Abstract
Episodic memory tasks are one of the most sensitive tools to discriminate Alzheimer’s disease (AD). This study aimed to validate a shorter version verbal memory test that will efficiently assess Chinese elderly with memory complaints. One hundred and eighty-five elderly with normal cognition (NC) and 217 AD patients were evaluated. Each participant received the Chinese Version Verbal Learning Test (CVVLT) consisting of 9 two-character nouns with 4 learning trials, 2 delayed recalls in 30 seconds and 10 minutes, and a word recognition test. In the NC elderly, age and sex had significant effects on recall scores in CVVLT, while education level showed an inverse correlation with 3 different patterns of errors made during the learning, recall, and recognition trials. AD patients had lower scores across all recall tests. In those with lower educational level, NC elderly had higher perseveration errors than AD patients. The cutoff value between the AD and NC groups in the 10-minute recall was 4/5 for those aged >75 years and 5/6 for those aged <75 years. This study has good validity in discriminating AD participants and the data here can help in diagnosing AD and mild cognitive impairment using the CVVLT.
Keywords: Chinese Verbal Learning Test, education, memory, dementia, cutoff value, validation
INTRODUCTION
Episodic memory deficits are considered to be an early sign of Alzheimer’s disease (AD) and are characterized by ineffective storage of new information, rapid forgetting, and inability to benefit from external cues (Dubois et al., 2007). Neuropsychological tests have been designed to evaluate memory registration, learning ability, recall, and recognition in patients with AD and other disorders (Dorrego et al., 1999; Mohs, 1996; Soininen & Scheltens, 1998). For example, the California Verbal Learning Test (CVLT-2) (Delis, Kramer, Kaplan, & Ober, 1987) is a widely used instrument for evaluating episodic memory that uses a list learning paradigm (Defer, Daniel, & Marie, 2006; Woodard, Goldstein, Roberts, & McGuire, 1999). The CVLT-2 measures multiple aspects of memory, including learning over multiple trials, retention over delays, free recall, cued recall and recognition, serial position effects, semantic organization, intrusions, and interference (Elwood, 1995).
In addition to the 16-item version designed for less impaired populations, there is a 9-item version that is suited for patients with more severely impaired memory (Delis et al. 1987; Woodard et al., 1999). This short version (CVLT-SF) consists of three words from three different semantic categories. It has good sensitivity and specificity in detecting deficits in dementia patients (Woodard et al., 1999) and has been used to predict dementia conversion (Lekeu et al., 2009). However, current research has been based entirely on English-speaking participants, which may not be valid when applied to individuals from other ethnic groups (Ponton et al., 1996).
Asian neuropsychologists have been adapting Western-based measures in clinical settings. Few studies have been conducted to evaluate the verbal learning test in Chinese speaking populations. Chiu et al. (Au et al., 2003) demonstrated episodic memory deficits in AD using a locally developed 16-word list-learning test (the Hong Kong List Learning Test). Another study with Chinese Rey auditory verbal learning test (Lee, Yuen, & Chan, 2002) used 15 word lists with 5 learning trials and recalls to assess the immediate memory span, learning, and recall ability. The long learning list may be beneficial in detecting subtle changes, but the longer testing time may not be suitable for older participants. Furthermore, most of the Chinese elderly are not highly educated, so a long learning list with abstract nouns can be frustrating, especially in those with memory complaints. A short word-list memory test with norms is needed for the Chinese elderly.
However, considering cultural differences, direct translation of words from Western-based batteries have several shortcomings, including differences in word familiarity, frequency, and phonemes. Direct translation may result in different characters in each noun that can influence learning, while familiarity of categories is also culturally biased.
The present study aimed to develop a validated short-form Chinese verbal learning test that is suitable for both the elderly with normal cognition (NC) and those with AD in Taiwan. A new verbal learning test using 9 two-character nouns that was different from the original CVLT-SF was developed to examine the effect of education, age, and gender on the performance of memory in NC and AD elderly, aside from their learning and memory profiles. A cutoff value for discriminating between AD and NC controls was also determined.
METHODS
Instrument
The Chinese Version Verbal Learning Test (CVVLT) consistsd of 9 two-character nouns presented over 4 learning trials, with recall assessed after 30-second and 10-minute delays, and a delayed word recognition test. The list was composed of 9 nouns, which translated into English as hat (
 ), strawberry (
), strawberry (
 ), ferry (
), ferry (
 ), sweater (
), sweater (
 ), pineapple (
), pineapple (
 ), train (
), train (
 ), belt (
), belt (
 ), star fruit (
), star fruit (
 ), and plane (
), and plane (
 ). We did not translate the original CVLT because of culture differences. Because Chinese elderly, especially women, were not familiar with the name of the instrument, the category of “instrument” was changed into “transportation”. We combined high frequency and median frequency in the two-character nouns based on our preliminary study about the categorical word frequency. Each of the items was within one of the following three categories: fruits, clothes, and transportation. The recognition test was composed of 27 word-lists, with 9 target words, 9 distracter prototypes, and 9 words unrelated to the learning list.
