Abstract
Background
Dimensional models of co-morbidity have the potential to improve the conceptualization of mental disorders in research and clinical work, yet little is known about how relatively uncommon disorders may fit with more common disorders. The present study estimated the meta-structure of psychopathology in the US general population focusing on the placement of five under-studied disorders sharing features of thought disorder: paranoid, schizoid, avoidant and schizotypal personality disorders, and manic episodes as well as bipolar disorder.
Method
Data were drawn from the National Epidemiologic Survey on Alcohol and Related Conditions, a face-to-face interview of 34 653 non-institutionalized adults in the US general population. The meta-structure of 16 DSM-IV Axis I and Axis II psychiatric disorders, as assessed by the Alcohol Use Disorder and Associated Disabilities Interview Schedule DSM-IV version (AUDADIS-IV), was examined using exploratory and confirmatory factor analysis.
Results
We document an empirically derived thought disorder factor that is a subdomain of the internalizing dimension, characterized by schizoid, paranoid, schizotypal and avoidant personality disorders as well as manic episodes. Manic episodes exhibit notable associations with both the distress subdomain of the internalizing dimension as well as the thought disorder subdomain. The structure was replicated for bipolar disorder (I or II) in place of manic episodes.
Conclusions
As our understanding of psychopathological meta-structure expands, incorporation of disorders characterized by detachment and psychoticism grows increasingly important. Disorders characterized by detachment and psychoticism may be well conceptualized, organized and measured as a subdimension of the internalizing spectrum of disorders. Manic episodes and bipolar disorder exhibit substantial co-morbidity across both distress and thought disorder domains of the internalizing dimension. Clinically, these results underscore the potential utility of conceptualizing patient treatment needs using an approach targeting psychopathological systems underlying meta-structural classification rubrics.
Keywords: Dimensional, externalizing, internalizing, metastructure, psychosis, thought disorders
Introduction
Substantial evidence indicates that the co-morbidity structure for many common psychiatric disorders can be parsimoniously represented by two latent dimensions that broadly capture the shared variance of these disorders (Krueger, 1999; Kessler et al. 2011). The first, often termed the ‘internalizing’ dimension, represents the propensity to experience unipolar mood and anxiety disorders, i.e. major depression, generalized anxiety disorder, panic disorder, and social and specific phobias. The second dimension, often termed the ‘externalizing’ dimension, represents the propensity to experience disinhibitory disorders, i.e. substance-use disorders, antisocial personality disorder and conduct disorder (Krueger et al. 2002). Further, the internalizing dimension is frequently (Krueger, 1999; Eaton et al. 2011) although not always (Kessler et al. 2011) found to encompass two subfactors: distress and fear. The distress subfactor is indicated by major depression, dysthymia and generalized anxiety disorder, while the fear subfactor is indicated by panic disorder, social phobia and simple phobia. Post-traumatic stress disorder (PTSD), while studied less often, has been found to indicate either the distress or the fear subfactor (Cox et al. 2002; Wolf et al. 2010). Despite varying prevalences of each individual disorder within different population subgroups, the internalizing– externalizing structure of disorders is found consistently across groups (Krueger et al. 2003; Kessler et al. 2011; Eaton et al. 2012). Identification of these dimensions has led to knowledge that the psychiatric disorders are indicators of a broader underlying dimensional structure. Subsequent important work has documented that both genetic and environmental risk factors for psychopathology can be more parsimoniously described in terms of their relation to the internalizing and externalizing dimensions than to specific disorders (Kendler et al. 2003; Kessler et al. 2011; Keyes et al. 2012). This literature has direct relevance to optimizing clinical treatment of patients with psychopathology. Rather than a focus solely on individual disorders, the empirically robust dimensional models of pathology suggest that a review of major psychopathological systems may be a useful way to identify appropriate treatment strategies (Barlow et al. 2011).
Despite this growth in knowledge on the internalizing and externalizing dimensions as constructs useful in modeling and understanding co-morbidity, important gaps remain in our understanding of psychopathological structure due to the limited range of disorders analysed. Disorders suggested on theoretical grounds as components of additional dimensions of psychopathology are those characterized by psychoticism (e.g. unusual beliefs, eccentricity and cognitive dysregulation) combined with pathological introversion or detachment (e.g. social isolation, lack of meaningful relationships) (Wolf et al. 1988; Kendler et al. 1993, 1995; Carpenter et al. 2009). Some diagnostic criteria for these disorders clearly differ from those of many internalizing and externalizing disorders. However, the disorders about which less is known have substantial co-morbidity and even some phenotypic overlap with disorders in the internalizing and externalizing dimensions (e.g. social anxiety and isolation are central to schizotypal and schizoid personality disorders and also social phobia), suggesting that they may be manifestations of a shared underlying dimension. The little empirical evidence to date is inconsistent. In psychiatric patients, schizophrenia and other disorders characterized by psychoticism form a distinct factor that is correlated with, yet distinct from, internalizing and externalizing dimensions (Wolf et al. 1988; Kotov et al. 2011a, b). In a UK-based general population sample, psychoticism and pathological introversion formed two factors distinct from each other as well as from the internalizing and externalizing dimensions (Markon, 2010). In contrast, in a Colorado community sample, schizophrenia loaded well with other internalizing disorders, and a two-factor model including schizophrenia provided a good fit to data (Verona et al. 2004). Thus, consensus has not been reached on the relation of disorders characterized by detachment and psychoticism to the metastructure of common disorders, leaving the patterns of co-morbidity and the position of these disorders within the internalizing–externalizing framework inadequately understood.
