Abstract
Background
Patients with co-occurrence of hypertension, hyperlipidemia, and diabetes have an increased risk of cardiovascular disease (CVD) events. Comprehensive programs addressing both tailored patient self-management and pharmacotherapy are needed to address barriers to optimal cardiovascular risk reduction. We are examining a Clinical Pharmacy Specialist (CPS), telephone administered intervention, relying on home monitoring, with a goal of providing tailored medication and behavioral intervention to Veterans with CVD risk.
Methods
Randomized controlled trial including patients with hypertension (blood pressure (BP) > 150/100 mmHg) or elevated low density liporotein (LDL) (> 130 mg/dl). Longitudinal changes in CVD risk profile and improvement in health behaviors over time will be examined.
Conclusion
Given the national prevalence of CVD and the dismal rates of risk factor control; intensive, but easily disseminated interventions are required to treat this epidemic. This study will be an important step in testing the effectiveness of a behavioral and medication intervention to improve CVD control among Veterans.
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in the U.S.; more than 80% of veterans have at least 2 CVD risk factors.1 Patients can decrease CVD risk through lifestyle changes, but changes may be difficult to maintain. Medication use is another risk reduction strategy, but 20-50% of patients are non-adherent. 2 Despite the availability of effective therapy for diabetes, hypertension, and hypercholesterolemia, only 13% of Veterans with CVD achieve target control. 3, 4
Comprehensive CVD programs that employ tailored patient self-management, pharmacotherapy and behavioral interventions are needed for cardiovascular risk reduction. The VA has increasingly emphasized a patient aligned care teams, or PACT. The PACT is an application of the patient-centered medical home5 that emphasizes team delivery of patient-centered care, coordination across specialties, open access, and value-driven care.5 PACTs stress the utility of non-face-to-face interventions. These encounters may reduce patients’ travel cost, reduce clinic no-show appointments, and may supplant some clinic visits. Telephone-based care may be critical in supporting the PACT vision of coordination across different settings of care while improving access to care.
The professional role of the person making the telephone calls is equally important. Clinical pharmacist specialists (CPS) have training to provide behavioral interventions and intensive medication management needed in this high-risk CVD population.6 A CPS is a pharmacist who has completed post-graduate residency training, is credentialed to prescribe, adjust, and monitor pharmacotherapy. CPS-directed care with clinical collaboration has demonstrated improvement in the management of the individual major CVD risk factors in outpatients.6, 7 We are conducting a randomized trial to evaluate the Cardiovascular Intervention Improvement Telemedicine Study (CITIES), a CPS-delivered intervention administered by telephone to Veterans with poorly controlled hypertension and/or hypercholesterolemia. We describe the trial and the intervention utilizing a clinical pharmacist specialist.
METHODS
Design, Setting and Recruitment
We are conducting a 12-month intervention comparing patients receiving the intervention to an educational control group among Veterans affiliated with primary care. The Durham VAMC Institutional Review Board approved the study.
Inclusion Criteria
Patients are eligible if they: 1) live in North Carolina or Virginia, 2) are ≥ 40 years of age, 3) are enrolled in one of three primary care clinics affiliated with the Durham VAMC (at least 1 visit with assigned primary care provider (PCP) in the past year), 4) have a diagnosis of hypertension or hypercholesterolemia, and 5) have poorly controlled hypertension mean clinic BP of > 150/100 mmHg and/or hypercholesterolemia LDL value > 130 mg/dl in the last year.
Exclusion Criteria
Patients are excluded if they: 1) have a diagnosis of metastatic cancer, dementia, active psychosis or serum creatinine > 2.5 mg/dl or no lab value on file and/or on dialysis; 2) reside in a nursing home; 3) are unable to see/read type printing on magazines/books; 4) have difficulty hearing on the telephone; 5) have limited/ no access to a telephone; 6) have been hospitalized with a stroke, myocardial infarction, or cardiac surgery in the past 3 months; or 7) who are actively enrolled in another clinical trial or clinical pharmacy services (Table 1).
Table 1.
