Abstract
Human epidermal growth factor receptor 2 (HER2 or ErbB2), a member of ErbB receptor tyrosine kinases, is overexpressed in approximately 20 % of human breast cancer, and the ErbB2 signaling pathway is a critical therapeutic target for ErbB2-overexpressing breast cancer. We investigated the inhibitory effects of the Gemini vitamin D analog BXL0124, the synthetic triterpenoid CDDO-Im and the combination on the tumorigenesis of ErbB2-overexpressing breast cancer. MMTV-ErbB2/neu transgenic mice were treated with BXL0124, CDDO-Im or the combination from 3 months of age until the end of the experiment. Formation and growth of MMTV-ErbB2/neu mammary tumors were monitored every week, and all three treatments delayed the development of mammary tumors without significant toxicity. Decreased activation of ErbB2 as well as other ErbB receptors, ErbB1 and ErbB3, in MMTV-ErbB2/neu mammary tumors was shown by all treatments. Protein levels of downstream targets of the ErbB2 signaling pathway, including activated-Erk1/2, activated-Akt, c-Myc, CycD1 and Bcl2, were repressed by all three treatments, with the combination treatment exhibiting the strongest effects. To investigate therapeutic efficacy, the combination of BXL0124 and CDDO-Im was given to MMTV-ErbB2/neu mice after mammary tumors were established between 23-30 weeks of age. Short-term treatment with the combination did not show effects on tumor growth nor the ErbB2 signaling pathway. The present study demonstrates BXL0124, CDDO-Im and the combination as potential agents for prevention, but not treatment, against the tumorigenesis of ErbB2-overexpressing breast cancer.
Keywords: Gemini Vitamin D analog, synthetic triterpenoid, ErbB2-positive breast cancer
Introduction
Human epidermal growth factor receptor 2 (HER2, also known as ErbB2) is a member of the ErbB family of transmembrane receptor tyrosine kinases, including epidermal growth factor receptor (EGFR, also known as ErbB1 or HER1), ErbB3 (HER3) and ErbB4 (HER4) (1). ErbB2, which presents in an activated conformation without known ligands, functions as a signal amplifier of other ErbB family receptors by forming heterodimers and regulates cell proliferation, survival and apoptosis (2). In breast cancer, the amplification of ErbB2 is one of the major genomic abnormalities and has been reported in approximately 20% of invasive breast cancer cases (3). The ErbB2-targeted therapies, such as trastuzumab and lapatinib, have substantially improved clinical outcomes of breast cancer patients with ErbB2-overexpressing tumors (1). The overexpression of ErbB2 has also been reported in premalignant lesions of the breast (4). Moreover, recent studies implicated ErbB2 in the early development of breast cancer (5, 6), suggesting ErbB2 is a molecular target for prevention as well as treatment of ErbB2-positive breast cancer.
1α,25(OH)2D3, a hormonally active form of vitamin D, modulates proliferation, survival and differentiation of various types of cells, in addition to its role as a regulator of calcium and phosphorus homeostasis (7, 8). 1α,25(OH)2D3 has been shown to inhibit the growth of various types of breast cancer cells, including the ErbB2-positive subtype (9). Moreover, knockout of the vitamin D receptor (VDR) facilitated the development of mammary tumors in MMTV-ErbB2/neu mice, indicating the inhibitory role of 1α,25(OH)2D3 on ErbB2-overexpressing mammary tumorigenesis (10). Previously, we reported that novel Gemini vitamin D analogs, which were synthesized to increase anti-cancer efficacy and to decrease hypercalcemic toxicity of 1α,25(OH)2D3, repressed the tumor growth of both estrogen receptor (ER)-positive and ER-negative subtypes of breast cancer in vivo (11). In addition, the Gemini vitamin D analog BXL0124 inhibited the growth of ErbB2-overexpressing mammary tumors in MMTV-ErbB2/neu transgenic mice, which spontaneously develop mammary tumors driven by ErbB2 overexpression (12).
Oleanane, also known as oleanolic acid, is a diverse natural triterpenoid that shows weak anti-cancer and anti-inflammatory activities in vivo (13). Numerous synthetic oleananes (SOs) were produced to improve the activities of natural oleanane. One of the most potent SOs, 2-cyano-3,12-dioxooleana-1,9(11)-dien-28-oic acid (CDDO) was further modified to produce derivatives, including CDDO-Me (methyl ester), CDDO-Im (imidazolide), CDDO-MA (methyl amide) and CDDO-EA (ethyl amide) (14). CDDO inhibited proliferation and induced apoptosis of ErbB2-overexpressing breast cancer cells (15, 16). Kinase activity and phosphorylation of ErbB2 were repressed by CDDO in the ErbB2-overexpressing breast cancer cells (15). In animal studies, CDDO-Me markedly delayed mammary tumor development in ER-negative ErbB2-overexpressing and BRCA1-deficent mouse models (17, 18). Although CDDO-Im also showed potent anti-cancer activity against ER-negative breast cancer cells (19), its activity on ErbB2-overexpressing breast cancer has not been investigated.
Homo- or hetero-dimerization of ErbB2 with other ErbB family receptors allows ErbB2 to activate wide ranges of downstream signaling pathways, including JAK2, STAT3, MAPK and PI3K/Akt (3). The complexity of the ErbB2 signaling pathway emphasizes the importance of using multiple therapies that target different components of the ErbB2 signaling pathway (3). In studies with MMTV-ErbB2/neu mice, the Gemini vitamin D analog BXL0124 was shown to target the ErbB2/Akt/Erk signaling pathway (12), while derivatives of CDDO were reported to inhibit activation of STAT3 (17). Moreover, CDDO was shown to directly interact with ErbB2 (18), which might contribute to the regulation of ErbB2 by CDDO. Previous studies with leukemia cells demonstrated that combined treatments of 1α,25(OH)2D3 or its analog with CDDO-Im had synergistic effects on the induction of monocytic differentiation (20, 21). In the present study, we investigated the inhibitory effects of the Gemini vitamin D analog BXL0124, the synthetic triterpenoid derivative CDDO-Im and the combination on both prevention and treatment of mammary tumorigenesis of MMTV-ErbB2/neu transgenic mice.
Materials and methods
Reagents
Gemini vitamin D analog BXL0124 (1α,25-dihydroxy-20R-21(3-hydroxy-3-deuteromethyl-4,4,4-trideuterobutyl)-23-yne-26,27-hexafluro-cholecalciferol, (22)) was provided by BioXell, Inc. (Nutley, NJ) and dissolved in dimethyl sulfoxide (DMSO, Sigma-Aldrich, St. Louis, MO). 1-[2-Cyano-3,12-dioxooleana-1,9(11)-dien-28-oyl]imidazole (CDDO-Im, (23, 24)) was provided by Dr. Michael B. Sporn at Dartmouth Medical School (Hanover, NH) and dissolved in DMSO. Dilutions of BXL0124 and CDDO-Im in sesame oil (Sigma-Aldrich) were used for oral administration in vivo.
