Abstract
Venezuelan equine encephalitis virus (VEEV) is an arbovirus that causes periodic outbreaks that impact equine and human populations in the Americas. One of the VEEV subtypes located in Mexico and Central America (IE) has recently been recognized as an important cause of equine disease and death, and human exposure also appears to be widespread. Here, we describe the use of an Internal Ribosome Entry Site (IRES) from encephalomyocarditis virus to stably attenuate VEEV, creating a vaccine candidate independent of unstable point mutations. Mice infected with this virus produced antibodies and were protected against lethal VEEV challenge. This IRES-based vaccine was unable to establish productive infection in mosquito cell cultures or in intrathoracically injected Aedes taeniorhynchus, demonstrating that it cannot be transmitted from a vaccinee. These attenuation, efficacy and safety results justify further development for humans or equids of this new VEEV vaccine candidate.
Keywords: Venezuelan equine encephalitis virus, vaccine, alphavirus, internal ribosome entry site
Introduction
Venezuelan equine encephalitis virus (VEEV; family Togaviridae, genus Alphavirus), the etiologic agent of Venezuelan equine encephalitis (VEE), is an arthropod-borne virus (arbovirus) of significant medical and veterinary importance throughout Central and South America. VEEV causes neurologic disease in horses, and infected people typically present with nonspecific flu-like symptoms including fever, malaise and headaches. The virus can cause encephalitis and death, but such severe manifestations are mostly observed in children. The epidemiology of VEE is complicated by the presence of several antigenic subtypes. Viruses within the VEE antigenic complex comprise antigenically and geographically distinct subtypes (IAB, IC, ID, IE, II-VI). Historically, major epidemics have been caused by the IAB and IC subtypes, which arise from ID enzootic progenitors (Brault et al., 2002; Greene et al., 2005). Enzootic subtypes circulate continuously within a rodent/mosquito cycle, serving as an ever-present source of future epizootic events.
Although the IE subtype has been primarily regarded as avirulent in equids (Garman et al., 1968; Walton et al., 1973), recent data suggest that these viruses cause widespread disease in horses and humans (Adams et al., 2012; Gonzalez-Salazar et al., 2003; Oberste et al., 1998). Outbreaks in Mexico in 1993 and 1996 were characterized by high equine mortality from VEEV IE infections (Oberste et al., 1998). These viruses were antigenically indistinguishable from other previous IE Mexican isolates (Oberste et al., 1998), and phylogenetically more similar to other enzootic IE strains than to other equine-virulent outbreak strains (Brault et al., 2002; Oberste et al., 1999), suggesting that VEEV IE viruses are a previously disregarded etiologic agent of VEE in equids and a significantly underestimated veterinary threat. Serosurveillance of humans, dogs, cattle and equids indicate that many infections occur within populations located along the Gulf Coast-bordering states of Mexico (Estrada-Franco et al., 2004), sometimes at a high prevelane rate (Adams et al., 2012).
The VEEV genome is a single-stranded, positive-sense RNA molecule, which is polyadenylated following the 3′ untranslated region (UTR) and capped at the 5′ UTR. Two open reading frames are translated to encode the nonstructural proteins (nsP1-4) and the structural proteins (C, E3, E2, 6k and E1). The structural genes are translated from a subgenomic RNA transcript generated via the subgenomic promoter (SGP) located partially within the nsP4 gene. The subgenomic transcript is found in molar excess to the genomic RNA, thus leading to the quick and abundant generation of structural proteins for virion assembly (Frolov et al., 1996).
Several vaccine candidates to protect against VEE have been generated. The best characterized, TC-83, was generated by passaging the virulent prototype IAB Trinidad donkey (TrD) strain 83 times in guinea pig heart cells to generate attenuating point mutations. This liveattenuated, tissue culture-adapted vaccine is currently used to vaccinate horses and has been successful in preventing the spread of transmission during outbreaks. Because TC-83 is reactogenic in human volunteers and does not induce efficient immune responses in all vaccine recipients (Pittman et al., 1996), it remains an Investigational New Drug (IND) for human use with limited availability for at risk laboratory and military personnel (Pittman et al., 1996). Long-term humoral immune responses are limited against other VEEV serotypes, particularly ID, IE, II, III and IV (Burke et al., 1977; Fillis and Calisher, 1979), which may lead to incomplete protection from disease. The cell culture passages used to generate TC-83 resulted in 12 point mutations (Kinney et al., 1989), of which 2 located in E2 gene and the 5′ UTR, respectively, are responsible for the attenuated phenotype (Kinney et al., 1993). As such, reversion to a wild type-like phenotype is possible under certain conditions. Furthermore, TC-83 was isolated from mosquitoes in Louisiana following its use in halting the 1969-72 epidemic in Texas (Pedersen et al., 1972), indicating that mosquitoes are capable of being infected by and disseminating TC-83.
Other live-attenuated vaccines were engineered to improve upon the aforementioned drawbacks of TC-83. A targeted mutagenesis approach was taken to create V3526, an attenuated IAB-based VEE vaccine with a PE2 (E2 precursor protein) cleavage mutation and an E1 (Phe253Ser) suppressor substitution (Davis et al., 1995). V3526 was attenuated (Ludwig et al., 2001), immunogenic and protected adult mice from virulent IAB challenge (Davis et al., 1995; Hart et al., 2000; Pratt et al., 2003), but the virus could still infect and disseminate within intrathoracically or orally exposed mosquitoes encoding the nonstructural genes from the relatively benign Sindbis virus and the structural genes of VEEV (Paessler et al., 2006), have the safety advantage of an attenuation mechanism that is independent of point mutations and that exhibits improved phenotypic stability (Kenney et al., 2011). However, some of these chimeric vaccines still suffer from the flaw of potential mosquito transmission.
For these reasons, we sought to develop a vaccine that 1) is easily tolerated, 2) contains a mechanism of attenuation independent of unstable point mutations, and 3) cannot be transmitted by mosquitoes from a vaccinee. Previously, Volkova et al. reported on the use of an Internal Ribosomal Entry Site (IRES) from encephalomyocarditis virus (EMCV) inserted within the TC-83 genome that fulfilled the above criteria (Volkova et al., 2008). The EMCV IRES was selected because it functions to initiate translation inefficiently in insect cells while retaining strong functionality in mammalian cells (Finkelstein et al., 1999; Woolaway et al., 2001). This feature provided the mammalian-restricted tropism desired for an arbovirus vaccine. TC-83 containing a mutagenized SGP and an EMCV IRES driving translation of the structural genes (VEEV/mutSGP/IRES) provided partial protection in mice challenged with a virulent subtype IC VEEV (Volkova et al., 2008). However, this protection was not complete, indicating a need for improvement (Volkova et al., 2008). Here, we describe the use of this IRES-based technology to create a more immunogenic vaccine candidate to protect against the IE serotype of VEEV.