CSP Intervention Encounter Type & Frequency (Encounters scheduled to occur every 4 weeks)
| Encounter 1 | Encounter 2 | Encounter 3 |
|---|---|---|
| Module Name | Module Name | Module Name |
| Medication Reconciliation Adjustment for Lipid & Asprin medications |
Self-Monitoring (BP, BG collected) | Medication |
| Risk Factor Knowledge I: Lipids and Anti-platelet | Medication Reconciliation Adjustment of HTN, BG, NRT medications if clinically indicated based on self monitoring |
Diet |
| Apnea | Risk Factor Knowledge 2 | Weight |
| Hypoglycemia | Smoking 1mo f/u | |
| Smoking |
| Encounter 4 | Encounter 5 | Encounter 6 |
|---|---|---|
| Module Name | Module Name | Module Name |
| Self Monitoring | Medication Reconciliation | Self-Monitoring |
| Medication adjustment of HTN & BG if clinically indicated based on self monitoring | Insomnia | Medication adjustment of HTN & BG if clinically indicated based on self monitoring |
| Exercise | Mental Health | Diet |
| Weight 1 Month follow-up | Exercise 1 Month follow-up |
| Encounter 7 | Encounter 8 | Encounter 9 |
|---|---|---|
| Module Name | Module Name | Module Name |
| Medication Adjustment Lipid & Aspirin |
Self Monitoring (BP, BG collected) | Medication |
| Hypoglycemia 2 | Medication (HTN, BG, NRT) | Diet |
| Alcohol | Smoking 6 month Follow-up | Weight 6 month follow-up |
| Choice Module |
| Encounter 10 | Encounter 11 | Encounter 12 |
|---|---|---|
| Module Name | Module Name | Module Name |
| Self Monitoring | Medication | Medication |
| Medication adjustment for HTN & DM medications | Mental Health | Choice Module/make-up |
| Insomnia | Alcohol |
| Encounter 13 | Encounter 14 | Encounter 15 |
|---|---|---|
| Anytime during 12 month intervention | Encounter 2,4,6,8, & 10 | Encounter 7-12 |
| Module Name | Module Name | Module Name |
| Subject Initiated-= When patient calls outside of intervention schedule | Self-Monitoring | Choice/Make-up (Includes Diet, Exercise, Smoking, Weight, Risk) |
Sample Identification
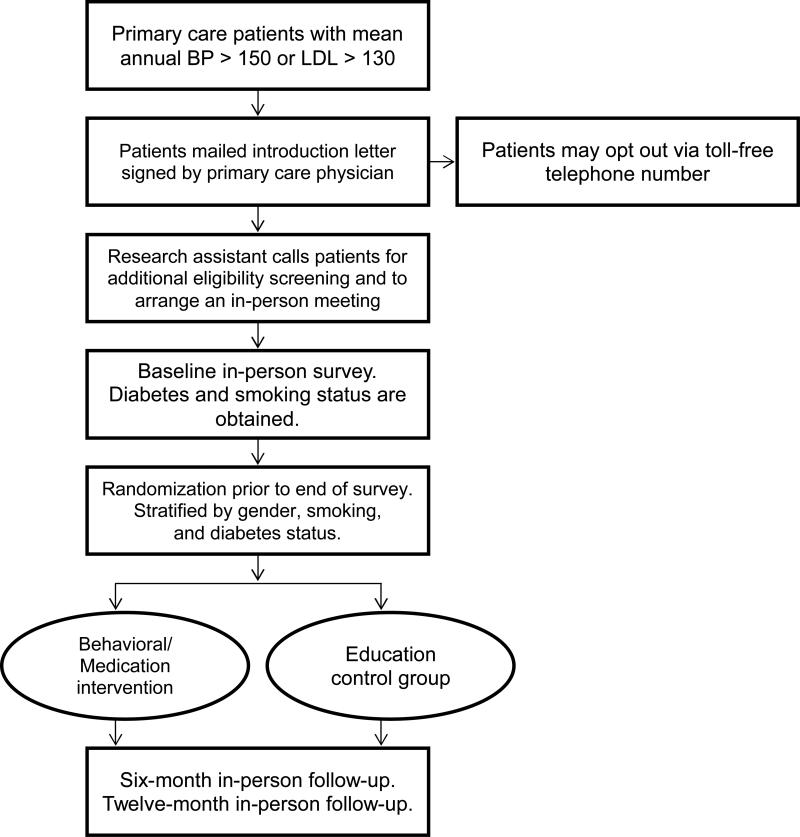
Participants meeting inclusion criteria 1-5 are initially identified from electronic medical records. The lists of identified patients are sorted by upcoming appointment (Figure 1). Patients meeting initial screening criteria are mailed an introductory letter signed by their PCP. The remaining patients who qualify are contacted by study personnel for additional eligibility screening and to schedule an in-person meeting. Once informed consent to participate has been obtained from patients, the baseline outcome assessment are completed. Patients are randomized to the intervention or the control group; randomization is stratified by gender, smoking, and diabetes status. Patients randomized to the control group receive educational material about CVD reduction but have no CPS contact.
