responsible for 1.7% of deaths in the cohort, 8.6% of deaths in the 15 to 44 year age group were due to SUDEP (Ficker et al., 1998). However, the incidence of seizure-related death and SUDEP in children has been reported to be much lower.
Previous population- and community-based studies of epilepsy in children have shown overall mortality rates of between 2.7 to 6.9 deaths per 1000 person-years (Berg et al., 2004, Callenbach et al., 2001, Camfield & Camfield, 2005, Sillanpaa et al., 1998). The incidence of death due to SUDEP in children has been reported to be 1.1 to 2 deaths per 10,000 person-years (Camfield & Camfield, 2005, Donner et al., 2001). A recently published cohort of children with epilepsy (including both prevalent and incident cases) reported an overall mortality rate of 6.9 deaths per 1000 person years (Sillanpaa & Shinnar, 2010). Epilepsy-related deaths accounted for 55% of all deaths and 30% of all deaths were due to SUDEP (Sillanpaa & Shinnar, 2010). This rate of SUDEP is much higher than previously reported. Risk factors in that study included remote symptomatic etiology of epilepsy, lack of 5 year terminal remission, and severe cognitive impairment (Sillanpaa & Shinnar, 2010). Other previously cited risk factors for increased mortality in epilepsy include poor seizure control, intractable epilepsy, status epilepticus at the time of initial diagnosis, history of tonic-clonic seizures, mental retardation/neurologic deficit, and remote symptomatic cause of epilepsy (Berg et al., 2004, Walczak et al., 2001, Camfield et al., 2002).
Few population-based studies of mortality and SUDEP in childhood-onset epilepsy have been published. Those studies that have been published have yielded variable results, with the most recent study demonstrating higher mortality rates than previously reported. Therefore, the aim of this study is to report mortality and SUDEP from a 30 year population-based incidence cohort of children with epilepsy.
Methods
Population demographics
Olmsted County, Minnesota is the home of Mayo Clinic and Olmsted Medical Center. It is geographically isolated from other providers of tertiary care. According to the 2000 US Decennial Census, the population of Olmsted County was 124,277 persons, with 90.3% Caucasian. The residents of Olmsted County are largely middle class and enjoy virtually universal access to high-quality health care. More than 95% of all medical care is provided by Mayo Clinic or Olmsted Medical Center. All inpatient and outpatient diagnoses from the medical records are indexed for computerized retrieval through the Rochester Epidemiology Project. Extensive indices are available for medical diagnoses, surgical procedures, and tissue diagnoses (Melton, 1996, Nickels et al., 2008).
Cohort identification and information retrieved
The Medical Diagnostic Index of the Rochester Epidemiology Project was searched for all codes related to seizure and convulsion in children between the ages birth through 17 years who were residents of Olmsted County from 1980 to 2009. All identified charts were reviewed by a pediatric epileptologist. All children ages 1 month through 17 years diagnosed with new-onset epilepsy while resident in Olmsted County from 1980 to 2009 and had follow-up beyond the initial epilepsy diagnosis were included. Children with neonatal seizures that resolved during the neonatal period were included only if there was seizure recurrence after age one month.
The date of epilepsy diagnosis was defined as the date the patient was first given the diagnosis of epilepsy by a physician, and is used as the baseline visit for analyses in this report.
The historical records of all patients were reviewed to abstract potential risk factors including seizure mode of onset, epilepsy etiology, history of status epilepticus, the presence and severity of neurologic impairment, and epilepsy outcome. Epilepsy outcome was characterized by seizure frequency, number of anti-seizure medications (AEDs) used, number of AEDs failed due to lack of efficacy, and epilepsy intractability at 1, 2, 3, 5, 10, 15, and 20 years after epilepsy onset. In addition, we followed all children through their most recent visit to determine vital status, cause of death, and whether autopsy was performed.
Cognitive function was assessed through either formal neuropsychometric testing (if available) or best clinical judgment by the reviewer (KN or EW), using developmental milestones and academic achievement to classify developmental quotient (defined as the child’s functional/developmental age divided by the chronological age and then multiplied by 100). Children were then classified as normal (estimated or measured developmental quotient of 80 or higher), mildly to moderate intellectual disability (estimated or measured developmental quotient of 50–79), or severe intellectual disability (estimated or measured developmental quotient of <50). (Table 1)
Table 1.
