Abstract
Health literacy represents the communication among patients, their social networks, providers, and health systems to promote patients’ understanding and engagement in their care. This is particularly relevant in kidney disease, in which the complexity of the medical condition and the extent of the health-care team require strategies to overcome health-literacy-related barriers. Limited literacy is common in patients with all stages of kidney disease and is associated with important outcomes, including reduced knowledge, less adherence, hospitalization, and death. A growing understanding and characterization of the health system, or organizational health literacy, may further our understanding of this dynamic relationship. Although various valid methods exist, assessment of health literacy within individuals or systematically within care settings has not been routinely performed. This may be in part due to the limited research in kidney-specific strategies to address limited health literacy. Future research to understand the mechanisms of health literacy will permit targeted, efficient interventions to bridge gaps and improve outcomes even in patients with complex kidney disease.
Keywords: Health literacy, Communication, ESRD, Transplantation, Education
The epidemic of kidney disease, which affects 26 million people in the United States and 600 million worldwide, continues to grow in parallel to other related chronic conditions, such as diabetes, hypertension, and obesity.1,2 Despite available established therapies to prevent progression of CKD and to manage its related conditions or complications, execution of these recommended treatments even in large integrated health systems is often unsatisfactory.3 Although many factors contribute to this suboptimal delivery and coordination of kidney disease care, it is fundamentally the patient who is tasked daily with understanding, implementing, and maintaining clinical recommendations for kidney-related self-care. Even with concerted multidisciplinary efforts, participation in self-management behaviors including adherence with complex medication schedules, dietary recommendations, management of co-morbid conditions, and preparation for renal replacement therapies is poor.4 Identifying and addressing specific barriers to this process are critical opportunities to improve CKD quality of care.
Over the past 2 decades, health literacy has been increasingly recognized as an important influence on the exchange and application of information among patients, their social networks, providers, and health systems. Consistent associations have been found among low health literacy and less preventive health behaviors, more hospitalizations, and a higher risk of mortality.5 In the United States, it is estimated that 90 million people have basic or below-basic literacy skills, and more than 110 million people have poor mathematical skills.6 Low health literacy is common and disproportionately affects those who are older, those with lower socioeconomic resources, and those with lower educational attainment.7 Thus, patients at higher risk for the development or progression of CKD may also be at higher risk for challenges engaging their health care. Interventions to address low health literacy in other conditions such as diabetes and heart failure have demonstrated improvements in patient’s knowledge, self-efficacy, behaviors, and clinical status,8 supporting health literacy as a potential target for care improvement in other related chronic conditions, including kidney disease.
In this review, we aim to define health literacy and describe available assessment measures. We also will examine the current research representing the understanding of health literacy among patients with CKD, ESRD, and kidney transplant. Finally, we will provide considerations for addressing low health literacy in clinical practice as well as future research.
What Is Health Literacy and How Do I Assess It?
Definition
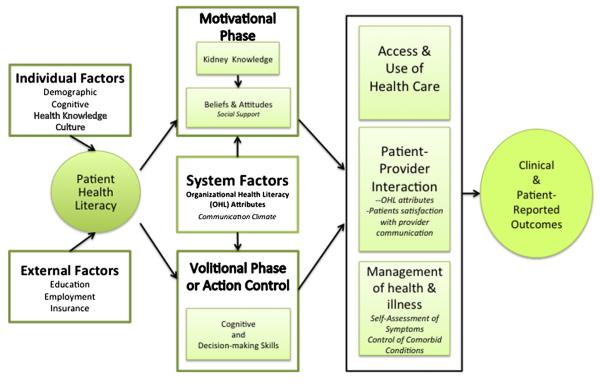
Health literacy is a comprehensive concept representing the diverse communication skills of individuals that are fundamental to optimizing interactions within the broader system of health care. These skills are more than reading and writing (print literacy), but also include listening and speaking (oral literacy), numeracy, as well as cultural and conceptual knowledge (Fig 1).9 The proposed definitions have evolved over time as the understanding of the role of health literacy in care itself has matured. A recent adaptation of the Institute of Medicine definition, “the degree to which individuals can obtain, process, understand, and communicate about health-related information needed to make informed health decisions”,10 emphasizes the critical dynamic aspect of the act of individuals not only consuming information but also transmitting it to close gaps in understanding. Organizations can also be characterized as being health literate when they systematically demonstrate complementary attributes such as integration of health literacy into their mission and daily operations, their commitment to ascertain and meet the needs of all of those served, and when they include ongoing strategies to ensure effective communication.11 Future definitions of health literacy may be even more explicit in this shared responsibility among patients, providers, organizations, and our community.