Of considerable further interest is the relationship of disorders characterized by mania, such as manic episodes and bipolar disorders, to the structure of psychopathology. One possibility that has been suggested on theoretical grounds is that manic episodes and bipolar disorders are manifestations of a psychoticism dimension (Goldberg et al. 2009), given the substantial shared genetic correlation between bipolar and schizophrenia spectrum disorders (Goldberg et al. 2009; Lichtenstein et al. 2009). Most studies of the internalizing and externalizing dimensions have not included manic episodes or bipolar disorders in metastructure analyses; those examinations that have included bipolar disorder have indicated placement on the internalizing dimension (Watson, 2005; Kessler et al. 2011; Forbush & Watson, 2012), though indicators of psychoticism were not included in these investigations. Kotov et al. (2011b) found that manic episodes were best placed as manifestations of a dimension of thought disorders. No studies to our knowledge have evaluated the meta-structure of psychopathology incorporating manic episodes. Thus, further analyses in representative datasets are required to converge on the structure of co-morbidity including manic episodes and bipolar disorders.
Given these gaps in knowledge, the aim of the present study was to determine whether disorders characterized by detachment and/or psychoticism form an additional factor in the well-established meta-structure of psychopathology formed by an internalizing and an externalizing dimension. To do this, we incorporated disorders primarily characterized by symptoms of social detachment and/or psychoticism: four personality disorders (schizotypal, schizoid, avoidant and paranoid personality disorder) and manic episodes and bipolar disorder. We use a large, national sample in the USA for this work, which allowed us to split the sample and conduct replication analyses of the factors identified. In total, we examine the co-morbidity structure of 17 Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) psychiatric disorders, the largest collection of disorders examined in the general population to date.
Method
Study design and sample
Data were drawn from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a study of non-institutionalized adults in the USA residing in homes or group quarters. NESARC data were collected at two time points: initial data were collected in 2001–2002 with 43 093 participants (response rate: 81% of those eligible). A second assessment was conducted in 2004–2005 with 34 653 participants [86.7% of original sample; ineligible respondents included deceased (n=1403); deported, mentally or physically impaired (n=781); or on active duty in the armed forces (n=950)]. The cumulative response rate over both waves was 70.2%. Young people, blacks and Hispanics were oversampled; data were weighted to reflect the demographic characteristics in the US population based on the 2000 census (Grant et al. 2009). The research protocol, including written informed consent procedures, received full ethical review and approval from the US Census Bureau and the US Office of Management and Budget. Further details of the study design and sampling methods can be found elsewhere (Grant et al. 2009). The present study included the 34 653 participants in the second assessment, as this was the wave that included measures of schizotypal personality disorder and PTSD. Among those who participated in the second assessment, 48% were women; 25.4% were aged <35 years, 31.1% were aged 35–49 years, 24.1% were aged 50–64 years, and 19.3% were aged ≥65 years. White subjects comprised 70.9% of the sample, African-Americans, 11.1%, Hispanics, 11.6%, Asian or Pacific Islander, 4.3%, and American Indians and Alaska Natives, 2.2%.
Measures
Participants were interviewed face-to-face with the Alcohol Use Disorder and Associated Disabilities Interview Schedule DSM-IV version (AUDADIS-IV; Grant et al. 2001), a fully structured instrument designed for administration by experienced lay interviewers.
Mood disorders
We examined the lifetime occurrence (i.e. those reported at any time point across either wave 1 or wave 2) of mood disorders diagnosed using DSM-IV criteria including major depressive episode, dysthymia, manic episodes, and bipolar I or II. Bipolar I and II diagnoses were based on respondent history of both major depressive episodes and manic episodes. Dichotomous indicators of the presence or absence of disorder were used as indicator variables of latent internalizing dimensions in factor analyses, as is common in this literature (Krueger et al. 1998). Good test–retest reliability for mood disorder diagnoses has been documented (Ruan et al. 2008). In preliminary analyses, we separated bipolar I and II. Results did not differ when bipolar I and II were combined. Analyses were conducted with manic episodes and replicated with bipolar disorder; given that major depressive episodes are necessary criteria for bipolar disorder, we wanted to examine whether the manic aspects of bipolar disorders showed a different relation with the meta-structure of psychopathology than the manic plus depressive aspects of bipolar disorders.