). We did not translate the original CVLT because of culture differences. Because Chinese elderly, especially women, were not familiar with the name of the instrument, the category of “instrument” was changed into “transportation”. We combined high frequency and median frequency in the two-character nouns based on our preliminary study about the categorical word frequency. Each of the items was within one of the following three categories: fruits, clothes, and transportation. The recognition test was composed of 27 word-lists, with 9 target words, 9 distracter prototypes, and 9 words unrelated to the learning list.
Participants
Four hundred and seventeen (417) participants were recruited from the memory clinic of the Department of Neurology of Taipei Veterans General Hospital and Kaohsiung Chang Gung Memorial Hospital. These included 232 patients with a clinical diagnosis of AD and 185 NC elderly. The human ethics committee of both hospitals approved the study protocol.
Trained neuropsychologists conducted the CVVLT and Mini-Mental State Examination (MMSE) (Folstein, Folstein, & McHugh, 1975). Each participant and a family member or primary caregiver were interviewed independently by a neuropsychologist or neurologist using the Clinical Dementia Rating (CDR) scale (Hughes, Berg, Danziger, Coben, & Martin, 1982). The CDR rated the participant’s impairments in 6 categories – memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care – on a 5-point scale (0, 0.5, 1, 2, and 3). Summarizing the impairment ratings, all of the participants were assigned a rating score of CDR-0 indicating no dementia, and 0.5, 1, 2, 3 indicating questionable, mild, moderate, and severe dementia, respectively. Only patients with CDR 1 and 2 were included in the analysis.
Neurologists interviewed all of the participants. The diagnosis of AD was based on the results of clinical interviews, neurologic examinations, neuropsychological tests, laboratory findings, and neuroimaging evaluation. The diagnostic neuropsychological battery for AD mainly depended on the MMSE and CDR. CVVLT was not used for the diagnosis of AD. All AD patients met the criteria of the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) (McKhann et al., 1984) and the Diagnostic and Statistical Manual of Mental disorders, 4th edition (American Psychiatric Association, 1994).
The NC elderly controls were volunteers or the spouses of the patients. All of them received the same standard clinical evaluation used for AD participants. None had a history of neurologic or psychiatric disorders, or showed any evidence of impairment in the neurologic examination. All of the NC controls had CDR 0.
Procedures and Scoring
The examiner read the 9-word list aloud at one-second intervals in fixed order over 4 learning trials (CVVLT 1 to 4). After each trial, the participant was asked to recall as many words as he/she could, in any order. After 30 seconds (CVVLT-30s) and 10 minutes (CVVLT-10m), the participant was again asked to recall the list. The number of correct items, intrusions, and perseveration errors were recorded in each trial. Intrusion was defined as the participant giving an incorrect item not present in the list, while perseveration errors meant that a participant gave a correct item more than once. On the cued recall trials, participant’s were asked to recall the 9-word lists as the examiner specified each category (i.e., fruit, clothes, and transportation).
The CVVLT ended with a recognition task. As each word on a 27-word list was read aloud, the participant indicated whether it was a target word or a distracter. Some distracters shared semantic categories with the target words (prototypic), while others sounded alike (unrelated categories). Intrusions were scored separately on free and cued recall trials, whereas perseverations were tallied over all trials. The total correct recall scores from the first 4 trials were also calculated (CVVLT-total) for further analysis.
Statistical analysis was done using the Statistical Package for Social Sciences (SPSS) software package (version 13 for Windows®, SPSS Inc., Chicago, IL). Two-tailed Student’s t tests were used to compare quantitative data between AD and cognitively normal participants. One-way analysis of variance (ANOVA) and a multivariate general linear model were used to analyze demographic factors or interactions with CVVLT scores. Post-hoc analysis with the Tukey method was used to avoid type one error in multiple comparisons.
Pearson correlation analysis was used to check the correlations between scores in CVVLT and other demographic data studies. Receiver operating characteristic (ROC) was used to evaluate the discriminatory potential of CVVLT scores for AD screening. The cutoff scores of CVVLT and their sensitivity and specificity were determined for the AD and NC control groups.
RESULTS
Of the 402 participants included, there were 227 males and 175 females. Their mean age was 75.1 ± 9.1 years (range: 51–94 years) and their mean education level was 11.3 ± 4.7 years of schooling (range: 0–19 years). There were 185 NC elderly and 217 with AD. Among the AD patients, 194 had CDR 1 and 23 had CDR 2. Table 1 shows the more detailed demographic and clinical features of the participants. In demographic comparison, the AD group was older and had lower educational levels (p < .001). Sex distributions in the two groups were not significantly different.
Table 1.