Figure 1.
Components of literacy. Adapted with permission from the National Academies Press.9
Understanding quantitative information is essential for establishing the presence and severity of and monitoring the status of kidney disease. Health numeracy, often considered a component of health literacy, is “the degree that individuals can apply numerical, graphical, and statistical skills to understand and act on health information needed to make effective health decisions.”12 Although health literacy and numeracy are similar, they are not perfectly correlated, and patients with adequate health literacy can have difficulty with numeracy-related tasks.13 The independent contributions of numeracy and health literacy in chronic disease care are active areas of research.
Assessment
There are various instruments that have been developed to evaluate health literacy, and they are primarily intended for use in a research setting. These include objective and subjective assessments as well as those in which the purpose is to screen for more severe skill deficits. Despite the acknowledged array of skills that constitute health literacy, the instruments used most widely focus on reading skills. Evaluation of numeracy requires administration of additional instruments. We will briefly review those most commonly used and highlight those reported among patients with kidney disease (Table 1). Additional detail regarding the performance of the health literacy measures is available elsewhere.14
Table 1.
Health Literacy Assessment Characteristics
| Measure | Objective(s) | Item Description | Items | Proctor | Time (min) |
Language | Score Range and Categories |
Brief Notes | References |
|---|---|---|---|---|---|---|---|---|---|
| Rapid Estimate of Adult Literacy in Medicine (REALM) |
Health literacy | Test of accuracy pronouncing medical terms |
66 | Yes | 3-5 | English | 0-66 0-18 ≤ 3rd grade 19-44 4th to 6th grade 45-60 7th to 8th grade 61-66 ≥ 9th grade |
-Commonly used -11-item version -Possible ceiling effect |
15 |
| Test of Functional Health Literacy in Adults (TOFHLA) |
Health literacy Numeracy |
Missing every 5th or 7th word Cloze procedure |
50 19 |
Yes | 12 10 |
English Spanish |
0-100 0-59 Inadequate 60-74 Marginal 75-100 Adequate |
-Less commonly used likely because of survey burden -Few studies using the numeracy items |
18 |
| Short Test of Functional Health Literacy in Adults (S-TOFHLA) |
Health literacy Numeracy |
Missing every 5th or 7th word Cloze procedure |
36 4 |
Yes | 7 | English Spanish |
0-36 0-16 Inadequate 17-22 Marginal 23-36 Adequate |
-Commonly used -Numeracy items usually not administered |
19 |
| Short Literacy Survey (SLS) |
Health literacy Screen |
Confidence in using health materials |
3 | Yes | 3-5 | English Spanish |
3-15 | -Brief, enhances ease of use - Validated as oral administration only to date |
24,25 |
| Single Item Screener | Health literacy Screen |
One question asking about help with written health materials |
1 | No | 1-2 | English Spanish |
1-5 3-5 lower literacy |
- Unclear strength of relationship with outcomes - Consider as screening item if very limited resources |
27 |
| REALM-T | Transplant health literacy |
Transplant-related medical terms |
69 | Yes | 3-5 | English Spanish |
0-69 Number of words correct |
- Related to the specific health situation - Brief - Limited studies |
17 |
| Newest Vital Sign | Health literacy Numeracy |
Questions about a nutrition food label including prose and numeracy |
6 | Yes | 5-10 | English Spanish |
0-6 0-1 Probable limited literacy 2-3 Possible limited literacy 4-6 Adequate |
- Brief - Applied in a health setting using a food label prompt - Less support for associations with clinical outcomes compared with other tools |
22 |
| Health Literacy Skills Instrument |
Applied health literacy |
Health context multiple- choice questions covering print and oral literacy, numeracy, and internet navigation |
10 | No | 10-15 | English | 0-100% | -Applied skills in different literacy domains - Can be self- administered or computer assisted - Limited information about associations with outcomes at this time |
21 |
| Wide Range Achievement Test-4 (WRAT) |
Objective math | Traditional timed computational math test |
40 | Yes | 15 | N/A | Age-standardized scores available to equate to a grade level |
- Also reading test available - May induce anxiety |
28 |
| Lipkus Numeracy Scale | Risk numeracy | Operational exercises focusing on probability, including multiple choice |
7 | No | 5-10 | English | 0-7 | - Limited to a specific domain of numeracy - Identifies those at risk of lower numeracy - Associations with outcomes in various health conditions |
29 |
| Subjective Numeracy Scale |
Numeracy | Subjective questions about use and confidence working with numbers |
8 | No | 8-10 | English | 1-6 | - Subjective and complements brief health literacy items - Growing research demonstrating associations with outcomes |
30 |
Abbreviation: N/A, not applicable.
