Abstract
Background
Evidence suggests that the urogenital pain of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) may be neuropathic.
Methods
This randomized, double-blind, placebo-controlled trial was conducted across 10 tertiary care centers in North America to determine whether pregabalin, which has been proved effective in other chronic pain syndromes, is effective in reducing CP/CPPS symptoms. In 2006–2007, 324 men with pelvic pain for at least 3 of the previous 6 months were enrolled in this study. Men were randomly assigned to receive pregabalin or placebo in a 2:1 ratio and were treated for 6 weeks. Pregabalin dosage was increased from 150 to 600 mg/d during the first 4 weeks. The primary outcome was a 6-point decrease in the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) total score. Multiple secondary outcomes were assessed.
Results
Of 218 men assigned to receive pregabalin, 103 (47.2%) reported at least a 6-point decrease in the NIHCPSI total score at 6 weeks compared with 35.8% (38 of 106 men) assigned to receive placebo (P = .07, exact Mantel-Haenszel test, adjusting for clinical sites). Compared with the placebo group, men assigned to receive pregabalin experienced reductions in the NIH-CPSI total score and sub-scores (P < .05), a higher Global Response Assessment response rate (31.2% and 18.9%; P = .02), and improvement in total McGill Pain Questionnaire score (P = .01). Results for the other outcomes did not differ between groups.
Conclusion
Pregabalin therapy for 6 weeks was not superior to placebo use in the rate of a 6-point decrease (improvement) in the NIH-CPSI total score in men with CP/CPPS.
Trial Registration
clinicaltrials.gov Identifier: NCT00371033
CHRONIC PROSTATITIS/chronic pelvic pain syndrome (CP/CPPS), the most common form of prostatitis, is characterized by genitourinary pain with or without voiding symptoms in the absence of uropathogenic bacteria or other identifiable causes.1 Prostatitis accounts for almost 1.8 million office visits per year in the United States.2 The direct per-patient costs of care for CP/CPPS are $3817 per year,3 and men with CP/CPPS often have a poor quality of life.4 Although a variety of clinical drug trials have been conducted, there is no standard therapy for CP/CPPS.
The pathogenesis of CP/CPPS is uncertain. However, indirect evidence suggests that CP/CPPS may be a neurogenic pain syndrome. Because the defining symptom in CP/CPPS is urogenital pain, it seems likely that neurologic involvement occurs, either locally or centrally. In men with long-standing CP/CPPS, a history of other neurologic disease (eg, migraine headaches, vertebral disk disease or surgery, and numbness or tingling in the limbs) was almost 5 times more likely in cases than in controls.5 One of the few biomarkers to correlate with the levels of pain in CP/CPPS is nerve growth factor, a neurotrophin that has been found to have a regulatory role in nociceptive nerves and to function as a mediator and amplifier of neurogenic inflammation.6 Another biomarker that correlates with CPP is macrophage inflammatory protein–1α,7 an inflammatory chemokine that also plays a role in hyperalgesia.8 Also, men with CP/CPPS have been found to have abnormalities of the afferent and efferent autonomic nervous systems,9,10 suggesting central nervous system sensitization.
Drugs found to be effective for treating neuropathic pain may prove beneficial in treating the symptoms of CP/CPPS. Pregabalin is an antiepileptic drug that has been approved for use in the chronic pain of postherpetic neuralgia, diabetic neuropathy, and fibromyalgia.11–13 We conducted a randomized clinical trial to determine whether pregabalin therapy reduces symptoms in men with CP/CPPS.
METHODS
PARTICIPANTS
We recruited men from 10 tertiary care clinical centers in North America (Cleveland Clinic, Cleveland, Ohio; Harvard Medical School, Massachusetts General Hospital & Brigham and Women's Hospital, Boston; Northwestern University, Chicago, Illinois; Queen's University, Kingston, Ontario, Canada; Stanford University Medical Center, Stanford, California; Temple University, Philadelphia, Pennsylvania; University of California, Los Angeles/King Drew University, Los Angeles; University of Maryland, Baltimore; University of Mississippi, Jackson; and University of Washington, Seattle). The protocol was approved by the institutional review board at each participating institution, and written informed consent was obtained from each participant. Participants were enrolled consecutively at each site. Men were eligible for the study if their age was at least 18 years, they reported symptoms of discomfort or pain in the pelvic region during at least 3 of the previous 6 months, and they had a total score of at least 15 of 43 on the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI)14 at screening and randomization visits approximately 2 weeks apart. The exclusion criteria included a calculated creatinine clearance less than 60 mL/min/1.73 m2 (to convert to milliliters per second per square meter, multiply by 0.0167), a platelet count less than 100 000 × 103/μL (to convert to × 109 per liter, multiply by 1.0), allergy to any antiseizure medication, known sensitivity to pregabalin, treatment with thiazolidinedione or antidiabetic agents, New York Heart Association class III or IV congestive heart failure, a history of thrombocytopenia or bleeding diathesis, and a history of alcohol abuse. Participants were not excluded if they had previous treatment for CP/CPPS or for taking analgesics for another condition if they continued to have pelvic pain despite the analgesic therapy and had a score of at least 15 on the NIH-CPSI. Previous treatment with gabapentin or pregabalin was allowed if it was completed at least 2 weeks before study enrollment.
STUDY DESIGN
Eligible participants were randomly assigned 2:1 in each clinical site via a centrally controlled Web-based data management system to receive treatment with either pregabalin or matching placebo using a permuted block randomization procedure with randomly assigned block sizes of 3, 6, and 9. Treatment dosage was escalated as follows: 150 mg/d (50 mg orally 3 times daily) for 2 weeks, then 300 mg/d (100 mg orally 3 times daily) for 2 weeks, and then 600 mg/d (200 mg orally 3 times daily) for 2 weeks. Men assigned to receive placebo underwent a similar escalation in the number of capsules prescribed. If a participant could not tolerate a scheduled dose increase, he was allowed to remain at the previously tolerated dosage. Study investigators and participants were unaware of treatment assignment. Percentage adherence to treatment was calculated by taking the mean of the percentage of capsules taken based on capsule counts reported by the participants at the 2-, 4-, and 6-week contacts.