Anxiety disorders
A total of five DSM-IV lifetime anxiety disorders were included, all of which have been previously examined in national samples as part of the psychopathology meta-structure (Eaton et al. 2011, 2012; Kessler et al. 2011): panic disorder (with or without agoraphobia), social phobia, specific phobia, generalized anxiety disorder, and PTSD. The test–retest reliability of anxiety disorder diagnoses ranged from fair (0.42, panic) to good (0.69, PTSD) (Grant et al. 2003).
Substance-use disorders
We examined any alcohol abuse or dependence diagnosis, any cannabis abuse or dependence diagnosis, any other (i.e. non-cannabis) illicit drug abuse or dependence diagnosis, and tobacco dependence (Hicks et al. 2007). AUDADIS-IV alcohol and drug dependence diagnoses demonstrated good to excellent test– retest reliability (κ=0.67–0.84) in clinical and general population samples (Hasin et al. 2007).
Personality disorders
A total of five personality disorders were included. We included antisocial personality disorder, given the extensive literature on the placement of this personality disorder within the externalizing spectrum (Krueger et al. 2002; Kendler et al. 2003). We also included avoidant, schizoid, schizotypal and paranoid personality disorder. The test–retest reliability of these diagnoses ranged from 0.53 (schizoid personality disorder) to 0.67 (schizotypal personality disorder) (Ruan et al. 2008). Antisocial personality disorder was assessed at both waves 1 and 2 of the NESARC (a diagnosis at either wave was included); schizoid personality disorder and paranoid personality disorder were assessed at wave 1; and schizotypal personality disorder was assessed at wave 2.
Analysis
Mplus version 5.21 was used for all analyses (Muthén & Muthén, 2010). Diagnoses were treated as categorical variables, and analyses incorporated the wave 2 weighting, clustering, and stratification variables. We first established symptom unidimensionality within each of the five disorders previously uncharacterized in the meta-structure in these data: schizotypal, avoidant, schizoid, and paranoid personality disorder as well as manic disorder. We used exploratory factor analysis (EFA) with binary symptom items and geomin rotated loadings, using the weighted least squares means and variance adjusted (WLSMV) estimator and DELTA parameterization. WLSMV allows for tractable estimation of complex models when manifest variables are categorical. Model comparisons were based on several indices of model fit including the comparative fit index (CFI), Tucker–Lewis index (TLI) and root mean squared error of approximation (RMSEA). Values of CFI/TLI >0.95, and values of RMSEA <0.06, are common guidelines for inferring good model fit (Hu & Bentler, 1999). We then divided the sample in half based on a random number generator, resulting in two randomly selected subsamples with no respondent overlap. In the first randomly selected subsample (n=17 326), we used EFA to empirically evaluate the factor structure that emerged across the 16 psychiatric diagnoses, using the same rotation and model fit indices outlined above.
Once an initial empirical structure was selected from the EFA, we used the second randomly selected subsample (n=17 327) to conduct confirmatory factor analysis (CFA) to refine a parsimonious model and determine the fit to the data. We estimated three models. (1) We selected disorders for factors in the CFA for which the standardized loadings from the EFA were greater than 0.3 (a conservative cut-off), and estimated a CFA model with the WLSMV estimator and DELTA parameterization. (2) Based on modification indices, we selected additional disorders for factors if the standardized estimated parameter change would be 0.3, similar to our selection criteria moving from EFA to CFA. We then estimated a second CFA model with these additional disorders included. (3) Finally, we removed disorders from factors if the standardized factor loading was less than 0.3, which would indicate limited relation with the underlying dimension. That is, we removed all coefficients less than 0.3, and re-estimated a final model that provided both good fit to the data and parsimony.
Results
Prevalence
Table 1 shows the prevalence of each of the 16 psychiatric disorders, in both the EFA and CFA randomly selected subsamples. Alcohol abuse/dependence, tobacco dependence and major depressive episode were the most common disorders, whereas avoidant, schizoid, antisocial and schizotypal personality disorders were the least common. There were no significant or appreciable differences in the prevalence of disorders across subsamples.
Table 1.