Figure 1.
Study Flow.
Intervention
During 12 monthly phone calls medication adjustments are made at intervals based on patients’ self management, lab values, medication interactions, reported and observed medication side effects, clinical assessment, patients’ report of medication adherence and disease monitoring (Figure 2). During these phone calls the CPS also delivers a tailored behavioral, concomitant telemedicine intervention to improve treatment adherence, exercise, diet, weight and smoking cessation. In particular the CPS focuses on: 1) expanding patients’ understanding of each medication and its role in disease management; 2) education on preventive care; and 3) offering strategies to enhance adherence.
The initial two encounters provide an intense review and complete medication history of the patients’ current and discontinued cardiovascular medications. The encounters also provide comprehensive medication education based on patients’ current understanding of their cardiovascular medications.
Self-Management Component
Home Blood Pressure (BP) Monitors
Patients randomized to the intervention receive a VA-issued home BP monitor. Patients receive training on BP monitor use and are instructed to use it every other day. 2,15 When the CPS contacts patients at the month prior to the potential medication management activation, the pharmacist reminds individuals to record their BP values. Poor BP control detected by home monitoring is defined as an average bi-weekly BP that falls above the threshold (<135/85 for non-diabetics and <130/80 for diabetics).2
Glucose Monitors
Insulin dependent patients, anticipated 50% of the study cohort based upon a prior study,16 are requested to perform daily self-monitored blood glucose testing (SMBG) equal to their number of daily insulin doses. Patients who are managed on oral hypoglycemic medications alone are encouraged to monitor blood glucose (BG) at least one time per week or if signs or symptoms of hypoglycemia occur based on VA policy.17 We evaluate each patient's monitoring technique at baseline, 6, and 12-month follow-up interviews.
Medication Management Intervention and Time Intervals
The goal of the intervention is to supplement clinic-based management to more efficiently implement interventions that may otherwise be left until the next appointment. This model has worked well in previous VA studies.2 For patients who require a prescription change, the pharmacist communicates the change with the VA pharmacy. At the next monthly contact, the pharmacist will assess new symptoms (e.g., hypotension, hypoglycemia). This will allow adequate time for the patient to obtain medication and get accustomed to the change. Any medication change that requires additional testing is ordered and followed-up. In cases where a medication change is made, a note is generated for the patient's medical record and co-signed by the patient's PCP acknowledging receipt of the treatment plan. This algorithmic method of assessing the need for medication management and providing documentation was previously tested.2 When serious adverse events occur, the pharmacist consults with the patient's PCP and study clinicians to take appropriate action and/or make further recommendations.
Blood Pressure
Individuals are instructed to record BP values for at least two weeks prior to the 2, 4, 6, 8 and 10-month CPS contacts, when medication management activation for hypertension may occur. A home BP value of >135/85 mm Hg is considered poorly controlled BP in patients without diabetes even though it is lower than the clinic based target of 140/90 mm Hg.4 This is the same BP goal set in a clinical trial of medication management based on home values that yielded a positive result without adverse events.18 We activate intensification of therapy in the intervention group based on a two-week average home BP of >135/85 for non-diabetics and >130/80 for diabetics. Through the use of standard scripts and prompts the clinical pharmacist is encouraged to consider principles in medication management decisions when clinically appropriate to ensure intervention fidelity and reproducibility.
Cholesterol
Non-fasting blood lipid concentrations are measured at baseline, 6, and 12-month visits. LDL-C is measured directly. Medication adjustments are made based on LDL-C concentrations obtained at one and seven months. This 6-month interval for assessment and treatment is recommended by the National Cholesterol Education Program. Medication management in accordance with VA guidelines will be triggered to LDL-C levels for high CVD risk patients defined as >100mg/dl.19
The cholesterol algorithm focuses on use of HMG-CoA reductase inhibitors as the primary means of bringing LDL–C to goal with a target LDL-C of <100mg/dl.20 Unless contraindicated, drug therapy is selected to provide the reduction necessary to obtain LDL-C goals.