The Rapid Estimate of Adult Literacy in Medicine (REALM), a brief 3-minute test, was one of the first measures of health literacy and remains one of the most common. It is a list of 66 words read aloud by participants and assessed by pronunciation accuracy.15 An 8-word version was developed, but it has had limited use.16 A kidney transplant version, the REALM-T, is composed of 69 transplant-specific words and was validated in one study to describe the health literacy of kidney transplant recipients.17
The Test of Functional Health Literacy in Adults (TOFHLA) is another commonly used measure of health literacy and uses a modified Cloze procedure in which reading passages about medical information are missing every 5th to 7th word.18 This type of test relies on the participant’s understanding of vocabulary and the context in which it is used to choose the correct replacement word. Participants are required to select the correct word for each of the passages and are given 12 minutes to complete 50 items. This version also includes 17 task-oriented numeracy items. More often implemented is the shortened form, or S-TOFHLA, consisting of 36 items and allowing a maximum of 7 minutes to complete.19 Although 4 numeracy items were originally included in the S-TOFHLA, many studies do not include them, and there is also evidence that they do not additionally contribute to associations between health literacy and other factors.20 Spanish versions have also been validated for use.
The Health Literacy Skills Instrument is a new survey with multiple-choice items evaluating an individual’s print and oral literacy, numeracy, and web-based navigation proficiency.21 Subjects are presented a stimulus that represents health information that may be encountered in daily life, and they are then asked to interpret and respond according to a theory-based framework of skills. There is little experience describing this new measure and its associations with clinical outcomes, but given that its applied content is substantially different from previous health literacy assessments, comparisons of its performance will be very informative.
Health literacy measures have commonly been administered for research purposes, but with the increasing recognition of the effect of limited literacy on clinical outcomes, there is increasing focus on screening in a clinical setting. The time and training of personnel to perform the assessment can be a barrier to administration. Thus, recently developed measures focus on brevity and potential utility in various clinical settings.
The Newest Vital Sign is a 6-question measure that can be administered in English or Spanish and is based on the interpretation of a nutrition label.22 It is a brief instrument requiring only 3 to 5 minutes. However, its performance demonstrates a tendency to overestimate limited literacy in patient populations and is one factor contributing to its limited use in research.23
Evidence is growing that brief, subjective health literacy screening (Short Literacy Survey [SLS]) items (1) “How often do you have someone help you read hospital materials?”, (2) ”How confident are you filling out medical forms by yourself?”, and (3) ”How often do you have problems learning about your medical condition because of difficulty understanding written information?” are associated with valid measures of health literacy24 and prospectively relate to important health outcomes such as mortality and hospitalizations.25 The SLS has also been validated in Spanish.26 These 3 items have been adapted and reduced even further to the Single Item Literacy Screener scale, “How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?”, and was sensitive and specific for identifying limited literacy.27
Assessment of health numeracy also includes objective and subjective measures. The Wide Range Achievement Test-428 and the Lipkus Numeracy Scale29 test arithmetic ability, but they may be intimidating for respondents. In contrast, the subjective scales of numeracy do not test the actual ability to perform mathematical computations, but instead they ask participants about their confidence, or perceived ability, of working with quantitative information. The Subjective Numeracy Scale includes 8 questions answered on a 6-point Likert Scale.30
There are several limitations of the literacy and numeracy assessments that must be taken into consideration when interpreting results or integrating these measures into research or practice. The REALM and the TOFHLA require staff to either directly administer the test or to ensure that the allocated time is not violated. This may not transfer easily to settings with limited staffing resources. Although the REALM and TOFHLA can identify patients who have significant health literacy deficits, there is less variation at the upper end of the scoring range, suggesting a possible ceiling effect. The current measures do not assess other potentially important components of health literacy, such as verbal literacy, technology and communication skills, and learning style. Although international health literacy research is increasing, few validated tools are available in languages other than English and Spanish.23,31,32
More importantly, it is critical to acknowledge that many patients with limited literacy and numeracy skills experience shame or embarrassment when they are evaluated in these domains.33,34 In one small study, most patients with limited literacy reported that it would be helpful for the physician or nurse to know that they had difficulty reading; however, the act of informing the provider and recording it in the medical record would cause them to feel ashamed.35 These concerns may be addressed within an organization by educating providers about the importance of health literacy screening and training providers in patient-centered clear communication to promote effective conversations in all patients.36 Promoting these strategies may be a characteristic found within a health-literate organization.