Prevalence of 16 DSM-IV Axis I and Axis II psychiatric disorders across two randomly selected subsamples of the general population
| Prevalence in sample 1a, % (S.E.) (n=17326) | Prevalence in sample 2a, % (S.E.) (n=17327) | χ2 (df=2) | p | |
|---|---|---|---|---|
| Major depressive episode | 22.0 (0.4) | 21.8 (0.5) | 0.1 | 0.77 |
| Dysthymia | 5.1 (0.2) | 5.1 (0.2) | 0.0 | 0.92 |
| Manic episodes | 5.2 (0.2) | 5.3 (0.2) | 0.1 | 0.79 |
| Panic disorder | 7.6 (0.3) | 7.2 (0.3) | 0.9 | 0.35 |
| Social phobia | 7.2 (0.3) | 6.9 (0.3) | 0.9 | 0.35 |
| Specific phobia | 15.3 (0.4) | 15.0 (0.5) | 0.3 | 0.58 |
| Generalized anxiety disorder | 7.7 (0.3) | 7.7 (0.3) | 0.0 | 0.99 |
| Post-traumatic stress disorder | 9.8 (0.3) | 9.2 (0.3) | 2.9 | 0.10 |
| Antisocial personality disorder | 3.7 (0.2) | 4.0 (0.2) | 0.8 | 0.37 |
| Alcohol abuse/dependence | 34.8 (0.8) | 34.3 (0.8) | 0.9 | 0.34 |
| Drug abuse/dependence | 6.2 (0.3) | 6.5 (0.3) | 0.8 | 0.37 |
| Marijuana abuse/dependence | 9.6 (0.4) | 9.7 (0.4) | 0.2 | 0.68 |
| Tobacco dependence | 23.2 (0.6) | 23.0 (0.6) | 0.1 | 0.76 |
| Paranoid personality disorder | 4.3 (0.2) | 4.3 (0.2) | 0.0 | 0.92 |
| Schizotypal personality disorder | 4.0 (0.2) | 3.8 (0.2) | 0.1 | 0.72 |
| Schizoid personality disorder | 3.1 (0.2) | 3.0 (0.2) | 0.1 | 0.71 |
| Avoidant personality disorder | 2.2 (0.1) | 2.4 (0.2) | 1.1 | 0.30 |
S.E., Standard error; df, degrees of freedom.
Sample 1 was used for exploratory factor analysis; sample 2 was used for confirmatory factor analysis.
EFA
In Supplementary Table S1 we show the results of EFAs examining the evidence for unidimensionality of symptoms within each diagnosis for the five psychiatric disorders previously uncharacterized in the meta-structure in these data. Model fit indices indicated that all disorders exhibited unidimensionality. In Supplementary Table S2 we show the tetrachronic correlation matrix for all disorders included in the present investigation.
Table 2 shows the results of a four-factor EFA incorporating all 17 psychiatric diagnoses. Taking into consideration both theoretical meaning and model fit, we judged a four-factor model to best represent the underlying patterns in these data. Model fit for the four-factor structure was excellent (CFI=0.995, TLI=0.991, RMSEA=0.01) and extracted factors characterized clinically meaningful dimensions of psychiatric disorders. Factor structures and model fit statistics for one- through to three-factor and five-factor models are given in Supplementary Table S3. Using model fit alone, a two-factor model provided good fit to these data, but additional factors explained substantial variance and were theoretically meaningful. All factors were significantly (p<0.01) correlated, with the highest correlations between factor 1 and factor 2 (r=0.64), factor 1 and factor 3 (r=0.58), and factor 2 and factor 3 (r=0.54).
Table 2.
Exploratory factor analysis of 16 DSM-IV psychiatric disorders in the general population of the USA (n=17326)
| Four-factor model
|
|||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Major depression | 0.87a | 0.02 | −0.01 | 0.00 | |
| Dysthymia | 0.75a | −0.09 | 0.17 | 0.01 | |
| Manic episodes | 0.37a | 0.14 | 0.33a | 0.17 | |
| Panic disorder | 0.30a | 0.41a | 0.08 | 0.06 | |
| Social phobia | −0.02 | 0.46a | 0.42a | 0.00 | |
| Specific phobia | −0.01 | 0.63a | 0.10 | 0.00 | |
| Generalized anxiety disorder | 0.57a | 0.33a | 0.01 | −0.05 | |
| Post-traumatic stress disorder | 0.40a | 0.37a | −0.05 | 0.01 | |
| Antisocial personality disorder | −0.04 | −0.02 | 0.30a | 0.60a | |
| Alcohol abuse/dependence | −0.05 | −0.01 | −0.01 | 0.79a | |
| Other drug abuse/dependence | 0.04 | 0.02 | 0.10 | 0.79a | |
| Marijuana abuse/dependence | 0.01 | −0.01 | −0.01 | 0.89a | |
| Nicotine dependence | 0.08 | 0.18 | −0.08 | 0.54a | |
| Schizotypal personality disorder | 0.12 | 0.22 | 0.31a | 0.11 | |
| Avoidant personality disorder | 0.06 | 0.19 | 0.71a | −0.09 | |
| Schizoid personality disorder | 0.01 | −0.02 | 0.77a | 0.01 | |
| Paranoid personality disorder | 0.02 | 0.00 | 0.80a | 0.06 | |
| Eigenvalue | 0.83 | ||||
| Comparative fit index | 0.99 | ||||
| Tucker–Lewis index | 0.99 | ||||
| Root mean squared error of approximation | 0.01 | ||||
|
| |||||
| Correlation between factors | 1 | 2 | 3 | 4 | |
|
| |||||
| 1 | 1.00 | ||||
| 2 | 0.64 | 1.00 | |||
| 3 | 0.58 | 0.54 | 1.00 | ||
| 4 | 0.37 | 0.34 | 0.30 | 1.00 | |
Factor loading >0.3.