Results
Construction of IRES-containing 68U201 genomes
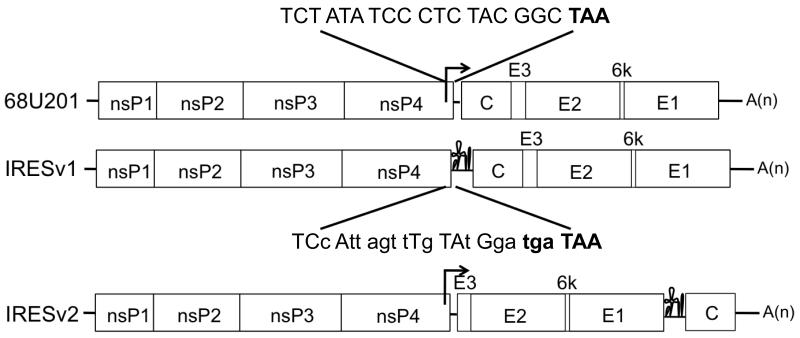
Previously, an infectious cDNA clone was generated based upon the 68U201 strain (Powers et al., 2000), a IE subtype isolate from a sentinel hamster in Guatemala in 1968. Virus generated from this clone has been well characterized in mice (Brault et al., 2002) and is also infectious in its mosquito vector (Kenney et al., 2012). Two basic modifications were made to this clone to generate new VEEV vaccine candidates: 68U201/IRESv1 and 68U201/IRESv2 (Fig. 1). These variants were primarily based upon previous studies using TC-83 (Volkova et al., 2008)(Guerbois, submitted) and chikungunya (Plante et al., 2011) viruses. Briefly, 68U201/IRESv1 had an EMCV IRES driving the translation of the entire structural protein region (capsid-E1). The clone was constructed by mutagenizing the SGP with 14 synonymous mutations including an added opal stop codon to maintain the amino acid sequence of nsP4 but ablate the activity of the promoter (Fig. 1). The EMCV IRES was inserted directly after the second engineered stop codon but before the start codon of the capsid protein. For 68U201/IRESv2, capsid protein translation was dependent upon the IRES. The SGP was unaltered, and remained functional, but was directly followed by the inserted start codon and E3 gene. The capsid gene was transferred at the end of the E1 coding sequence, fused directly behind the EMCV IRES sequence (Fig. 1).
Fig.1. Diagram of the wt 68U201 VEEV genome and IRES-based vaccine candidates.
The mutated portion of the subgenomic promoter is shown on the top, with synonymous mutations shown in lowercase and stop codons highlighted in bold at the bottom.
68U201/IRES characterization in vitro
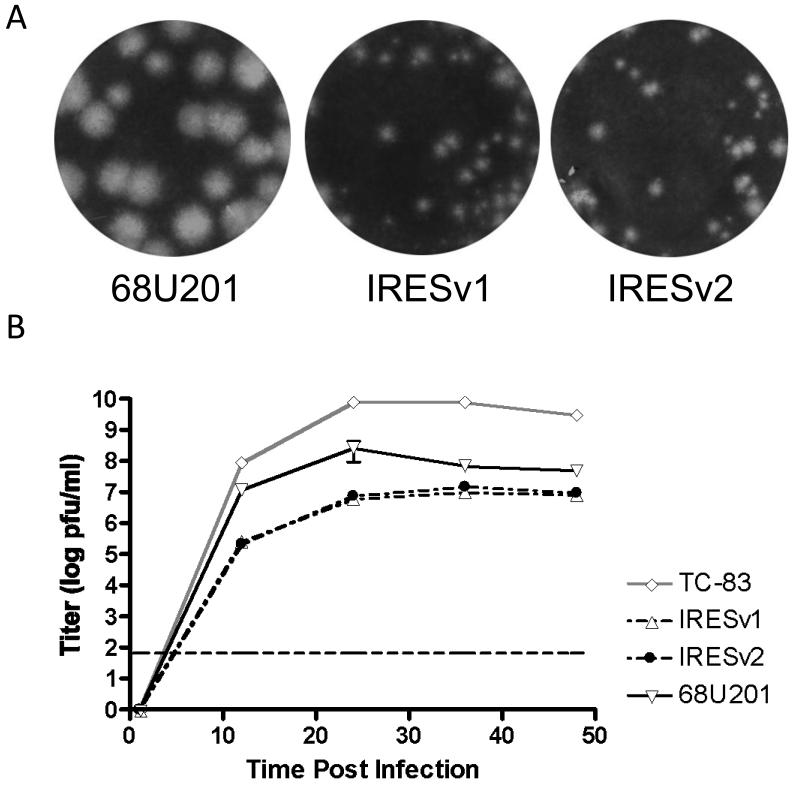
One of the attractive features of inserting an IRES in lieu of the SGP is the ability to attenuate viral replication independently of point mutations. In vitro attenuation of the 68U201/IRESv1 and v2 viruses was measured by plaque size and replication curves compared to both 68U201 and/or TC-83. The sizes and morphologies of the plaques produced from these infections are shown in Fig. 2A. 68U201/IRESv1 and v2 viruses produced much smaller plaques than 68U201, but similar in size to TC-83 (data not shown). This attenuation was also reflected in the titers achieved following RNA electroporation; maximum titers of either 68U201/IRESv1 or v2 were approximately 1-5×106 plaque-forming units per milliliter (pfu/ml) whereas 68U201 vRNA produced a titer of approximately 1×108 pfu/ml under identical conditions (data not shown). Both 68U201/IRESv1 and v2 constructs had the same specific infectivity (PFU/μg RNA electroporated into Vero cells) as the parental 68U201 infectious clone (data not shown).
Fig.2. In vitro characteristics of vaccine candidates, their parent strain 68U201, and vaccine strain TC-83.
(A) Vero cell plaques measured 48 hpi in a 6-well plate. (B) Replication curves were performed in triplicate replicates at an MOI of 0.1 pfu/Vero cell. The timepoint at 1 hpi was below the limit of detection (dashed line) and arbitrarily assigned a titer of 1 pfu/ml. Error bars denote standard deviation.
To better quantify the replication kinetics of the IRES vaccines, Vero cells were infected at a multiplicity of infection (MOI) of 0.1 pfu/cell and media were harvested at various time points (Fig. 2B). At all time points tested, the titers of both 68U201 and TC-83 exceeded those of either 68U201/IRESv1 or v2. Both 68U201/IRES viruses produced similar titers at all time points tested (Fig. 2B). At the last time point taken, the monolayers infected with 68U201 or TC-83 were destroyed whereas both 68U201/IRESv1 and v2 had begun to show signs of widespread CPE.