Animals and experimental procedures
Female MMTV-ErbB2/neu transgenic mice (6-7 weeks old) were purchased from the Jackson Laboratory (Bar Harbor, ME). MMTV-ErbB2/neu mice were given 0.3 μg/kg body weight of BXL0124 for 56 weeks, which is the dose and duration of treatment used previously to show anti-tumor activity without toxicity (12). Short-term or single treatment of CDDO-Im as high as 100 μg/kg body weight has been shown to be well-tolerated in mice (20, 25). For long-term treatment in the present study, MMTV-ErbB2/neu mice were administrated 3 μmole/kg body weight of CDDO-Im (≈ 1.6 μg/kg body weight). The dose selection was based on previously reported studies (20, 25). In the prevention study protocol, 15 week old mice received by oral administration the vehicle control (DMSO: sesame oil = 3: 97 [v:v] in 0.1 ml volume, n=19), BXL0124 (0.3 μg/kg body weight, n=19), CDDO-Im (3 μmole/kg body weight, n=20) or the combination of BXL0124 (0.3 μg/kg body weight) and CDDO-Im (3 μmole/kg body weight) (n=19) three times a week. The body weight and tumor size of each animal were measured weekly. The mice with large (tumor sizes ranging from 0.85-1.18 cm3) tumors were sacrificed earlier. All remaining mice were sacrificed when they were 56 weeks old.
In the treatment study protocol, mice were kept without treatment until they developed mammary tumors between 23-30 weeks of age. Following the development of mammary tumors, the sizes of tumors were measured, and mice were paired and separated into control or treatment groups with similar average tumor sizes with a final animal number of 11 or 13, respectively. Then, the mice were treated orally with the vehicle control or combination of BXL0124 (0.3 μg/kg body weight) and CDDO-Im (3 μmole/kg body weight) six times a week for three weeks.
The tumor size of each animal was also measured three times a week. Tumors were harvested and weighed at necropsy. The tumors were fixed in 10% formalin and transferred to 70% ethanol for immunofluorescent staining or flash frozen and stored in −80°C for Western blot analysis or RNA analysis. All animal studies were conducted in accordance with the protocol approved by the Institutional Animal Care and Use Committee at Rutgers, the State University of New Jersey (Protocol Number: 04-001).
Determination of serum calcium level
The detailed procedure of the determination of calcium concentration in serum samples (POINTE Scientific, INC., Canton, MI) was described previously (11).
Fluorescence microscopy
The tumors were embedded in paraffin (Electron Microscopy Sciences, Hatfield, PA) and then sectioned at 4 μm. The tumor samples were incubated in PBS containing 10% donkey serum to block non-specific binding and then incubated overnight at 4°C with a combination of primary antibodies against pErbB2 (1:100, Cell Signaling Technology, Danvers, MA) and ErbB2 (1:40, Cell Signaling Technology), diluted in SignalStain antibody diluent (Cell Signaling Technology, Beverly, MA). Subsequently, the tumor samples were incubated with fluorophore-conjugated secondary antibodies (Alexa Fluor 488 or 546; 1:200, Life Technologies, Carlsbad, CA) and TO-PRO-3 iodide nuclear antibody (1 μM, Life Technologies) at room temperature for 60 and 15 minutes, respectively. The images were taken using confocal microscope (Eclipse Ti, Nikon Instrument Inc., Melville, NY) with laser at 488 nm (pErbB2), 546 nm (ErbB2), and 633 nm (TO-PRO-3).
Western blot analysis
The detailed procedure was described previously (26). The primary antibodies recognizing ErbB1, pErbB1, pErbB2, pErbB3, Erk1/2, pErk1/2, Akt, pAkt, JAK2, pJAK2, pSrc (Tyr416), pSrc (Tyr527), STAT3, pSTAT3, c-Myc and RXRα were from Cell Signaling Technology (Beverly, MA); ErbB3, p21, CycD1, Bcl2 and PPARγ were from Santa Cruz Biotechnology (Santa Cruz, CA); ErbB2 and VDR were from Thermo Scientific Pierce (Waltham, MA); PCNA was from EMD Millipore (Billerica, MA), β-actin was from Sigma-Aldrich. Secondary antibodies were from Santa Cruz Biotechnology. Densitometric quantification of Western blot data was performed using Image J program (NIH, Bethesda, MD), and each protein level was normalized to the protein level of corresponding β-actin.
Quantitative real-time polymerase chain reaction
The procedure was described previously (27); the labeled primers for all genes in the experiments were obtained from Life Technologies.
Statistical analysis
Log-rank Test was used to test the difference in tumor-free distributions, and survival distributions between treatment groups. Chi-squared test was used to evaluate the differences in proportions of mice sacrificed at the end of experiment (Week 56) instead of during the experiment. The statistical analyses of tumor weights, body weights and serum calcium levels were performed using one-way analysis of variance (ANOVA) with Dunnett's adjustment. Data with two samples was analyzed with the student's t-test. All the statistical calculations were performed using SAS (Version 9.2, Cary, NC) and Graph Pad Prism 4.0 (GraphPad Software Inc.). The data are presented as the mean ± S.E. P values <0.05 were considered significant.
Results
Oral administration of the Gemini vitamin D analog BXL0124, the synthetic triterpenoid CDDO-Im and the combination inhibited mammary tumorigenesis in MMTV-ErbB2/neu transgenic mice
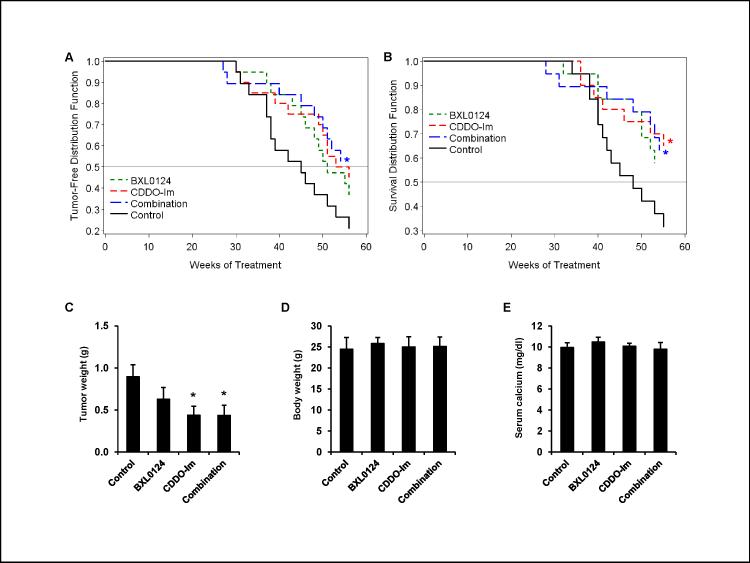
The effects of BXL0124, CDDO-Im and the combination on the development of ErbB2-overexpressing mammary tumors were investigated by utilizing the MMTV-ErbB2/neu transgenic mouse model. MMTV-ErbB2/neu mice were treated with vehicle control, BXL0124, CDDO-Im or the combination, beginning at 15 weeks of age. The development of mammary tumors was delayed by the treatments with BXL0124, CDDO-Im and the combination (Fig. 1A). The differences in tumor-free distributions were significant (p=0.0294) between the combination and the control groups, borderline significant (p=0.0731) between the CDDO-Im and the control group, and not significant (p=0.1542) between the BXL0124 and the control group (Fig. 1A). The percent of tumor-free mice at the end of the experiment at week 56 was significantly higher with the combination group (52.6, p=0.0436), but not with BXL0124 (36.8, p=0.2832) and CDDO-Im (45.0, p=0.1128) groups, compared to the control group (21.1) (Fig. 1A). The survival distribution of mice sacrificed before the end of the experiment due to large tumors was significantly different between the CDDO-Im group and the control group (p=0.0437) and the combination and the control groups (p=0.0449), while the difference of survival distributions between the BXL0124 and the control group (p=0.0789) was borderline significant (Fig. 1B). The estimated median time until mice were sacrificed because of large tumors (>0.85 cm3) was 48 weeks for the control group, while the median times for all other groups were over 56 week (Fig. 1B). While BXL0124 (0.63 ± 0.14 g), CDDO-Im (0.44 ± 0.11 g) and the combination (0.43 ± 0.12 g) showed reduced average tumor burden as compared to controls (0.89 ± 0.14 g) at necropsy, only the reductions of tumor burden by CDDO-Im and the combination were statistically significant (p<0.05) (Fig. 1C). Average body weight and serum calcium level were not affected by BXL0124, CDDO-Im and the combination, indicating all the drug treatments were not toxic to animals at the given concentration for the given duration (Fig. 1D and 1E).