We highlight the disorders that loaded into each factor with a standardized loading of at least 0.3. These disorders were selected to form each factor of the initial CFA.
CFA
Next, we tested this empirically derived model using CFA. Informed by the good fit statistics of the two-factor EFA model and the high correlation among factors 1, 2 and 3 in the four-factor model, we began by estimating a two-factor model in which factors 1, 2 and 3 were subdimensions of a larger factor. We included all disorders with a standardized factor loading of above 0.300 on a particular factor from the four-factor EFA model. The results of this initial model are in Supplementary Table S4. While this model fit the data well (CFI=0.981, TLI=0.976, RMSEA=0.016), we sought to refine the model for parsimony by removing disorders with low parameter estimates, and used standardized loading values of <0.3 as our cutoff to remove disorders from factors. We removed panic disorder (estimate=0.21) from factor 1, generalized anxiety disorder (estimate=0.23) and PTSD (estimate=0.26) from factor 2, and antisocial personality disorder (estimate=0.27) from factor 3.
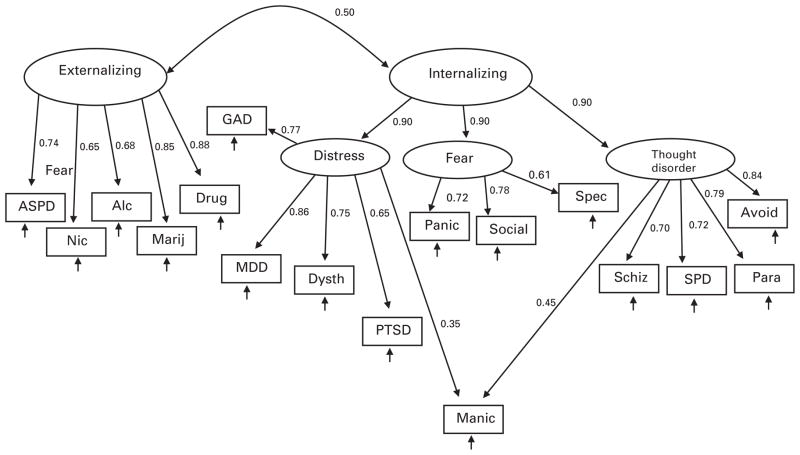
After removing disorders with low standardized loadings, we arrived at a final model. In Fig. 1 we show the structure of our final model in subsample 2 (n=17327). This model provided an excellent fit to the data in the whole subsample 2 (CFI=0.969, TLI=0.964, RMSEA=0.019), as well as among men (CFI=0.978, TLI=0.974, RMSEA=0.016) and women (CFI=0.982, TLI=0.978, RMSEA=0.016) separately. Importantly, we were able to reduce the number of free parameters from 42 in the initial model to 37 in the final model, indicating greater parsimony while maintaining good model fit.
Fig. 1.
Best-fitting model for internalizing, externalizing and thought disorder dimensions of psychopathology among women and men in the USA (n=17 327). Values are standardized factor loadings (all significant, p<0.001). Arrows without numbers indicate unique variances, including error. ASPD, antisocial personality disorder; Nic, nicotine dependence; Alc, alcohol dependence; Marij, marijuana dependence; Drug, other drug dependence; GAD, generalized anxiety disorder; MDD, major depressive disorder; Dysth, dysthymic disorder; PTSD, post-traumatic stress disorder; Panic, panic disorder with or without agoraphobia; Manic, manic episodes; Social, social phobia; Spec, specific phobia; Schiz, schizoid personality disorder; SPD, schizotypal personality disorder; Avoid, avoidant personality disorder; Para, paranoid personality disorder.
As shown in Fig. 1 the ‘internalizing’ factor comprised three subfactors, two of which have been well replicated in previous empirical studies: ‘distress’ (characterized by major depression, dysthymia, manic episodes, generalized anxiety disorder and PTSD), and ‘fear’ (characterized by social phobia, specific phobia, and panic disorder with or without agoraphobia). The third factor was characterized by schizotypal, avoidance, schizoid, and paranoid personality disorders as well as manic episodes; in keeping with prior literature (Markon, 2010; Kotov et al. 2011a) we termed this factor ‘thought disorder’. Finally, the ‘externalizing’ factor was characterized by antisocial personality disorder, alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence and other drug abuse/dependence.
In Fig. 1, we display the path coefficients for the relation of each disorder to the latent dimensions, and the relation of the latent dimensions to each other. The magnitude of these coefficients was similar among both men and women. Correlation between internalizing and externalizing factors was significant (r=0.50, p<0.01). Mania exhibited cross-loading between the ‘thought disorder’ and the ‘distress’ subfactors of ‘internalizing’.
Sensitivity analyses
We conducted two additional analyses to test the robustness of our final model.