Data abstracted from medical records
| Category | Information |
|---|---|
| Demographics | Sex |
| Duration of follow-up | |
| Neurologic examination | Motor/sensory exam |
| Cognition | |
| History of status epilepticus | |
| Epilepsy classification | Seizure mode of onset |
| Epilepsy etiology | |
| Epilepsy outcome | Number of AEDs used |
| Number of AEDs failed due to lack of efficacy | |
| Seizure control | |
| Intractable epilepsy | |
| Mortality | Death status |
| Cause of death | |
| Autopsy performed | |
Epilepsy was defined as being predisposed to unprovoked seizures. While the majority of children had two or more unprovoked seizures, those who had a single unprovoked seizure and evidence of a chronic abnormality of the brain that increased the likelihood of further seizures and were treated with anti-seizure medications were also included (Fisher et al., 2005). Such abnormalities included EEG findings of epileptiform discharges and intermittent rhythmic focal delta activity, focal abnormality on neuroimaging, initial presentation in status epilepticus, and abnormal neurodevelopmental examination. Children with two unprovoked seizures occurring within a single day were also likely to have epilepsy and were included (Camfield & Camfield, 2000). Children with neonatal seizures were included if there was seizure recurrence after one month of age. Those children treated after a single unprovoked seizure, but without any of the preceding abnormalities, and those with only febrile convulsions were excluded. In addition, those with only acute symptomatic seizures, defined as “seizure at the time of a systemic insult or in close association with an acute neurologic insult” were excluded (Beghi et al., 2010, Wirrell et al., 2011).
Epilepsy was classified according to the new ILAE Commission on Classification and Terminology 2005–2009 Report. According to the new classification scheme, epilepsy was classified based on mode of onset (generalized/bilateral cortical or subcortical, focal/networks limited to one hemisphere, unknown, or spasms) and underlying etiology (due to known or presumed genetic defect, due to structural or metabolic abnormalities, or due to unknown causes). Epilepsy was further classified into individual specific electroclinical syndromes and constellations, if applicable (Berg et al., 2010, Wirrell et al., 2011). Medically intractable epilepsy was defined as one or more seizures every six months over the year previous to follow-up and failure of two or more anti-epileptic medications for lack of efficacy.
Definite SUDEP was defined as meeting all of the following criteria: 1) history of epilepsy; 2) death or cardiorespiratory compromise was sudden, and not the direct result of seizure or status epilepticus; 3) death was unexpected (otherwise healthy); 4) death occurred during normal activities; 5) no other cause of death was found, including after autopsy. Probable SUDEP fulfilled the previous criteria, except autopsy was not performed (Donner et al., 2001).
Statistical analysis
All statistical analyses were performed using PASW Statistics 18.0 (SPSS Inc., Chicago, IL, U.S.A.) and SAS version 9.2 (SAS Institute, Cary, NC, U.S.A.). Cox regression models were fit to estimate Hazards Ratios (HR) and 95% confidence intervals and p-values were calculated. Kaplan-Meier curves were drawn for visual display of those findings of most clinical interest. All statistical tests were performed at the conventional two-sided alpha level of 0.05. Standardized Mortality Ratios (SMR) were calculated by using person-years methodology and age-, sex-, and calendar-year specific mortality rates observed in the Olmsted County population from 1980 to 2009. These rates were available as part of the Rochester Epidemiology Project infrastructure (St. Sauver et al., 2011).
This study was approved by the Institutional Review Boards of the Mayo Clinic and Olmsted Medical Center.
Results
Demographics
From 1980 to 2009, there were 467 children, 53% male, age one month through 17 years diagnosed with epilepsy while residents of Olmsted County, MN with follow-up beyond the diagnosis of epilepsy; 107 were diagnosed from 1980–1989, 160 from 1990–1999, and 200 from 2000–2009. These patients were followed for a median of 7.87 years after the time of diagnosis (25th percentile 3.63 years, 75th percentile 14.08 years, range 0.04–29.49 years). At last follow-up, 131 children were age 1 month to 10 years, 171 were age 10–19 years, 128 were age 20–29 years, and 37 were older than age 30 years. The neurologic exam was abnormal (motor or sensory findings) in 119 children (25.5%) and cognitive development was severely delayed in 83 children (17.8%) and moderately delayed in 109 children (23.3%).