Figure 1. Inhibitory effects of BXL0124, CDDO-Im and the combination on the mammary tumorigenesis in MMTV-ErbB2/neu transgenic mice.
MMTV-ErbB2/neu transgenic mice were treated orally with vehicle control (DMSO, n=19), BXL0124 (0.3 μg/kg body weight, n=19), CDDO-Im (3 μmole/kg body weight, n=20) or the combination of BXL0124 and CDDO-Im (n=19) 3 times a week, beginning at 3 months of age. (A) The distribution function of tumor-free animals in each group was shown. Statistical significance was evaluated by using the Chi-squared test (*p<0.05). (B) The distribution of survival of animals in each group was shown. Statistical significance was evaluated by using the Chi-squared test (*p<0.05). Average tumor weight (C), body weight (D), and serum calcium level (E) were shown. Data is presented as mean ± S.E. Statistical significance was determined by using ANOVA followed by Dunnett's adjustment (* p<0.05).
BXL0124, CDDO-Im and the combination repressed the activation of ErbB2 which was prominent at the leading edge of mammary tumors in MMTV-ErbB2/neu mice
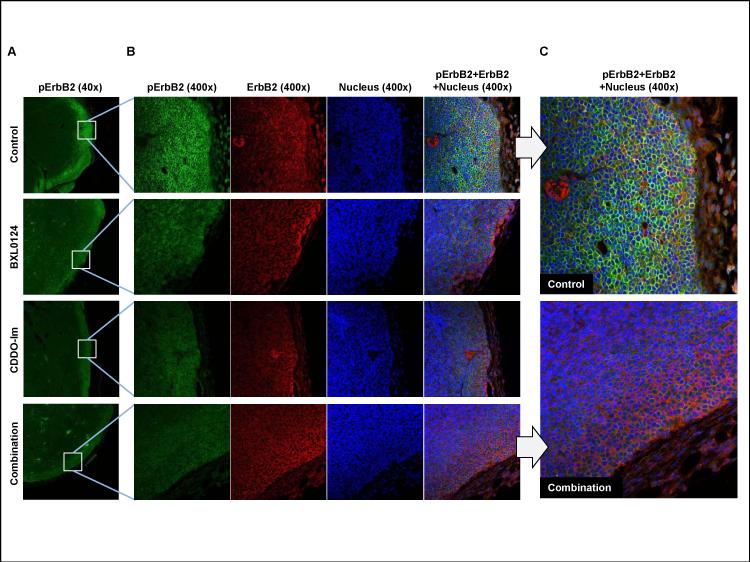
Since activation of ErbB2 is one of the key factors that drive tumorigenesis of ErbB2-overexpressing breast cancer, the effects of BXL0124, CDDO-Im and the combination on the activation of ErbB2 (determined by the phosphorylated form of ErbB2) were investigated in MMTV-ErbB2/neu mammary tumors. As shown in the pictures at 40x magnification, the activation of ErbB2 (pErbB2, shown as green) was prominent at the leading edge of MMTV-ErbB2/neu mammary tumor where the tumor interacted with surrounding stromal tissues (Fig. 2A). The edge areas of tumors were magnified (400x), and the pictures of pErbB2 (green), total ErbB2 (red), nuclei (blue) and merged images of the three were shown (Fig. 2B). BXL0124, CDDO-Im and the combination markedly decreased protein levels of activated ErbB2 (pErbB2), while the protein level of total ErbB2 was not affected by the treatments (Fig. 2B). The merged images of pErbB2, ErbB2 and nuclei for the control and combination treatment groups were enlarged for better presentation (Fig. 2C).
Figure 2. Activation of ErbB2 at the leading edge area of MMTV-ErbB2/neu mammary tumors and its repression by BXL0124, CDDO-Im and the combination.
Four MMTV-ErbB2/neu mammary tumors from each group were randomly selected and analyzed by immunofluorescent microscopy. (A) A representative immunofluorescent staining of pErbB2 (green) for each group of MMTV-ErbB2/neu mammary tumors was shown (40x magnification). (B) Representative immunofluorescent staining of pErbB2 (green), total ErbB2 (red), nuclei (blue) and the merged image of all three stains on the edge area of MMTV-ErbB2/neu mammary tumors were shown (400x magnification). (C) The pictures of the control and combination groups with merged images of the three stains for pErbB2, ErbB2 and nuclei, were enlarged for better presentation.
The activation of the ErbB family receptors, ErbB2, ErbB1 and ErbB3, in MMTV-ErbB2/neu mammary tumors was inhibited by BXL0124, CDDO-Im and the combination
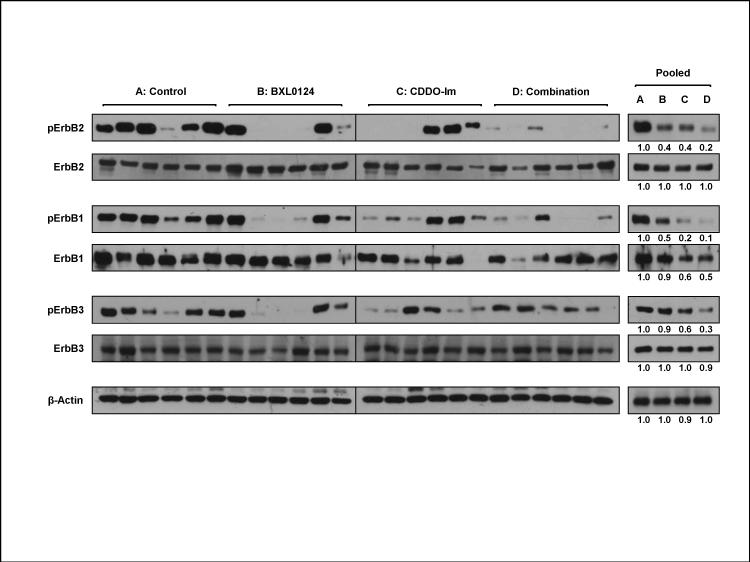
ErbB2 heterodimerizes with ErbB1 or ErbB3 and transactivation has been shown to play a critical role in tumorigenesis of ErbB2-overexpressing breast cancer (28). Therefore, we investigated the effects of BXL0124, CDDO-Im and the combination on the activation of ErbB2 as well as ErbB1 and ErbB3 in the mammary tumors of MMTV-ErbB2/neu mice. Six tumors were randomly selected after excluding large (>0.9 cm3) or small (<0.2 cm3) tumors, and levels of given proteins were analyzed as individual samples (Fig.3; left panel). The same amount of the six individual samples (3 μg per sample) were combined for each group and analyzed as pooled samples (Fig. 3; right panel). The protein level of activated ErbB2 was markedly decreased by BXL0124, CDDO-Im and the combination, while the protein level of total ErbB2 was not changed by any of the treatments (Fig. 3). BXL0124, CDDO-Im and the combination repressed the protein level of activated ErbB1 (pErbB1), and the protein level of total ErbB1 was also reduced by CDDO-Im and the combination (Fig. 3). The protein level of activated ErbB3 (pErbB3) was also repressed by all three treatments, while the protein level of total ErbB3 remained unchanged by any of the treatments (Fig. 3).