68U201/IRES viruses in adult mice
To determine the ability of 68U201/IRES viruses to serve as vaccines, adult female CD1 mice were vaccinated subcutaneously (s.c.) with 1×105 pfu and monitored for signs of illness and changes in weight. TC-83 and 68U201 were used as controls.
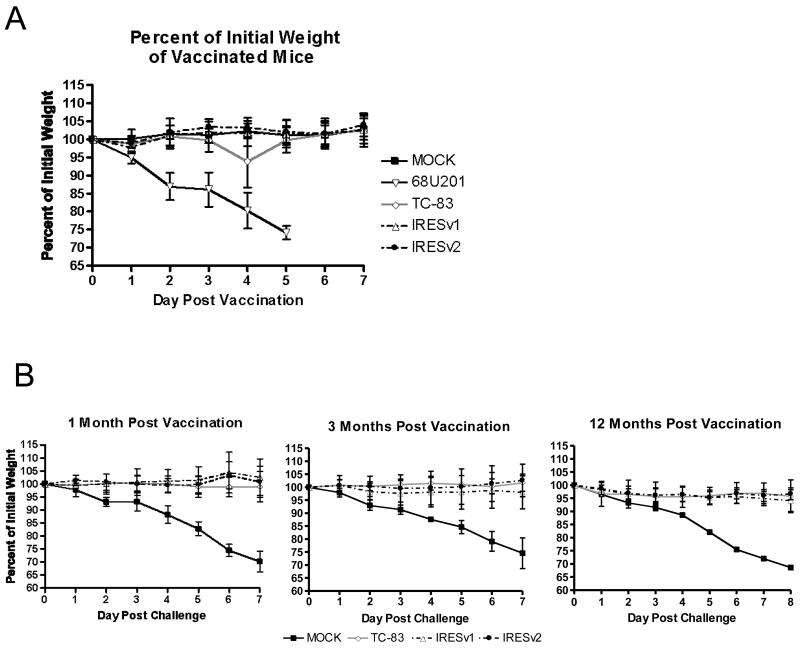
All mice tolerated the 68U201/IRES vaccines well; there were no significant fluctuations in weight or signs of illness for at least 7 days after infection, except in mice vaccinated with TC-83 on day 4 (Fig. 3A). While this difference was statistically significant compared to the MOCK cohort (P<0.001), other studies with TC-83 within our laboratory did not to show this weight change on day 4, suggesting a short-term affect within the cage. The only other mice that showed morbidity and mortality were infected with the parental 68U201 strain (Fig. 3A). Mice began to show signs of illness by day 2 post infection, which corresponded with daily weight losses and fulfilled the criteria for morbidity resulting in euthanasia.
Fig.3. Safety, immunogenicity and efficacy of vaccines in mice.
Female CD1 mice, aged 6-8 weeks, were vaccinated or infected s.c. with 1×105 pfu of virus, and weighed for 7-8 days thereafter. (A) The percent of initial weight following vaccination and (B) the percent of initial weight after challenge at 1, 3, or 12 months after vaccination. Error bars indicate standard deviation.
All mice vaccinated with TC-83, 68U201/IRESv1 or v2 that were challenged with a lethal dose of 68U201 at 1, 3, or 12 months post vaccination were protected from morbidity and mortality (Fig. 3B). No vaccinated mice showed statistical changes in weight over time compared to any other groups except for the MOCK-vaccinated group. Like after initial vaccination, the only mice that showed signs of illness lost weight, which followed in most cases with death (Fig. 3B and Table 1). The mouse (1 of 5, Table 1) that survived challenge at 3 months post mock-vaccination showed signs of illness and weight loss during the first 7 days, but never met euthanasia criteria. It eventually began to gain weight and survived. Vaccinated mice challenged at one-year post vaccination, although fully protected against disease resulting from 68U201 infection (Table 1), showed slight weight loss (Fig. 3B) in the absence of overt signs of illness. This may have been due to the old age (14 months) or the mass (49.7 +/− 8.3 grams) of the mice at the time of challenge. Regardless, signs of illness and weight loss were greatest in the unvaccinated mice, all of which succumbed to infection by day 10.
Table 1.
Efficacy of vaccines one to twelve months after vaccination.
| 1 month after vaccination | 3 months after vaccination |
12 months after vaccination |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Vaccine | Na | % Survival |
MDDb | N | % Survival |
MDD | N | % Survival |
MDD |
| MOCK | 10 | 0 | 7.3+/−1.1 | 5 | 20 | 7.3+/− 1.5 |
3 | 0 | 6.7+/−2.9 |
| TC-83 | 19 | 100 | n/a | 5 | 100 | n/a | 3 | 100 | n/a |
| 68U201/IRESv1 | 21 | 100 | n/a | 10 | 100 | n/a | 6 | 100 | n/a |
| 68U201/IRESv2 | 12 | 100 | n/a | 10 | 100 | n/a | 7 | 100 | n/a |
N= number of mice in challenged cohort
MDD= mean day of death, +/− standard deviation, after challenge with 68U201 VEEV
Sera obtained on days 1 and 2 after vaccination were titrated to determine viremia (Fig. 4). No mice vaccinated with 68U201/IRESv1 or v2 produced detectable viremia on day 2, so all comparisons were made from day 1 samples. 68U201 produced a detectable viremia in all mice tested, with an average of 1×106 pfu/ml serum. TC-83 also produced a detectable viremia in all mice tested, but with a much lower average titer. 68U201/IRESv1- and v2-vaccinated mice showed reductions in viremia titer compared to both TC-83 and 68U201. Most striking was the viremia profile exhibited by 68U201/IRESv1-infected mice; fewer than half had a detectable viremia, the average of which was barely above the limit of detection.
Fig.4. Viremia following vaccination.
Sera taken on day 1 post vaccination were titrated for the presence of virus. The limit of detection is shown as a dashed line with a value of 67 pfu/ml. The combined data from three separate experiments are shown.