Seizures were focal onset in 317 children (67.8%), generalized in 113 (24.2%), spasms occurred in 14 (3.0%), with the remainder of seizures being of unknown onset (19 children; 4.1%) or both generalized and focal (4 children; 0.9%). In 232 of the subjects (49.7%) the etiology of epilepsy was unknown; 109 were genetic (23.3%), 124 were due to structural or metabolic etiology (26.6%), and the remaining 2 children exhibited both genetic and structural etiology. At last follow-up, the majority of subjects (389 children; 83.3%) were treated with 0 or 1 AEDs, with the remainder of children being treated with with 2 to 5 AEDs. A total of 145 subjects (31.0%) had failed one or more AEDs due to lack of efficacy at the time of last follow-up.
Seizure control was excellent in the majority of patients, with 66.8% seizure-free for more than one year at last follow-up, and an additional 10.3% were experiencing seizures only once every 6–12 months. Frequent seizures, defined as more than one seizure every three months, occurred in 16.9% of children. Medically refractory epilepsy was present at some time during follow-up in 28.5% of children, but only 16.5% were intractable at last follow-up. In addition, 20.1% of children had ever experienced status epilepticus. (Table 2)
Table 2.
Descriptive information of the 467 included children with epilepsy
| N(%) or | ||
|---|---|---|
| Characteristic | Group | Median (min, max) |
| Number of children | --- | 467 |
| Male sex | --- | 246 (52.7%) |
| Follow-up, years | --- | 7.87 (0.04, 29.5) |
| Neurological examination | Normal | 348 (74.5%) |
| Abnormal | 119 (25.5%) | |
| Cognitive development | Normal | 275 (58.9%) |
| Mild/moderate delay | 109 (23.3%) | |
| Severe delay | 83 (17.8%) | |
| Status epilepticus ever | No | 373 (79.9%) |
| Yes | 94 (20.1%) | |
| Mode of onset | Generalized/ bihemispheric | 113 (24.2%) |
| Focal/unihemispheric | 317 (67.9%) | |
| Unknown | 19 (4.1%) | |
| Spasms | 14 (3.0%) | |
| Generalized and focal | 4 (0.9%) | |
| Etiology | Genetic | 109 (23.3%) |
| Metabolic/structural | 125 (26.6%) | |
| Unknown | 233 (49.7%) | |
| Genetic and metabolic/ structural | 2 (0.4%) | |
| AEDs used at last visit | No AED | 190 (40.7%) |
| 1 | 199 (42.6%) | |
| 2 | 58 (12.4%) | |
| 3 | 15 (3.2%) | |
| ≥4 | 5 (1.1%) | |
| AEDs discontinued | No failed AED | 322 (69.0%) |
| due to lack of efficacy | 1 | 71 (15.2%) |
| 2 | 31 (6.6%) | |
| ≥3 | 43 (9.2%) | |
| Seizure control at last follow-up | Seizure free >12 months | 312 (66.8%) |
| Seizure 6–12 months | 48 (10.3%) | |
| Seizure 3–6 months | 28 (6.0%) | |
| Seizure >3 every months | 79 (16.9%) | |
| Epilepsy intractable | Intractable ever | 134 (28.7%) |
| Intractable/surgery at last visit | 94 (20.1%) | |
| Children died | --- | 16 (3.4%) |
| Autopsy performed | --- | 2 (12.5%) |
| Cause of death | Respiratory complications | 9 (56.3%) |
| Progressive neurometabolic/neurodegenerative disease | 4 (25.0%) | |
| Seizure | 1 (6.3%) | |
| SUDEP | 1 (6.3%) | |
| Unrelated non-neurologic cause | 1 (6.3%) |
Mortality
Sixteen (3.4%) of the children died, or 3.51 deaths per 1000 person-years. This rate was significantly higher than the expected mortality as calculated from age-, sex-, and calendar-year specific death rates in Olmsted County (expected deaths was 1.77, SMR = 9.04; 95% CI 5.35–14.37; p < 0.0001). Two of the deaths were epilepsy-related (12.5%) for a rate of 0.44 per 1000 person years. One of these children died of definite SUDEP (0.22 deaths per 1000 person years) and one died of aspiration during a seizure (0.22 deaths per 1000 person years). The remaining 14 deaths (87.5%) were due to other complications of underlying disease, including respiratory failure related to progressive metabolic disease (4), respiratory complications related to profound neurologic impairment (9), and complications of non-neurologic disease (graft vs host disease) (1).