Organizational health literacy is increasingly recognized as an important factor to engage patients, and measures endorsed by the National Quality Forum are available to assess the practices of health systems. Recently, the Institute of Medicine Roundtable on Health Literacy described 10 attributes of a health-literate organization representing, in part, organizational commitment, infrastructure to support accessible technology, training of the workforce, and inclusion of health literacy in policies and practices, all to support effective communication.37 Tools to perform an environmental assessment of health literacy,38 or an assessment of the communication climate,39 are available and represent various views from stakeholders in the health systems, including administrators, providers, and patients.
Why Is Health Literacy Important in Kidney Disease Care?
Conceptual Model
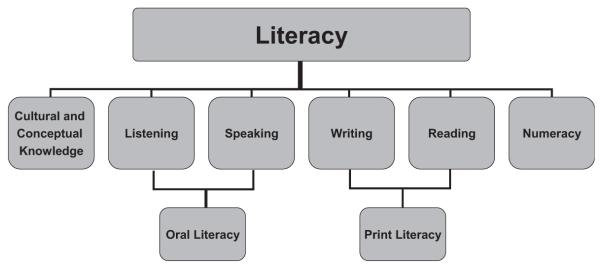
Various conceptual models to depict the role of health literacy and patient outcomes have been proposed,40 including one within the context of kidney disease.41 The ongoing treatment of kidney disease to prevent its development, progression, and ultimately to optimize care in the setting of end-stage kidney disease (ESKD) requires detailed intensive coordination of the patient, their social network, their health providers, and the health system. Thus, we propose considering a model demonstrating an integrated framework of health literacy and health action that includes patient- and system-level factors as determinants of patients’ motives, behaviors, and ultimately health outcomes to comprehensively describe the complexity of kidney care.42-43a (Fig 2) This view suggests that individual and organizational health literacy contribute to a patient’s knowledge of his/her condition, to attitudes about its importance, to engaged social supports, and to decision-making skills to influence health actions such as access and use of care, the effectiveness of patient-provider interactions, and finally self-care behaviors. Initial studies in kidney disease provide support for this approach.
Figure 2.
Integrated conceptual model of health literacy.43a
CKD and ESKD
Health literacy has a potential role in all aspects of kidney disease care; however, there remains a poor understanding and low concern about kidney disease among those at risk or with diagnosed CKD. In 195 participants with hypertension, all at least at risk of future development of CKD were asked how concerned they were about developing kidney disease over the next 10 years.44 Among those with adequate health literacy, 21% were not concerned, compared with 85% among those with the lowest health literacy.44 Poor understanding of kidney disease may be contributing to its low observed importance.
Available research of health literacy in patients with nondialysis-dependent CKD is limited to a single cohort from one academic medical center.45,46 In almost 400 patients with established CKD under the care of a nephrologist, the prevalence of limited health literacy was 19%. Objective kidney knowledge was independently associated with health literacy, but perceived kidney knowledge was not significantly related. There are currently no reports examining health literacy and clinical outcomes in CKD.
More research has evaluated health literacy in dialysis patients, with a total of 8 patient groups. Two studies describe the prevalence of limited health literacy as 5% to 50% among a total of 32 peritoneal dialysis patients.47,48 In hemodialysis, the largest study of 480 participants found 32% with limited literacy,49 similar to other studies, although these range from 16% to 50%.48,50-53 Limited health literacy is consistently associated with fewer years of education, non-White race, and male gender.49,52 The disparities observed in these vulnerable populations may be explained in part to differences in health literacy, as seen with diabetes and numeracy.54
In a 2-year prospective cohort of 480 incident hemodialysis patients, limited health literacy was associated with a 50% greater risk of mortality, even after adjustment for age, gender, race, diabetes, and serum albumin.49 Limited health literacy has been found in other samples to be associated with higher average blood pressure,53 more missed dialysis treatments, and more frequent use of emergency room services.55 In addition, those with limited literacy were more likely to have ESKD-related hospitalizations with an adjusted incidence rate ratio of 1.55 (1.03-2.34; P = .04).55 Other determinants along the causal pathway remain to be determined.
