While keratoacanthomas (KAs) and squamous cell carcinomas (SCCs) have been reported in response to a number of systemic drugs such as vemurafenib, sorafenib, or voriconazole, 1–3 their association with Smoothened inhibitors has not been previously noted. Herein, we report 2 cases of new KAs developing within 2 months of starting vismodegib therapy in individuals with no history of KAs or SCCs.
Report of Cases
Case 1
The first case involves rapid onset of KA on the arm after 2 weeks of vismodegib treatment for locally advanced basal cell carcinoma (BCC) on lower eyelid. A 100-year-old healthy white woman presented with a slowly growing papule on her right lower eyelid. A biopsy 2 years earlier had shown infiltrative BCC, but she had refused surgery owing to her lack of symptoms. She had no history of SCCs. Over time, the eyelid BCC began to grow and impinge on her visual field, and she sought treatment. At that point, a 2-cm ulcerated tumor involving the lower eyelid was noted. A computed tomography scan revealed a 1.8 × 1.7 × 1.1-cm mass without obvious involvement of the orbit. She declined radiation and surgical treatments owing to their adverse effects and started vismodegib treatment at 150 mg/d.
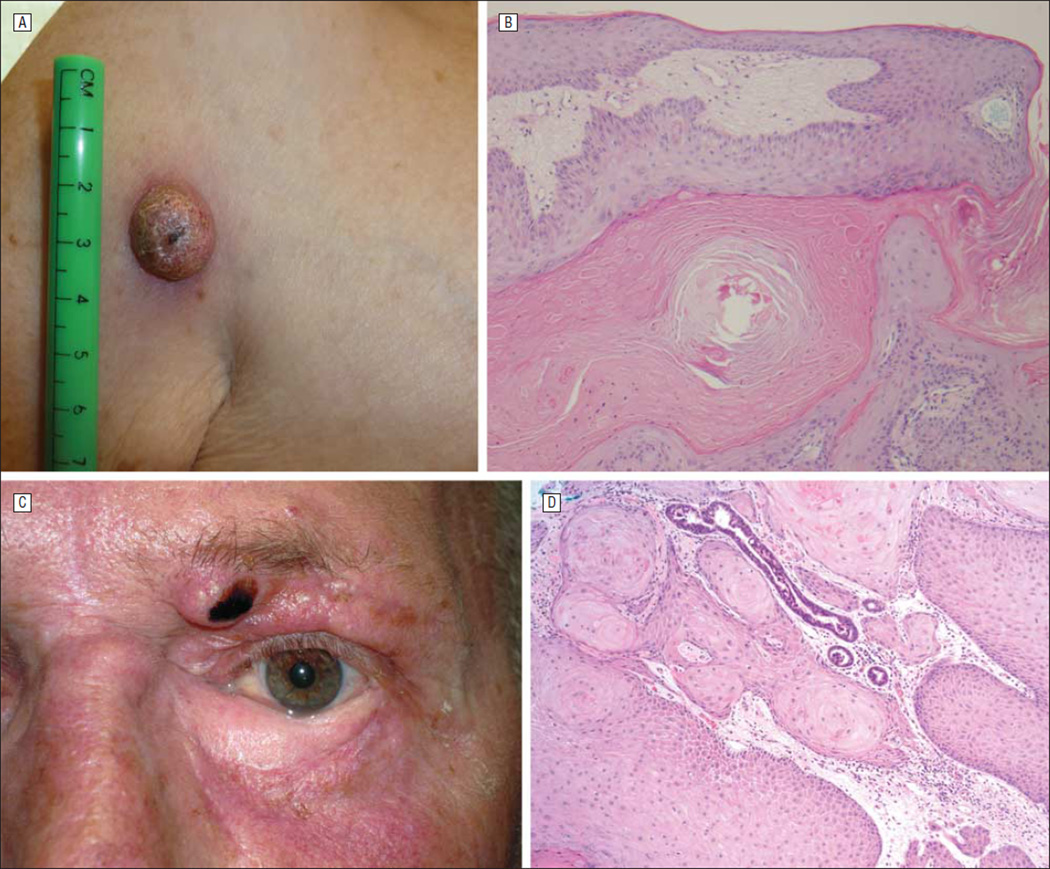
A careful full-body skin examination performed prior to the start of drug therapy had revealed no concerning skin lesions or lymphadenopathy. Two weeks after start of vismodegib treatment, she developed a rapidly enlarging 2-cm mass on her upper arm (Figure, A) with central depression. Biopsy confirmed an SCC, KA type (Figure, B). The KA was excised, and the patient continued on vismodegib treatment with ongoing regression of the eyelid BCC.