Adverse events (AEs) were evaluated by means of standardized queries at each study contact, including telephone calls at weeks 2 and 4 and a clinic visit at week 6. All adverse signs and symptoms and preexisting conditions that worsened, whether considered related to the study drug, were reported and were graded according to Medical Dictionary for Regulatory Activities version 6.0 criteria.15
OUTCOMES
The primary outcome was response, defined as a decrease (improvement) in the NIH-CPSI score of at least 6 points from baseline to week 6. The NIH-CPSI measures the 3 key domains of CP/CPPS: pain (location, frequency, and severity; possible score, 0–21), urinary symptoms (irritative and obstructive; possible score, 0–10), and impact/quality of life (possible score, 0–12), for a total possible score of 0 to 43. A 6-point decrease in NIHCPSI score has been shown to be clinically perceptible in previous clinical trials of men with CP/CPPS.16
Men who withdrew from the study before primary outcome at 6 weeks were considered nonresponders and were included in the denominator for determining the primary outcome response rate in an intent-to-treat analysis. Several secondary outcomes were assessed, including the Global Response Assessment (GRA).17 The GRA is a 7-question patient self-reported assessment that measures perception of change in symptoms (improvement, no change, or deterioration). The responses are centered at zero (no change in symptoms). It has been used as a primary end point for trials of interstitial cystitis (IC)18,19 and has been adopted for use in trials of CP/CPPS.16,17 Changes in the GRA correspond to changes in all the major symptom indices used for trials in IC and CP/CPPS.16,18 Men who reported that they were moderately or markedly improved on a 7-point GRA at the end of the study were identified as treatment responders for this secondary outcome. Comparison of the GRA between treatment arms includes men who withdrew early (3 in the placebo group and 8 in the pregabalin group), as prespecified in the Data Analysis and Monitoring Plan.
Other measures included the subscores of the NIH-CPSI (pain, urinary symptoms, and quality of life); the McGill Pain Questionnaire (ranges: 0–45 for total, 0–33 for sensory, and 0–12 for affective scores, with higher scores indicating greater pain)20; the Medical Outcomes Study 12-Item Short Form Health Survey (SF-12) (range, 0–100 for the Physical [PCS] and Mental [MCS] Component Summary scores, with the mean set at 50 and higher scores indicating better quality of life)21; the Hospital Anxiety and Depression Scale (HADS) (range, 0–42, with higher scores indicating greater anxiety and depression)22; and the Sexual Health Inventory for Men (SHIM) (range, 1–25, with higher scores indicating better sexual function).23
DATA MANAGEMENT AND STATISTICAL METHODS
Descriptive statistics were computed by treatment arm at baseline randomization for demographics, selected medical history measures, and all the primary and secondary symptom measures. Distributions of baseline characteristics were compared between treatment groups using Fisher exact tests, exact Kruskal-Wallis tests (for ordered categories), or Wilcoxon rank sum tests. These tests were conducted primarily to evaluate the success of randomization, thereby identifying any imbalances that could potentially affect treatment arm comparisons.
All AEs were included in a safety analysis regardless of whether these events were considered by the investigator to be related to treatment. Conditions that were present at baseline but did not change were excluded from the AE analysis. Comparisons of overall AE rates were performed using the Kruskal-Wallis test after classifying each patient according to worst grade reported across all body systems. The AE rates were compared between treatment arms for any body system with more than 5% AEs in either arm by classifying each patient according to the worst grade reported in that specific body system.
The primary outcome analysis compared response rates between treatment arms using the exact conditional test version of the Mantel-Haenszel test to control for clustering by clinical center.24 For secondary efficacy outcomes, cross-sectional descriptive statistics and changes from baseline were calculated across time. Changes across time were presented only for those with complete data at all follow-up visits to aid in assessment of changes. Pooled rate differences (and their 95% confidence intervals) in response rates across clinical centers were calculated using the “metan” routine in STATA version 10 (StataCorp LP, College Station, Texas) to implement a Mantel-Haenszel estimator for the pooled rate difference across clinical centers.25
Sample size requirements for this trial were based on 90% power to detect a difference in response rates of 40% to 60% (effect size of 20%) in the primary outcome, defined as a decline of 6 points or more in the NIH-CPSI total score. The estimated response rate of 40% for the placebo group was based on additional analyses (Richard Landis, PhD, unpublished data, 2005) of the data from a previous CP/CPPS study.26 Using a 2-sided α = .05 level of significance, a total of 318 participants (212 taking pregabalin and 106 taking placebo) were required. This proposed sample size included 15% inflation to compensate for clinical site variability and interim monitoring. An independent Data and Safety Monitoring Board established by the National Institute of Diabetes and Digestive and Kidney Diseases reviewed safety and efficacy data when 171 patients had reported the primary outcome; the board recommended continuation of the trial at that time.
RESULTS
BASELINE DATA
Recruitment began April 1, 2006, and ended on November 30, 2007. The treatment groups were well balanced with respect to baseline characteristics (Table 1). The mean (SD) age of the pregabalin group was 48.0 (13.0) years (age range, 21–78 years) compared with 45.2 (12.2) years (age range, 19–76 years) for the placebo group. There was no difference in racial composition between groups. Overall, 79.3% of participants were white, 11.9% were black, and the remaining 8.6% were multiethnic/multiracial or other. Educational level, employment status, and annual family income were also comparable between the 2 treatment arms. Of these men 56.7% were college graduates, 75.2% were employed, and 64.4% reported an annual family income exceeding $50 000.
Table 1.