First, we removed ‘thought disorder’ from the subdimension of ‘internalizing’ and tested a model in which there were three factors: ‘internalizing’ (with subdomains of ‘distress’ and ‘fear’), ‘externalizing’ and ‘thought disorder’. This model fit the data well (CFI=0.972, TLI=0.967, RMSEA=0.019). However, the free parameters were increased from 37 to 39, indicating less parsimony, and ‘internalizing’ and ‘thought disorder’ were highly correlated (r=0.87); together, these findings reinforced the decision to include ‘thought disorder’ as a subdimension of ‘internalizing’.
Next, we analysed bipolar disorder I or II in place of manic episodes. Bipolar diagnoses were constructed by requiring respondents to have histories of both major depressive episodes and manic episodes. The resulting model is shown in Supplementary Fig. S1, and indicated that bipolar disorder I or II fits the same structure as manic episodes, with cross-loading on both the ‘thought disorder’ and ‘distress’ subfactors of the ‘internalizing’ dimension. Relative to the loading of manic episodes on the ‘distress’ factor (0.35), the loading of bipolar disorder on the ‘distress’ factor (0.44) was higher. Conversely, the loading of bipolar disorder (0.35) on the ‘thought disorder’ factor was lower than the loading of manic episodes (0.45) on the ‘thought disorder’ factor. No loadings of other disorders on factors appreciably changed. This model provided excellent fit to the data (CFI=0.969, TLI=0.963, RMSEA=0.02).
Discussion
The present study adds considerably to our understanding of how co-morbid patterning of psychopathological disorders arise in the context of disorders characterized by detachment and psychoticism. We highlight two novel findings.
First, the primary goal of the present study was to determine whether there was evidence for a dimension of psychopathology characterized by detachment and psychoticism. We document that when suitable indicators are included, this factor emerges. Specifically, in addition to well-established dimensions of internalizing and externalizing disorders, we document an empirically derived psychopathological factor in the general population characterized by schizoid personality disorder, paranoid personality disorder, manic episodes and/or bipolar disorders, and schizotypal personality disorder. This factor was best represented as a subdimension of the internalizing spectrum, correlated highly with disorders characterized by distress and fear, yet emerging as a unique cluster of diagnoses indicative of an additional underlying dimension within the internalizing structure. These findings expand previous structural work indicating that many common, putatively distinct Axis I and Axis II disorders share dimensional underpinnings. Further, these results are similar to findings from two other studies in which a dimension characterized by disordered thought has been demonstrated. Kotov et al. (2011b) identified a dimension characterized by manic episodes, schizotypal personality disorder and schizophrenia spectrum disorders, and Markon (2010), in a symptom-level analysis, identified a thought disorder factor, beyond internalizing and externalizing. Our work adds to a growing literature indicating that the tendency to experience disorders characterized by social isolation, inability to form long-term relationships, and/or psychoticism and other odd behavior represents unique variation within the meta-structure of psychopathology (Markon, 2010; Kotov et al. 2011a, b). We find that these disorders are best represented on a dimension within the internalizing spectrum and distinguishable from externalizing liabilities.
Second, we document that manic episodes and bipolar disorders exhibit notable associations with both the distress subdomain of the internalizing dimension as well as the thought disorder dimension. Mania and bipolar disorders are traditionally categorized as mood disorders due to the substantial dysregulation in affect, yet genetically informative studies also indicate a shared genetic mechanism between bipolar disorder and schizophrenia and other disorders characterized by psychoticism and social isolation (Kendler & Gardner, 1997). Other empirical evidence has supported a reconceptualization of mania and bipolar disorders as highly co-morbid with disorders on the psychosis spectrum (Carpenter et al. 2009; Goldberg et al. 2009; Kotov et al. 2011b). In a proposed change to the nosology of bipolar disorder, the current DSM, fifth edition (DSM-5) proposal moves bipolar and related disorders to an independent category from depressive disorders. Our findings support this notion, providing a potentially novel perspective on the positioning of bipolar disorders, as our results suggest that these disorders are ‘in between’ the distress and thought disorder dimensions. That is, mania and related bipolar disorders may be more accurately conceptualized as belonging simultaneously within two broader spectrums of psychopathology than within a single dimension. Further research is warranted to determine if these findings for mania are replicable.
Third, while our recent data indicated that schizotypal personality disorder is a strong predictor of persistent substance-use disorders in the general population (Hasin et al. 2011), the present investigation does not indicate that this relationship arose due to shared etiology of schizotypal and substanceuse disorders. Substantial evidence indicates that alcohol, nicotine and illicit substances are often used by individuals with schizotypal personality disorder to self-medicate troubling symptoms (Batel, 2000), which could be driving the relationships between schizotypal personality disorder and substance-use disorders.