Respiratory complications of metabolic disease or profound neurologic impairment were the cause of death in the majority of children in all attained age groups, although more deaths occurred in the younger age group. Eleven of the children who died were in the one month to ten year attained age group (11/131 children, 8% died); nine of these deaths (82%) were due to respiratory complications. The other two deaths were due to SUDEP and aspiration during a seizure. Four deaths were in the 10–19 year attained age group (4/171 children, 2% died); three were due to respiratory complications (75%) and one was due to graft vs host disease. One death was in the 20 years and older attained age group (1/165, 0.6% died) and was due to respiratory complications
Risk factors for mortality
Multiple significant risk factors were identified, including abnormal neurologic exam, intellectual disability, structural/metabolic etiology for epilepsy, history of status epilepticus, and poorly controlled epilepsy (the use of more than one AED at last follow-up, continued frequent seizures, and diagnosis of intractable epilepsy). Table 3 summarizes the risk factors separately by baseline characteristics, and outcome categories. Of particular note is that only one child without intellectual disability died, and the cause of death was non-neurologic disease (HR for intellectual disability = 20.86, p = 0.003). Similarly, only one child with a normal neurologic exam died (HR for abnormal neurologic exam = 41.69; p = 0.0003). Mode of onset was not predictive of mortality, whereas a structural or metabolic etiology of epilepsy was associated with a marked increased risk of mortality (HR=11.29, p = 0.0002). Interestingly, an unknown etiology was associated with a significantly decreased risk of mortality, suggesting that epilepsy of unknown etiology is more benign, at least with regards to mortality.
Table 3.
Risk factors for death in children with epilepsy.
| Deaths | Person- | Hazard | ||||||
|---|---|---|---|---|---|---|---|---|
| Strata | N | N (%) | years | Ratio | 95% CI | P-value | ||
| Baseline characteristics | ||||||||
| Neurologic exam | ||||||||
| Normal | 348 | 1 (0.3) | 3,334 | 1.0 | (reference) | --- | ||
| Abnormal | 119 | 15 (12.6) | 1,224 | 41.69 | (5.51 – 315.62) | 0.0003 | ||
| Cognitive function | ||||||||
| Normal | 275 | 1 (0.4) | 2,617 | 1.0 | (reference) | --- | ||
| Abnormal | 192 | 15 (7.8) | 1,942 | 20.86 | (2.76 – 157.97) | 0.003 | ||
| Status epilepticus | ||||||||
| No, never | 373 | 7 (1.9) | 3,448 | 1.0 | (reference) | --- | ||
| Yes, ever | 94 | 9 (9.6) | 1,110 | 4.42 | (1.64 – 11.90) | 0.003 | ||
| Mode of onset * | ||||||||
| Generalized | 117 | 3 (2.6) | 1,129 | 0.71 | (0.20 – 2.49) | 0.59 | ||
| Focal | 321 | 12 (3.7) | 3,135 | 1.37 | (0.44 – 4.24) | 0.59 | ||
| Other † | 33 | 1 (3.0) | 340 | 0.80 | (0.11 – 6.08) | 0.83 | ||
| Etiology * | ||||||||
| Genetic | 111 | 2 (1.8) | 1,054 | 0.47 | (0.11 – 2.06) | 0.31 | ||
| Structural / Metabolic | 126 | 13 (10.3) | 1,283 | 11.29 | (3.22 – 39.63) | 0.0002 | ||
| Unknown | 231 | 1 (0.4) | 2,230 | 0.07 | (0.01 – 0.52) | 0.01 | ||
| Outcome categories | ||||||||
| Currently using ≥ 2 AEDs | ||||||||
| No | 389 | 5 (1.3) | 3,858 | 1.0 | (reference) | --- | ||
| Yes | 78 | 11 (14.1) | 700 | 11.89 | (4.13 – 34.25) | < 0.0001 | ||
| Seizure frequency | ||||||||
| Less often than 6 mo. | 360 | 2 (0.6) | 3,742 | 1.0 | (reference) | --- | ||
| More often than 6 mo. | 107 | 14 (13.1) | 817 | 30.45 | (6.91 – 134.14) | < 0.0001 | ||
| Intractable at last follow-up ‡ | ||||||||
| No | 373 | 2 (0.5) | 3,652 | 1.0 | (reference) | --- | ||
| Yes | 94 | 14 (14.9) | 907 | 28.09 | (6.38 – 123.65) | < 0.0001 | ||
Because no category was clearly the "referent" group, analyses were performed for each stratum compared to the other two strata pooled.