Baseline Characteristics of the Participants by Treatment Arm
| Characteristic | Pregabalin Arm | Placebo Arm | Total | P Value | |
|---|---|---|---|---|---|
| Randomized participants, No. | 218 | 106 | 324 | ||
| Evaluable participants, No. | 216 | 103 | 319 | ||
| Age, y | |||||
| Mean (SD) | 48.0 (13.0) | 45.2 (12.2) | 47.0 (13.1) | .09 | |
| Median (range) | 47.0 (21–78) | 46.0 (19–76) | 47.0 (19–78) | ||
| Race, No. (%) |
|
.17a | |||
| North American Indian/North Native | 1 (0.5) | 3 (2.9) | 4 (1.3) | ||
| Asian/Asian American | 0 | 4 (3.9) | 4 (1.3) | ||
| Black | 24 (11.1) | 14 (13.6) | 38 (11.9) | ||
| Native Hawaiian/other Pacific Islander | 0 | 1 (1.0) | 1 (0.3) | ||
| White | 178 (82.4) | 75 (72.8) | 253 (79.3) | ||
| Other | 11 (5.1) | 1 (1.0) | 12 (3.8) | ||
| Multirace | 2 (1.0) | 4 (3.9) | 6 (1.9) | ||
| Missing | 0 | 1 (1.0) | 1 (0.3) | ||
| Educational level, No. (%) |
|
.97 | |||
| Less than high school | 5 (2.3) | 2 (1.9) | 7 (2.2) | ||
| High school/GED | 30 (13.9) | 17 (16.5) | 47 (14.7) | ||
| Some college | 58 (26.9) | 26 (25.2) | 84 (26.3) | ||
| Graduated from college | 78 (36.1) | 35 (34.0) | 113 (35.4) | ||
| Graduate school | 45 (20.8) | 23 (22.3) | 68 (21.3) | ||
| Employment, No. (%) |
|
.25 | |||
| Employed | 166 (76.9) | 74 (71.8) | 240 (75.2) | ||
| Unemployed | 12 (5.6) | 13 (12.6) | 25 (7.8) | ||
| Retired | 27 (12.5) | 11 (10.7) | 38 (11.9) | ||
| Full-time homemaker | 1 (0.5) | 0 | 1 (0.3) | ||
| Disabled | 10 (4.6) | 5 (4.9) | 15 (4.7) | ||
| Annual family income, No. (%) |
|
.70 | |||
| < $10 000 | 12 (7.1) | 7 (8.4) | 19 (7.5) | ||
| $10 001–$25 000 | 16 (9.4) | 7 (8.4) | 23 (9.1) | ||
| $25 001–$50 000 | 29 (17.1) | 19 (22.9) | 48 (19.0) | ||
| $50 001–$100 000 | 64 (37.6) | 25 (30.1) | 89 (35.2) | ||
| >$100 000 | 49 (28.8) | 25 (30.1) | 74 (29.2) | ||
| Missing | 46 | 20 | 66 | ||
| Ever diagnosis of IC, CP, or CPPS, No. (%) |
|
.99 | |||
| Yes | 139 (64.4) | 67 (64.4) | 206 (64.4) | ||
| No | 77 (35.6) | 37 (35.6) | 114 (35.6) | ||
| Years since first diagnosis |
|
.62 | |||
| Mean (SD) | 8.7 (9.5) | 9.2 (9.2) | 8.8 (9.4) | ||
| Median (range) | 5.2 (0.2–47.7) | 6.0 (0–36.2) | 5.3 (0–47.7) | ||
| Missing, No. | 78 | 37 | 115 | ||
| Years since first symptom began |
|
.87 | |||
| Mean (SD) | 10.3 (10.6) | 9.9 (9.8) | 10.2 (10.3) | ||
| Median (range) | 6.5 (0.5–48.7) | 6.3 (0–40.8) | 6.5 (0–48.7) | ||
| Missing, No. | 49 | 22 | 71 | ||
| Family ever diagnosis of IC/PBS |
|
.59 | |||
| Yes | 13 (7.8) | 4 (4.9) | 17 (6.8) | ||
| No | 154 (92.2) | 78 (95.1) | 232 (93.2) | ||
| Missing, No. | 49 | 21 | 70 | ||
| Family ever diagnosis of CP/CPPS, No. (%) |
|
.81 | |||
| Yes | 14 (8.3) | 7 (9.3) | 21 (8.6) | ||
| No | 155 (91.7) | 68 (90.7) | 223 (91.4) | ||
| Missing | 47 | 28 | 75 | ||
| Participants with a baseline CPSI score, No.b | 217 | 104 | 321 | ||
| NIH-CPSI total score (possible score, 0–43) | .64 | ||||
| Mean (SD) | 26.2 (5.6) | 25.9 (6.1) | 26.1 (5.7) | ||
| Median (range) | 25.5 (15.0–42.5) | 25.5 (15.0–43.0) | 25.5 (15.0–43.0) | ||
| NIH-CPSI pain subscore (possible score, 0–21) | .96 | ||||
| Mean (SD) | 12.3 (3.0) | 12.4 (3.1) | 12.4 (3.0) | ||
| Median (range) | 12.5 (4.0–20.5) | 12.0 (6.0–21.0) | 12.0 (4.0–21.0) | ||
| NIH-CPSI urinary symptoms subscore (possible score, 0–10) | .35 | ||||
| Mean (SD) | 4.9 (2.7) | 4.7 (2.7) | 4.8 (2.7) | ||
| Median (range) | 5.0 (0–10.0) | 4.5 (0–10.0) | 5.0 (0–10.0) | ||
| NIH-CPSI QOL subscore (possible score, 0–12) | .64 | ||||
| Mean (SD) | 8.9 (2.0) | 8.9 (2.0) | 8.9 (2.0) | ||
| Median (range) | 9.0 (4.0–12.0) | 9.0 (5.0–12.0) | 9.0 (4.0–12.0) | ||
| SF-12 PCS score (possible score, 0–100) | .51 | ||||
| Mean (SD) | 44.9 (10.1) | 43.9 (10.3) | 44.6 (10.2) | ||
| Median (range) | 46.9 (17.9–64.3) | 44.4 (20.0–60.1) | 46.1 (17.9–64.3) | ||
| Missing, No. | 3 | 1 | 4 | ||
| SF-12 MCS score (possible score, 0–100) | .43 | ||||
| Mean (SD) | 41.8 (10.6) | 42.8 (10.6) | 42.1 (10.6) | ||
| Median (range) | 41.3 (12.2–61.2) | 44.1 (18.0–62.0) | 42.2 (12.2–62.0) | ||
| Missing, No. | 3 | 1 | 4 |
Abbreviations: CP/CPPS, chronic prostatitis/chronic pelvic pain syndrome; GED, General Educational Development; IC, interstitial cystitis; MCS, Mental Component Summary; NIH-CPSI, National Institutes of Health Chronic Prostatitis Symptom Index; PBS, painful bladder syndrome; PCS, Physical Component Summary; QOL, quality of life; SF-12, 12-Item Short Form Health Survey.