Figure 3. Inhibition of the activation of ErbB family receptors by BXL0124, CDDO-Im and the combination on MMTV-ErbB2/neu mammary tumors.
Six tumors from each group were randomly selected based on similar sizes and analyzed as individual tumors (left panel). These six individual tumors from each group were combined as a single pooled sample (right panel). Protein levels of pErbB2, ErbB2, pErbB1, ErbB1, pErbB3 and ErbB3 were determined by Western blot analysis. β-Actin was used as a loading control. For the pooled samples (right panel), quantitation of Western blots was performed by Image J 1.44p (NIH), and the numbers are provided at the bottom of each Western blot.
BXL0124, CDDO-Im and the combination differentially down-regulated mRNA levels of ErbB family receptors and their ligands in MMTV-ErbB2/neu mammary tumors
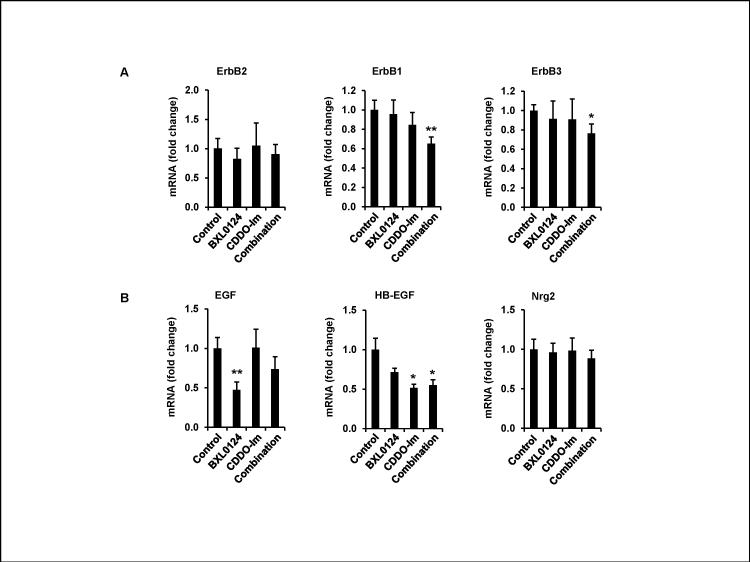
The effects of BXL0124, CDDO-Im and the combination on the mRNA level of ErbB family receptors in MMTV-ErbB2/neu mammary tumors were investigated (Fig. 4). The fold change of average mRNA level for each group relative to control group was shown (Fig. 4). BXL0124, CDDO-Im and the combination did not have significant effects on the mRNA level of ErbB2 (Fig. 4A). The mRNA levels of ErbB1 and ErbB3 were not significantly changed by BXL0124 or CDDO-Im, whereas the combination significantly decreased the mRNA levels of ErbB1 (p<0.01) and ErbB3 (p<0.05) (Fig. 4A). The mRNA levels of EGF and HB-EGF, key ligands of ErbB1, as well as neuregulin1 (Nrg1) and neuregulin2 (Nrg2), key ligands of ErbB3, were measured to investigate the effect of BXL0124, CDDO-Im and the combination on ErbB ligands. BXL0124 significantly decreased the mRNA level of EGF in ErbB2-overexpressing mammary tumors (p<0.01) (Fig. 4B). The mRNA level of HB-EGF was significantly decreased by CDDO-Im (p<0.05) and the combination (p<0.05) (Fig. 4B). The mRNA level of Nrg1 was low (cycle number of qPCR > 30) in all ErbB2-overexpressing mammary tumors (data not shown), and the mRNA level of Nrg2 did not show significant changes by any of the treatments (Fig. 4B).
Figure 4. Effects of BXL0124, CDDO-Im and the combination on the mRNA levels of ErbB family receptors and their ligands in MMTV-ErbB2/neu mammary tumors.
(A) The mRNA expression levels of ErbB family receptors, ErbB2, ErbB1 and ErbB3 in MMRV-ErbB2/neu mammary tumors were determined by qPCR (n=6) (B) The mRNA expression levels of ErbB ligands, EGF, HB-EGF and Nrg2 in MMTV-ErbB2/neu mammary tumors were determined by qPCR (n=6). Data is presented as mean ± S.E. Statistical significance was determined by ANOVA with Dunnett's adjustment (* p<0.05, ** p<0.01).
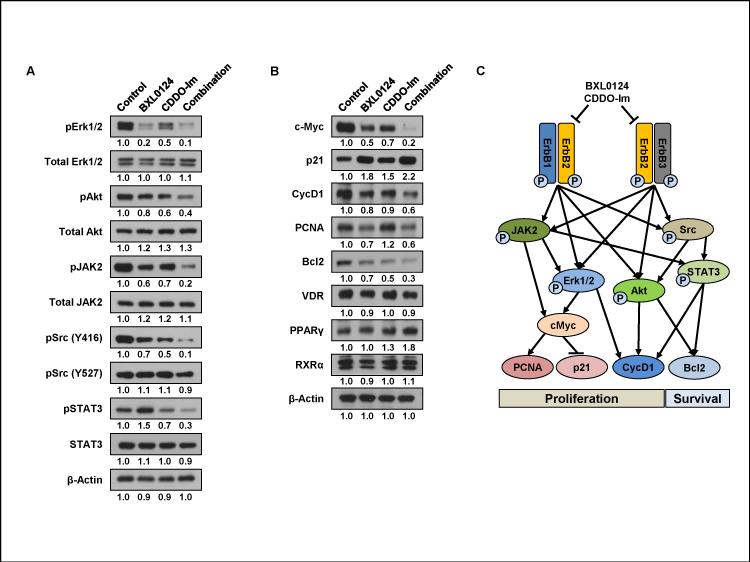
Treatment with BXL0124, CDDO-Im and the combination repressed downstream signaling pathways and molecular targets of ErbB2 to regulate proliferation and survival of MMTV-ErbB2/neu mammary tumors
We investigated the effects of BXL0124, CDDO-Im and the combination on the downstream signaling pathways of ErbB receptors in MMTV-ErbB2/neu mammary tumors (Fig. 5). The protein levels of activated Erk1/2 (pErk1/2) and Akt (pAkt), two key downstream molecules of ErbB2 signaling, were markedly inhibited by BXL0124, CDDO-Im and the combination, while the protein level of total Erk1/2 and Akt were not affected (Fig. 5A). BXL0124, CDDO-Im and the combination also markedly decreased the activation of JAK2 (determined by phosphorylated-JAK2, pJAK2) and Src [determined by phosphorylated-Src at Y416 position, pSrc (Y416)], intracellular kinases that regulate downstream targets of ErbB signal (Fig. 5A). The protein level of total JAK2 and the inactive form of Src [pSrc (Y527)] did not show changes in any of the treatment groups (Fig. 5A). Activation of STAT3 was inhibited by CDDO-Im and the combination, whereas BXL0124 moderately increased the activation of STAT3 (determined by phosphorylated-STAT3, pSTAT3) (Fig. 5A).
Figure 5. Effects of BXL0124, CDDO-Im and the combination on the downstream signaling pathways of ErbB receptors in MMTV-ErbB2/neu mammary tumors.