Figure.
Development of distant keratoacanthomas (KAs) while undergoing vismodegib therapy. A, Clinical photograph of the rapid-onset 2-cm nodule on the right arm of patient 1 after 2 weeks of vismodegib treatment for an eyelid basal cell carcinoma (BCC). B, Histologic image from case 1 shows a cup-shaped, well-differentiated squamous cell carcinoma (SCC) invaginating into the dermis that was filled with keratin, consistent with KA (hematoxylin-eosin, original magnification ×100). C, Clinical photograph of KA development on the inferior medial brow of patient 2 after 7 weeks of vismodegib therapy for a periocular BCC. D, Histologic image shows a well-differentiated SCC, or KA (hematoxylin-eosin, original magnification ×100).
Case 2
Our second case involves a new KA development on the brow after 7 weeks of vismodegib treatment for locally advanced BCC on the medial canthus. A 53-year old healthy white man with no history of SCCs presented with a recurrent BCC on the left medial periorbital location after extensive excision and reconstruction 13 years earlier. He was started on treatment with vismodegib, 150 mg/d, and showed complete clinical regression of BCC after 7 weeks of treatment. However, at this time, he was noted to develop a 1-cm nodule with central depression on the medial and inferior aspect of his left eyebrow, separate from his BCC (Figure, C). Histologic analysis of a biopsy specimen showed a well-differentiated SCC, or KA (Figure, D). The KA was subsequently excised by Mohs micrographic surgery.
Comment
While these cases are observational in nature, the fact that neither of these patients had a history of SCC and subsequently developed it while undergoing vismodegib treatment is worthy of further scrutiny. Other oral chemotherapies such as vemurafenib1 and sorafenib2 or antifungal medications such as voriconzole3 have been associated with the development of KAs or squamous cell carcinomas. It is possible that vismodegib may promote the growth of squamous malignant neoplasms as well.
Longer follow-up times and additional patient observations are needed to confirm this phenomenon. Nonetheless, these findings call for close dermatologic surveillance for new skin tumors in patients treated with vismodegib.
Footnotes
Conflict of Interest Disclosures: Drs Tang, Epstein, and Chang have been investigators in studies sponsored by Genentech. Dr Chang has been an investigator in studies sponsored by Infinity and Novartis.
Additional Contributions: Olena Mykhaylichenko provided administrative support.
References
- 1.Su F, Viros A, Milagre C, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. N Engl J Med. 2012;366(3):207–215. doi: 10.1056/NEJMoa1105358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dubauskas Z, Kunishige J, Prieto VG, Jonasch E, Hwu P, Tannir NM. Cutaneous squamous cell carcinoma and inflammation of actinic keratoses associated with sorafenib. Clin Genitourin Cancer. 2009;7(1):20–23. doi: 10.3816/CGC.2009.n.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epaulard O, Saint-Raymond C, Villier C, et al. Multiple aggressive squamous cell carcinomas associated with prolonged voriconazole therapy in four immunocompromised patients. Clin Microbiol Infect. 2010;16(9):1362–1364. doi: 10.1111/j.1469-0691.2009.03124.x. [DOI] [PubMed] [Google Scholar]