Based on a comparison of the proportion of white vs nonwhite participants.
The baseline score is the mean score from 2 baseline visits.
In response to a urologic diagnosis question included in multiple National Institute of Diabetes and Digestive and Kidney Diseases–sponsored clinical trials, only 64.4% of participants in this study reported having ever been diagnosed as having IC, CP, or CPPS. Of those previously diagnosed, the mean (SD) symptom duration since diagnosis was 8.8 (9.4) years (range, 0–47.7 years). Of those reporting that they knew when their IC, CP, or CPPS symptoms began, the mean (SD) duration of symptoms was 10.2 (10.3) years (range, 0–48.7 years). None of these diagnosis or duration characteristics differed between treatment arms.
The NIH-CPSI total and domain scores are summarized by treatment arm in Table 1. For each of these measures, the 2 baseline scores were averaged to provide an overall baseline score to which follow-up scores were compared. The mean (SD) NIH-CPSI total score was 26.1 (5.7) (range, 15.0–43.0). Furthermore, at baseline, the SF-12 mean (SD) PCS score was 44.6 (10.2) (range, 17.9–64.3), and the mean (SD) MCS score was 42.1 (10.6) (range, 12.2–62.0), indicating lower-than-average quality of life. None of these baseline symptom scores differed between treatment arms.
PARTICIPANT FOLLOW-UP AND ADHERENCE
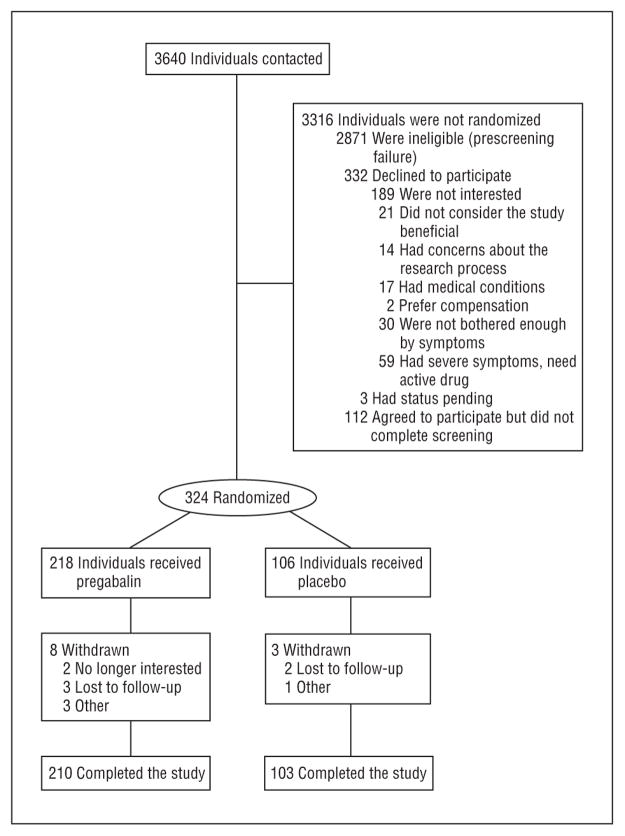
Of the 324 randomized participants, 313 (96.6%) completed 6 weeks of follow-up through the primary endpoint visit (Figure 1). Of the 11 withdrawals, 8 were treated with pregabalin (3.7% of that group) and 3 were treated with placebo (2.8% of that group) (P = .62, log rank test). All the participants were included in the intent-to-treat analysis. Of the 313 individuals who completed the study, 225 (71.9%) reported taking at least 95% of their allocated capsules, and 66 (21.1%) reported taking 75% to 95% of their allocated medications. Capsule count adherence rates were similar between the treatment arms. Overall, 236 participants (72.8%) completed at least 1 week at the highest dose, including 154 of those taking pregabalin (70.6%) and 82 of those in the placebo arm (77.4%). At the primary outcome assessment (week 6), 190 of the 313 participants (60.7%) reported maintaining the highest dose (Table 2).
Figure 1.
Flow of participants through the study phases. Patients had more than 1 reason to decline to participate.
Table 2.
Dose Titration by Treatment Arm
| Variable | Participants, No. (%) | ||
|---|---|---|---|
|
| |||
| Pregabalin Arm (n = 218) | Placebo Arm (n = 106) | Total (N = 324) | |
| Maximum dosage, mg/d | |||
| 150 | 14 (6.4) | 6 (5.7) | 20 (6.2) |
| 300 | 39 (17.9) | 12 (11.3) | 51 (15.7) |
| 600 | 154 (70.6) | 82 (77.4) | 236 (72.8) |
| Never took study drug | 11 (5.0) | 6 (5.7) | 17 (5.2) |
| Dosage at primary end point, mg/d | |||
| 150 | 36 (17.1) | 14 (13.6) | 50 (16.0) |
| 300 | 32 (15.2) | 12 (11.7) | 44 (14.1) |
| 600 | 122 (58.1) | 68 (66.0) | 190 (60.7) |
| Not taking study drug | 20 (9.5) | 9 (8.7) | 29 (9.3) |
| Missing/withdrawn | 8 | 3 | 11 |
SAFETY
Overall, 59.0% of the participants (191 of 324) reported at least 1 AE, classified primarily as mild (83 of 324 [25.6%]) or moderate (79 of 324 [24.4%]) in severity. There were no serious AEs. There was no difference in the overall distribution of AEs between treatment arms (P = .40). Categories for which at least 5% of participants reported AEs in either arm are summarized in Table 3. The pregabalin arm had more neurologic AEs than did the placebo arm (P = .01), whereas the placebo arm had more pain AEs than did the pregabalin arm (P = .003). Headache was the most common pain, with 10 patients taking pregabalin (4.6%) and 18 taking placebo (17.0%) reporting this AE.