Demographic data and scores in the Chinese Version Verbal Learning Test
| NC (n = 185) | AD (n = 217) | |||
|---|---|---|---|---|
| Age range (mean ± SD) | 51–94 (70.9 ± 9.5) | 57–94 (78.8 ± 6.9) | ||
| Sex (M/F) | 101/84 | 126/91 | ||
| Education (mean ± SD) | 0–18 (13.1 ± 3.6) | 0–19 (9.8 ± 5.0)* | ||
| MMSE (mean ± SD) | 17–30 (28.7 ± 1.8) | 2–26 (18.0 ± 5.1)* | ||
| CDR = 1 (n = 194) | CDR = 2 (n = 23) | |||
| Chinese Version Verbal Learning Test | ||||
| Trial 1 (mean ± SD) | 5.1 ± 1.5 | 2.4 ± 1.5* | 2.5 (1.5) | 1.3 (1.4) |
| Trial 2 (mean ± SD) | 6.8 ± 1.4 | 3.3 ± 1.5* | 3.4 (1.5) | 1.9 (1.8) |
| Trial 3 (mean ± SD) | 7.5 ± 1.3 | 3.8 ± 1.7* | 3.9 (1.5) | 2.3 (1.5) |
| Trial 4 (mean ± SD) | 7.9 ± 1.0 | 3.9 ± 1.7* | 4.1 (1.6) | 2.4 (1.9) |
| Total recall (mean ± SD) | 26.0 ± 4.4 | 13.4 ± 5.8* | 13.9 (5.2) | 7.86 (6.4) |
| 30 sec recall (mean ± SD) | 7.6 ± 1.6 | 2.3 ± 1.9* | 2.32 (1.8) | 1.09 (1.4) |
| 10 min recall (mean ± SD) | 7.4 ± 1.7 | 0.9 ± 1.5* | 0.87 (1.4) | 0.43 (0.9) |
Note: Data are presented as mean ± SD standard deviation. Abbreviations: NC, normal control; AD, Alzheimer dementia
p < .001 comparing with control,
p < 0.001 comparing CDR 1 with 2.
CVVLT in the NC Elderly
Age
Age had a significant effect in the performance of CVVLT in 185 NC elderly (Table 2). It was inversely correlated with immediate and delayed recall scores in NC participants (r = −.304, p < .001 in CVVLT-30s; r = −.276, p < 0.001 in CVVLT-10m). All nondemented participants were categorized into three age groups: ≤ 65, 65–74, and ≥ 75 years. ANOVA revealed a significant difference among these groups in the CVVLT learning trials (CVVLT-1, F = 10.66, p = .0001; CVVLT-2, F = 15.5, p = .0001; CVVLT-3, F = 17.6, p = .0001; and CVVLT-4, F = 5.31, p = .006) and recall scores (CVVLT-30s, F = 10.53, p = .0001; CVVLT-10m, F = 7.1, p = .001).
Table 2.
Comparison between AD and NC participants from different education and age groups
| Education | All ages
|
Age < 75
|
Age ≥ 75
|
||||
|---|---|---|---|---|---|---|---|
| AD N = 217 | Control N = 185 | AD N = 43 | Control N = 115 | AD N = 174 | Control N = 70 | ||
| CVVLT-1 | 0–6 | 2.2 (1.7)* | 4.8 (1.3) | 2.9 (1.7)* | 4.9 (1.4) | 1.9 (1.7)* | 4.5 (1.3) |
| 7–11 | 2.6 (1.5)* | 4.8 (1.4) | 3.4 (2.9)* | 5.2 (1.5) | 2.4 (1.4)* | 4.4 (1.2) | |
| ≥ 12 | 2.4 (1.3)* | 5.2 (1.5) | 2.4 (1.6)* | 5.7 (1.4) | 2.4 (1.3)* | 4.5 (1.3) | |
| CVVLT-2 | 0–6 | 3.0 (1.9)* | 6.3 (1.1) | 3.5 (1.6)* | 6.5 (1.1) | 2.9 (2.1)* | 5.8 (1.3) |
| 7–11 | 3.4 (1.6)* | 6.7 (1.1) | 3.3 (1.8)* | 7.1 (1.0) | 3.4 (1.5)* | 6.2 (1.3) | |
| ≥ 12 | 3.4 (1.4)* | 7.0 (1.5) | 3.4 (1.6)* | 7.4 (1.4) | 3.4 (1.4)* | 6.2 (1.4) | |
| CVVLT-3 | 0–6 | 3.5 (1.9)* | 7.0 (1.2) | 4.2 (1.7)* | 7.2 (1.0) | 3.2 (1.9)* | 6.5 (1.7) |
| 7–11 | 3.8 (1.7)* | 7.4 (1.3) | 4.2 (2.2)* | 7.9 (1.0) | 3.7 (1.6)* | 6.9 (1.3) | |
| ≥ 12 | 4.00 (1.2)* | 7.6 (1.3) | 3.5 (1.1)* | 8.0 (1.1) | 4.1 (1.2)* | 7.0 (1.3) | |
| CVVLT-4 | 0–6 | 3.6 (1.9)* | 7.4 (0.8) | 4.3 (1.9)* | 7.3 (0.9) | 3.4 (1.9)* | 7.5 (0.6) |
| 7–11 | 4.0 (1.7)* | 7.9 (1.0) | 4.3 (2.0)* | 8.1 (0.8) | 3.9 (1.8)* | 7.6 (1.1) | |
| ≥ 12 | 4.1 (1.4)* | 8.0 (1.0) | 4.1 (1.5)* | 8.2 (0.9) | 4.1 (1.4)* | 7.7 (1.2) | |
| CVVLT-total | 0–6 | 12.3 (7.0)* | 25.4 (3.6) | 14.8 (6.4)* | 25.9 (3.4) | 11.3 (7.1)* | 23.3 (4.5) |
| 7–11 | 13.7 (5.9)* | 26 (4.3) | 15.0 (7.4)* | 27.6 (3.4) | 13.5 (5.6)* | 23.9 (4.5) | |
| ≥ 12 | 14 (4.0)* | 26.0 (4.4) | 13.4 (4.7)* | 27.7 (4.3) | 14.1 (3.9)* | 24 (4.5) | |
| CVVLT_30_sec | 0–6 | 2.2 (2.0)* | 7.1 (1.2) | 2.5 (2.1)* | 7.3 (1.4) | 2.0 (2.0)* | 6.8 (0.5) |
| 7–11 | 2.5 (1.9)* | 7.7 (1.4) | 2.1 (2.1)* | 7.9 (1.2) | 2.2 (1.8)* | 6.9 (1.6) | |
| ≥ 12 | 2.1 (1.7)* | 7.6 (1.7) | 1.8 (1.7)* | 7.8 (1.3) | 2.1 (1.7)* | 6.9 (1.8) | |
| CVVLT_10 min | 0–6 | 0.9 (1.7)* | 7.2 (1.4) | 1.1 (1.8)* | 7.3 (1.4) | 0.9 (1.8)* | 6.8 (1.7) |