(A) The effects of BXL0124, CDDO-Im and the combination on the activation of direct downstream molecules of ErbB receptors, Erk1/2, Akt, JAK2, Src and STAT3, were determined by Western blot analysis (n=6). (B) The regulation of molecular targets of the ErbB signaling pathways, c-Myc, p21, CycD1, PCNA, GSK3β, Bcl2, by each treatment was investigated with Western blot analysis. The protein levels of VDR, PPARγ and RXRα were measured by Western blot analysis (n=6). β-Actin was used as a loading control. Quantitation of Western blots was performed by Image J 1.44p (NIH), and the numbers are provided at the bottom of each Western blot. (C) A schematic diagram of downstream signaling pathways of ErbB receptors that were regulated by BXL0124, CDDO-Im and the combination in mammary tumors of MMTV-ErbB2/neu mice.
The effects of BXL0124, CDDO-Im and the combination on protein levels of downstream targets of the ErbB2 signaling pathway were further investigated. c-Myc, a transcriptional regulator of multiple genes involving cell proliferation, was markedly decreased by BXL0124, CDDO-Im and the combination (Fig. 5B). BXL0124, CDDO-Im and the combination increased p21, while the three treatments decreased cyclin D1 (Fig. 5B). Proliferating cell nuclear antigen (PCNA) was repressed by BXL0124 and the combination (Fig. 5B). Bcl2, a key regulator of cell survival, was also markedly decreased by BXL0124, CDDO-Im and the combination (Fig. 5B). The effects of BXL0124, CDDO-Im and the combination on their receptors, vitamin D receptor (VDR) for BXL0124 and peroxisome proliferator activated receptor γ (PPARγ) for CDDO-Im were investigated. There were no effects on VDR, but PPARγ was increased by the combination (Fig. 5B). VDR forms heterodimers with retinoid X receptor α (RXRα) to regulate the expression of VDR-targeted genes (29). PPARγ also forms heterodimers with RXR, and the RXR agonists, such as bexarotene, potentiate the biological function of PPAR ligands, including CDDO or CDDO-Im (20, 30). Therefore, we determined the protein level of RXRα, which was not affected by BXL0124, CDDO-Im or the combination (Fig. 5B). The proposed ErbB signaling pathways regulated by BXL0124, CDDO-Im and the combination is shown in Figure 5C.
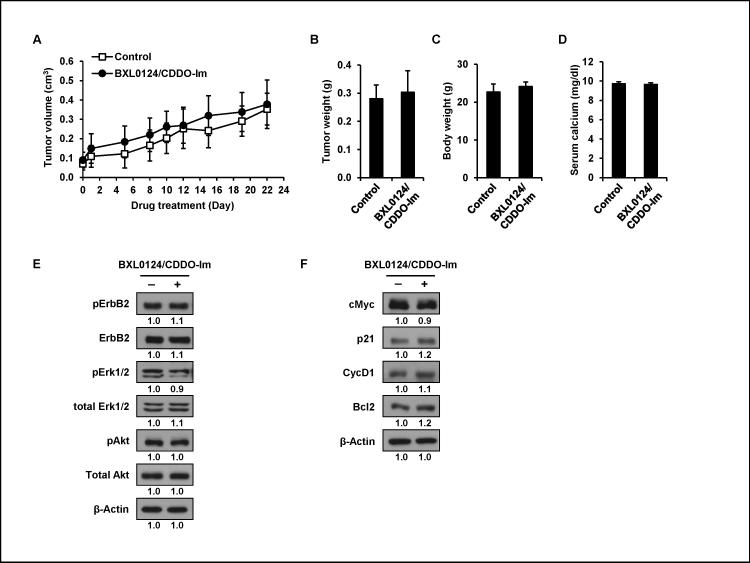
Short-term treatment with the combination of BXL0124 and CDDO-Im did not show anti-tumor activity on established mammary tumors in MMTV-ErbB2/neu transgenic mice
In the prevention study, MMTV-ErbB2/neu mice were treated prior to the development of mammary tumors, and long-term treatment with the combination of BXL0124 and CDDO-Im showed the most potent chemopreventive activity. In the treatment study, MMTV-ErbB2/neu mice were kept without treatment until they developed mammary tumors. Following the development of mammary tumors, the tumor size was measured, and mice were assigned to control (n=11) or treatment group (n=13) with a similar average tumor size (0.07 cm3 for control and 0.08 cm3 for treatment) in each group. Mice were then treated with control or the combination of BXL0124 (0.3 μg/kg BW) and CDDO-Im (3 μmole/kg BW) for three weeks. The 3-week treatment with the combination did not affect the growth rate of MMTV-ErbB2 mammary tumors (Fig. 6A). There were no distinctive differences between the control and treatment groups for the average tumor weight (Fig. 6B), body weight (Fig. 6C) and serum calcium level (Fig. 6D). Five tumor samples from each group were combined and analyzed to study the effects of short-term treatment with the combination on the ErbB2 signaling pathway and its downstream targets. Protein levels of total and activated ErbB2, Erk1/2 and Akt were not affected by the combination (Fig. 6E). The protein levels of downstream target molecules, c-Myc, p21, CycD1 and Bcl2 were also not changed by the combination treatment (Fig. 6F).
Figure 6. Effects of short-term treatment with the combination of BXL0124 and CDDO-Im on mammary tumors of MMTV-ErbB2/neu mice.
MMTV-ErbB2/neu transgenic mice with established mammary tumors were treated orally with vehicle control (DMSO, n=11) or the combination of BXL0124 (0.3 μg/kg body weight) and CDDO-Im (3 μmole/kg body weight) (n=13) six times a week for three weeks. (A) The tumor size was measured three times a week to determine the growth rate of tumors. Average tumor weight (B), body weight (C) and serum calcium levels (D) of each group were shown. Data is presented as mean ± S.E. (n=11 for control and n=13 for the combination). (E) The effects of the combination on the activation the ErbB2 signaling pathway were determined by Western blot analysis. Five tumors within similar size (tumor sizes ranging 0.28-0.51 cm3) were selected from each group and pooled for Western blot analysis. (F) The regulation of downstream targets of the ErbB2 signaling pathway by the combination was investigated with Western blot analysis. Five tumors with similar size (tumor sizes ranging 0.28-0.51 cm3) were selected from each group and pooled for Western blot analysis. β-Actin was used as a loading control. Quantification of Western blot was performed by Image J 1.44p (NIH), and the numbers are provided at the bottom of each Western blot.
Discussion
The present study demonstrated that the Gemini vitamin D analog BXL0124, the synthetic triterpenoid CDDO-Im and the combination delayed the development of mammary tumors in MMTV-ErbB2/neu mice (Fig. 1). Although both BXL0124 and CDDO-Im markedly inhibited the activation of ErbB2, BXL0124 and CDDO-Im showed different activities on the suppression of downstream signaling pathways of ErbB2 (Fig. 3 and 5). The combination was more effective than the individual compounds for inhibiting the activation of ErbB2 (Fig. 3). Moreover, the combination had additive effects on the suppression of the multiple downstream signaling pathways of ErbB2 (Fig. 5), emphasizing the advantage of the combination on the inhibition of the ErbB2 signaling pathway.
The study by Lee et al. showed that BXL0124 significantly decreased the mammary tumor burden in MMTV-ErbB2/neu mice (12). Previously, MMTV-ErbB2/neu mice were administered BXL0124 by intraperitoneal injection (12), whereas MMTV-ErbB/neu mice were given BXL0124 by oral gavage in the present study. BXL0124 decreased mammary tumor burden by 30% (Fig. 1), although the effect was lower than previously reported. The different routes of BXL0124 administration could influence the bioavailability of BXL0124 in animals, which might be the reason for the lower efficacy of BXL0124 shown in the present study.