Table 3.
Adverse Events Reported by at Least 5% of Participants in Either Arm
| Adverse Event | Pregabalin Arm, % | Placebo Arm, % | P Valuea |
|---|---|---|---|
| Constitutional symptoms | 24.3 | 20.8 | .57 |
| Neurologic symptoms | 38.5 | 22.6 | .01 |
| Gastrointestinal disturbance | 18.3 | 18.9 | >.99 |
| Ocular/visual symptoms | 6.9 | 2.8 | .20 |
| Renal/genitourinary symptoms | 5.5 | 1.9 | .16 |
| Pain | 17.4 | 33.3 | .003 |
Fisher exact test.
EFFICACY/PRIMARY OUTCOME
Of men assigned to the pregabalin group, 47.2% (103 of 218) were responders (a ≥6-point drop in the NIHCPSI total score) compared with 35.8% (38 of 106) of men assigned to the placebo group (P = .07, exact Mantel-Haenszel test, controlling for clinical sites) (Table 4).
Table 4.
Primary and Secondary Outcome Measures at Baseline and 6 Weeks and Differences in Change Across Time by Treatment Arm
| Outcome Measure | Baseline | 6 wk | Differences in Change, Pregabalin–Placebo, No. (95% CI)a | P Value | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Pregabalin Arm | Placebo Arm | Pregabalin Arm | Placebo Arm | |||
| Primary outcome | ||||||
| NIH-CPSI responder rate (≥6-point decline), No./total No. (%) | NA | NA | 103/218 (47.2) | 38/106 (35.8) | 10.9 (−0.0 to 21.8) | .07 |
| Secondary outcomesb | ||||||
| GRA responder rate, No./total No. (%) | NA | NA | 68/218 (31.2) | 20/106 (18.9) | 12.0 (2.6 to 21.5) | .02 |
| NIH-CPSI score, mean (SD) | ||||||
| Total | 26.2 (5.6) | 25.9 (6.1) | 19.7 (8.5) | 21.6 (8.9) | −2.4 (−4.1 to −0.6) | .01 |
| Pain domain | 12.3 (3.0) | 12.4 (3.1) | 9.1 (4.6) | 10.1 (4.7) | −1.0 (−2.0 to −0.04) | .04 |
| Urinary symptoms domain | 4.9 (2.7) | 4.7 (2.7) | 3.7 (2.6) | 4.0 (2.7) | −0.7 (−1.2 to −0.2) | .01 |
| QOL domain | 8.9 (2.0) | 8.9 (2.0) | 6.9 (2.9) | 7.4 (3.1) | −0.7 (−1.2 to −0.1) | .02 |
| HADS score, mean (SD) | 14.8 (7.5) | 14.1 (7.3) | 12.4 (7.8) | 12.2 (7.8) | −0.7 (−2.0 to 0.7) | .36 |
| IIEF-SHIM score, mean (SD) | 16.9 (7.9) | 17.4 (7.1) | 16.4 (8.4) | 17.2 (7.8) | −0.6 (−2.1 to 0.9) | .40 |
| McGill Pain Questionnaire score, mean (SD) | 13.8 (8.7) | 14.1 (8.5) | 9.6 (8.8) | 12.4 (9.1) | −2.3 (−4.0 to −0.7) | .01 |
| MOS SF-12 score, mean (SD) | ||||||
| PCS | 44.9 (10.1) | 43.9 (10.3) | 46.9 (10.1) | 44.3 (10.6) | 1.3 (−0.5 to 3.2) | .34 |
| MCS | 41.8 (10.6) | 42.8 (10.6) | 45.0 (11.2) | 44.6 (10.6) | 1.4 (−0.9 to 3.8) | .22 |
Abbreviations: CI, confidence interval; GRA, Global Response Assessment; HADS, Hospital Anxiety and Depression Scale; IIEF-SHIM, International Index of Erectile Function Sexual Health Inventory for Men; MCS, Mental Component Summary; MOS SF-12, Medical Outcomes Study 12-Item Short Form Health Survey; NA, not applicable; NIH-CPSI, National Institutes of Health Chronic Prostatitis Symptom Index; PCS, Physical Component Summary; QOL, quality of life.
The pooled rate difference and the 95% CI for this rate difference in response rates across clinical centers were calculated using the “metan” routine in STATA version 10 (StataCorp LP, College Station, Texas) to implement a Mantel-Haenszel estimator for the pooled rate difference across clinical centers.25
Sample sizes for secondary outcomes ranged from 201 to 210 for the pregabalin arm and from 98 to 103 for the placebo arm.
