Abstract
Background and purpose
Excessive wear of acetabular liners in hip replacements may lead to osteolysis and cup loosening. Different head materials are currently used. We measured differences in wear between alumina and cobalt-chrome heads with the same polyethylene liner.
Patients and methods
39 patients (43 hips) with osteoarthritis were included in a study with 10-year follow-up. Wear was measured as proximal and 3D penetration of the head in the liner with radiostereometry (RSA). All the patients were followed clinically with Harris hip score (HHS) for up to 10 years. Radiolucent lines and osteolytic lesions were assessed on plain radiographs.
Results
With alumina heads, proximal wear (95% CI) after 10 years was 0.62 (0.44–0.80) mm as compared to 1.40 (1.00–1.80) mm in the cobalt-chrome group. For 3D wear, the results were 0.87 (0.69–1.04) mm for alumina heads and 1.78 (1.35–2.21) mm for cobalt-chrome heads. Median (range) HHS was 98 (77–100) in the alumina group and it was 93 (50–100) in the cobalt-chrome group (p = 0.01). We found no difference in osteolysis between the groups.
Interpretation
We found better wear properties with alumina heads than with cobalt-chrome heads. We recommend the use of alumina heads in patients in whom a high wear rate might be anticipated.
Polyethylene (PE) wear is a major limitation for long-term survival of total hip replacements (THRs). Production of wear particles induces osteolysis and leads to aseptic loosening of the implant (Dumbleton et al. 2002, Wilkinson et al. 2005, Purdue et al. 2006). Dumbleton et al. (2002) suggested that the threshold for acceptable linear wear should be 0.1 mm per year and that osteolysis is almost non-existent if wear is reduced to below 0.05 mm per year. They also reported that osteolysis and loosening increases if the wear rate is more than 0.2 mm/year.
The problem of wear has been addressed in different ways, such as head size and material choice. The use of smaller femoral heads reduces wear (Kesteris et al. 1996), but it increases dislocation-rate (Bystrom et al. 2003) and reduces range of motion (Burroughs et al. 2005). Different bearing surfaces such as ceramic-on-ceramic have low wear rates, but they have other disadvantages such as nano-sized wear particles, breakage, chipping, and squeaking (Keurentjes et al. 2008, Lang et al. 2008). Breakage of ceramic heads has been reported to range from 0.004% to 13% (Willmann 2000, Allain et al. 2003). A well-functioning ceramic head is thought to give less wear than a metal head when coupled with PE, because of a smoother surface and better wettability (Saikko et al. 2001, Hannouche et al. 2011). Metal-on-metal bearings have low wear rates, but reports from international registries have shown higher revision rates for resurfacing THR than for conventional THR.
Wear is related to activity (Schmalzried et al. 2000 ) and therefore young and active patients could possibly have higher prosthesis wear. Other factors that may have an influence on wear rates in THR are cup positioning, implant fixation method, implant material, and coating of implant. Possible patient factors are weight, age, gender, and level of activity.
The aim of this study was to investigate a possible difference in wear patterns between 2 different head materials (cobalt-chrome and alumina) of the same size (28 mm) articulating on liners made of identical PE in the same type of acetabular shell. Metal heads such as cobalt-chrome are cheap, durable, and well proven with PE acetabular components (Furnes et al. 2007). Other materials should be as safe and should have durability superior to that of metal heads, to replace them as the material of choice for use with PE in THR. One RSA study showed better wear properties for alumina heads than for cobalt-chrome heads with cemented cups (Dahl et al. 2012). Another study showed the opposite with uncemented cups (Sychterz et al. 2000).