Blood Glucose
Using a similar strategy to home BP monitoring, we instruct individuals with diabetes on medications to provide glucose values at least two weeks prior to the 2, 4, 6, 8 and 10-month potential medication management activation. Clinically relevant findings reported by the patient including medication side effect, signs of symptoms of hyper or hypoglycemia, difficulties with administering medications or testing blood glucose may activate the intervention at any time. The medication management of diabetes focuses on achieving target HbA1c <7.0% and pre-prandial fasting glucose between 70-130 mg/dl according to the American Diabetes Association (ADA) standards of care.21
Smoking Cessation
Smoking status is assessed at encounters 1, 2 and 8 months. A tailored behavioral intervention is initiated for smoking patients in encounter 2 and 8. Barriers to initiating and maintaining smoking cessation are explored and benefits emphasized. Among those in the process of quitting smoking or recently stopped, strategies to maintain this behavior are explored. The pharmacist explores potential barriers to smoking cessation using motivational interviewing techniques and sets goals for smoking cessation.
Antiplatelet Therapy Use
The use of aspirin is strongly supported by the ADA and has been recommended for prevention of CVD events in high-risk diabetic and non-diabetic individuals.22 Dosages used in most clinical trials ranged from 75 to 325 mg/day.23 Unless contraindicated as evidence by drug allergy, prior sensitivity, or gastrointestinal bleeding within the prior six months, daily aspirin should be considered. Use of aspirin is assessed at one and seven months with recommendations for use for those who are eligible and currently using.
Side Effects of Medication
At each phone call, the CPS queries the patient about any specific medication side effects. In the event of a side effect, the CPS examines how side effects may be impacting medication adherence and considers alternatives. The CPS contacts the provider if a patient reports any potentially life-threatening side effect.
Behavioral Modules
The behavioral component of the intervention is activated monthly and is accompanied by medication reconciliation. Behavior change theories are used for understanding treatment adherence.24, 25 Understanding the factors that hinder or promote health behaviors are central to the Transtheoretical Model 26 which is incorporated in the intervention. All information reviewed in the modules is supplemented with written materials in the study handbook provided to intervention patients at enrollment.
Medication Adherence
Individuals lacking pill refills are queried about difficulties obtaining their prescriptions. Information on how to order and obtain medications is provided to all intervention patients. Patients who are medication non-adherent receive specific education.
Knowledge/Risk Perception
Patients receive tailored information about risk for CVD events based on their specific risk factors and laboratory values. To facilitate patient interpretation and understanding, this risk information is presented along with potential avenues for achievable risk reduction tailored to the patient's determinants of risk.
Diet
Patients may receive up to four diet modules. The diet modules focus on nutritional methods to improve cholesterol, BP, and HbA1c levels. The diet modules address salt intake, portion control, understanding food labels, heart healthy diets, and healthy carbohydrate foods. The CPS emphasizes food that is focused on increasing individuals’ vegetable, fruit, fiber, and protein intake – all that have been shown to be related to improve LDL glucose and BP outcomes.
Weight Loss
The CPS assesses patients’ stage of readiness to change for weight loss. The CPS explores potential barriers to meeting recommended levels of weight loss using motivational interviewing techniques as well as set goals for weight loss. The CPS helps to assure that patients set realistic goals.
Exercise
Once a patient's motivation regarding exercise is identified, the CPS may facilitate patient's progression through stages. For patients not exercising and not ready to change, the CPS explores reasons for lack of activity. The CPS provides information about benefits of increasing physical actively. Among patients who are thinking about changing their activity levels, or who have already changed, the CPS reinforces these behaviors and problem solve and address any foreseeable barriers that may limit their abilities to start or maintain an exercise regimen. The CPS also explores potential barriers to meeting recommended levels of exercise using motivational interviewing techniques as well as set goals for exercise.