SECONDARY OUTCOMES
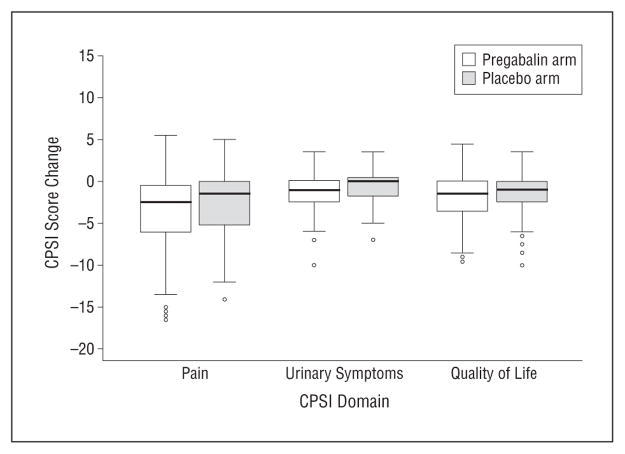
Of the men who were assessed at 6 weeks, the NIH-CPSI total score decreased by a mean of 6.6 points in the pregabalin arm and 4.2 points in the placebo arm (median, 5.1-point decrease for pregabalin and 2.5-point decrease for placebo, P = .01). Similar results were observed for each of the 3 NIH-CPSI subscores, with improvements of 3.3 (pregabalin) and 2.2 (placebo) of 21 points for the pain subscore (P = .04), 1.2 (pregabalin) and 0.6 (placebo) of 10 points for the urinary symptoms subscore (P = .01), and 2.1 (pregabalin) and 1.4 (placebo) of 12 points for the quality-of-life subscore (P = .02) (Figure 2).
Figure 2.
Box and whisker plot comparing Chronic Prostatitis Symptom Index (CPSI) score changes from baseline to week 6 in the pregabalin and placebo arms for each domain. The horizontal line in the middle of each box indicates the median, and the top and bottom borders of the box mark the 75th and 25th percentiles, respectively. The whiskers above and below the box mark the 90th and 10th percentiles, respectively. The points beyond the whiskers are outliers beyond the 90th or 10th percentiles.
The GRA response rate was significantly higher in men treated with pregabalin (31.2%) compared with placebo (18.9%) (P = .02). For this comparison, missing or withdrawn participants were considered nonresponders. Men treated with pregabalin showed more improvement than did those receiving placebo in the McGill Pain Questionnaire total score (P = .01), indicating more improvement in the pregabalin group for the sensory (P = .03) and affective (P = .02) subdomains. There were no differences between the pregabalin and placebo groups in SF-12 (P = .34 for PCS and P = .22 for MCS), HADS (P = .36), or SHIM (P = .40) scores.
COMMENT
Among men with long-standing CP/CPPS who had been treated previously for this condition, a 6-week course of pregabalin compared with placebo did not result in a statistically significant reduction in the NIH-CPSI total score by at least 6 points, the primary outcome, an amount of change previously shown to be clinically perceptible to participants. The results of most of the secondary outcomes should be interpreted with caution because only men who completed the 6-week treatment schedule were analyzed. However, for the GRA analysis, men who did not complete the study were considered nonresponders, thereby maintaining an intent-to-treat analysis and minimizing bias introduced by analyzing only men who completed the study.
The reason for the discrepancy between the results for the primary outcome and the GRA is unclear. The underlying NIH-CPSI continuous scales demonstrated “shifts” in efficacy across the entire distribution of the changes (from baseline to 6 weeks) in the total score and each subscore (pain, urinary symptoms, and quality of life) that was not detected at the same level of statistical significance when dichotomizing the change. This slight loss in power attenuates the P value from .01 to .04 for continuous end points to .07 for the dichotomous primary outcome. Although the GRA response (also a dichotomous measure) attained statistical significance, the GRA placebo rate was only 19% compared with 36% for the 6-point decrease in the NIH-CPSI total score criterion for response. The GRA may provide a more comprehensive evaluation of a patient's overall condition than the condition-specific symptoms measured using the NIH-CPSI. A variety of secondary outcomes, including SF-12, SHIM, and HADS scores, did not differ between treatment arms, suggesting that not all relevant aspects of CP/CPPS may be treated with pregabalin.
Sensitivity analyses from previous clinical trials showed that although a 4-point decrease in the NIH-CPSI total score is clinically perceptible, a 6-point decrease provides a more robust indication of perceived improvement.16 Although a 4-point decrease was used in another clinical trial for CP/CPPS,27 we chose a 6-point decline in the NIH-CPSI total score as the primary outcome to correspond to a potentially greater clinical benefit that would likely outweigh the possible risk that pregabalin therapy might pose from AEs. The dose range was chosen based on previous trials showing the beneficial dose of pregabalin to be 300 mg/d for postherpetic neuralgia and diabetic neuropathy12,13 and 450 mg/d for fibromyalgia.11 Pregabalin therapy proved safe in the present population. Although 59.0% of participants reported AEs, all were mild or moderate in severity, and the overall incidence was similar in the 2 treatment arms. Neurologic AEs were more common in the pregabalin group, but the rate was not dose related.
This trial has several limitations. Participants had longstanding symptoms; it is possible that patients with a shorter duration of symptoms may respond differently. Therapy was for 6 weeks only. It may take a longer period of treatment before a beneficial effect is seen. However, previous trials of pregabalin in other disorders have demonstrated an improvement in pain after only several days of treatment.12 There were several positive features of this study. This group of participants with longstanding symptoms represents the most difficult group of men with CP/CPPS to treat. We used the NIH-CPSI, which is a validated outcome measure designed specifically for use in trials of CP/CPPS.14 We also used a wide range of secondary outcomes that have been shown to be important in CP/CPPS and also gave valuable information on differences in response between treatment arms.
In summary, 6 weeks of treatment with an increasing dosage of pregabalin up to 600 mg/d did not produce a clinically significant (6-point) decrease in a condition-specific symptom index for CP/CPPS compared with placebo therapy. Based on P = .07, recent recommendations on interpretation of results of clinical trials suggest that pregabalin might be superior to placebo.28 Given these results, the hypothesis is that men with a neurologic basis for their symptoms respond better to pregabalin therapy. Development and validation of practical approaches to the identification of clinically relevant sub-populations of patients with CP/CPPS to predict response to treatment and direct tailored therapy is the focus of active investigation in ongoing clinical studies.
Acknowledgments
Funding/Support: No author received compensation for the performance of this study except as salary support from a grant from the National Institutes of Health. This study was supported by cooperative agreements U01 DK65209, UO1 DK65268, U01 DK65297, U01 DK65187, U01 DK65277, U01 DK65189, U01 DK65174, U01 DK65266, U01 DK65257, U01 DK65186, and U01 DK65287 from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Center for Minority Health and Health Disparities. Pregabalin and matching placebo capsules were provided by Pfizer Inc.