Understanding kidney disease requires patients to interpret, apply, and use quantitative information especially as it relates to fundamental laboratory assessments. However, only 1 study to date reports an assessment of numeracy among patients with kidney disease. Using the 3-item probability-based numeracy scale administered to 75 advanced CKD patients and 112 dialysis patients, numeracy was systematically poor.56 No association was observed with type of vascular access; however, those with higher numeracy scores were more likely to be waitlisted or receive a kidney transplant. In addition, numeracy performance correlated highly with other tests of cognitive function.56
Kidney Transplant
Kidney transplantation is the optimal therapy for those who are medically eligible among those with advanced CKD or ESKD. The evaluation process requires intensive patient engagement, posing a challenge for even the most skilled. Although the concepts of health literacy are pertinent to kidney transplant candidates and recipients, the literature characterizing health literacy of the kidney-transplant-specific patient population is limited.41
In a small study of 62 prevalent dialysis patients, 32% of patients had inadequate health literacy and in adjusted analyses had a 78% less likelihood of referral for kidney transplantation.51 A second single-center cross-sectional study of 124 kidney transplant recipients found that only 9% had limited health literacy. In this same study, a transplant-specific health literacy measure was evaluated, REALM-T.17 The results of the REALM-T, but not the S-TOFHLA, improved with increased time posttrans-plant. Transplant knowledge was not associated with health literacy in this study, but power to evaluate this may have been limited.17 In 44 kidney transplant clinic participants, health literacy was assessed using the Newest Vital Sign and found 41% with limited health literacy.57 This escalated to 89% among Spanish-speaking participants. Finally, in another small pilot study of 36 patients, the numeracy items from the TOFHLA were administered without the literacy items and 72% were reported to have poor numeracy scores.58
Social support is critical to successful kidney transplantation. Patients with limited social support may be ineligible for transplantation because the caregiver is expected to assist as a member of the health team to facilitate self-care and effective health actions. In nontransplant patients, limited health literacy of caregivers has been associated with uncertainty in medication administration, dosing errors, and poor health outcomes.59-61 Therefore, the health literacy of caregivers should also be considered when assessing factors influencing transplant care.
Strategies to Address Health Literacy in Kidney Disease
Interventions designed to address patients with low health literacy and numeracy have led to improvement in patient outcomes. Between 2003 and 2011, over 42 intervention studies describing health literacy or numeracy interventions have been published.62 Successful interventions often not only target health literacy but also address moderators for health literacy, such as costs and accessibility to care. Interventions have also been designed to increase a sense of self-efficacy, decrease use of health-care services and costs, modify health behaviors, and improve quality of life.8,62
Educational materials that can be used cooperatively by providers and patients may improve the effectiveness of information delivery and enhance opportunities for goal-setting and shared decision-making. For example, the Diabetes Literacy and Numeracy Education Toolkit is a set of 24 modules written at a 6th-grade reading level with illustrations; it is used to aid in diabetes education.63 The effect of the Diabetes Literacy and Numeracy Education Toolkit modules on glycemic control were tested in a randomized control trial at 2 centers. At both study sites, patients in the intervention group had a significant decrease in hemoglobin A1C at 3 months compared with patients in the control group; however, this did not persist at the 6-month follow-up.64
Information technology solutions for education and communication are appealing because of their brevity and their ease of use for most. Examples of applications for mobile devices include programs that assist the user in tracking their diet and making changes. One application allows for touch-screen icons, barcode scanning, and voice recording assisting patients with limited literacy. Patients using this device reported a change in their dietary habits, and plans for development of a smartphone application are in place.65 However, there remains a digital divide in which some patients are much less likely to use technology, including older, less advantaged, and at times lower literacy patients. Low health literacy has been associated with less frequent use of a computer to research medications and health conditions in diabetic patients.66 As our interactions evolve, it will be important to preserve patient-centered forms of communication in all forms of traditional and nontraditional health encounters.