Patients and methods
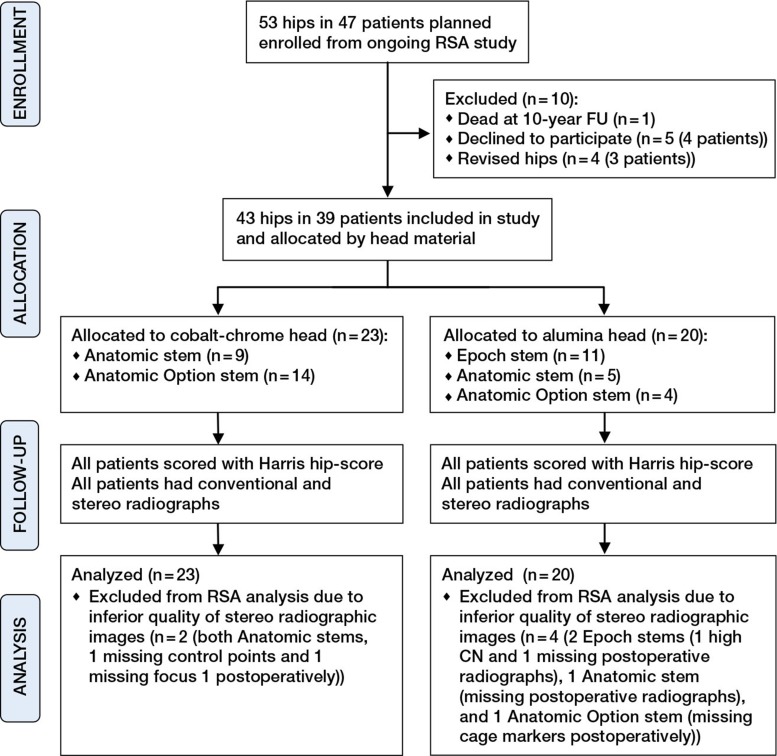
The cohort we studied was recruited from a randomized controlled multicenter study (Karrholm et al. 2002). In the original study, 53 hips in 47 patients were operated with total hip replacement (THR). 39 patients (43 hips) were included in the present study (Figure). In all patients, the indication was primary or secondary osteoarthritis without anatomical abnormalities. The patients were randomized to 3 groups. All of them received a Trilogy acetabular component. This is a hemispheric porous-coated (titanium mesh) cup with a polyethylene liner (compression-molded GUR 1050; Ticona, Summit, NJ) sterilized with γ-irradiation in nitrogen. All patients received the same liner material, but the liner thickness varied with the shell size. All cups were also fixated with 2–3 screws. On the femoral side, the patients were randomized to either Epoch, Anatomic, or Anatomic Option (Zimmer, Warsaw, IN). Epoch is a porous-coated composite stem with reduced stiffness, Anatomic is a proximally porous-coated titanium alloy stem, and Anatomic Option is a cemented cobalt-chrome (Zimaloy) stem. Palacos bone-cement (Schering Plough; Labo N.V., Belgium) was used in all the cemented cases. The uncemented stems had additional plasma-sprayed hydroxyapatite-tricalcium phosphate coating. All Epoch stems had alumina heads (Biolox Forte; CeramTec, Plochingen, Germany). 29 of 38 Anatomic and Anatomic Option stems had cobalt-chrome heads; 9 had the same alumina heads as the Epoch stems. The intention was to operate all patiaents in the study with alumina heads, but this was changed because the approval for these heads on the taper of the Anatomic stems was withdrawn. After this withdrawal, all Anatomic stems received cobalt-chrome heads. The same surgeon (FS) operated most patients and was present at all operations. The groups were comparable with regard to age, sex, weight, side, cup size, liner thickness, and preoperative Harris hip score (Table 1).
CONSORT 2010 flow diagram.
Table 1.
Description of patients and groups
| Cobalt-chrome | Alumina | |
|---|---|---|
| n | 23 | 20 |
| Age at operation a | 60 (53–72) | 64 (34–70) |
| Sex, M/F | 6/17 | 9/11 |
| Weight at operation a | 70 (58–98) | 78 (51–95) |
| Preoperative Harris hip score a | 52 (28–69) | 55 (25–67) |
| Side, left/right | 11/12 | 8/12 |
| Cup size a | 52 (48–60) | 54 (50–60) |
| Liner thickness a | 7.3 (6.3–10.4) | 7.3 (7.3–10.4) |
| Stem type | ||
| Epoch | 0 | 11 |
| Anatomic option | 14 | 4 |
| Anatomic | 9 | 5 |
aMedian (range)
Clinical outcome
All patients were scored with the Harris hip score preoperatively, and this examination was repeated after 10 years. Revisions and reasons for these were noted.
RSA
Index RSA was acquired with analog technique and measuring cage 41 (RSA Biomedical, Umeå, Sweden). The analog radiographs were scanned (Scanmaker 9800xl; Microtec Lab. Inc., Cerritos, CA), digitized, and re-marked with digital technique using UmRSA digital measuring software version 6.0 (RSA Bomedical). 10-year RSA was acquired digitally using measuring cage 43 and the same software as used for the index RSA. The acetabular components were also marked and measured using markerless technique (Borlin et al. 2006). The Trilogy cup is a hemisphere, and therefore the center of the hemisphere can be found using edge-detection methods. Linear wear was measured as penetration of the center of the head in the cup along the vertical (y-) axis and as a vector of all 3 axes (x-, y-, and z-axis). Cup movement was measured as migration and rotation of the cup in relation to the acetabular markers. Precision was determined from 71 double examinations as absolute mean difference (95% CI of the mean) between the double examinations postoperatively and after 10 years (Table 2). We included examinations with condition number (CN) below 120 and mean error below 0.3 in the study, as this is generally accepted to be adequate quality for RSA measurements (Valstar et al. 2005).