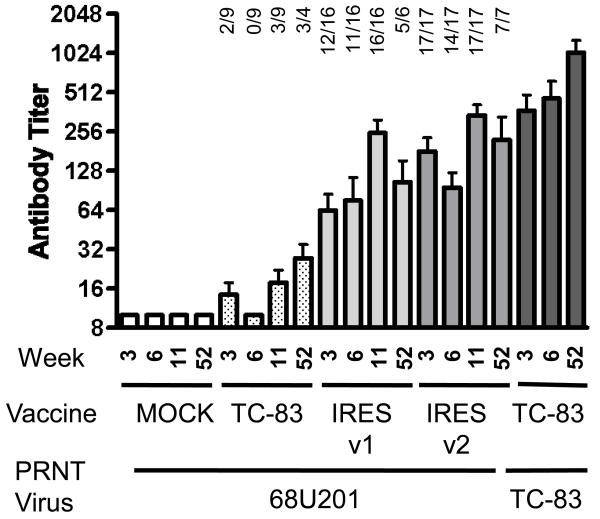
The antibody profiles in vaccinated mice were also assessed. Sera were harvested 3, 6, 11 and 52 weeks post vaccination to determine neutralizing antibodies levels by plaque reduction neutralization test (PRNT, Fig. 5). Seroconversion was determined by a PRNT80 titer of 1/20 or greater. By week 3, all 68U201/IRESv2 mice (17/17) and most 68U201/IRESv1 (12/16) mice had antibodies that neutralized 68U201 in vitro. At week 11, all 68U201/IRESv1 (17/17) and v2 (16/16)-vaccinated mice seroconverted. There was no statistical difference noted between titers on weeks 3 and 11 for either 68U201/IRESv1 or v2 (one-way ANOVA). Sera tested one year after vaccination showed the presence of 68U201-neutralizing antibodies in most animals tested. Titers from TC-83-vaccinated mice tested against heterologous strain 68U201 were low, likely due to poor cross-neutralization between IAB and IE viruses. When these sera were tested against TC-83, all mice had high neutralizing antibody titers at all time points tested (Fig. 5). Sera from MOCK-vaccinated mice failed to show neutralization.
Fig.5. Immunogenicity of vaccines.
Reciprocal PRNT80 titers at weeks 3, 6, 11 and 52 post vaccination were determined using VEEV strain 68U201 (IRES-based vaccines) or TC-83 (TC-83-vaccinated mice). Error bars denote standard error. All PRNT values <20 are recorded as 10, one dilution below the limit of detection. All PRNT titers >640 are reported as 640. The numbers above the bars denote the number of seropositive mice in each cohort.
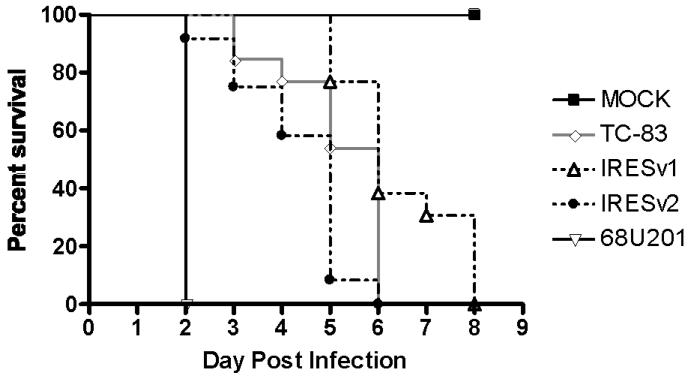
68U201/IRES attenuation in 6-day-old mice
Since the 68U201/IRES vaccines were well tolerated in adult mice, we sought to assess their attenuation in a sensitive and strict in vivo model: intracranial (i.c.) infection of 6-day-old mice. All mice inoculated with PBS survived and experienced normal growth during the 2-week observation period. The highest achievable i.c. dose, 2×104 pfu/mouse, was used for all groups. Ultimately, all viruses killed the mice, but at different times (Fig. 6). 68U201-infected mice (N=9) died by day 2. 68U201/IRESv2 (N=12) killed mice between 2 and 5 days post-infection with a mean day of death (MDD) of 4.3 days. 68U201/IRESv1 (N=13), on the other hand, had a MDD of 6.4 days and a significantly longer average survival than 68U201/IRESv2 (P<0.005, Logrank test).
Fig.6. Survival of 6-day-old mice injected intracranially with vaccines.
Six-day-old CD1 mice were injected i.c. with 2×104 pfu of each virus or MOCK-infected with PBS.
Data obtained from a separate virulence study were also used to compare the 68U201/IRES vaccines to TC-83 virulence. Six-day-old CD1 pups injected i.c. with 2.3×104 pfu of TC-83 began dying by day 3 post infection, with all pups succumbing to infection by day 7 (M. Guerbois, unpublished data). This time course is comparable to 68U201/IRESv2 infection in mice (Fig. 6), suggesting that 68U201/IRESv1 and v2 vaccines are similar if not less neurovirulent in young mice than the current TC-83 vaccine.
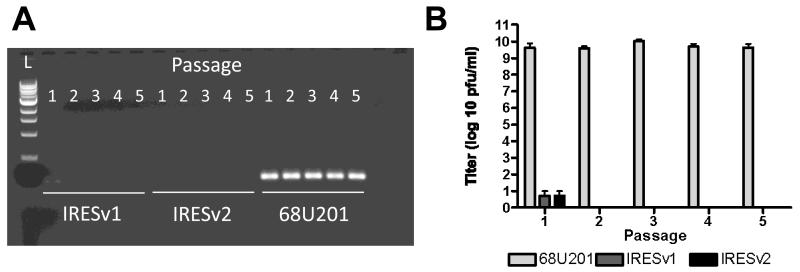
68U201/IRES virus infections in mosquito cells
An attractive feature of the EMVC IRES-based arbovirus vaccines is their inability to replicate in mosquito cells (Finkelstein et al., 1999; Woolaway et al., 2001). To confirm this phenotype for 68U201/IRES viruses, 68U201/IRESv1 and v2 were blindly passaged 5 times on C6/36 cells. 68U201 was used as a control. Infectious virus was observed in 68U201/IRES viruses-infected cultures only on the first passage, likely residual inoculum virus, which was also reflected in the low amount of viral RNA detected by reverse transcriptase polymerase chain reaction (RT-PCR, Fig. 7). At all 5 passages, 68U201 infectious virus and viral RNA were observed at high quantities (Figs. 7A and 7B). These results are consistent with blind passage of other IRES-containing alphavirus vaccines (Pandya et al., 2012; Plante et al., 2011; Volkova et al., 2008), reflecting the inability of IRES to drive translation of viral structural proteins in insect cells.
Fig.7. Infection of mosquito cells by vaccine strains.
Vaccine stains and controls were passaged 5 times on C6/36 cells with a starting MOI of 0.1 Vero pfu/cell. (A) 48 hpi, supernatants were analyzed by RT-PCR with primers amplifying in the nsP4 region of the genome to detect the presence of viral RNA. (B) Titers obtained from each passage are shown. Error bars show standard deviation from duplicate samples.
68U201/IRES viruses in mosquitoes
Although these 68U201/IRES viruses could not replicate within mosquito cells in culture, we also confirmed their inability to infect mosquitoes in vivo. Aedes taeniorhynchus, an epidemic vector for VEEV, were inoculated intrathoracically (i.t.), the most permissive route, with approximately 1×103 pfu/mosquito of 68U201, 68U201/IRESv1 or 68U201/IRESv2. Cytopathic studies performed on the clarified media from homogenized whole mosquitoes taken on day 10-post inoculation revealed infectious virus only in the 68U201-injected mosquitoes (24/24). No homogenates from mosquitoes infected with 68U201/IRESv1 or v2 showed signs of CPE (0/24).