The recent study by Liby et al. showed that CDDO-Me, equivalently potent as CDDO-Im with better stability, prevented mammary tumorigenesis in MMTV-ErbB2/neu mice, and its inhibitory effect was synergistic in combination with the rexinoid LG100268 (LG268) (17). Studies with breast cancer cell lines demonstrated that CDDO-Me and LG268 had different molecular targets and biological functions (17). In the present study, the combination of BXL0124 and CDDO-Im significantly delayed development of MMTV-ErbB2/neu mammary tumors, although its inhibitory effect was not significantly better than the effect of single treatment with CDDO-Im (Fig. 1). Interestingly, BXL0124 suppressed the p-ERK1/2/c-Myc/PCNA proliferation pathway, whereas CDDO-Im inhibited the pSrc/pSTAT3/Bcl2 survival pathway (Fig. 5C). In addition, the doses of BXL0124 and CDDO-Im used in the present study were much lower than their maximum tolerated doses, showing no signs of toxicity or weight loss during the in vivo experiment. Synthetic triterpenoids, including CDDO-Im, act on different molecular targets depending on the concentration (14). Therefore, further investigation with higher doses of CDDO-Im than the dose used in the present study might be necessary to determine synergistic effects in combination with other drugs. CDDO-Me also significantly arrested the growth of established mammary tumors in MMTV-ErbB2/neu mice in the previous report (17), which was not achieved with CDDO-Im in the present study. Liby et al. used higher dose of CDDO-Me in the treatment protocol (100 mg/kg diet ≈ 25 mg/kg body weight) than the dose used in the prevention protocol (60 mg/kg diet ≈ 15 mg/kg body weight) (17). In the present study, the dose of CDDO-Im used in the treatment and prevention protocols was same (3 μmole/kg body weight ≈ 1.6 μg/kg body weight). In addition, MMTV-ErbB2/neu mice were fed with diet containing CDDO-Me in the study by Liby et al. (17), whereas MMTV-ErbB2/neu mice were given CDDO-Im by oral gavage in the present study. Therefore, it might be difficult to directly compare the anti-cancer activities of CDDO-Me and CDDO-Im based on the results of these two studies. Further evaluation with same dose of CDDO-Me and CDDO-Im by the same route of administration might be necessary to make conclusive comparison.
Pharmacodynamic study by Yates et al. showed that CDDO-Im could be readily absorbed through the digestive system of mice after oral administration and was pharmacologically active in inducing Nrf2-regulated genes in many organs, including liver, lung, kidney and intestine (25). In the present study, we also demonstrated that CDDO-Im could be orally delivered and was biologically active to prevent ErbB2 overexpression-driven mammary tumorigenesis (Fig. 1). Although CDDO-Im is one of the most potent synthetic triterpenoids in various bioassays in vitro and in vivo, it was found to be unstable in human plasma (20, 31, 32). Moreover, the solid form of CDDO-Im was decomposed within one year when stored at 4°C (33). 1-[2-cyano-3,12-dioxooleana-1,9(11)-dien-28-oyl]-4-ethynylimiadazole, one of the recently developed N-acylimidazole analogues of CDDO, was shown to be nearly as potent as CDDO-Im while its solid form was more stable than that of CDDO-Im (33). Further preclinical evaluation of the stable N-acylimidazole analogue of CDDO is presently ongoing for potential clinical development as a chemopreventive or chemotherapeutic agent (33).
The transactivation of ErbB2 via heterodimerization with ErbB1 is one of the key mechanisms to potentiate the activation of its downstream signaling such as MAPK and PI3K/Akt (2). A study using the normal mammary epithelial cell line, MCF10A, demonstrated that overexpression of wild-type ErbB2 was insufficient to induce invasive transformation of MCF10A cells in 3D culture, which required additional stimulation by EGF (34). In addition, transactivation of ErbB2 and ErbB1 by EGF caused the resistance of ErbB2-overexpressing breast cancer against ErbB2-targeting antibodies (35). In the present study, the protein levels of activated ErbB2 but not total ErbB2 were markedly decreased by BXL0124, CDDO-Im and the combination (Fig. 3), indicating that inhibition of ErbB2 activation rather than inhibition of ErbB2 expression was a key anti-cancer mechanism of the compounds. We also found a strong correlation between ErbB2 activation and ErbB1 activation (Fig. 3), suggesting the transactivation of ErbB2 and ErbB1 in MMTV-ErbB2/neu mammary tumors. In addition, we found that the treatments significantly inhibited mRNA levels of ErbB1 ligands, EGF and HB-EGF (Fig. 4B), indicating ligand-induced transactivation of ErbB2 and ErbB1 as a critical target of the treatment.
c-Myc is a key transcriptional regulator of cellular proliferation, differentiation and apoptosis, and its amplification has been frequently found in human breast cancer (36). In ErbB2-overexpressing breast cancer cells, c-Myc was demonstrated as one of key effectors of ErbB2 signaling to sustain ErbB2-driven cell proliferation (37). In human breast cancer, the strong correlation between gene amplification of ErbB2 and c-Myc was reported, and patients with amplification of both ErbB2 and c-Myc had substantially worse clinical outcomes than patients with single-gene amplification (38, 39). A recent trastuzumab trial, HER2-positive National Surgical Adjuvant Breast and Bowel Project (NSABP) B31, demonstrated that c-Myc alterations were associated with different clinical benefits with trastuzumab in patients with early stage ErbB2-overexpressing breast cancer (40). In the present study, c-Myc was highly expressed in MMTV-ErbB2/neu mammary tumors, and the treatments with BXL0124, CDDO-Im and the combination markedly decreased the protein level of c-Myc (Fig. 5B). In addition, the regulation of c-Myc by the treatments was associated with altered protein levels of downstream targets of c-Myc, p21 and PCNA, to regulate cell proliferation (Fig. 5B and 5C), emphasizing the importance of c-Myc as key downstream effector of ErbB2 signaling.
The amplification of ErbB2 has been reported in both premalignant ductal carcinoma in situ and invasive ductal carcinoma, suggesting the involvement of ErbB2 signaling in both early development and late progression of mammary tumorigenesis (3). Moreover, preclinical studies reported that chemotherapeutic drugs targeting ErbB receptors, such as gefitinib (ErbB1) and lapatinib (both ErbB1 and ErbB2), also had preventive effects on the development of ErbB2-overexpressing mammary tumors (41, 42). Therefore, we investigated the effects of the combination of BXL0124 and CDDO-Im on ErbB2-overexpressing mammary tumorigenesis in prevention and treatment studies. Our results showed that the combination treatment was effective in blocking or delaying the development of ErbB2-overexpressing mammary tumors, while it was not active on established mammary tumors. One explanation is that the activation of ErbB2 at an early stage of tumorigenesis may be inhibited by the treatment, leading to reduction of mammary tumor formation. Once the tumors are established, however, ErbB2 is overexpressed and highly activated such that the combination treatment would not reverse the activation of ErbB2 signaling. It is also possible that the duration of treatment was too short to elicit any effect. The short-term treatment did not induce apoptosis that can contribute to the reduction of established tumors. Higher dose of CDDO-Im should be tested for the activity of the combination on the established MMTV-ErbB2/neu mammary tumors, since high concentrations of CDDO-Im were required to induce apoptosis in breast cancer cells (19, 43). Further long-term treatment or dose-escalation studies may be necessary to confirm the inactivity of the treatment on established tumors.