| 7–11 | 0.9 (1.4)* | 7.7 (1.3) | 1.2 (1.5)* | 7.9 (1.2) | 0.8 (1.3)* | 6.7 (2.0) | |
| ≥ 12 | 0.9 (1.5)* | 7.3 (1.8) | 0.6 (1.0)* | 7.8 (1.3) | 1.0 (1.5)* | 6.5 (2.2) | |
| Recognition hit | 0–6 | 6.25 (2.7)* | 8.5 (0.7) | 4 (1.73)* | 8.33 (1.2) | 7.31 (1.6) | 8.56 (0.7) |
| 7–11 | 6.56 (2.6)* | 5.5 (1.9) | 7.8 (1.1) | 7.75 (3.4) | 6.63 (2.5)* | 8.93 (0.3) | |
| ≥ 12 | 6.9 (2.6)* | 8.6 (0.8) | 3.67 (3.5)* | 8.66 (0.5) | 7.75 (1.6) | 8.64 (0.7) | |
| Cue recall | 0–6 | 1.39 (1.8)* | 7.5 (1.2) | 0.4 (0.5)* | 8.33 (1.2) | 1.62 (1.6)* | 7.33 (1.1) |
| 7–11 | 1.74 (1.6)* | 7.91 (1.2) | 1.4 (2.1)* | 8.17 (1.03) | 2.38 (0.9) | 8.14 (1.1) | |
| ≥ 12 | 2.03 (1.8)* | 7.82 (1.3) | 1 (1.7) | 8.03 (0.9) | 1.63 (2.1) | 7.95 (1.3) | |
Note.
p < .001 when comparing AD with age and education matched controls. CVVLT = Chinese Version Verbal Learning Test, AD = Alzheimer dementia. The three education groups are: n = 80 for education 0–6 years group, n = 137 for education 7–11 years group, and n = 185 for education ≥ 12 years.
Post-hoc analyses of CVVLT scores showed that participants in the ≤ 65 and 65–75 age groups did not have significant differences in learning or recall scores, but their scores were significantly higher than those in the ≥ 75 age group. Thus, only two age groups, <75 and ≥ 75 years, were used in subsequently analyses to examine the effect of age.
Age also showed a negative correlation with scores by cueing (r = −.216, p = .003). t test showed that the score was higher in the <75 age group (t = 3.36, p = .001), while there were no differences in recognition scores. Error analysis in the two age groups showed that only intrusions in CVVLT-2 and CVVLT-30s were significantly higher in the ≥ 75 age group (p < .05).
Education
Pearson correlation showed no significance between educational levels and CVVLT correct scores, but educational levels were inversely correlated with errors in learning, recall, and recognition trials. Educational levels were divided into three groups (Group 1: 0–6 years; Group 2: 7–12 years; and Group 3: >12 years) for further analysis. There were no differences among the three levels of education and CVVLT recall (from trial 1 to 10 min) and cued recall after post-hoc analysis. Educational level also showed a significant effect on total perseveration errors between Group 1 and Group 3 (p = .008), but it had no effects on total intrusion errors, intrusion, or perseveration errors in cued recalls.
Sex
Male participants had higher scores in the 1st to 3rd trials (p < .05). However, sex did not show any effect after trial 4 and in the scores of all recall and recognition tests.
Interaction of sex and education
Because educational level was significantly higher in males (male vs. female 13.7 ± 2.9 vs. 12.3 ± 4.2, p = .01), additional analyses controlling for the effects of education were conducted. A two-way between group ANOVA was conducted to explore the impact of sex and education on CV-VLT-10m score. The participants were divided into three groups according to their education (Group 1: 0–6 years; Group 2: 7–12 years; and Group 3: >12 years). The main effects for both sex (p = .39) and education (p = .44) did not reach statistical significance, and there was a marginal sex–education interaction effect (p = .06)
Interaction of age and education
According to previous findings by ANOVA for age groups, 75 years old was chosen as the boundary to compare the scores of 10-minute recall in three educational levels (Table 3). A two-way between group ANOVA was conducted to explore the impact of two age groups and three education groups on CVVLT-10m score. Age showed a significant effect on the CVVLT-10m score (p = .015), although the main effect for education and the interaction effect (p = .2) did not reach statistical significance.