Discussion
The IE VEEV subtype is genetically and geographically distinct from others. This subtype is endemic to Central America and Mexico, with recent outbreaks in 1993 and 1996 (Gonzalez-Salazar et al., 2003). Historically, IE subtypes were considered avirulent in horses, but recent findings revealed that viruses isolated during epizootics can cause equine encephalitis (Gonzalez-Salazar et al., 2003; Oberste et al., 1998), and human exposure in Mexico appears to be widespread (Adams et al., 2012). We sought to create a vaccine, for either human or equine use, for these IE-endemic regions that would be better matched for the viruses found in these areas, but not by the incorporation of attenuating point mutations. Instead, we used the EMCV IRES technology applied within the IE VEEV 68U201 genome to protect against lethal IE infection in mice. This approach has several important features. First, the backbone was based upon a IE strain to offer better long-term protection against VEEV strains endemic to Central America. Second, the method of attenuation was based upon the ablation of the subgenomic promoter’s function and the dependence of some or all of the viral structural proteins’ translation on the EMCV IRES. We hypothesized this attenuation based on restricting the amount of subgenomic transcript produced during infection, which in turn dramatically limits the quantity of structural proteins and virions. This method, independent of attenuating point mutations, provides phenotype stability during virus propagation. Also, if the IRES element is lost due to a deletion or recombination event, the resulting virus will not be viable because the structural proteins cannot be translated. Lastly, the IRES chosen has unique vertebrate-restrictive translational properties, thereby dramatically reducing the virus’ likelihood of mosquito transmission in nature.
The proof-of-concept studies on the IRES technology were first conducted with TC-83 (Volkova et al., 2008). Although TC-83 and 68U201 are both strains of VEEV, they reacted differently to the incorporation of the IRES sequence. Unlike the 68U201/IRESv1, TC-83/mutSGP/IRES had a 10-fold lower specific infectivity than the parental TC-83 viral RNA (Volkova et al., 2008). Twenty-four hours after electroporation, TC-83/mutSGP/IRES produced a mixture of large and small plaques, indicating phenotypic and potential genetic instability. When individual plaques were sequenced, point mutations in nsP2 were observed that when incorporated back into the genome, raised the specific infectivity of the TC-83/mutSGP/IRES/1 to TC-83 levels. 68U201/IRESv1 produced uniformly small plaques 24-48 hours after electroporation and had a specific infectivity similar to the wt 68U201 infectious clone, so the same selective pressure to create compensatory mutations was not present in the IRES-bearing strain 68U201.
Using the murine model, we demonstrated that the IRES-bearing 68U201 vaccine candidates are immunogenic and protective. Antibodies that neutralize the parental 68U201 virus were detected within 3 weeks of 68U201/IRESv1 vaccination, but not within all vaccinated mice. In comparison, all 68U201/IRESv2-vaccinated mice produced detectable neutralizing antibodies by week 3, suggesting that v2 may be more rapidly immunogenic. However, by week 11, both 68U201/IRESv1 and v2 produced neutralizing antibodies in all mice. A PRNT80 titer of 20, considered to be alphavirus-protective in vivo (Paessler and Weaver, 2009), was achieved by most of the 68U201/IRES-vaccinated mice at the time of challenge (1 month post infection), and antibody titers remained high a year post vaccination. However, even mice that lacked a detectable PRNT80 titer (e.g. most TC-83- and some 68U201/IRES-vaccinated mice) were still fully protected against lethal challenge, indicating that other components of the immune response such as T-cell function (Brooke et al., 2010; Paessler et al., 2007), are probably important.
In addition to being immunogenic, the 68U201/IRES vaccines also showed properties associated with increased safety, both virological and environmental, compared to TC-83. Both 68U201/IRESv1 and v2 were just as attenuated, if not more, than TC-83 when injected i.c. into infant mice. The survival curves for TC-83 and 68U201/IRESv2 showed no statistical difference, but 68U201/IRESv1 was attenuated compared to both as measured in mean days survival. Because only the highest achievable dose was used, it is possible that lower inoculated doses would reveal a difference in virulence between TC-83 and 68U201/IRESv2. Second, the levels of viremia in 68U201/IRES-vaccinated mice were reduced in titer and duration compared to both 68U201 and TC-83. No 68U201/IRES was detected in the serum after the first day following vaccination. This limits the timeframe for a potential transmission event from the vaccinee to a mosquito. Furthermore, this possibility of transmission of the IRES-based vaccines is remote because they are unable to infect mosquitoes. Even following i.t. inoculation, the most permissive route of infection, neither 68U201/IRESv1 nor v2 replicated within Ae. taeniorhynchus mosquitoes.
The encouraging results from our initial studies with these IRES-based 68U201 VEE vaccines indicate that further development is warranted. Although lower doses of our vaccine may be sufficient to protect horses from VEEV disease (Fine et al., 2007), increasing the titers generated by Vero cells of our vaccines would advantageous. Work is currently ongoing to increase these titers by serial passage in several cell lines approved for vaccine development. Additional studies are also needed to further test the efficacy of our IRES-based VEE vaccines, including protection against aerosol exposure in mice and nonhuman primates (NHP). VEEV is highly infectious by the aerosol route, which is a likely route of accidental laboratory exposure or intentional exposure during a terrorist attack. The latter is a particular concern as VEEV is highly weaponizable, prompting the U.S. government to classify it as a Select Agent. Both murine (Steele et al., 1998) and NHP (Reed et al., 2005) models for VEEV aerosol exposure have been established, allowing for the efficacy of the 68U201/IRES vaccines to be measured.
The IRES-based attenuation technology described here has also been successfully applied to other alphaviruses to create safe and efficacious vaccines (Pandya et al., 2012; Plante et al., 2011; Volkova et al., 2008). The technology is easily transferable between different alphaviruses because the mechanism of attenuation is a property of changes the alphavirus gene expression, and not of a particular virus strain. It therefore should be applicable to other known or as yet unidentified alphavirus that may emerge in the future.
Materials and methods
Cell lines and viruses
Vero (green monkey kidney) cells were maintained in Dulbecco’s minimum essential medium (DMEM) supplemented with 5-6% fetal bovine serum (FBS) and penicillin/streptomycin (P/S). BHK-21 (baby hamster kidney) cells were maintained in DMEM with 10% FBS and P/S. C6/36 (Aedes albopictus) mosquito cells were grown in BHK media supplemented with 1% tryptose broth phosphate (TBP). All mammalian cells were stored at 37°C while insect cells were grown at 29°C. All of the viruses in this study were rescued from cells transfected with in vitro transcribed RNA generated from infectious clone cDNA templates. In some cases, viruses were passed once in Vero cell culture to increase titer and create stocks for use.