Several groups have developed interventions to address limited health literacy in patients with kidney disease. Although some patients turn to the internet to learn about kidney disease, the level of available material is often written above the recommended 5th-grade reading level, making it inaccessible to patients with limited literacy.67 Developing literacy-sensitive tools to aid patients in education and health-monitoring is necessary because patients may not understand the information they may find online or lack access to the internet. Although some of the current interventions are internet based, many focus on evaluating the patients’ current knowledge and performing literacy-sensitive, in-person teaching to improve knowledge and outcomes. For advanced kidney disease this may be supported by Medicare as a clinical service.68
One example of an effort to overcome disparities in the rates of preemptive and early kidney transplant is the Talking About Live Kidney Donation study. This program includes a low-literacy education and social-work-based intervention to increase knowledge of living kidney donation, especially preemptive living kidney transplantation.69 Patients in the intervention group either received a video and booklet or had patient and family social work visits in addition to the educational video and booklet. Both interventions improved the participants’ pursuit of preemptive living-donor kidney transplantation. Although the study was designed to reach low-literacy patients, the actual skills of the enrolled participants were more advanced. The effect of the intervention stratified by literacy level was not reported.69 Future opportunities exist to apply this type of literacy-sensitive intervention to a more diverse group of patients to determine its value.
Summary
Our understanding of the role of health literacy in kidney disease is just beginning. A greater number of patients are assessed, permitting more detailed and comprehensive evaluations of the factors associated with risk of limited literacy, associations with social determinants, and important clinical outcomes. Through additional collaboration and research the influential modifiable practices of patients and health systems will advance our care. Measures to assess health literacy are available; however, most have been applied in research settings. The short subjective measures show promise to characterize patients at highest risk and may be a consideration even in busy clinical settings. Finally, our strategies to address health literacy in kidney disease remain equally undeveloped because of limited research in the area. Health literacy has influenced the fundamental care of complex conditions such as diabetes, heart failure, and HIV. We anticipate the same effect will ultimately be revealed for the care of patients with kidney disease.
CLINICAL SUMMARY.
Limited health literacy is common, observed in 10% to 50% of patients with kidney disease, and it is associated with kidney knowledge, adherence, hospitalizations, and death.
Organizational health literacy may be an important factor in understanding and addressing barriers to effective kidney care.
Brief subjective assessments of health literacy show promise for use in clinical settings and large cohort studies.
Few studies examine the effect of interventions to address health literacy in kidney disease.
Acknowledgment
Dr. K. Cavanaugh is supported by grants form the National Institutes of Health (K23DK080952) and the American Society of Nephrology Carl W. Gottschalk Research Scholar Grant.
Footnotes
The authors have no financial conflicts of interest to disclose.
References
- 1.Szczech LA, Harmon W, Hostetter TH, et al. World Kidney Day 2009: problems and challenges in the emerging epidemic of kidney disease. J Am Soc Nephrol. 2009;20(3):453–455. doi: 10.1681/ASN.2009010041. [DOI] [PubMed] [Google Scholar]
- 2.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80(12):1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 3.Rutkowski M, Mann W, Derose S, et al. Implementing KDOQI CKD definition and staging guidelines in Southern California Kaiser Permanente. Am J Kidney Dis. 2009;53(3 suppl 3):S86–S99. doi: 10.1053/j.ajkd.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 4.Curtin RB, Walters BA, Schatell D, Pennell P, Wise M, Klicko K. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis. 2008;15(2):191–205. doi: 10.1053/j.ackd.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 6.Kuntner M, Greenberg E, Baer J. A First Look at the Literacy of America’s Adults in the 21st Century. National Center for Education Statistics; Jessup, MD: 2005. NCES publication no. 2006470. [Google Scholar]
- 7.Kutner M, Greenberg E, Jin Y, Paulsen C. [Accessed December 5, 2012];The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy (NCES 2006-483) Available at: http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483.