There is symptomatic overlap in many of the disorders in the thought disorder dimension that probably contribute to the co-morbidity among them. For example, schizoid personality disorder includes the lack of close friends and an interest in solitary activity; similarly, avoidant personality disorder includes being unwilling to get involved with people and inhibited in new interpersonal situations, and schizotypal personality disorder includes lack of close friends and social anxiety as symptoms. Schizoid, avoidant and schizotypal personality disorders are also highly co-morbid with social phobia (Pulay et al. 2009; Kotov et al. 2011a), probably a reflection at least in part of shared symptoms as well. Paranoid personality disorder is characterized by suspicions of criticism and partner fidelity, and, similarly, paranoid ideation is a symptom of schizotypal personality disorder. The similarity in phenotypic presentation across these disorders probably drives, to at least some degree, the co-morbidity across disorders. This is not an issue unique to disorders on the thought disorder dimension; for example, psychomotor agitation and sleep disturbance are symptoms of major depressive episodes as well as manic episodes and generalized anxiety disorder. The symptomatic overlap is probably reflective of these disorders as dimensional liabilities rather than discrete and mutually exclusive categories (Krueger & Markon, 2011, 2012). Dimensional models such as presented here highlight these issues of phenotypic and symptom overlap.
The approach to co-morbidity research executed here, an empirically driven model-based assessment of structure, has yielded substantial insights into the etiology of psychopathology. Factor analyses reveal patterns of co-occurrence that are potentially useful in a number of other clinical and etiological research paradigms. As is increasingly recognized, common risk factors for psychiatric disorders often make an impact on the latent liability to express certain dimensions of psychopathology rather than specific disorders (Kessler et al. 2011; Keyes et al. 2012). Efforts such as the National Institute of Mental Health (NIMH)-led research domain criteria are now underway to develop new representations of psychopathological symptomatology in order to better understand the etiology and pathophysiology of psychiatric disorder without reliance on binary diagnostic indicators (Insel et al. 2010). These findings suggest that the continued search for genetic and other etiological underpinnings of psychiatric disorders could be more fruitfully examined by using a dimensional approach to phenotype definition that accounts for the underlying co-morbidity structure while allowing for clusters of symptoms to form independent liabilities. This approach might help parse dimensions related to fear versus detachment, for example, and characterize the neurobiological underpinnings and psychosocial antecedents of each. However, we note that replication of this model in other data sources is essential to confirming the structure we have empirically derived in the present study. Additionally, validation of the model using external correlates that are specific to disordered thought and detachment versus other dimensions of psychopathology (e.g. specific treatment utilization or medication efficacy) would be beneficial to further characterize and describe these dimensions. This type of data was not available in the present study but should be sought in alternative data sources.
Limitations are noted. Future research in this area should include a greater number of disorders characterized by psychoticism in order to more fully characterize this psychopathological dimension. We note that a previous study using a range of disorder symptoms found that detachment and psychoticism represent two distinct structures; it is possible that with more indicators of these dimensions we would be able to separate factors for these phenomena (Markon, 2010). However, the disorders included in the present study have substantial phenotypic overlap with schizophrenia and other disorders with psychotic features, and the literature has documented the comorbidity among disorders such as schizotypal and schizoid personality disorders with schizophrenia (Cohen et al. 2010). A recent study of psychiatric out-patients found that psychosis is also a manifestation of a latent distribution that is characterized by many of the same disorders documented here, including schizoid, paranoid and schizotypal personality disorder as well as mania (Kotov et al. 2011b). Nevertheless, feasibility constraints in conjunction with low estimated general population prevalence precluded a full assessment of schizophrenia in the NESARC, and we were therefore unable to include schizophrenia in our assessment of psychoticism. We also note that the NESARC survey assessed some personality disorders that were not included in the present model as they were not relevant to the empirical demonstration of a dimension characterized by social detachment and/or psychoticism (e.g. narcissistic personality disorder). Using the knowledge gained by the present study, future work will establish the broader meta-structure including these and other disorders. Further, we note that schizotypal personality disorder was assessed at wave 2 only, while the other personality disorders were assessed at wave 1 only. While we cannot directly assess the effect of measurement wave on our results, we note that schizotypal personality disorders exhibited similar loadings to other personality disorders on the thought disorder dimension in the final CFA model, indicating a high correlation with other disorders measuring the same underlying dimension regardless of the wave in which the disorder was assessed. Finally, we note that this dimensional model of DSM-derived psychiatric disorders does not account for the substantial heterogeneity of clinical presentation within diagnostic categories. However, this is a broader issue with categorical diagnoses in general, since individuals within a diagnostic category can manifest a range of clinically meaningful and heterogeneous phenotypes. Future research using symptoms rather than diagnoses may be helpful.
The present study is also characterized by several substantial strengths. In a nationally representative sample of adults, we document the structure of 16 DSM-IV Axis I and Axis II disorders, indicating that disorders characterized by detachment and psychoticism should be conceptualized, organized and measured as a subdimension of the internalizing spectrum of disorders, with strong clinical, etiological and structural links between manic episodes and bipolar disorder across psychopathological dimensions within the internalizing spectrum. Given the large sample size, we were able to estimate the structure in one half of the sample and conduct validation analyses in a randomly selected second half, an important strength of the present work. These results should be incorporated into etiological studies in order to identify potentially important risk factors, and should be considered in the development of new classifications of psychiatric disorders. Further, these results underscore the importance of clinical assessment and treatment protocols that focus on a comprehensive review of major areas of psychopathological variation, to better conceptualize patients that may have comorbid problems in multiple domains.