Vaccine clone construction
The infectious cDNA clone derived from VEEV subtype IE strain 68U201 has been described previously (Powers et al., 2000), and served as the parental plasmid for all manipulations. 68U201/IRESv1 was created by mutagenizing the SGP with 14 mutations and by inserting the capsid gene-fused IRES (Fig. 1). Briefly, the SGP was mutated, the 5′ UTR of the subgenomic RNA was deleted and a unique ClaI site was added upstream of the EMCV IRES-capsid fusion using the following primers in 3 PCR reactions. The VEEV/mutSGP/IRES clone was used as a PCR template to amplify the EMCV IRES sequence (Volkova et al., 2008). Primers that annealed within nsP4 or capsid were used to obtain PCR and final fusion PCR products. The fusion PCR product was ligated into the 68U201 genome between the NheI and BspHI sites.
The 68U201/IRESv2 infectious cDNA clone was constructed similarly. The capsid gene was deleted from the 68U201 infectious cDNA by PCR mutagenesis such that the E3 gene contained the ATG start codon and began directly after the SGP. Capsid, with flanking start and stop codons, was fused to the IRES sequence and inserted within the 3′UTR (Fig. 1).
All final constructions were sequenced and found to have no unexpected changes through the PCR-amplified regions. A list of all primers used in generating these constructs is available upon request.
Vaccine rescue and titration
RNA was in vitro transcribed from linearized cDNA using the T7 Ambion mMessage mMachine kit (Austin, Texas), then electroporated into BHK or Vero cells. In some cases, the cDNA template was destroyed by DNase treatment and the RNA was precipitated by LiCl and ethanol as per the manufacter’s protocol. The final RNA concentration was determined by UV spectrophotometry. Electroporation conditions were as follows using the BTX electropororator (Harvard apparatus company, Holliston, MA): BHK (2 mm cuvette, 680V, 10 pulses at 99 μs, 100ms interval with unipolar polarity) and Vero (4 mm cuvette, 350V, 1 pulse at 7 ms, 100ms interval with unipolar polarity). Virus was harvested from clarified (287 × G for 5 minutes) supernatants collected 24 and 48 hours after electroporation.
All viruses were titrated on Vero cell monolayers. Briefly, serial dilutions of virus were allowed to adsorb to the monolayers for 1 hour prior to overlaying with DMEM supplemented with 2% FBS and 0.4% agarose. Approximately 2 days after infection, monolayers were fixed with formaldehyde and subsequently stained with 0.5% crystal violet to visualize plaques. All titers are expressed as pfu/ml. Specific infectivity was determined by titrating an aliquot of freshly electroporated cells onto Vero cell monolayers, then overlaying the plates as done for titration. Specific infectivity was measured by counting the number of plaques produced by electroporated cells divided by the amount of RNA used for the electroporation.
Replication curves
Vero cells seeded into 6-well plates were infected in triplicate with virus at a MOI of 0.1 pfu/cell for 1 hour at 37°C, then washed 4 times with media prior to adding 2.1 ml of DMEM containing 2% FBS and P/S. Immediately thereafter, 100 μl of culture fluid was removed for the 1 hour post infection (hpi) titration. At each timepoint (12, 24, 36, 48 hpi), 100 μl of cell culture supernatant were removed and replaced with fresh media. Supernatants were titrated in 12-well plates as described above.
Animal infections
All animal work was performed in accordance with UTMB policy as approved by the UTMB Institutional Animal Care and Use Committee. Adult female CD1 mice (Charles River, Wilmington, MA), aged approximately 6-8 weeks, were injected s.c. in the right hind leg or back with 100 μl of virus diluted in DMEM with 2% FBS, or with PBS. All inocula were titrated to confirm dose. Vaccinated and challenged mice were observed daily for signs of illness (including ruffled fur, hunched posture and hind limb paralysis) for 7-10 days. Individual weight measurements were also recorded. During the vaccination phase of the experiment, mice were considered moribund if they exhibited paralysis, extreme lethargy or greater than a 20% loss in initial body weight. However, moribund criteria during the challenge experiments did not include the weight loss. Moribund mice that were euthanized were recorded as dead on the following day.
Mice were bled retro-orbitally and clarified serum was tested for the presence of virus by plaque assay, or for neutralizing antibody by plaque reduction neutralization test (PRNT, see below). One capillary tube (volume ~ 70 μl) of blood was combined with 225 μl of PBS prior to clarification by centrifugation for 5 minutes at 3380 × G. PBS-diluted serum was removed and stored at −80°C. Blood samples within cohorts were taken on days 1 and 2 to determine levels of viremia. Mice held for long-term antibody studies were bled on weeks 3, 6, 11 and 52 post vaccination.
Intracranial inoculations were performed on 6-day-old offspring from individual litters of pregnant CD1 mice. Approximately 20 μl of virus inoculum was injected i.c. into each mouse, and pups were monitored daily for survival.
Plaque reduction neutralization test
Sera obtained from mice 3, 6, 11 and 52 weeks post-vaccination were tested for the presence of neutralizing antibody by PRNT. Individual sera were heat inactivated at 56°C for 1 hour, then chilled prior to use. Two-fold dilutions were incubated with 70 μl (approximately 800 pfu/ml) of 68U201 or TC-83 for 1 hour at 37°C, after which Vero cell monolayers were infected with the serum/virus mixture as described for virus titration. Plaques were counted at each dilution to determine the PRNT80 titers for the corresponding serum, ie the serum dilution at which there was at least a 80% reduction in the number of plaques observed with the uninfected mouse serum. Approximately 20-30 plaques were observed in monolayers incubated with uninfected murine serum.
Serial passages
Serial passages in C6/36 cells were performed in duplicate in 6-well plates without intermediate titration. The first passage was infected at an MOI of 0.1 pfu/cell (based upon Vero titers) for one hour, cells were then washed 4 times with 1 ml PBS and finally covered with 2 ml of C6/36 media and maintained at 29°C. Supernatants were harvested 48 hrs post infection, centrifuged 5 min at 1791 × G and 3 aliquots of 450 μl were placed at −80°C. Subsequent passages were performed by infecting C6/36 cells with 400 μl of the previous passage.
One aliquot from each passage was used to perform a plaque titration on Vero cells and to isolate viral RNA. Viral RNA extraction was performed on 100 μl of supernatant using the QIAamp Viral RNA Mini Kit (QIAGEN, Valencia, CA), as per manufacturer’s instructions, with a final elution volume of 50 μl. Reverse-transcription polymerase chain reaction (RT-PCR) was performed on 2.5 μl of isolated vRNA using QIAGEN OneStep kit (per manufacturer’s protocol) with primers annealing within nsP4.