Table 2.
Mean migration of the center of the prosthetic head, in mm, in relation to the cup measured with RSA, significance level for difference, and precision of measurements from 71 double examinations. 95% CI of mean in parentheses and range in square brackets
| Direction | Cobalt-chrome | Alumina | p-value | Precision |
|---|---|---|---|---|
| Proximal (y-axis) | 1.40 (1.00 to 1.80) [0.38 to 3.6] | 0.62 (0.44 to 0.80) [0.23 to 1.33] | 0.001 | 0.09 (0.06–0.11) |
| Medial (x-axis) | –0.38 (–0.72 to –0.04) [–1.81 to 0.67] | –0.10 (–0.27 to –0.08) [–0.76 to 0.26] | 0.2 | 0.11 (0.08–0.14) |
| Posterior (z-axis) | –0.59 (–0.84 to –0.34) [–1.64 to 0.82] | –0.32 (–0.54 to –0.10) [–0.94 to 0.37] | 0.1 | 0.18 (0.13–0.23) |
| 3D (x-, y-, and z-axis) | 1.78 (1.35 to 2.21) [0.62 to 4.3] | 0.87 (0.69 to 1.04) [0.33 to 1.49] | < 0.001 | Not applicable |
Radiography
All patients had conventional radiographs taken at 10 years. These were analyzed using mdesk (RSA Biomedical). This software allows measurement of implant positioning, distribution of radiolucent lines (RLLs) between cup and pelvis, and osteolytic lesions. RLLs wider than 1 mm in the AP view were measured. Osteolytic lesions were measured in mm2 on the AP radiograms. Cup positioning in relation to pelvic landmarks was also determined.
Statistics
A mixed-model analysis was performed for difference in wear between groups since we had 2 patients with bilateral implants in the final wear analysis, thus not being independent observations. The regression analysis was done with xtreg in Stata software version 11.0. The significance level was set to p = 0.05 for differences between groups. We used Pearson’s correlation coefficient to check for correlation between continuous variables. Calculations were done using the PASW statistics package version 18.
Ethics
The study was conducted in accordance with the Helsinki Declaration. The regional ethical committee in Norway approved the study (REK Sör S-93122).
Results
Clinical outcome
There were 2 revisions in each group at 10 years. In the alumina group, 1 patient with bilateral Epoch stems was revised on both sides due to pain. She had measurable wear in both hips, but not enough to be revised for this reason alone. In the cobalt-chrome group, 1 patient was revised due to stem loosening and 1 was revised because of inexplicable pain. Both had Anatomic Option stems. Median (range) Harris hip score after 10 years was 93 (50–100) in the cobalt-chrome group and 98 (77–100) in the alumina group (p = 0.01).
RSA
RSA analyses were performed on patients who had radiographs of adequate quality postoperatively and after 10 years. This left us with 21 patients in the cobalt-chrome group and 16 in the alumina group. We found more than 50% reduction of head penetration (wear) both proximally and in 3D in the alumina group, compared to the cobalt-chrome group. The mean difference (95% CI) between the groups was 0.78 (0.34–1.22) mm for proximal wear and 0.91 (0.44–1.38) mm for 3D wear. Wear was measured for both groups along all axes (Table 2). We found no statistically significant difference in wear between the subgroups with different stems and fixation methods. There was also no statistically significant difference between men and women or between younger and older patients (i.e. less than or more than 60 years of age at operation) in this material. All cups were found to be stable.
Radiography
Mean area of osteolysis (95% CI) was 30 (21–39) mm2 in the cobalt-chrome group and 22 (14–30) mm2 in the alumina group (p = 0.2). 2 of 23 cases had no osteolysis in the cobalt-chrome group, as compared to 3 of 20 cases in the alumina group.
Most osteolytic lesions were found in the area of screw fixation. There was no significant difference in the distribution of radiolucent lines between the 2 groups. We found no systematic bias in cup positioning in relation to the pelvis between the groups.