Mode of onset category "other" includes both spasms and unknown onset mode.
Children who had undergone surgery during follow-up are included in the intractable “yes” group.
Poorly controlled epilepsy was also a significant risk factor. Analyses separate within strata of outcomes categories are presented in the bottom of Table 3. We note that the expectation was that these analyses would show statistical significance. In particular, these analyses are stratified on information not available at baseline, but rather information which became clear over several years of disease progression. These analyses support that mortality in children may be reduced or monitoring of children may be improved if we were better able to predict certain characteristics of epilepsy early in the disease course. Namely, such clinical tools as genetic testing, or improved diagnostics may allow children to be classified as intractable earlier in the disease course, and subsequently may be monitored more closely to decrease mortality.
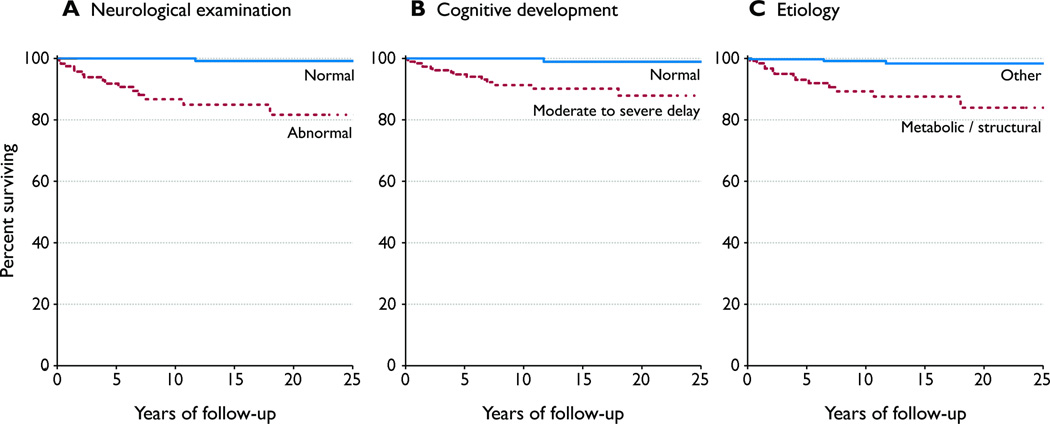
We also performed a Cox regression model including abnormal neurologic exam, abnormal cognitive function, status epilepticus, and structural or metabolic etiology. On multivariable Cox regression model of these baseline characteristics, only abnormal neurologic exam remained statistically significant (Table 4; Figure 1).
Table 4.
Multivariable Cox regression model.
| Risk factor | HR | 95% CI | P-value |
|---|---|---|---|
| Abnormal neurologic exam | 12.80 | (1.40 – 116.96) | 0.02 |
| Abnormal cognitive function | 3.78 | (0.42 – 33.80) | 0.23 |
| Status epilepticus, ever | 1.34 | (0.48 – 3.77) | 0.58 |
| Metabolic/structural etiology | 2.62 | (0.69 – 9.90) | 0.16 |
Figure 1.
The Kaplan-Meier curves for mortality separate by baseline characteristics: A) neurological examination, normal vs. abnormal; B) cognitive development, moderate to severe delay vs. normal; C) etiology, metabolic/structural vs. other.
Discussion
This was a large population-based study of 467 children over a 30 year period, with more than 4,500 person-years of follow-up. We found an increased mortality rate in children with epilepsy, 3.5 per 1000 person years, which is higher than expected in the Olmsted County population (SMR = 9.04) and ten times the national mortality rate for children in 2005 of 0.32 per 1000 person years (Martin et al., 2008). The results of this study are within the wide range of previously reported population- and community-based studies of childhood-onset epilepsy that demonstrated mortality rates of 2.7 to 6.9 per 1000 person years (Berg et al., 2004 , Sillanpaa & Shinnar, 2010). However, this is much lower than the 21.5 deaths per 1000 person years reported in a prospective population based study of mortality in children and adults with epilepsy (Cockerell et al, 1994). This is also lower than the 6.90 per 1000 person years in a recently reported population-based study of children with epilepsy (Sillanpaa & Shinnar, 2010).