Mosquito infections
Aedes (Ochlerotatus) taeniorhynchus derived from a colony founded from adult females collected near Talahassee, Florida were i.t.-inoculated with 1 μl of undiluted 68U201/IRESv1 or 68U201/IRESv2 stocks, as well as a titer-matched dilution of 68U201 (1 × 106 PFU/ml). Fifty female mosquitoes were injected per virus, plus one cohort was injected with PBS as control. After injection, mosquitoes were incubated for 10 days at 27°C, then placed individually into 2 ml tubes containing 350 μl DMEM supplemented with 10% FBS, 1% P/S and Fungizone (amphotericin B) at a final concentration of 5 μg/ml. Whole mosquitoes were homogenized in Qiagen Tissue Lyser II for 4 min at 26p/sec, then supernatants were clarified by centrifugation for 5 min at 1791 × G. Vero cells were infected with 100 μl of clarified supernatant, incubated for 1 hour at 37°C, then covered with 1 ml DMEM 2% FBS, and kept for 5 days with monitoring for signs of cytopathic effects (CPE).
Statistical analyses and graph presentation
Prism software (Version 4, GraphPad Software, La Jolla, CA) was used for both the statistical analyses as well as the graphical generation of data. Significances in weight were performed using a two-way ANOVA with a Bonferroni Post-Test. PRNT80 and viremia statistics were performed using a one-way ANOVA with a Tukey’s Multiple Comparisons Post-Test. Statistics on survival curves were analyzed using the Logrank Test.
Highlights.
VEEV genomes containing an EMCV IRES (VEEV/IRES) are attenuated in vitro
Mice tolerate VEEV/IRES vaccines well with no signs of illness
VEEV/IRES- vaccinated mice are protected against lethal wt VEEV infection
VEEV/IRES vaccines are unable to replicate in mosquitoes or mosquito cells
ACKNOWLEDGEMENTS
We thank R Seymour, R Yun, G Leal, and E Wang for their help with animal work and J Peterson for providing mosquitoes. We thank NA Bergren for his technical assistance and manuscript editing. We also thank J Huang for her assistance in rearing and preparing mosquitoes. SLR was funded through T32 grant AI007536-11 and AI007536-12. KSP was supported by the Sealy Center for Vaccine Development and T32 AI7526-11. This research was supported by a grant from the National Institute of Allergy and Infectious Disease (NIAID) through the Western Regional Center of Excellence for Biodefense and Emerging Infectious Disease Research, National Institutes of Health (NIH) grant U54 AIO57156.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams AP, Navarro-Lopez R, Ramirez-Aguilar FJ, Lopez-Gonzalez I, Leal G, Flores-Mayorga JM, Rosa A.P.A.T.d., Saxton-Shaw KD, Singh AJ, Borland EM, Powers AM, Tesh RB, Weaver SC, Estrada-Franco JG. Venezuelan Equine Encephalitis Virus Activity in the Gulf Coast Region of Mexico, 2003-2010. PLoS Negl Trop Dis. 2012;6:e1875. doi: 10.1371/journal.pntd.0001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault AC, Powers AM, Holmes EC, Woelk CH, Weaver SC. Positively charged amino acid substitutions in the e2 envelope glycoprotein are associated with the emergence of venezuelan equine encephalitis virus. J Virol. 2002;76:1718–1730. doi: 10.1128/JVI.76.4.1718-1730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke CB, Deming DJ, Whitmore AC, White LJ, Johnston RE. T cells facilitate recovery from Venezuelan equine encephalitis virus-induced encephalomyelitis in the absence of antibody. J Virol. 2010;84:4556–4568. doi: 10.1128/JVI.02545-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke DS, Ramsburg HH, Edelman R. Persistence in Humans of Antibody to Subtypes of Venezuelan Equine Encephalomyelitis (Vee) Virus after Immunization with Attenuated (Tc-83) Vee Virus-Vaccine. J Infect Dis. 1977;136:354–359. doi: 10.1093/infdis/136.3.354. [DOI] [PubMed] [Google Scholar]
- Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, Johnston RE. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995;212:102–110. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- Estrada-Franco JG, Navarro-Lopez R, Freier JE, Cordova D, Clements T, Moncayo A, Kang W, Gomez-Hernandez C, Rodriguez-Dominguez G, Ludwig GV, Weaver SC. Venezuelan equine encephalitis virus, southern Mexico. Emerg Infect Dis. 2004;10:2113–2121. doi: 10.3201/eid1012.040393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillis CA, Calisher CH. Neutralizing Antibody-Responses of Humans and Mice to Vaccination with Venezuelan Encephalitis (Tc-83) Virus. J Clin Microbiol. 1979;10:544–549. doi: 10.1128/jcm.10.4.544-549.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine DL, Roberts BA, Teehee ML, Terpening SJ, Kelly CL, Raetz JL, Baker DC, Powers AM, Bowen RA. Venezuelan equine encephalitis virus vaccine candidate (V3526) safety, immunogenicity and efficacy in horses. Vaccine. 2007;25:1868–1876. doi: 10.1016/j.vaccine.2006.10.030. [DOI] [PubMed] [Google Scholar]
- Finkelstein Y, Faktor O, Elroy-Stein O, Levi BZ. The use of bi-cistronic transfer vectors for the baculovirus expression system. J Biotechnol. 1999;75:33–44. doi: 10.1016/s0168-1656(99)00131-5. [DOI] [PubMed] [Google Scholar]
- Frolov I, Hoffman TA, Pragai BM, Dryga SA, Huang HV, Schlesinger S, Rice CM. Alphavirus-based expression vectors: strategies and applications. Proc Natl Acad Sci U S A. 1996;93:11371–11377. doi: 10.1073/pnas.93.21.11371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garman JL, Scherer WF, Dickerman RW. A study of equine virulence of naturally occurring Venezuelan encephalitis virus in Veracruz with description of antibody responses. Bol Oficina Sanit Panam. 1968;65:238–252. [PubMed] [Google Scholar]
- Gonzalez-Salazar D, Estrada-Franco JG, Carrara AS, Aronson JF, Weaver SC. Equine amplification and virulence of subtype IE Venezuelan equine encephalitis viruses isolated during the 1993 and 1996 Mexican epizootics. Emerg Infect Dis. 2003;9:161–168. doi: 10.3201/eid0902.020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene IP, Paessler S, Austgen L, Anishchenko M, Brault AC, Bowen RA, Weaver SC. Envelope glycoprotein mutations mediate equine amplification and virulence of epizootic Venezuelan equine encephalitis virus. Journal of Virology. 2005;79:9128–9133. doi: 10.1128/JVI.79.14.9128-9133.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart MK, Caswell-Stephan K, Bakken R, Tammariello R, Pratt W, Davis N, Johnston RE, Smith J, Steele K. Improved mucosal protection against Venezuelan equine encephalitis virus is induced by the molecularly defined, live-attenuated V3526 vaccine candidate. Vaccine. 2000;18:3067–3075. doi: 10.1016/s0264-410x(00)00042-6. [DOI] [PubMed] [Google Scholar]