Discussion
We found more than 50% reduction in wear for alumina heads on conventional polyethylene liners compared to cobalt-chrome heads. This is of considerable interest, as wear is a major reason for aseptic loosening and osteolysis in hip-replacement surgery. This study was conducted using conventional polyethylene, which is less wear-resistant than modern crosslinked polyethylene (Rohrl et al. 2007). Use of alumina heads instead of cobalt-chrome heads on modern polyethylene could reduce wear even further. The difference in wear between alumina and cobalt-chrome heads may also be less when articulating with crosslinked polyethylene. We found no statistically significant difference in osteolysis, although there was a tendency of more osteolysis in the cobalt-chrome group. 10 years may be too short a follow-up time for increased wear to manifest itself as increased osteolysis. Our findings do not support the so-called threshold for tolerable linear wear of 0.1 mm per year. The cobalt-chrome group had a wear pattern well above this threshold and the alumina group a wear pattern well below this threshold, but we did not find any difference in survival or osteolysis up to 10 years. A tendency of increased osteolysis and reduced clinical outcome at 10 years could be an indication for earlier failures in this group in future. Even though we found wear reduction of more than 50% for alumina heads and a tendency of less osteolysis in the alumina group, we cannot say that this was clinically significant after 10 years as there was no difference in the number of revisions between the groups. This has also been reported in the Australian joint registry, where revision rates of THRs with ceramic and metal heads articulating on modified PE have been compared; results with conventional PE have not been compared (Graves 2011).
The number of patients was too small to trust the observed difference in clinical outcome in our material. There were also substantial confounders to this finding, such as different stems and fixation methods. The Harris hip scores were generally high in both groups. The patients in our study were 61 years old on average at operation, and they will use their prosthesis for far more than the 10 years covered here.
The present study had several strengths. The patients were recruited from a randomized trial of stem fixation with RSA, so we had good check of the patients, and only 5 of them were lost to follow-up at 10 years. 1 investigator performed the clinical follow-up for all patients. Conventional radiographs were investigated in addition to RSA, for possible explanations of difference in wear other than head material—such as offset, height of hip center, and cup inclination—and to evaluate bone loss and signs of loosening of cups and stems. The reduction in wear was highly significant even though the number of patients was small.
The weaknesses of our study were that it was not originally designed to study wear, and that randomization was not done by head material, but by stem type. Thus, different stems and fixation methods were used on the femoral side. One might speculate that this could have an influence on the wear of the articulation. We found no difference in wear whether patients in the alumina group had Epoch or Anatomic/Anatomic Option stems. There was also no difference in wear between Anatomic and Anatomic Option stems in the cobalt-chrome group. This indicates that stem type is not a major confounder. When we break this material down, the subgroups become very small with only a few patients in each group; therefore, it is probably underpowered with regard to analysis of subgroups such as high/low BMI, men/women, and young/old patients. RSA examinations were obtained with different calibration cages and with analog technique postoperatively but digital technique at 10 years. We used markerless technique for our wear measurements; this relies on using the contour of the femoral head to calculate the center of the head. This contour is easier to determine on the more radiopaque cobalt-chrome heads, but we found no statistically significant difference in precision between the head materials. We had problems with a lack of visible markers and poor spread of markers in the acetabular segment, which was a limitation regarding the evaluation of cup stability. The patients had no clinical signs of cup loosening up to 10 years, and we found no large osteolytic lesions on conventional X-rays. We therefore considered the cups to be stable despite this limitation. The study was performed with conventional polyethylene. Most hip-replacement surgeons have changed their practice and have left this socket material in favor of modern crosslinked PE.
In summary, we found more than 50% wear reduction when using alumina heads rather than cobalt-chrome heads in this study. We recommend the use of this head material in patients in whom a high wear rate might be anticipated.
Acknowledgments
JD: wrote the manuscript, collected clinical data, performed analyses with RSA and mdesk, and performed statistical analyses. FS: planned the study, operated most of the patients, contributed to the radiographic analyses, and proofread the manuscript. LN: planned the study and proofread the manuscript. SMR: contributed to writing of the manuscript and contributed to both the RSA analyses and the statistical evaluation.
We thank radiographer Mona Risdal for performing the RSA examinations, and for scanning and marking all the images. We also thank Ingar Holme of the Department of Biostatistics for invaluable help with the statistical analyses.
No competing interests declared.