Primary Outcome
The CVD risk profile, a composite score of CVD risk, was selected as the primary endpoint to account for the given synergistic effects of the intervention.9 The Cardiovascular Risk Profile9, combines smoking status, diabetic status, total and high-density lipoprotein (HDL) cholesterol, SBP differentiated according to treatment for hypertension, and age (Table 2). Data for CVD risk profile calculation will be collected at baseline, 6, and 12 months. The computed risk profile represents risk of CVD event or mortality in the next 10 years. We chose the CVD risk profile because risk factors for CVD often coexist; it is increasingly clear that CVD risk factors increase the total or absolute CVD in a multiplicative rather than additive manner.9 This particular risk profile was derived for use in primary care settings.9 Individual components of this risk profile are targets of the intervention (e.g., SBP, lipids, and smoking status). While other Framingham risk profiles exist10, 11 their adopted use in primary care patients has been slow due to requirements for variables that are not routinely available. The CVD risk profile incorporates both modifiable and non-modifiable patient characteristics. The modifiable characteristics include SBP, total cholesterol, High Density Lipoprotein (HDL-C), and current smoking status. Non-modifiable characteristics include age and gender. The formulas presented in the D'Agostino et al 9 are used to calculate the actual risk probability.
Table 2.
| Primary Outcomes | Data needed to calculate CVD risk profile (total cholesterol, HDL, smoking status, SBP (treated or untreated), age, gender, diabetes status) | Continuous | |
| Secondary Outcomes | Body mass index | continuous | |
| Exercise81 | Construct validity, reliability and is sensitive to change. Predictive of VO2 and other performance measures 0.44 to 0.68.82 | continuous | |
| Diet17,70 | predictive validity; correlated with percentage energy and cholesterol.83 | continuous | |
| Medication adherence 84/pill refill85 | alpha = .68; sensitivity of 55% & specificity of 87% compared with pill counts.84 | Categorical | |
| Smoking cessation | salivary cotinine | categorical | |
| Quality-adjusted Life Years (QALYs) | continuous |
Secondary Outcomes
Secondary outcomes include improvements in health behaviors over time (Table 2). The outcome variables, improved health behaviors, will include the following: medication adherence, physical activity, improved dietary pattern, lower body mass index.12,13 Medication adherence is measured by patient self-report using a modified Morisky Questionnaire and medication possession ratio at baseline, 6 months, and 12 months.12 ReComp, a validated, continuous, multiple-interval measure calculates the proportion of days that a medication was available to patients during an observation period in patients with hypertension.14 Unlike traditional medication possession ratio measures, ReComp also considers the possibility of oversupply, or stockpiling, of medications by examining a predetermined global time period of medication adherence.
Study Fidelity
To ensure that the tailored information is standardized, the CPS uses a custom intervention software application that contains predetermined scripts and patient-specific tailored algorithms. At the conclusion of the study, the application database will contain an entire record for each patient describing what occurred during the 12-month intervention period. The duration of each call is recorded for later use in cost-effectiveness and other types of implementation-related analyses.
Statistical Methodology
Statistical analyses will examine: 1) changes in CVD risk profile over time, 2) improvement in health behaviors over time.
Changes in CVD Risk Profile over Time
A general linear model (GLM) will be used to estimate changes in CVD risk profile over time. This model will examine whether Veterans who receive the intervention have greater improvement of their general CVD risk profile over the 12 months of follow-up as compared to the control group.27 The stratification variables of gender, diabetes, and smoking status will also be included as predictors. Because of the small number of time points, we will apply an unstructured covariance matrix to take into account the within-patient correlation between repeated measures over time. Changes in LDL will be examined with a linear model and an unstructured covariance matrix. For Veterans with diabetes, changes in HbA1c will also be examined with a linear model.
Improvement in Health Behaviors Over Time
With the exception of medication adherence, health behaviors are continuous variables. Therefore, a linear model will estimate changes in the secondary outcomes of health behaviors over time. The measure of medication adherence will be dichotomized to represent “adherence” and “non-adherence”. The probability of adherence over time will be modeled using generalized estimating equations with a logit link. For all models, we use an unstructured covariance to take into account the within patient correlation over time.
Power and Sample Size Considerations
Sample size was estimated via methods and software discussed by Rochon.28 A two-sided type-I error rate of 5% and a power of 80% was applied in all calculations. We used preliminary data from the V-STITCH study15 to estimate quantities needed for sample size calculation. We anticipated a mean probability of CVD risk of 40%, a standard deviation of 19.5% in both treatment groups at baseline, and the correlation between baseline, months 6 and 12 was assumed to be 0.7. We generated sample size estimates for an intervention-by-time effect that resulted in differential intervention-group improvement of 6% by 12 months. A minimum of 197 patients per intervention group was estimated, for a total study size of 394 patients. Assuming a 15% dropout rate and rounding up to protect against deviations from our assumptions, we plan to enroll and randomize 500 patients, 250 in each group.