The higher mortality rate seen in the recent population-based study by Shinnar and Sillanpaa is likely related to the increased severity of disease in this cohort, as well as the longer duration of follow-up (40 years) in that study. Remote symptomatic epilepsy and poorly controlled epilepsy have previously been shown to be associated with increased risk for death in children with epilepsy. This is supported by the higher mortality in children with symptomatic epilepsy, compared to those with cryptogenic or idiopathic epilepsy, 11.1 vs 3.23 per 1000 person years, seen in the recent population-based study (Sillanpaa & Shinnar, 2010). This was also seen in our study, with mortality in those with structural/metabolic cause being 10.1 per 1000 person years, compared to 0.9 per 1000 person years in children with epilepsy due to genetic or unknown cause.
Furthermore, 50% of the subjects in the previous study had remote symptomatic epilepsy, defined as “epilepsy associated with a major neurologic abnormality or insult” (Sillanpaa & Shinnar, 2010). By contrast, 27% of the children in our study had epilepsy due to structural or metabolic abnormalities and 29% were diagnosed with intractable epilepsy at some time during follow-up, which is similar to the other population- and community-based studies (Berg et al., 2004, Camfield & Camfield, 2005). Previous population-based studies of mortality in children with developmental disabilities have also demonstrated increased mortality, with increasing mortality reflecting increased disability (Decoufle & Autry, 2002, Strauss et al., 1998).
Finally, although the length of follow-up in our study was shorter, a previous population-based study of SUDEP in adults demonstrated that SUDEP was responsible for 8.6% of deaths and another population based study in children demonstrated SUDEP was the cause of death in 3.8% (Camfield et al., 2002, Ficker et al., 1998). Therefore, the lower mortality rate, and especially SUDEP, in our study is not explained by the shorter follow-up. Thus, the lower mortality rate in this population-based study, like that seen in previous population-based studies, most likely reflects the expected mortality rate in children with epilepsy.
This study identified multiple significant risk factors for mortality in children with epilepsy, including abnormal cognition, abnormal neurologic exam, structural/metabolic etiology for epilepsy, history of status epilepticus, and poorly controlled epilepsy (the use of more than one AED at last follow-up, continued frequent seizures at follow-up, and diagnosis of intractable epilepsy). These findings are similar to previous studies, which demonstrated developmental delay, refractory epilepsy, and AED polypharmacy to be risk factors for increased mortality (Berg et al., 2004, Brorson & Wranne, 1987, Callenbach et al., 2001, Cockerell et al., 1994, Decoufle & Autry, 2002, Weber et al., 2005). However, the majority of deaths (87.5%) were not directly related to the underlying epilepsy, but rather due to complications, primarily respiratory, of the underlying neurologic disease. Therefore, there were multiple epilepsy-related risk factors for mortality present in these children, and this is likely due to poor seizure control being more common in children with neurologic impairment.
Epilepsy-related death in our study occurred in only two of the children (12.5%), or 0.44 per 1000 person years. SUDEP occurred in only one of these children, or 0.22 per 1000 person years. This is significantly lower than the recent study of mortality in children with epilepsy, in which 55% of deaths were due to epilepsy and 30% of deaths were related to SUDEP (Sillanpaa & Shinnar, 2010). However, our findings are consistent with previous studies of SUDEP in children reported as 0 to 4% (Camfield & Camfield, 2005, Cockerell et al., 1994, Weber et al., 2005). Therefore, the higher prevalence of SUDEP in the recent study is likely due to the high proportion of patients with profound neurologic impairment in that cohort.
There may be several potential limitations of this study. First, this study was historical and it is possible that we failed to find all children with epilepsy or that treatment and epilepsy outcome was incompletely documented in the medical records. However, our incidence rates were similar to previously published population-based studies of childhood onset epilepsy, suggesting a complete cohort was obtained. Furthermore, we did not directly examine or interview all children to verify syndrome classification. However, we screened the complete Medical Diagnostic Index of the Rochester Epidemiology Project for children diagnosed at any time with seizure or convulsion. All identified charts were then reviewed by a pediatric epileptologist. Furthermore, complete medical records, including neuroimaging, laboratory results, electroencephalograms, and all documentation from both the inpatient and outpatient settings was available for each child, minimizing the possibility that information was missed.
Mortality in children with epilepsy was higher than would be expected in the general pediatric population. However, death occurred significantly more in children with neurologic impairment and poorly controlled epilepsy. Furthermore, death related to epilepsy, including SUDEP, occurred in only two patients. The remaining deaths were due to complications of the underlying neurologic disease or unrelated disease. Mortality due to epilepsy alone was similar to the expected mortality in children.