References
- Allain J, Roudot-Thoraval F, Delecrin J, Anract P, Migaud H, Goutallier D. Revision total hip arthroplasty performed after fracture of a ceramic femoral head. A multicenter survivorship study . J Bone Joint Surg (Am) 2003;85(5):825–30. doi: 10.2106/00004623-200305000-00009. [DOI] [PubMed] [Google Scholar]
- Borlin N, Rohrl SM, Bragdon CR. RSA wear measurements with or without markers in total hip arthroplasty . J Biomech. 2006;39(9):1641–50. doi: 10.1016/j.jbiomech.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes . J Arthroplasty. 2005;20(1):11–9. doi: 10.1016/j.arth.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Bystrom S, Espehaug B, Furnes O, Havelin LI. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register . Acta Orthop Scand. 2003;74(5):514–24. doi: 10.1080/00016470310017893. [DOI] [PubMed] [Google Scholar]
- Dahl J, Söderlund P, Nivbrant B, Nordsletten L, Rohrl S. Less wear with aluminum-oxide heads than cobalt-chrome heads with ultra high molecular weight cemented polyethylene cups: a ten-year follow-up with radiostereometry . Int Orthop. 2012;36(3):485–90. doi: 10.1007/s00264-011-1334-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty . J Arthroplasty. 2002;17(5):649–61. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- Furnes O, Havelin LI, Espehaug B, Steindal K, Egil Sørås TE. The Norwegian Arthroplasty Register . http://nrlweb.ihelse.net/eng/Report2007.pdf Report. 2007
- Graves S. Australian Orthopaedis Association National Joint Repalcement Registry. 2011.
- Hannouche D, Zaoui A, Zadegan F, Sedel L, Nizard R. Thirty years of experience with alumina-on-alumina bearings in total hip arthroplasty . Int Orthop. 2011;35(2):207–13. doi: 10.1007/s00264-010-1187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karrholm J, Anderberg C, Snorrason F, Thanner J, Langeland N, Malchau H, et al. Evaluation of a femoral stem with reduced stiffness. A randomized study with use of radiostereometry and bone densitometry . J Bone Joint Surg (Am) 2002;84(9):1651–8. [PubMed] [Google Scholar]
- Kesteris U, Ilchmann T, Wingstrand H, Onnerfalt R. Polyethylene wear in Scanhip arthroplasty with a 22 or 32 mm head: 62 matched patients followed for 7-9 years . Acta Orthop Scand. 1996;67(2):125–7. doi: 10.3109/17453679608994655. [DOI] [PubMed] [Google Scholar]
- Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings . Clin Orthop. 2008;466(6):1438–43. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang JE, Whiddon DR, Smith EL, Salyapongse AK. Use of ceramics in total hip replacement . J Surg Orthop Adv. 2008;17(1):51–7. [PubMed] [Google Scholar]
- Purdue PE, Koulouvaris P, Nestor BJ, Sculco TP. The central role of wear debris in periprosthetic osteolysis . HSS J. 2006;2(2):102–13. doi: 10.1007/s11420-006-9003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrl SM, Li MG, Nilsson KG, Nivbrant B. Very low wear of non-remelted highly cross-linked polyethylene cups: An RSA study lasting up to 6 years . Acta Orthop. 2007;78(6):739–45. doi: 10.1080/17453670710014509. [DOI] [PubMed] [Google Scholar]
- Saikko V, Ahlroos T, Calonius O, Keranen J. Wear simulation of total hip prostheses with polyethylene against CoCr, alumina and diamond-like carbon. Biomaterials. (Research Support . Non-U.S. Gov’t) 2001;22(12):1507–14. doi: 10.1016/s0142-9612(00)00306-9. [DOI] [PubMed] [Google Scholar]
- Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, et al. Wear is a function of use, not time . Clin Orthop. 2000;(381):36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- Sychterz CJ, Engh CA. Jr., Young AM, Hopper RH, Jr., Engh CA. Comparison of in vivo wear between polyethylene liners articulating with ceramic and cobalt-chrome femoral heads . J Bone Joint Surg (Br) 2000;82(7):948–51. doi: 10.1302/0301-620x.82b7.9885. [DOI] [PubMed] [Google Scholar]
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants . Acta Orthop. 2005;76(4):563–72. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- Wilkinson JM, Hamer AJ, Stockley I, Eastell R. Polyethylene wear rate and osteolysis: critical threshold versus continuous dose-response relationship . J Orthop Res. 2005;23(3):520–5. doi: 10.1016/j.orthres.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Willmann G. Ceramic femoral head retrieval data . Clin Orthop. 2000;(379):22–8. doi: 10.1097/00003086-200010000-00004. [DOI] [PubMed] [Google Scholar]