Discussion
CITIES is a telephone-based strategy that focuses on clinically-indicated management of hypertension, hypercholesterolemia, diabetes, smoking cessation and anti-platelet therapy through promoting patient self management, medication management, and behavioral interventions. An estimated one-in-three American adults have CVD. The burden of the disease remains high; more than 80% of veterans have at least 2 risk factors for CVD.1 Clinical and economic consequences of this anticipated increase in CVD are enormous.
Given the national prevalence of CVD and the dismal rates of risk factor control, intensive, but easily disseminated interventions are required to treat this epidemic. Comprehensive programs that employ tailored patient self-management, pharmacotherapy and behavioral interventions are needed to address multiple barriers to optimal cardiovascular risk reduction. CPS directed care with physicians or nurses have demonstrated improvement in the management of the individual major CVD risk factors in outpatients.6-8 Currently within PACTs, face-to-face CPS-directed and nurse management is mostly employed. While this approach has proven to be successful, the process can be time and labor intensive. Efficient modes of interventions to manage patients who are at increased risk for CVD are needed due to : 1) the expensive and scarce resource of CPS in the VA, 2) patients’ travel limitations, 3) space restrictions, 4) the need to determine the best use of resources with the development of PACTS, and 5) increasing demand for health care it is imperative we investigate more
This intervention is designed to address these barriers of face-to-face care. First, in an effort to increase efficiency the behavioral modules are only activated for those with identified problems and when activated, the modules are tailored to the patient's needs and readiness to change. Secondly, the medication algorithms are automated through a comprehensive database making it easy to implement evidence based medication decision.
Clinical inertia, the phenomenon of providers failing to intensify medication regimens at encounters with patients who have uncontrolled risk factors, has been cited to potentially account for a significant proportion of CVD events, suggesting that alternative methods for interventions may be needed.29 Also, clinic visits are primarily focused on symptom management, leaving little time for comprehensive risk factor and medication management. An intervention delivered in patients’ homes for non-symptom, chronic disease healthcare offers one possibility to reduce healthcare barriers. Telephone interventions allow more patients to be reached and these interventions may be more convenient than in-person interventions. Delivering an intervention by telephone may enhance the interventions’ cost-effectiveness, primarily due to reduced costs and visit rates coupled with the clinicians’ ability to follow a much larger panel over which to spread fixed intervention costs than would be possible with an in-person intervention.
If successful this telephone-based intervention can facilitate individualized, personal interaction (i.e., tailored to participants’ current concerns, health goals, and specific barriers to achieving these goals) at lower costs to the system and patients. In addition if the proposed intervention is able to achieve or surpass national control targets set by Healthy People 2010 and the VA, information from this study could significantly improve current clinical practice.
ACKNOWLEDGEMENTS
This study was funded by a grant from the VA Health Service Research and Development to Dr. Bosworth (VA HSR&D IIR (08-297). Dr. Bosworth was supported by research career scientist award from the VA Health service research and development (VA HSR&D 08-027). Ms. Zullig is supported by funding from the National Cancer Institute (5R25CA116339). No authors have conflicts of interest. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
REFERENCES
- 1.Richlie D, Winters S, Prochazka AV. Dyslipidemia in veterans: Multiple risk factors may break the bank. Arch Intern Med. 1991;151:1433–1436. doi: 10.1001/archinte.151.7.1433. [DOI] [PubMed] [Google Scholar]
- 2.Bosworth H. Hypertension Intervention Nurse Telemedicine Study (HINTS): Testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control.. National Institute of Health (NIH) Workshop, Future of Telehealth: Essential Tools and Technologies for Clinical Research and Care; Bethesda MD. 2009.2009. [Google Scholar]
- 3.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Therapeutic goal attainment in patients with hypertension and dyslipidemia. Med Care. 2006;44(1):39–46. doi: 10.1097/01.mlr.0000188982.25397.37. [DOI] [PubMed] [Google Scholar]