Supplementary Material
Acknowledgments
This research was supported in part by grants from the National Institute on Alcoholism and Alcohol Abuse (no. K05 AA014223 and U01 AA018111, both to D.S.H.), and support from the New York State Psychiatric Institute.
Footnotes
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291712002292.
Declaration of Interest
None.
References
- Barlow D, Farchione T, Fairholme C, Ellard K, Boisseau C, Allen L, Ehrenreich-May J. Unified Protcol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. Oxford University Press; New York: 2011. [Google Scholar]
- Batel P. Addiction and schizophrenia. European Psychiatry. 2000;15:115–122. doi: 10.1016/s0924-9338(00)00203-0. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Bustillo JR, Thaker GK, van Os J, Krueger RF, Green MJ. The psychoses: cluster 3 of the proposed meta-structure for DSM-V and ICD-11. Psychological Medicine. 2009;39:2025–2042. doi: 10.1017/S0033291709990286. [DOI] [PubMed] [Google Scholar]
- Cohen AS, Emmerson LC, Mann MC, Forbes CB, Blanchard JJ. Schizotypal, schizoid and paranoid characteristics in the biological parents of social anhedonics. Psychiatry Research. 2010;178:79–83. doi: 10.1016/j.psychres.2008.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, Grant BF, Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. Journal of Abnormal Psychology. 2012;121:282–288. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: relationship to the internalizing–externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychological Medicine. 2012 doi: 10.1017/S0033291712001092. Published online 21 May 2012. [DOI] [PubMed] [Google Scholar]
- Goldberg DP, Andrews G, Hobbs MJ. Where should bipolar disorder appear in the meta-structure ? Psychological Medicine. 2009;39:2071–2081. doi: 10.1017/S0033291709990304. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Fenton MC, Skodol A, Krueger R, Keyes K, Geier T, Greenstein E, Blanco C, Grant B. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Archives of General Psychiatry. 2011;68:1158–1167. doi: 10.1001/archgenpsychiatry.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, McGue M. Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: a longitudinal twin study. Journal of Abnormal Psychology. 2007;116:433–447. doi: 10.1037/0021-843X.116.3.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO. The risk for psychiatric disorders in relatives of schizophrenic and control probands: a comparison of three independent studies. Psychological Medicine. 1997;27:411–419. doi: 10.1017/s003329179600445x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, McGuire M, Gruenberg AM, O’Hare A, Spellman M, Walsh D. The Roscommon Family Study. III. Schizophrenia-related personality disorders in relatives. Archives of General Psychiatry. 1993;50:781–788. doi: 10.1001/archpsyc.1993.01820220033004. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Walsh D. Evaluating the spectrum concept of schizophrenia in the Roscommon Family Study. American Journal of Psychiatry. 1995;152:749–754. doi: 10.1176/ajp.152.5.749. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu C, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustun TB. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Archives of General Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, Hasin D. Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Chang SW, Fochtmann LJ, Mojtabai R, Carlson GA, Sedler MJ, Bromet EJ. Schizophrenia in the internalizing–externalizing framework: a third dimension? Schizophrenia Bulletin. 2011a;37:1168–1178. doi: 10.1093/schbul/sbq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011b;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal–epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: progress and opportunities. Archives of General Psychiatry. 2011;68:10–11. doi: 10.1001/archgenpsychiatry.2010.188. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Toward a clinically useful and empirically based dimensional model of psychopathology. World Psychiatry. 2012;11:23–24. doi: 10.1016/j.wpsyc.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein P, Yip BH, Bjork C, Pawitan Y, Cannon TD, Sullivan PF, Hultman CM. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet. 2009;373:234–239. doi: 10.1016/S0140-6736(09)60072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BL. MPlus User’s Guide. 5. Muthén and Muthén; Los Angeles: 2010. [Google Scholar]
- Pulay AJ, Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Saha TD, Smith SM, Pickering RP, Ruan WJ, Hasin DS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2009;11:53–67. doi: 10.4088/pcc.08m00679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verona E, Sachs-Ericsson N, Joiner TE., Jr Suicide attempts associated with externalizing psychopathology in an epidemiological sample. American Journal of Psychiatry. 2004;161:444–451. doi: 10.1176/appi.ajp.161.3.444. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Wolf AW, Schubert DS, Patterson MB, Grande TP, Brocco KJ, Pendleton L. Associations among major psychiatric diagnoses. Journal of Consulting and Clinical Psychology. 1988;56:292–294. doi: 10.1037//0022-006x.56.2.292. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the genetic structure of comorbidity. Journal of Abnormal Psychology. 2010;119:320–330. doi: 10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.