- 8.Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(suppl 3):30–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- 9.Nielsen-Bohlman L, Panzer A, Kindig D. Health Literacy: a Prescription to End Confusion. National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- 10.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(suppl 2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine . How Can Health Care Organizations Become More Health Literate?: Workshop Summary. National Academies Press; Washington, DC: 2012. [PubMed] [Google Scholar]
- 12.Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med. 2005;29(4):375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 13.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 14.Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304(1):76–84. doi: 10.1001/jama.2010.896. [DOI] [PubMed] [Google Scholar]
- 15.Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23(6):433–435. [PubMed] [Google Scholar]
- 16.Bass PF, III, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18(12):1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon EJ, Wolf MS. Health literacy skills of kidney transplant recipients. Prog Transplant. 2009;19(1):25–34. doi: 10.1177/152692480901900104. [DOI] [PubMed] [Google Scholar]
- 18.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 19.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 20.Baker DW, Wolf MS, Feinglass J, Thompson JA. Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med. 2008;23(6):723–726. doi: 10.1007/s11606-008-0566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bann CM, McCormack LA, Berkman ND, Squiers LB. The Health Literacy Skills Instrument: a 10-item short form. J Health Commun. 2012;17(suppl 3):191–202. doi: 10.1080/10810730.2012.718042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mancuso JM. Assessment and measurement of health literacy: an integrative review of the literature. Nurs Health Sci. 2009;11(1):77–89. doi: 10.1111/j.1442-2018.2008.00408.x. [DOI] [PubMed] [Google Scholar]
- 24.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 25.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26(3):265–271. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7:21. doi: 10.1186/1471-2296-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilkinson GS, Robertson GJ. Wide Range Achievement Test 4 (WRAT 4) Psychological Assessment Resources; Lutz, FL: 2006. [Google Scholar]
- 29.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 30.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 31.Al Sayah F, Williams B, Johnson JA. Measuring health literacy in individuals with diabetes: a systematic review and evaluation of available measures. Health Educ Behav. 2013;40(1):42–55. doi: 10.1177/1090198111436341. [DOI] [PubMed] [Google Scholar]
- 32.Jordan JE, Osborne RH, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J Clin Epidemiol. 2011;64(4):366–379. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 33.Elson PR. Literacy and health. CMAJ. 1993;149(10):1379, 1382. [PMC free article] [PubMed] [Google Scholar]
- 34.Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Educ Couns. 1996;27(1):33–39. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 35.Wolf MS, Williams MV, Parker RM, Parikh NS, Nowlan AW, Baker DW. Patients’ shame and attitudes toward discussing the results of literacy screening. J Health Commun. 2007;12(8):721–732. doi: 10.1080/10810730701672173. [DOI] [PubMed] [Google Scholar]
- 36.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21(8):888–890. doi: 10.1111/j.1525-1497.2006.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brach C, Dreyer B, Schyve P, et al. [Accessed September 25, 2012];Attributes of a health literate organization. IOM Roundtable on Health Literacy Discussion Paper. Available at: http://www.iom.edu/Activities/PublicHealth/~/media/Files/Activity Files/PublicHealth/HealthLiteracy/10attributes.pdf.
- 38.Health Literacy Universal Precautions Toolkit. Agency for Healthcare Research and Quality; Rockville, MD: [Accessed September 25, 2012]. 2010. AHRQ Publication No. 10-0046-EF. Available at: http://www.ahrq.gov/qual/literacy/index.html. [Google Scholar]
- 39.Wynia MK, Johnson M, McCoy TP, Griffin LP, Osborn CY. Validation of an organizational communication climate assessment toolkit. Am J Med Qual. 2010;25(6):436–443. doi: 10.1177/1062860610368428. [DOI] [PubMed] [Google Scholar]
- 40.Sorensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Devraj R, Gordon EJ. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis. 2009;53(5):884–889. doi: 10.1053/j.ajkd.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 42.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 43.von Wagner C, Steptoe A, Wolf MS, Wardle J. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav. 2009;36(5):860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 43a.Fransen MP, von Wagner C, Essink-Bot ML. Diabetes self-management in patients with low health literacy: Ordering findings from literature in a health literacy framework. Patient Educ Couns. 2012;88(1):44–53. doi: 10.1016/j.pec.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 44.Boulware LE, Carson KA, Troll MU, Powe NR, Cooper LA. Perceived susceptibility to chronic kidney disease among high-risk patients seen in primary care practices. J Gen Intern Med. 2009;24(10):1123–1129. doi: 10.1007/s11606-009-1086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL. Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis. 2011;57(3):387–395. doi: 10.1053/j.ajkd.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int. 2011;80(12):1344–1351. doi: 10.1038/ki.2011.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kleinpeter MA. Health literacy affects peritoneal dialysis performance and outcomes. Adv Perit Dial. 2003;19:115–119. [PubMed] [Google Scholar]