Footnotes
Author Contributions: Drs Pontari and Landis had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Pontari, Krieger, Litwin, White, Anderson, McNaughton-Collins, Nickel, Shoskes, Alexander, O'Leary, Zeitlin, Landis, Propert, Kusek, Nyberg, and Schaeffer. Acquisition of data: Pontari, Litwin, White, Anderson, McNaughton-Collins, Nickel, Shoskes, Alexander, O'Leary, Zeitlin, Landis, and Schaeffer. Analysis and interpretation of data: Pontari, Krieger, Litwin, Nickel, Shoskes, Alexander, O'Leary, Chuai, Landis, Cen, Propert, Nyberg, and Schaeffer. Drafting of the manuscript: Pontari, Krieger, Nickel, O'Leary, Zeitlin, Landis, Cen, and Propert. Critical revision of the manuscript for important intellectual content: Pontari, Krieger, Litwin, White, Anderson, McNaughton-Collins, Nickel, Shoskes, O'Leary, Chuai, Landis, Propert, Kusek, Nyberg, and Schaeffer. Statistical analysis: Litwin, Shoskes, Chuai, Landis, Cen, and Propert. Obtained funding: Pontari, Litwin, Anderson, McNaughton-Collins, Nickel, Alexander, O'Leary, Landis, and Nyberg. Administrative, technical, and material support: Pontari, Krieger, Litwin, White, Propert, Kusek, and Nyberg. Study supervision: Pontari, Litwin, Anderson, O'Leary, Landis, and Nyberg.
Financial Disclosure: Dr Pontari received consulting fees from Sanofi-Aventis, Pfizer, and GlaxoSmithKline and reported clinical trial participation with Pfizer; Dr Krieger received consulting and advising fees from Pfizer; Dr Litwin received consulting fees from Sanofi-Aventis; Dr Anderson received consulting fees from Bioness Inc, investigator fees from Boston Scientific and Allergan, and speaker fees from GlaxoSmithKline and Astella; Dr Nickel reports receiving consulting fees from Merck, GlaxoSmithKline, Pfizer, Ortho Women's Health, Farr Labs, Watson, Medtronic, NeurAxon, and Genyous Biomed and research support from Merck, GlaxoSmithKline, Allergan, Watson, Pfizer, and American Medical Systems; Dr Shoskes received consulting fees from Roche, is on the advisory board of Farr Labs, and has a financial interest in Triurol; Dr Alexander received lecture fees from Boehringer Ingelheim; Dr O'Leary received consulting fees from Sanofi-Aventis; Dr Landis received consulting fees from Sanofi-Aventis; Dr Kusek holds stock in Decode Genetics; and Dr Schaeffer was a consultant for Alita Pharmaceuticals, American Medical Systems, NovaBay Pharmaceuticals, Regeneron Pharm Inc, IMS Health, Exoxemis Inc, CombinatoRx Inc, Monitor Company Group LP, and Advanstar Communications and received meeting honorarium from the Scientific Consulting Group.
Previous Presentation: This study was presented at the meeting of the American Urological Association; April 26, 2009; Chicago, Illinois.
Additional Information: The 10 participating institutions were as follows: Cleveland Clinic, Cleveland, Ohio; Harvard Medical School, Massachusetts General Hospital & Brigham and Women's Hospital, Boston; Northwestern University, Chicago, Illinois; Queen's University, Kingston, Ontario, Canada; Stanford University Medical Center, Stanford, California; Temple University, Philadelphia, Pennsylvania; University of California, Los Angeles/King Drew University, Los Angeles; University of Maryland, Baltimore; University of Mississippi, Jackson; and University of Washington, Seattle.
Contributor Information
Dr Michel A. Pontari, Department of Urology, Temple University, Philadelphia, Pennsylvania.
Dr John N. Krieger, Department of Urology, University of Washington, Seattle.
Dr Mark S. Litwin, Departments of Urology and Health Services, David Geffen School of Medicine and School of Public Health, University of California, Los Angeles.
Dr Paige C. White, Department of Surgery, University of Mississippi, and Coast Urology Center, Gulfport.
Dr Rodney U. Anderson, Department of Urology, Stanford University Medical Center, Stanford, California.
Dr Mary McNaughton-Collins, Department of Medicine, Massachusetts General Hospital, Boston.
Dr J. Curtis Nickel, Department of Urology, Queen's University, Kingston, Ontario, Canada.
Dr Daniel A. Shoskes, Glickman Urological and Kidney Institute, Cleveland Clinic, Cleveland, Ohio.
Dr Richard B. Alexander, Department of Urology, University of Maryland, Baltimore.
Dr Michael O'Leary, Department of Surgery, Harvard Medical School, and Division of Urology, Brigham and Women's Hospital, Boston.
Dr Scott Zeitlin, Departments of Urology and Health Services, David Geffen School of Medicine and School of Public Health, University of California, Los Angeles.
Ms Shannon Chuai, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia.
Dr J. Richard Landis, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia.
Ms Liyi Cen, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia.
Dr Kathleen J. Propert, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia.
Dr John W. Kusek, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, Maryland.
Dr Leroy M. Nyberg, Jr, Retired.
Dr Anthony J. Schaeffer, Department of Urology, Feinberg School of Medicine, Northwestern University, Chicago, Illinois.