Although the findings of this study demonstrated significantly lower rates of mortality and SUDEP when compared to the most recent population-based study of mortality in children with epilepsy, this is likely due to different population demographics. In addition, we feel our study is more consistent with other population-based studies. Therefore, although mortality in children with epilepsy is significantly higher than the expected, a large proportion of this excess is likely related to the underlying neurologic disease, rather than the epilepsy. Furthermore, children with epilepsy who are not medically intractable and are otherwise neurologically normal have an exceedingly low risk of seizure-related death. Therefore, while it is important to counsel patients and families about the risk of seizure-related death and SUDEP, we can be reassured that this risk is low. However, it is also important to understand that seizure-related death and SUDEP do occur in children and the risk factors for this, primarily the underlying neurologic disease, are not preventable.
Significance.
Although mortality in children with epilepsy was higher than what would be expected in the general pediatric population, death occurred significantly more in children with neurologic impairment and poorly controlled epilepsy. Epilepsy-related death, including SUDEP, was rare and mortality due to epilepsy alone was similar to the expected mortality in the general population (Observed deaths = 2, expected deaths = 1.77; standardized mortality ratio (SMR) = 1.13, 95% confidence interval 0.19 – 3.73, p = 0.86). By contrast, most children died due to complications of the underlying neurologic disease or unrelated disease rather than the epilepsy.
Acknowledgements
This study was supported by a CR20 Research award from the Mayo Foundation, and made possible by the Rochester Epidemiology Project (R01 Grant # R01-AG034676;Dr. W.A. Rocca PI).
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Footnotes
Conflict of interest
None of the authors has any conflict of interest to disclose.
References
- Annegers J, Coan S. SUDEP: overview of definitions and review of incidence data. Seizure. 1999;8:347–352. doi: 10.1053/seiz.1999.0306. [DOI] [PubMed] [Google Scholar]
- Beghi E, Carpio A, Forsgren L, Hesdorffer D, Malmgren K, Sander J, Tomson T, Hauser W. Recommendation for a definition of acute symptomatic seizure. Epilepsia. 2010;51:671–675. doi: 10.1111/j.1528-1167.2009.02285.x. [DOI] [PubMed] [Google Scholar]
- Berg A, Berkovic S, Brodie M, Buchhalter J, Cross J, van Emde Boas W, Engel J, French J, Glauser T, Mathern G, Moshe S, Nordli D, Plouin P, Scheffer I. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia. 2010;51:676–685. doi: 10.1111/j.1528-1167.2010.02522.x. [DOI] [PubMed] [Google Scholar]
- Berg A, Shinnar S, Testa F, Levy S, Smith S, Beckerman B. Mortality in childhood-onset epilepsy. Arch Pediatr Adolesc Med. 2004;158:1147–1152. doi: 10.1001/archpedi.158.12.1147. [DOI] [PubMed] [Google Scholar]
- Brorson L, Wranne L. Long-term prognosis in childhood epilepsy: survival and seizure prognosis. Epilepsia. 1987;28:324–330. doi: 10.1111/j.1528-1157.1987.tb03651.x. [DOI] [PubMed] [Google Scholar]
- Callenbach P, Westendorp R, Geerts A, Arts W, Peeters E, van Donselaar C, Peters A, Stroink H, Brouwer O. Mortality risk in children with epilepsy: the Dutch study of epilepsy in childhood. Pediatrics. 2001;107:1259–1263. doi: 10.1542/peds.107.6.1259. [DOI] [PubMed] [Google Scholar]
- Camfield C, Camfield P, Veugelers P. Death in children with epilepsy: a population-based study. Lancet. 2002;359:1891–1895. doi: 10.1016/S0140-6736(02)08779-2. [DOI] [PubMed] [Google Scholar]
- Camfield P, Camfield C. Epilepsy can be diagnosed when the first two seizures occur on the same day. Epilepsia. 2000;41:1230–1233. doi: 10.1111/j.1528-1157.2000.tb00331.x. [DOI] [PubMed] [Google Scholar]