- 48.Pollock JB, Jaffery JB. Knowledge of phosphorus compared with other nutrients in maintenance dialysis patients. J Ren Nutr. 2007;17(5):323–328. doi: 10.1053/j.jrn.2007.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cavanaugh KL, Wingard RL, Hakim RM, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21(11):1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Foster M, Brice JH, Shofer F, et al. Personal disaster preparedness of dialysis patients in North Carolina. Clin J Am Soc Nephrol. 2011;6(10):2478–2484. doi: 10.2215/CJN.03590411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol. 2009;4(1):195–200. doi: 10.2215/CJN.03290708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Green JA, Mor MK, Shields AM, et al. Prevalence and demographic and clinical associations of health literacy in patients on maintenance hemodialysis. Clin J Am Soc Nephrol. 2011;6(6):1354–1360. doi: 10.2215/CJN.09761110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adeseun GA, Bonney CC, Rosas SE. Health literacy associated with blood pressure but not other cardiovascular disease risk factors among dialysis patients. Am J Hypertens. 2012;25(3):348–353. doi: 10.1038/ajh.2011.252. [DOI] [PubMed] [Google Scholar]
- 54.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009;32(9):1614–1619. doi: 10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Green JA, Mor MK, Shields AM, et al. Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis. :10. doi: 10.1053/j.ajkd.2012.12.014. 1053/j.ajkd.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 56.Abdel-Kader K, Dew MA, Bhatnagar M, et al. Numeracy skills in CKD: correlates and outcomes. Clin J Am Soc Nephrol. 2010;5(9):1566–1573. doi: 10.2215/CJN.08121109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Escobedo W, Weismuller P. Assessing health literacy in renal failure and kidney transplant patients. Prog Transplant. 2013;23(1):47–54. doi: 10.7182/pit2013473. [DOI] [PubMed] [Google Scholar]
- 58.Chisholm MA, Fair J, Spivey CA. Health literacy and transplant patients and practitioners. Public Health. 2007;121(10):800–803. doi: 10.1016/j.puhe.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 59.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of non-standardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292–298. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 60.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents’ medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. 2010;164(2):181–186. doi: 10.1001/archpediatrics.2009.269. [DOI] [PubMed] [Google Scholar]
- 61.Lau DT, Berman R, Halpern L, Pickard AS, Schrauf R, Witt W. Exploring factors that influence informal caregiving in medication management for home hospice patients. J Palliat Med. 2010;13(9):1085–1090. doi: 10.1089/jpm.2010.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Berkman ND, Sheridan SL, Donahue KE, et al. Health Literacy Interventions and Outcomes: An Updated Systematic Review. Agency for Healthcare Research and Quality; Rockville, MD: 2011. Evidence Report/Technology Assessment No. 199. Prepared by RTI International–University of North Carolina Evidence-Based Practice Center under contract No. 290-2007-10056-I. AHRQ Publication Number 11-E006. [Google Scholar]
- 63.Wolff K, Cavanaugh K, Malone R, et al. The Diabetes Literacy and Numeracy Education Toolkit (DLNET): materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educ. 2009;35(2):233–236. 238–241, 244–245. doi: 10.1177/0145721709331945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cavanaugh K, Wallston KA, Gebretsadik T, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32(12):2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Connelly K, Siek KA, Chaudry B, Jones J, Astroth K, Welch JL. An offline mobile nutrition monitoring intervention for varying-literacy patients receiving hemodialysis: a pilot study examining usage and usability. J Am Med Inform Assoc. 2012;19(5):705–712. doi: 10.1136/amiajnl-2011-000732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mayberry LS, Kripalani S, Rothman RL, Osborn CY. Bridging the digital divide in diabetes: family support and implications for health literacy. Diabetes Technol Ther. 2011;13(10):1005–1012. doi: 10.1089/dia.2011.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Calderon JL, Zadshir A, Norris K. A survey of kidney disease and risk-factor information on the World Wide Web. MedGenMed. 2004;6(4):3. [PMC free article] [PubMed] [Google Scholar]
- 68.Young HN, Chan MR, Yevzlin AS, Becker BN. The rationale, implementation, and effect of the Medicare CKD education benefit. Am J Kidney Dis. 2011;57(3):381–386. doi: 10.1053/j.ajkd.2010.10.056. [DOI] [PubMed] [Google Scholar]
- 69.Boulware LE, Hill-Briggs F, Kraus ES, et al. Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Dis. 2013;61(3):476–486. doi: 10.1053/j.ajkd.2012.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]