- 4.Staessen JA, Thijs L. Development of diagnostic thresholds for automated self-measurement of blood pressure in adults. First International Consensus Conference on Blood Pressure Self-Measurement. Blood Press Monit. 2000;5(2):101–9. [PubMed] [Google Scholar]
- 5.Piette JDHB, Beard AJ, Blaum C, Greenstone CL, Krein SL, Tremblay A, Forman J, Kerr EA. Improving chronic illness care for veterans within the framework of the patient-centered medical home: Experiences from the ann arbor patient-aligned care team laboratory. Translational Behavioral Medicine. 2011:615–623. doi: 10.1007/s13142-011-0065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Arch Intern Med. 2011;171(16):1441–53. doi: 10.1001/archinternmed.2011.399. [DOI] [PubMed] [Google Scholar]
- 7.Chisholm-Burns MA, Lee JK, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, et al. US Pharmacists’ Effect as Team Members on Patient Care: Systematic Review and Meta-Analyses. Med Care. 2010 doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 8.Chisholm-Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923–33. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 9.D'Agostino RB, Sr., Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 10.Grundy SM, Pasternak R, Greenland P, Smith S, Jr., Fuster V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation. 1999;100(13):1481–92. doi: 10.1161/01.cir.100.13.1481. [DOI] [PubMed] [Google Scholar]
- 11.Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 12.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Stewart AL, Gillis D, Grossman M, Castrillo M, Pruitt L, McLellan B, et al. Diffusing a research-based physical activity promotion program for seniors into diverse communities: CHAMPS III. Prev Chronic Dis. 2006;3(2):A51. [PMC free article] [PubMed] [Google Scholar]
- 14.Bryson CL, Au DH, Young B, McDonell MB, Fihn SD. A refill adherence algorithm for multiple short intervals to estimate refill compliance (ReComp). Med Care. 2007;45(6):497–504. doi: 10.1097/MLR.0b013e3180329368. [DOI] [PubMed] [Google Scholar]
- 15.Bosworth HB, Olsen MK, Dudley T, Orr M, Goldstein MK, Datta SK, et al. Patient education and provider decision support to control blood pressure in primary care: a cluster randomized trial. Am Heart J. 2009;157(3):450–6. doi: 10.1016/j.ahj.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Edelman D, Fredrickson SK, Melnyk SD, Coffman CJ, Jeffreys AS, Datta S, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689–96. doi: 10.7326/0003-4819-152-11-201006010-00001. [DOI] [PubMed] [Google Scholar]
- 17.Department of Veterans Affairs OoQaP . Diabetes Mellitus Algorithm G: Glycemic Control. Washington, D.C: [Google Scholar]
- 18.Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17(10):921–7. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 20.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 21.Standards of medical care in diabetes--2008. Diabetes Care. 2008;31(Suppl 1):S12–54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 22.Hennekens CH, Knatterud GL, Pfeffer MA. Use of aspirin to reduce risks of cardiovascular disease in patients with diabetes: clinical and research challenges. Diabetes Care. 2004;27(11):2752–4. doi: 10.2337/diacare.27.11.2752. [DOI] [PubMed] [Google Scholar]
- 23.A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. Jama. 1982;247(12):1707–14. doi: 10.1001/jama.1982.03320370021023. [DOI] [PubMed] [Google Scholar]
- 24.Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, Fiore C, Harlow LL, Redding CA, Rosenbloom D, Rossi SR. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13:39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- 25.DiClemente CC, Prochaska J. Toward a comprehensive transtheoretical model of change. In: Healther WRMN, editor. Treating addictive behaviors. Plenum Press; New York: 1998. pp. 3–24. [Google Scholar]
- 26.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 27.Fitzmaurice G, Laird NM, Ware JH. Applied Longitudinal Analysis. Wiley Series in Probability and Statistics. 2004 [Google Scholar]
- 28.Rochon J. Application of GEE procedures for sample size calculations in repeated measures experiments. Statistics in Medicine. 1998;17:1643–1658. doi: 10.1002/(sici)1097-0258(19980730)17:14<1643::aid-sim869>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 29.McFarlane SI, Jacober SJ, Winer N, Kaur J, Castro JP, Wui MA, et al. Control of cardiovascular risk factors in patients with diabetes and hypertension at urban academic medical centers. Diabetes Care. 2002;25(4):718–23. doi: 10.2337/diacare.25.4.718. [DOI] [PubMed] [Google Scholar]