References
- 1.Krieger JN, Nyberg L, Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999;282(3):236–237. doi: 10.1001/jama.282.3.236. [DOI] [PubMed] [Google Scholar]
- 2.Pontari MA, Joyce GF, Wise M, McNaughton-Collins M Urologic Diseases in America Project. Prostatitis. J Urol. 2007;177(6):2050–2057. doi: 10.1016/j.juro.2007.01.128. [DOI] [PubMed] [Google Scholar]
- 3.Calhoun EA, McNaughton Collins M, Pontari MA, et al. Chronic Prostatitis Collaborative Research Network. The economic impact of chronic prostatitis. Arch Intern Med. 2004;164(11):1231–1236. doi: 10.1001/archinte.164.11.1231. [DOI] [PubMed] [Google Scholar]
- 4.McNaughton Collins M, Pontari MA, O'Leary MP, et al. Chronic Prostatitis Collaborative Research Network. Quality of life is impaired in men with chronic prostatitis: the Chronic Prostatitis Collaborative Research Network. J Gen Intern Med. 2001;16(10):656–662. doi: 10.1111/j.1525-1497.2001.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pontari MA, McNaughton-Collins M, O'Leary MP, et al. CPCRN Study Group. A case-control study of risk factors in men with chronic pelvic pain syndrome. BJU Int. 2005;96(4):559–565. doi: 10.1111/j.1464-410X.2005.05684.x. [DOI] [PubMed] [Google Scholar]
- 6.Miller LJ, Fischer KA, Goralnick SJ, et al. Nerve growth factor and chronic prostatitis/chronic pelvic pain syndrome. Urology. 2002;59(4):603–608. doi: 10.1016/s0090-4295(01)01597-7. [DOI] [PubMed] [Google Scholar]
- 7.Desireddi NV, Campbell PL, Stern JA, et al. Monocyte chemoattractant protein-1 and macrophage inflammatory protein-1α as possible biomarkers for the chronic pelvic pain syndrome. J Urol. 2008;179(5):1857–1862. doi: 10.1016/j.juro.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang N, Inan S, Inan S, et al. A proinflammatory chemokine, CCL3, sensitizes the heat- and capsaicin-gated ion channel TRPV1 [published correction appears in Proc Natl Acad Sci USA. 2005;102(19):7050] Proc Natl Acad Sci USA. 2005;102(12):4536–4541. doi: 10.1073/pnas.0406030102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang CC, Lee JC, Kromm BG, Ciol MA, Berger RE. Pain sensitization in male chronic pelvic pain syndrome: why are symptoms so difficult to treat? J Urol. 2003;170(3):823–827. doi: 10.1097/01.ju.0000082710.47402.03. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz U, Liu YW, Berger RE, Yang CC. Autonomic nervous system changes in men with chronic pelvic pain syndrome. J Urol. 2007;177(6):2170–2174. doi: 10.1016/j.juro.2007.01.144. [DOI] [PubMed] [Google Scholar]
- 11.Crofford LJ, Rowbotham MC, Mease PJ, et al. Pregabalin 1008-105 Study Group. Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(4):1264–1273. doi: 10.1002/art.20983. [DOI] [PubMed] [Google Scholar]
- 12.Dworkin RH, Corbin AE, Young JP, Jr, et al. Pregabalin for the treatment of post-herpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2003;60(8):1274–1283. doi: 10.1212/01.wnl.0000055433.55136.55. [DOI] [PubMed] [Google Scholar]
- 13.Rosenstock J, Tuchman M, LaMoreaux L, Sharma U. Pregabalin for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial. Pain. 2004;110(3):628–638. doi: 10.1016/j.pain.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Litwin MS, McNaughton-Collins M, Fowler FJ, Jr, et al. Chronic Prostatitis Collaborative Research Network. The National Institutes of Health Chronic Prostatitis Symptom Index: development and validation of a new outcome measure. J Urol. 1999;162(2):369–375. doi: 10.1016/s0022-5347(05)68562-x. [DOI] [PubMed] [Google Scholar]
- 15.Cancer Therapy Evaluation Program. [Accessed July 20, 2010];Common Terminology Criteria for Adverse Events v3.0 (CTCAE) National Cancer Institute Web site. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Published August 9, 2006.
- 16.Propert KJ, Litwin MS, Wang Y, et al. Chronic Prostatitis Collaborative Research Network (CPCRN) Responsiveness of the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) Qual Life Res. 2006;15(2):299–305. doi: 10.1007/s11136-005-1317-1. [DOI] [PubMed] [Google Scholar]
- 17.Propert KJ, Alexander RB, Nickel JC, et al. Chronic Prostatitis Collaborative Research Network. Design of a multicenter randomized clinical trial for chronic prostatitis/chronic pelvic pain syndrome. Urology. 2002;59(6):870–876. doi: 10.1016/s0090-4295(02)01601-1. [DOI] [PubMed] [Google Scholar]
- 18.Propert KJ, Mayer RD, Wang Y, et al. Interstitial Cystitis Clinical Trials Group. Responsiveness of symptom scales for interstitial cystitis. Urology. 2006;67(1):55–59. doi: 10.1016/j.urology.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Propert KJ, Payne C, Kusek JW, Nyberg LM. Pitfalls in the design of clinical trials for interstitial cystitis. Urology. 2002;60(5):742–748. doi: 10.1016/s0090-4295(02)01775-2. [DOI] [PubMed] [Google Scholar]
- 20.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 24.Mehta C, Patel N. Proc-StatXact for SAS Users: Statistical Software for Exact Non-parametric Inference. Cambridge, MA: Cytel Software Corp; 1997. [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alexander RB, Propert KJ, Schaeffer AJ, et al. Chronic Prostatitis Collaborative Research Network. Ciprofloxacin or tamsulosin in men with chronic prostatitis–chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004;141(8):581–589. doi: 10.7326/0003-4819-141-8-200410190-00005. [DOI] [PubMed] [Google Scholar]
- 27.Nickel JC, Krieger JN, McNaughton-Collins M, et al. Chronic Prostatitis Collaborative Research Network. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. N Engl J Med. 2008;359(25):2663–2673. doi: 10.1056/NEJMoa0803240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pocock SJ, Ware JH. Translating statistical findings into plain English. Lancet. 2009;373(9679):1926–1928. doi: 10.1016/S0140-6736(09)60499-2. [DOI] [PubMed] [Google Scholar]