ErbB2 has been a critical target for breast cancer patients with ErbB2-overexpressing tumors, and ErbB2-targeting therapies such as trastuzumab have markedly improved clinical outcomes of ErbB2-overexpressing breast cancer patients. However, there is still a need to search for chemopreventive agents for the ErbB2-positive subtype of breast cancer. Moreover, with the complexity of the inter-connected signaling pathway of ErbB2 and other ErbB family receptors, drugs or combination of drugs targeting different components of the ErbB2 signaling pathway might be more effective. In the present study, we demonstrate that both BXL0124 and CDDO-Im targeted multiple components of the ErbB2 signaling pathway and delayed the development of ErbB2-overexpressing mammary tumors. The combination of BXL0124 and CDDO-Im showed additive effects on the inhibition of the ErbB2 signaling pathway, suggesting BXL0124, CDDO-Im and the combination as potentially useful chemopreventive agents in ErbB2-overexpressing breast cancers.
Acknowledgements
We would like to thank the Laboratory of Animal Service at the Department of Chemical Biology for animal care.
Grant support
This work was supported in part by the National Institutes of Health [R01 CA127645 to N.S.], and the Trustees Research Fellowship Program at Rutgers, The State University of New Jersey [to N.S.].
Footnotes
Disclosure of potential conflicts of interest: Michael B. Sporn, Karen T. Liby and Nanjoo Suh have a commercial research grant from Reata Pharmaceuticals Inc.; Michael B. Sporn, Karen T. Liby and Nanjoo Suh have patent interests in synthetic triterpenoids.
References
- 1.Arteaga CL, Sliwkowski MX, Osborne CK, Perez EA, Puglisi F, Gianni L. Treatment of HER2-positive breast cancer: current status and future perspectives. Nat Rev Clin Oncol. 2012;9:16–32. doi: 10.1038/nrclinonc.2011.177. [DOI] [PubMed] [Google Scholar]
- 2.Graus-Porta D, Beerli RR, Daly JM, Hynes NE. ErbB-2, the preferred heterodimerization partner of all ErbB receptors, is a mediator of lateral signaling. EMBO J. 1997;16:1647–55. doi: 10.1093/emboj/16.7.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hynes NE, Lane HA. ERBB receptors and cancer: the complexity of targeted inhibitors. Nat Rev Cancer. 2005;5:341–54. doi: 10.1038/nrc1609. [DOI] [PubMed] [Google Scholar]
- 4.Allred DC, Clark GM, Molina R, Tandon AK, Schnitt SJ, Gilchrist KW, et al. Overexpression of HER-2/neu and its relationship with other prognostic factors change during the progression of in situ to invasive breast cancer. Hum Pathol. 1992;23:974–9. doi: 10.1016/0046-8177(92)90257-4. [DOI] [PubMed] [Google Scholar]
- 5.Roses RE, Paulson EC, Sharma A, Schueller JE, Nisenbaum H, Weinstein S, et al. HER-2/neu overexpression as a predictor for the transition from in situ to invasive breast cancer. Cancer Epidemiol Biomarkers Prev. 2009;18:1386–9. doi: 10.1158/1055-9965.EPI-08-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pradeep CR, Zeisel A, Kostler WJ, Lauriola M, Jacob-Hirsch J, Haibe-Kains B, et al. Modeling invasive breast cancer: growth factors propel progression of HER2-positive premalignant lesions. Oncogene. 2012;31:3569–83. doi: 10.1038/onc.2011.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bikle D. Nonclassic actions of vitamin D. J Steroid Biochem Mol Biol. 2009;94:26–34. doi: 10.1210/jc.2008-1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams JS, Hewison M. Update in vitamin D. J Steroid Biochem Mol Biol. 2010;95:471–8. doi: 10.1210/jc.2009-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deeb KK, Trump DL, Johnson CS. Vitamin D signalling pathways in cancer: potential for anticancer therapeutics. Nat Rev Cancer. 2007;7:684–700. doi: 10.1038/nrc2196. [DOI] [PubMed] [Google Scholar]
- 10.Zinser GM, Welsh JE. Vitamin D receptor status alters mammary gland morphology and tumorigenesis in MMTV-neu mice. Carcinogenesis. 2004;25:2361–72. doi: 10.1093/carcin/bgh271. [DOI] [PubMed] [Google Scholar]
- 11.Lee HJ, Paul S, Atalla N, Thomas PE, Lin X, Yang I, et al. Gemini vitamin D analogues inhibit estrogen receptor-positive and estrogen receptor-negative mammary tumorigenesis without hypercalcemic toxicity. Cancer Prev Res (Phila) 2008;1:476–84. doi: 10.1158/1940-6207.CAPR-08-0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HJ, So JY, DeCastro A, Smolarek A, Paul S, Maehr H, et al. Gemini vitamin D analog suppresses ErbB2-positive mammary tumor growth via inhibition of ErbB2/AKT/ERK signaling. J Steroid Biochem Mol Biol. 2010;121:408. doi: 10.1016/j.jsbmb.2010.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishino H, Nishino A, Takayasu J, Hasegawa T, Iwashima A, Hirabayashi K, et al. Inhibition of the tumor-promoting action of 12-O-tetradecanoylphorbol-13-acetate by some oleanane-type triterpenoid compounds. Cancer Res. 1988;48:5210–5. [PubMed] [Google Scholar]
- 14.Liby KT, Yore MM, Sporn MB. Triterpenoids and rexinoids as multifunctional agents for the prevention and treatment of cancer. Nat Rev Cancer. 2007;7:357–69. doi: 10.1038/nrc2129. [DOI] [PubMed] [Google Scholar]
- 15.Konopleva M, Zhang W, Shi YX, McQueen T, Tsao T, Abdelrahim M, et al. Synthetic triterpenoid 2-cyano-3, 12-dioxooleana-1, 9-dien-28-oic acid induces growth arrest in HER2-overexpressing breast cancer cells. Mol Cancer Ther. 2006;5:317–28. doi: 10.1158/1535-7163.MCT-05-0350. [DOI] [PubMed] [Google Scholar]
- 16.Bishayee A, Ahmed S, Brankov N, Perloff M. Triterpenoids as potential agents for the chemoprevention and therapy of breast cancer. Front Biosci. 2011;16:980. doi: 10.2741/3730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liby K, Risingsong R, Royce DB, Williams CR, Yore MM, Honda T, et al. Prevention and Treatment of Experimental Estrogen Receptor–Negative Mammary Carcinogenesis by the Synthetic Triterpenoid CDDO-Methyl Ester and the Rexinoid LG100268. Clin Cancer Res. 2008;14:4556–63. doi: 10.1158/1078-0432.CCR-08-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim EH, Deng C, Sporn MB, Royce DB, Risingsong R, Williams CR, et al. CDDO-Methyl ester delays breast cancer development in BRCA1-mutated mice. Cancer Prev Res (Phila) 2012;5:89–97. doi: 10.1158/1940-6207.CAPR-11-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim EH, Deng CX, Sporn MB, Liby KT. CDDO-imidazolide induces DNA damage, G2/M arrest and apoptosis in BRCA1-mutated breast cancer cells. Cancer Prev Res (Phila) 2011;4:425–34. doi: 10.1158/1940-6207.CAPR-10-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Place AE, Suh N, Williams CR, Risingsong R, Honda T, Honda Y, et al. The novel synthetic triterpenoid, CDDO-imidazolide, inhibits inflammatory response and tumor growth in vivo. Clin Cancer Res. 2003;9:2798–806. [PubMed] [Google Scholar]