Table 3.
Mean CVVLT cutoff scores, sensitivity, and specificity values for different age groups
| Group | CVVLT-1
|
CVVLT-total
|
CVVLT-10m
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Cutoff | Sensi. | Speci. | Cutoff | Sensi. | Speci. | Cutoff | Sensi. | Speci. | |
| All | 3/4 | 0.77 | 0.80 | 20/21 | 0.92 | 0.91 | 3/4 | 0.93 | 0.97 |
| 4/5 | 0.93 | 0.57 | 21/22 | 0.94 | 0.85 | 4/5 | 0.96 | 0.95 | |
| 5/6 | 0.98 | 0.88 | |||||||
| 6/7 | 0.99 | 0.77 | |||||||
| Age <75 | 4/5 | 0.81 | 0.77 | 22/23 | 0.91 | 0.92 | 4/5 | 0.95 | 0.97 |
| 5/6 | 0.95 | 0.49 | 23/24 | 0.93 | 0.82 | 5/6 | 0.97 | 0.92 | |
| 6/7 | 1 | 0.82 | |||||||
| Age ≥ 75 | 3/4 | 0.81 | 0.74 | 18/19 | 0.86 | 0.92 | 4/5 | 0.96 | 0.92 |
| 4/5 | 0.95 | 0.49 | 19/20 | 0.91 | 0.85 | 5/6 | 0.98 | 0.80 | |
| 5/6 | 0.99 | 0.19 | 20/21 | 0.94 | 0.80 | 6/7 | 0.99 | 0.69 | |
Note. Sensi = sensitivity, Speci = specificity, CVVLT-1 = Chinese Version Verbal Learning Test 1st trial, CVVLT-total = Chinese Version Verbal Learning Test scores sum from trials 1 to 4; CVVLT-10m = Chinese Version Verbal Learning Test 10 minute recall score.
CVVLT in the AD Elderly and Comparison with NC Controls
Multivariate ANOVA was performed to test the effects of age, gender, and education in the AD participants and the NC control group. There was an interaction between age and education on the performance of CCVLT-total (all p < .001), whereas the effect of gender was via the interaction of education. To control the interactions, comparisons between the two groups was done by dividing them into two age groups and three educational groups (Table 2). The AD group had lower scores than the controls across all learning and recall scores (p < .001). The retention rate was calculated by dividing scores in recall (CVVLT-30s and CVLLT-10m) by those in CVVLT-4, which revealed a significantly lower retention rate in AD (CV-VLT-30s AD vs. nondemented control: 54% vs. 95%, p = .001, and CVVLT-10m AD vs. nondemented control: 20% vs. 92%, p = .001). Regarding performance in cued recall and recognition, AD participants had lower scores in both cued recall and recognition tests (p < .001). These differences were noted in all three age groups.
Correlations between MMSE scores and CVVLT-total (r = .808), CVVLT-30s (r = .814), and CVVLT-10m (r = .797) scores were high (all p < .001). The three recall scores selected from MMSE also showed a high correlation with CVVLT-total (r = .888), CVVLT-30s (r = .811), and CVVLT-10m (r = .682) (all p < .001) scores.
From cued recall and recognition recalls, AD participants had lower scores in the three educational levels as compared to NC participants. After controlling for age and education, the effects were more prominent in a few subgroups (Table 2).
In the analysis of error patterns, the AD group had significantly higher scores in cued intrusion and perseveration (p < .001) errors as compared to the NC group. Errors in the recognition test showed that unrelated list errors and miss errors were higher in AD (p < .001), but there was no difference in prototypic errors.
Comparing all the CVVLT scores in AD participants with their CDR scores showed that across all learning trials, recall, and recognition tests, participants with CDR 1 had higher scores than CDR 2 participants (p < .001). However, participants with CDR 1 and 2 had no significant differences in error analysis.