- Camfield P, Camfield C. Sudden unexpected death in people with epilepsy: a pediatric perspective. Semin Pediatr Neurol. 2005;12:10–14. doi: 10.1016/j.spen.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Cockerell O, Johnson A, Sander J, Hart Y, Goodridge D, Shorvon S. Mortality from epilepsy: results from a prospective population-based study. Lancet. 1994;344:918–921. doi: 10.1016/s0140-6736(94)92270-5. [DOI] [PubMed] [Google Scholar]
- Decoufle P, Autry A. Increased mortality in children and adolescents with developmental disabilities. Paediatr Perinat Epidemiol. 2002;16:375–382. doi: 10.1046/j.1365-3016.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- Donner E, Smith C, Snead O. Sudden unexplained death in children with epilepsy. Neurology. 2001;57:430–434. doi: 10.1212/wnl.57.3.430. [DOI] [PubMed] [Google Scholar]
- Ficker D. Sudden unexplained death and injury in epilepsy. Epilepsia. 2000;41:S7–S12. doi: 10.1111/j.1528-1157.2000.tb01519.x. [DOI] [PubMed] [Google Scholar]
- Ficker D, So E, Shen W, Annegers J, O'Brien P, Cascino G, Belau P. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology. 1998;51:1270–1274. doi: 10.1212/wnl.51.5.1270. [DOI] [PubMed] [Google Scholar]
- Fisher R, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, Engel JJ. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE) Epilepsia. 2005;46:470–472. doi: 10.1111/j.0013-9580.2005.66104.x. [DOI] [PubMed] [Google Scholar]
- Martin J, Kung H, Mathews T, Hoyert D, Strobino D, Guyer B, Sutton S. Annual summary of vital statistics: 2006. Pediatrics. 2008;121:788–801. doi: 10.1542/peds.2007-3753. [DOI] [PubMed] [Google Scholar]
- Melton LR. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- Nickels K, Katusic S, Colligan R, Weaver A, Voigt R, Barbaresi W. Stimulant medication treatment of target behaviors in children with autism: a population-based study. J Dev Behav Pediatr. 2008;29:75–81. doi: 10.1097/dbp.0b013e31815f24f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson L, Tomson T, Farahmand B, Diwan V, Persson P. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia. 1997;38:1062–1068. doi: 10.1111/j.1528-1157.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- Shinnar S, Pellock J. Update on the epidemiology and prognosis of pediatric epilepsy. J Child Neurol. 2002;17:S4–S17. doi: 10.1177/08830738020170010201. [DOI] [PubMed] [Google Scholar]
- Sillanpaa M, Jalava M, Kaleva O, Shinnar S. Long-term prognosis of seizures with onset in childhood. N Engl J Med. 1998;338P:1715–1722. doi: 10.1056/NEJM199806113382402. [DOI] [PubMed] [Google Scholar]
- Sillanpaa M, Shinnar S. Long-term mortality in childhood-onset epilepsy. N Engl J Med. 2010;363:2522–2529. doi: 10.1056/NEJMoa0911610. [DOI] [PubMed] [Google Scholar]
- St. Sauver J, Grossardt B, Yawn B, Melton L, Rocca W. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss D, Shavelle R, Anderson T. Life expectancy of children with cerebral palsy. Pediatr Neurol. 1998;18:143–149. doi: 10.1016/s0887-8994(97)00172-0. [DOI] [PubMed] [Google Scholar]
- Vlooswijk M, Majoie H, De Krom M, Tan I, Aldenkamp A. SUDEP in the Netherlands: a retrospective study in a tertiary referral center. Seizure. 2007;16:153–159. doi: 10.1016/j.seizure.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Walczak T, Leppik I, D'Amelio M, Rarick J, So E, Ahman P, Ruggles K, Cascino G, Annegers J, Hauser W. Incidence and risk factors in sudden unexpected death in epilepsy: a prospective cohort study. Neurology. 2001;56:519–525. doi: 10.1212/wnl.56.4.519. [DOI] [PubMed] [Google Scholar]
- Weber P, Bubl R, Blauenstein U, Tillmann B, Lutschg J. Sudden unexplained death in children with epilepsy: a cohort study with an eighteen-year follow-up. Acta Paediatr. 2005;94:564–567. doi: 10.1111/j.1651-2227.2005.tb01940.x. [DOI] [PubMed] [Google Scholar]
- Wirrell E, Grossardt B, Wong-Kisiel L, Nickels K. Incidence and classification of new-onset epilepsy and epilepsy syndromes in children in Olmsted County, Minnesota from 1980 to 2004: A population-based study. Epilepsy Res. 2011;95:110–118. doi: 10.1016/j.eplepsyres.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]