- 21.Ji Y, Lee HJ, Goodman C, Uskokovic M, Liby K, Sporn M, et al. The synthetic triterpenoid CDDO-imidazolide induces monocytic differentiation by activating the Smad and ERK signaling pathways in HL60 leukemia cells. Mol Cancer Ther. 2006;5:1452–8. doi: 10.1158/1535-7163.MCT-06-0136. [DOI] [PubMed] [Google Scholar]
- 22.Maehr H, Lee HJ, Perry B, Suh N, Uskokovic MR. Calcitriol derivatives with two different side chains at C-20. V. Potent inhibitors of mammary carcinogenesis and inducers of leukemia differentiation. J Med Chem. 2009;52:5505–19. doi: 10.1021/jm900780q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Honda T, Honda Y, Favaloro FG, Jr., Gribble GW, Suh N, Place AE, et al. A novel dicyanotriterpenoid, 2-cyano-3,12-dioxooleana-1,9(11)-dien-28-onitrile, active at picomolar concentrations for inhibition of nitric oxide production. Bioorg Med Chem Lett. 2002;12:1027–30. doi: 10.1016/s0960-894x(02)00105-1. [DOI] [PubMed] [Google Scholar]
- 24.Sporn MB, Liby KT, Yore MM, Fu L, Lopchuk JM, Gribble GW. New synthetic triterpenoids: potent agents for prevention and treatment of tissue injury caused by inflammatory and oxidative stress. J Nat Prod. 2011;74:537. doi: 10.1021/np100826q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yates MS, Tauchi M, Katsuoka F, Flanders KC, Liby KT, Honda T, et al. Pharmacodynamic characterization of chemopreventive triterpenoids as exceptionally potent inducers of Nrf2-regulated genes. Mol Cancer Ther. 2007;6:154–62. doi: 10.1158/1535-7163.MCT-06-0516. [DOI] [PubMed] [Google Scholar]
- 26.Lee HJ, Ju J, Paul S, So JY, DeCastro A, Smolarek A, et al. Mixed tocopherols prevent mammary tumorigenesis by inhibiting estrogen action and activating PPAR-gamma. Clin Cancer Res. 2009;15:4242–9. doi: 10.1158/1078-0432.CCR-08-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee HJ, Liu H, Goodman C, Ji Y, Maehr H, Uskokovic M, et al. Gene expression profiling changes induced by a novel Gemini Vitamin D derivative during the progression of breast cancer. Biochem Pharmacol. 2006;72:332–43. doi: 10.1016/j.bcp.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 28.Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2:127–37. doi: 10.1038/35052073. [DOI] [PubMed] [Google Scholar]
- 29.Staal A, Van Wijnen AJ, Birkenhäger J, Pols H, Prahl J, DeLuca H, et al. Distinct conformations of vitamin D receptor/retinoid X receptor-alpha heterodimers are specified by dinucleotide differences in the vitamin D-responsive elements of the osteocalcin and osteopontin genes. Mol Endocrinol. 1996;10:1444–56. doi: 10.1210/mend.10.11.8923469. [DOI] [PubMed] [Google Scholar]
- 30.Crowe DL, Chandraratna R. A retinoid X receptor (RXR)-selective retinoid reveals that RXR-alpha is potentially a therapeutic target in breast cancer cell lines, and that it potentiates antiproliferative and apoptotic responses to peroxisome proliferator-activated receptor ligands. Breast Cancer Res. 2004;6:R546–R55. doi: 10.1186/bcr913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Townson JL, Macdonald IC, Liby KT, Mackenzie L, Dales DW, Hedley BD, et al. The synthetic triterpenoid CDDO-Imidazolide suppresses experimental liver metastasis. Clin Exp Metastasis. 2011;28:309–17. doi: 10.1007/s10585-011-9374-z. [DOI] [PubMed] [Google Scholar]
- 32.Liby K, Yore MM, Roebuck BD, Baumgartner KJ, Honda T, Sundararajan C, et al. A novel acetylenic tricyclic bis-(cyano enone) potently induces phase 2 cytoprotective pathways and blocks liver carcinogenesis induced by aflatoxin. Cancer Res. 2008;68:6727–33. doi: 10.1158/0008-5472.CAN-08-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Honda T, Dinkova-Kostova AT, David E, Padegimas EM, Sundararajan C, Visnick M, et al. Synthesis and biological evaluation of 1-[2-cyano-3,12-dioxooleana-1,9(11)-dien-28-oyl]-4-ethynylimidazole. A novel and highly potent anti-inflammatory and cytoprotective agent. Bioorg Med Chem Lett. 2011;21:2188–91. doi: 10.1016/j.bmcl.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 34.Pradeep C, Zeisel A, Köstler W, Lauriola M, Jacob-Hirsch J, Haibe-Kains B, et al. Modeling invasive breast cancer: growth factors propel progression of HER2-positive premalignant lesions. Oncogene. 2011;31:3569–83. doi: 10.1038/onc.2011.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Motoyama AB, Hynes NE, Lane HA. The efficacy of ErbB receptor-targeted anticancer therapeutics is influenced by the availability of epidermal growth factor-related peptides. Cancer Res. 2002;62:3151–8. [PubMed] [Google Scholar]
- 36.Blancato J, Singh B, Liu A, Liao D, Dickson R. Correlation of amplification and overexpression of the c-myc oncogene in high-grade breast cancer: FISH, in situ hybridisation and immunohistochemical analyses. Br J Cancer. 2004;90:1612–9. doi: 10.1038/sj.bjc.6601703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neve RM, Sutterlüty H, Pullen N, Lane HA, Daly JM, Krek W, et al. Effects of oncogenic ErbB2 on G1 cell cycle regulators in breast tumour cells. Oncogene. 2000;19:1647. doi: 10.1038/sj.onc.1203470. [DOI] [PubMed] [Google Scholar]
- 38.Berns EMJJ, Klijn JGM, van Putten WLJ, van Staveren IL, Portengen H, Foekens JA. c-myc amplification is a better prognostic factor than HER2/neu amplification in primary breast cancer. Cancer Res. 1992;52:1107–13. [PubMed] [Google Scholar]
- 39.Al-Kuraya K, Schraml P, Torhorst J, Tapia C, Zaharieva B, Novotny H, et al. Prognostic relevance of gene amplifications and coamplifications in breast cancer. Cancer Res. 2004;64:8534–40. doi: 10.1158/0008-5472.CAN-04-1945. [DOI] [PubMed] [Google Scholar]
- 40.Perez EA, Jenkins RB, Dueck AC, Wiktor AE, Bedroske PP, Anderson SK, et al. C-MYC Alterations and Association With Patient Outcome in Early-Stage HER2-Positive Breast Cancer From the North Central Cancer Treatment Group N9831 Adjuvant Trastuzumab Trial. J Clin Oncol. 2011;29:651–9. doi: 10.1200/JCO.2010.30.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lu C, Speers C, Zhang Y, Xu X, Hill J, Steinbis E, et al. Effect of epidermal growth factor receptor inhibitor on development of estrogen receptor–negative mammary tumors. J Natl Cancer Inst. 2003;95:1825–33. doi: 10.1093/jnci/djg117. [DOI] [PubMed] [Google Scholar]
- 42.Strecker TE, Shen Q, Zhang Y, Hill JL, Li Y, Wang C, et al. Effect of lapatinib on the development of estrogen receptor–negative mammary tumors in mice. J Natl Cancer Inst. 2009;101:107–13. doi: 10.1093/jnci/djn436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hyer ML, Croxton R, Krajewska M, Krajewski S, Kress CL, Lu M, et al. Synthetic triterpenoids cooperate with tumor necrosis factor-related apoptosis-inducing ligand to induce apoptosis of breast cancer cells. Cancer Res. 2005;65:4799–808. doi: 10.1158/0008-5472.CAN-04-3319. [DOI] [PubMed] [Google Scholar]