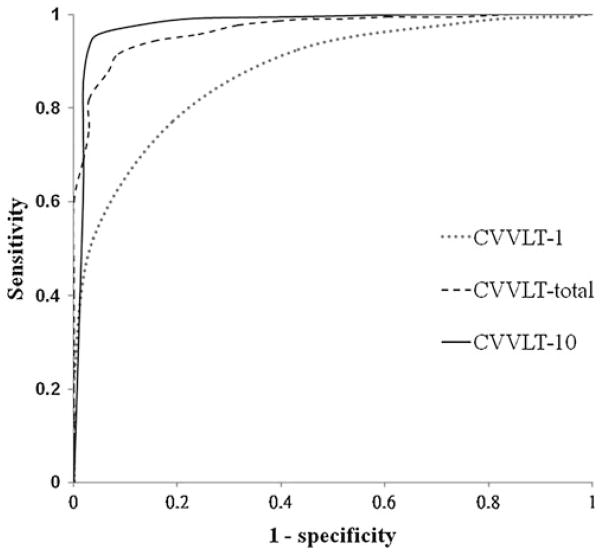
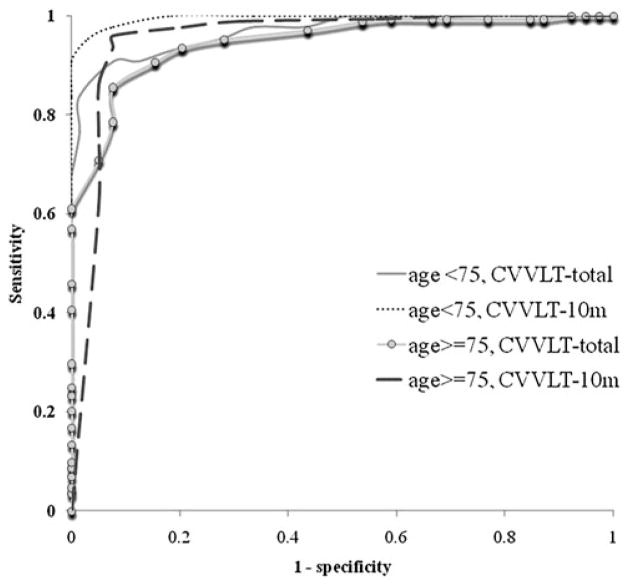
ROC analysis was used to evaluate the discriminatory potential of CVVLT-1, CVVLT-total, and CVVLT-10m scores in the screening of dementia. Both the sensitivity and specificity were calculated. The cutoff scores were determined by the minimum distance between a point on the ROC curve and the original point, with sensitivity 1 and 1-specificity of 0 in a two-axis plot for sensitivity, and 1-specificity for specific demographic groups. A summary of the CVVLT-1, CVVLT-total, and CVVLT-10m cutoff scores for the two age groups, as well as their respective sensitivity and specificity values, are listed in Table 3. The ROC curves for the participants, as well as the curves in the two age groups, are shown in Figures 1 and 2, respectively.
Fig. 1.
The receiver operating characteristic (ROC) curves of the Chinese Version Verbal Learning Test (CVVLT) for all participants. The ROC area in CVVLT-1 = 0.869, CVVLT-total = 0.967, and CVVLT-10m = 0.978.
Fig. 2.
The receiver operating characteristic (ROC) curves of the Chinese Version Verbal Learning Test (CVVLT) for participants in the two age groups. The ROC areas in the <75 years age group were: CVVLT-1 = 0.824, CVVLT-total = 0.968, CVVLT-10m = 0.995. The ROC areas in the ≥ 75 years age group were: CVVLT-1 = 0.852, CVVLT-total = 0.948, and CVVLT-10m = 0.953.
DISCUSSION
The main goal of this study was to validate the practical use of a 9-word verbal learning test for the Chinese-speaking population aged ≥ 50 years old. The CVVLT was modified according to the culture and word frequency difference from the American English CVLT. Because the categories were not identical in the CVLT and the CVVLT, a direct comparison between the scores of CVLT and CVVLT performed in Chinese-speaking and English-speaking populations could not be made. The norm data for this verbal memory test was established to make CVVLT more clinically useful in differentiating AD with NC controls, and different cutoff values of CVVLT-10m were suggested based on different age groups. For those aged <75 years, a cutoff value of 4/5 could achieve higher specificity, whereas 5/6 was used for higher sensitivity. For those aged >75 years, the suggested cutoff value was 4/5.
Educational level affected recall and recognition scores (Otto et al., 1994) in the original CVLT. However, in the NC population here, educational level did not show any effect on memory recall. This might be a result of the item design in this study, which was designed for the lower educated elderly. Furthermore, although education did not directly influence the results of recognition and recall, it had an interaction with age and sex. In this study, the nondemented group might not be the proper control group for AD cases, partly because of their drastically higher mean educational level. However, they were subgrouped according to their educational level to minimize the possible effects caused by different educational levels between AD and the nondemented group.
In Western CVLT, men have poorer memory performance than women (Delis et al., 1988; Reite, Cullum, Stocker, Teale, & Kozora, 1993). In the current study, men in the NC group have better performance in the learning trial, with an interaction of higher educational levels. Similar to the original CVLT (Delis et al. 1987; Taylor, Saint-Cyr, & Lang, 1990), this study shows that recall scores decline with age. The effect can be negligible if the educational level is <7 years. Because this is the first report on the 9-word Chinese version of this test, more cases may be needed to confirm the trends.
This study reveals that there are more intrusion errors in the older NC group. Huh and his colleagues (Huh, Kramer, Gazzaley, & Delis, 2006) suggested that degeneration of the frontal lobes may contribute to response errors in older adults. The frontal lobe theory may partly explain the observation that age is inversely correlated with immediate and delayed recall scores in the NC group. Another study shows that hippocampal volume is negatively related to the performance of acquisition and recall measures both in normal and AD elderly (Petersen et al., 2000). The response errors related to aging must also be considered during data interpretation in both the NC and AD groups.