- Kenney JL, Adams AP, Gorchakov R, Leal G, Weaver SC. Genetic and Anatomic Determinants of Enzootic Venezuelan Equine Encephalitis Virus Infection of Culex (Melanoconion) taeniopus. PLoS Negl Trop Dis. 2012;6:e1606. doi: 10.1371/journal.pntd.0001606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney JL, Volk SM, Pandya J, Wang E, Liang X, Weaver SC. Stability of RNA virus attenuation approaches. Vaccine. 2011;29:2230–2234. doi: 10.1016/j.vaccine.2011.01.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney RM, Chang GJ, Tsuchiya KR, Sneider JM, Roehrig JT, Woodward TM, Trent DW. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J Virol. 1993;67:1269–1277. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney RM, Johnson BJB, Welch JB, Tsuchiya KR, Trent DW. The Full-Length Nucleotide-Sequences of the Virulent Trinidad Donkey Strain of Venezuelan Equine Encephalitis-Virus and Its Attenuated Vaccine Derivative, Strain Tc-83. Virology. 1989;170:19–30. doi: 10.1016/0042-6822(89)90347-4. [DOI] [PubMed] [Google Scholar]
- Ludwig GV, Turell MJ, Vogel P, Kondig JP, Kell WK, Smith JF, Pratt WD. Comparative neurovirulence of attenuated and non-attenuated strains of Venezuelan equine encephalitis virus in mice. Am J Trop Med Hyg. 2001;64:49–55. doi: 10.4269/ajtmh.2001.64.49. [DOI] [PubMed] [Google Scholar]
- Oberste MS, Fraire M, Navarro R, Zepeda C, Zarate ML, Ludwig GV, Kondig JF, Weaver SC, Smith JF, Rico-Hesse R. Association of Venezuelan equine encephalitis virus subtype IE with two equine epizootics in Mexico. Am J Trop Med Hyg. 1998;59:100–107. doi: 10.4269/ajtmh.1998.59.100. [DOI] [PubMed] [Google Scholar]
- Oberste MS, Schmura SM, Weaver SC, Smith JF. Geographic distribution of Venezuelan equine encephalitis virus subtype IE genotypes in Central America and Mexico. Am J Trop Med Hyg. 1999;60:630–634. doi: 10.4269/ajtmh.1999.60.630. [DOI] [PubMed] [Google Scholar]
- Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, Weaver SC, Frolov I. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J Virol. 2006;80:2784–2796. doi: 10.1128/JVI.80.6.2784-2796.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paessler S, Weaver SC. Vaccines for Venezuelan equine encephalitis. Vaccine. 2009;27(Suppl 4):D80–85. doi: 10.1016/j.vaccine.2009.07.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paessler S, Yun NE, Judy BM, Dziuba N, Zacks MA, Grund AH, Frolov I, Campbell GA, Weaver SC, Estes DM. Alpha-beta T cells provide protection against lethal encephalitis in the murine model of VEEV infection. Virology. 2007;367:307–323. doi: 10.1016/j.virol.2007.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya J, Gorchakov R, Wang E, Leal G, Weaver SC. A vaccine candidate for eastern equine encephalitis virus based on IRES-mediated attenuation. Vaccine. 2012;30:1276–1282. doi: 10.1016/j.vaccine.2011.12.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen CE, Robinson DM, Cole FE. Isolation of Vaccine Strain of Venezuelan Equine Encephalomyelitis Virus from Mosquitos in Louisiana. Am J Epidemiol. 1972;95:490. doi: 10.1093/oxfordjournals.aje.a121416. [DOI] [PubMed] [Google Scholar]
- Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996;14:337–343. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- Plante K, Wang E, Partidos CD, Weger J, Gorchakov R, Tsetsarkin K, Borland EM, Powers AM, Seymour R, Stinchcomb DT, Osorio JE, Frolov I, Weaver SC. Novel Chikungunya Vaccine Candidate with an IRES-Based Attenuation and Host Range Alteration Mechanism. PLoS Pathog. 2011;7:e1002142. doi: 10.1371/journal.ppat.1002142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers AM, Brault AC, Kinney RM, Weaver SC. The use of chimeric Venezuelan equine encephalitis viruses as an approach for the molecular identification of natural virulence determinants. J Virol. 2000;74:4258–4263. doi: 10.1128/jvi.74.9.4258-4263.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt WD, Davis NL, Johnston RE, Smith JF. Genetically engineered, live attenuated vaccines for Venezuelan equine encephalitis: testing in animal models. Vaccine. 2003;21:3854–3862. doi: 10.1016/s0264-410x(03)00328-1. [DOI] [PubMed] [Google Scholar]
- Reed DS, Lind CM, Lackemeyer MG, Sullivan LJ, Pratt WD, Parker MD. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine. 2005;23:3139–3147. doi: 10.1016/j.vaccine.2004.12.023. [DOI] [PubMed] [Google Scholar]
- Steele KE, Davis KJ, Stephan K, Kell W, Vogel P, Hart MK. Comparative neurovirulence and tissue tropism of wild-type and attenuated strains of Venezuelan equine encephalitis virus administered by aerosol in C3H/HeN and BALB/c mice. Vet Pathol. 1998;35:386–397. doi: 10.1177/030098589803500508. [DOI] [PubMed] [Google Scholar]
- Turell MJ, Ludwig GV, Kondig J, Smith JF. Limited potential for mosquito transmission of genetically engineered, live-attenuated Venezuelan equine encephalitis virus vaccine candidates. Am J Trop Med Hyg. 1999;60:1041–1044. doi: 10.4269/ajtmh.1999.60.1041. [DOI] [PubMed] [Google Scholar]
- Volkova E, Frolova E, Darwin JR, Forrester NL, Weaver SC, Frolov I. IRES-dependent replication of Venezuelan equine encephalitis virus makes it highly attenuated and incapable of replicating in mosquito cells. Virology. 2008;377:160–169. doi: 10.1016/j.virol.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton TE, Alvarez O, Jr., Buckwalter RM, Johnson KM. Experimental infection of horses with enzootic and epizootic strains of Venezuelan equine encephalomyelitis virus. J Infect Dis. 1973;128:271–282. doi: 10.1093/infdis/128.3.271. [DOI] [PubMed] [Google Scholar]
- Woolaway KE, Lazaridis K, Belsham GJ, Carter MJ, Roberts LO. The 5 ′ untranslated region of Rhopalosiphum padi virus contains an internal ribosome entry site which functions efficiently in mammalian, plant, and insect translation systems. Journal of Virology. 2001;75:10244–10249. doi: 10.1128/JVI.75.21.10244-10249.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]