This study shows that education affects error analysis in the NC group. Lower educational levels tend to make more intrusion errors in the early learning trials, while perseveration errors occur in the late learning stage and delayed recalls. Age also affects perseveration errors in NC participants. When AD participant and controls are compared, the controls have more perseverations than AD in low educational levels, while AD participants have more intrusions at high educational levels. The lower perseveration errors in AD patients than controls can be related to the disease process in AD, since they have low recall scores. At the same time, age may also exert an effect on errors, either intrusion or perseveration, in the AD group since the disease develops in older ages. Intrusions are generally useful in diagnosing AD (Delis et al., 1988; Fuld, Katzman, Davies, & Terry, 1982), but their effect may be stronger among Chinese with higher educational levels.
As expected, AD patients have lower scores in the short and delayed recall tests compared with NC participants across all age and educational subgroups. One may argue regarding delayed recall in CVVLT that the AD may have lower numbers of words learned from trial 4, which may affect their scores on short- and long-delayed recall. This study demonstrates the low retention rate of CVVLT-30s, while CVVLT-10m suggests that AD may have lower long-delay savings. Findings of rapid forgetting rate is consistent with observations in Western literature (Welsh, Butters, Hughes, Mohs, & Heyman, 1992). Since delayed recall precedes the recognition test, the low retention rate is related to higher forgetting rates, rather than the influence of the distracter list. It is also observed that AD patients do not benefit from external organization cues and the recognition test. The combination of poor performance in delayed recall, cued recall, and recognition tests is consistent with the hypothesis that AD memory deficits are primarily related to encoding rather than retrieval problems.
It is hoped that the CVVLT not only discriminates between AD and NC participants but also differentiates the severity of AD. This study shows that CVVLT scores across all learning and recall tasks decline as AD worsens. Patients with CDR 1 have higher learning and retention scores, and their memory scores can be facilitated by external cues and clustering. The Cognitive Ability Screening Instrument (CASI), a common cognitive test in Taiwan, can effectively recognize AD subjects. However, the short-term memory scale in CASI does not show any decline as the severity of CDR progresses, due to the floor effect. Another Chinese verbal learning test (Au et al., 2003) reveals that delayed recall is not useful in discriminating between mild and more severely demented patients. The data here suggest that CV-VLT may be an assessment for monitoring the progression of AD in the CDR 1 and 2 stages.
In this study, the cutoff values of CVVLT have been set to improve the diagnosis of AD. Adjusting different cutoff points to age can improve sensitivity and specificity to discriminate between AD and NC elderly. The area of ROC curves of CVVLT-1, CVVLT-total, and CVVLT-10m in diagnosing AD are 0.824, 0.968, and 0.995 for those aged <75 years and 0.852, 0.948, and 0.953 for those aged >75 years, respectively. Although the CVVLT-1 score has lower specificity and sensitivity than CVVLT-total and CVVLT-10m, it can be used as a clinical screening tool.
The norm data of the CVVLT in the elderly in this study can help diagnose amnesic mild cognitive impairment (MCI), which is supported by performance on objective memory tests. According to the data here, a 10-minute delayed recall in CVVLT lower than 1 standard deviation below normal, that is CVVLT-10m ≤ 6, is suggested as the standard in diagnosing amnesic MCI at all ages. The validity of this value to amnesic MCI should be further investigated through longitudinal MCI studies.
This study has some limitations. The correlation of CV-VLT scores with the severity of CDR scores is observed in cross-sectional data with AD participants of different CDR stages. The association between the decline in CVVLT and the decline in CDR should be confirmed by prospectively following the same patients over time. Moreover, this is a hospital-based study. Subjects who visit the hospital for memory problems or those who volunteer for research are usually easier to communicate with and are more cooperative than the elderly in the community. The acceptance of undergoing neuropsychological tests in these participants is also better. The results of this study have to be corroborated by further community-based studies.
In conclusion, this is the first report of the CVVLT with a sample size of 402 Chinese elderly. The CVVLT can effectively discriminate between AD and NC elderly, and its performance declines as AD progresses. The results here can be applied to the elderly in other areas with Chinese as their mother language.
Acknowledgments
This study was supported in part by grants from Chang Gung Memorial Hospital (CMRPG860171), the National Science Council (NSC 95 – 2314 – B – 075 - 002, NSC 96 – 2314 – B – 075 - 001), and Taipei Veterans General Hospital (V96C1-061).
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, (DSM-IV) 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Au A, Chan AS, Chiu H. Verbal learning in Alzheimer’s dementia. Journal of the International Neuropsychological Society. 2003;9:363–375. doi: 10.1017/S1355617703930025. [DOI] [PubMed] [Google Scholar]
- Defer GL, Daniel F, Marie RM. Study of episodic memory in multiple sclerosis using the California Verbal Learning Test: The data favour altered encoding. Revue Neurologique. 2006;162:852–857. doi: 10.1016/s0035-3787(06)75089-5. [DOI] [PubMed] [Google Scholar]
- Delis DC, Freeland J, Kramer JH, Kaplan E. Integrating clinical assessment with cognitive neuroscience: Construct validation of the California Verbal Learning Test. Journal of Consulting Clinical Psychology. 1988;56:123–130. doi: 10.1037//0022-006x.56.1.123. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. The California Verbal Learning Test: Research edition, Adult version. San Antonio, TX: The Psychological Corporation; 1987. [Google Scholar]
- Dorrego MF, Sabe L, Garcia Cuerva A, Kuzis G, Tiberti C, Boller F, Starkstein SE. Remote memory in Alzheimer’s disease. Journal of Neuropsychiatry and Clinical Neuroscience. 1999;11:490–497. doi: 10.1176/jnp.11.4.490. [DOI] [PubMed] [Google Scholar]
- Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, et al. Research criteria for the diagnosis of Alzheimer’s disease: Revising the NINCDS-ADRDA criteria. Lancet Neurology. 2007;6:734–746. doi: 10.1016/S1474-4422(07)70178-3. [DOI] [PubMed] [Google Scholar]
- Elwood RW. The California Verbal Learning Test: Psychometric characteristics and clinical application. Neuropsychology Review. 1995;5:173–201. doi: 10.1007/BF02214761. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fuld PA, Katzman R, Davies P, Terry RD. Intrusions as a sign of Alzheimer dementia: Chemical and pathological verification. Annals of Neurology. 1982;11:155–159. doi: 10.1002/ana.410110208. [DOI] [PubMed] [Google Scholar]
- Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. British Journal of Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- Huh TJ, Kramer JH, Gazzaley A, Delis DC. Response bias and aging on a recognition memory task. Journal of the International Neuropsychological Society. 2006;12:1–7. doi: 10.1017/S1355617706060024. [DOI] [PubMed] [Google Scholar]
- Lee T, Yuen K, Chan C. Normative data for neuropsychological measures of fluency, attention, and memory measures for Hong Kong Chinese. Journal of Clinical and Experimental Neuropsychology. 2002;24:615–632. doi: 10.1076/jcen.24.5.615.1001. [DOI] [PubMed] [Google Scholar]
- Lekeu F, Magis D, Marique P, Delbeuck X, Bechet S, Guillaume B, et al. The California Verbal Learning Test and other standard clinical neuropsychological tests to predict conversion from mild memory impairment to dementia. Journal of Clinical and Experimental Neuropsychology. 2009;20:1–12. doi: 10.1080/13803390902889606. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Mohs RC. The Alzheimer’s Disease Assessment Scale. International Psychogeriatrics. 1996;8:195–203. doi: 10.1017/s1041610296002578. [DOI] [PubMed] [Google Scholar]
- Otto MW, Bruder GE, Fava M, Delis DC, Quitkin FM, Rosenbaum JF. Norms for depressed patients for the California Verbal Learning Test: Associations with depression severity and self-report of cognitive difficulties. Archives of Clinical Neuropsychology. 1994;9:81–88. [PubMed] [Google Scholar]
- Petersen RC, Jack CR, Jr, Xu YC, Waring SC, O’Brien PC, Smith GE, et al. Memory and MRI-based hippocampal volumes in aging and AD. Neurology. 2000;54:581–587. doi: 10.1212/wnl.54.3.581. [DOI] [PubMed] [Google Scholar]
- Ponton MO, Satz P, Herrera L, Ortiz F, Urrutia CP, Young R, et al. Normative data stratified by age and education for the Neuropsychological Screening Battery for Hispanics (NeSBHIS): Initial report. Journal of the International Neuropsychological Society. 1996;2:96–104. doi: 10.1017/s1355617700000941. [DOI] [PubMed] [Google Scholar]
- Reite M, Cullum CM, Stocker J, Teale P, Kozora E. Neuropsychological test performance and MEG-based brain lateralization: Sex differences. Brain Research Bulletin. 1993;32:325–328. doi: 10.1016/0361-9230(93)90195-h. [DOI] [PubMed] [Google Scholar]
- Soininen HS, Scheltens P. Early diagnostic indices for the prevention of Alzheimer’s disease. Annals of Medicine. 1998;30:553–559. doi: 10.3109/07853899809002604. [DOI] [PubMed] [Google Scholar]
- Taylor AE, Saint-Cyr JA, Lang AE. Memory and learning in early Parkinson’s disease: Evidence for a “frontal lobe syndrome”. Brain Cognition. 1990;13:211–232. doi: 10.1016/0278-2626(90)90051-o. [DOI] [PubMed] [Google Scholar]
- Welsh KA, Butters N, Hughes JP, Mohs RC, Heyman A. Detection and staging of dementia in Alzheimer’s disease. Use of the neuropsychological measures developed for the Consortium to Establish a Registry for Alzheimer’s Disease. Archives of Neurology. 1992;49:448–452. doi: 10.1001/archneur.1992.00530290030008. [DOI] [PubMed] [Google Scholar]
- Woodard JL, Goldstein FC, Roberts VJ, McGuire C. Convergent and discriminant validity of the CVLT (dementia version). California Verbal Learning Test. Journal of Clinical and Experimental Neuropsychology. 1999;21:553–558. doi: 10.1076/jcen.21.4.553.878. [DOI] [PubMed] [Google Scholar]