Abstract
Background and purpose
Restoration of bone stock at revision hip surgery remains a challenge. Alternative graft materials with suitable mechanical properties for impaction grafting have been sought due to issues with infection, antigenicity, cost, and availability of allograft. We have previously presented good short-term results of the use of BoneSave, a biphasic porous ceramic bone graft substitute, consisting of sintered 80% tricalcium phosphate and 20% hydroxyapatite, in a 50:50 mix with femoral head allograft. We now present the medium-term results.
Methods
We conducted a retrospective review of a cohort of 43 consecutive patients undergoing impaction grafting of contained acetabular defects by multiple surgeons at a single center. 34 patients received uncemented acetabular components and 9 received cemented components. Patients were followed up radiographically and with the self-reported satisfaction scale (SAPS), Oxford hip score (OHS), and the Short-Form 12 (SF12) health survey. Kaplan-Meier survivorship analysis was performed with revision of the acetabular component, revision of any part of the construct, and reoperation as endpoints.
Results
The fate of all cases was known. Median follow-up of the surviving patients was 80 (69–106) months. 15 patients died during the follow-up period, 14 with their construct in situ. The survivorship of the grafted acetabulum and acetabular component was 94% (95% CI: 99–78) at 7 years. 1 patient had been revised for aseptic loosening of the acetabulum and 1 for deep infection. The mean OHS was 31 (SD 12), the mean SF12 physical-component score (PCS) was 38 (SD 13), the median SAPS was 83 (0–100), and the median SF12 mental-component score (MCS) was 55 (23–65). The graft material became incorporated in all 3 zones of the acetabulum in 23 out of 24 cases that had complete radiographic follow-up.
Interpretation
These medium-term results show that BoneSave is a reliable material for impaction grafting of the acetabulum when used in conjunction with femoral head allograft.
The creation of a stable construct and the restoration of bone stock in the face of bone loss is a challenge in revision hip replacement. Instability and aseptic loosening of the implanted construct account for the majority of revision hip replacement failures (Springer et al. 2009). Impaction grafting of donor allograft was popularized in the 1990s, with promising results (Gie et al. 1993, Slooff et al. 1996). A variety of problems have been identified with donor allograft, including infection (Simonds et al. 1992) and antigenicity (Friedlaender et al. 1984). Issues surrounding the rising incidence of revision (Kurtz et al. 2007), insufficient availability (Galea et al. 1998), and cost of allograft (Leung et al. 2010) have led to the search for suitable alternatives. Experience of the use of impaction allografting alone on the femoral side has included a high incidence of massive early stem subsidence (12%) (Eldridge et al. 1997). These results are not reflected in the excellent results of the originating centers (Schreurs et al. 2006).
We have previously reported the short-term results of impaction grafting of contained acetabular defects with a 50:50 mix of BoneSave, a biphasic tricalcium phosphate/hydroxyapatite (TCP/HA) porous ceramic bone graft substitute, and morcellized femoral head allograft (Blom et al. 2009). TCP and HA have been shown to osseointegrate (Ransford et al. 1998), but the ability of such a porous ceramic bone graft substitute to maintain structural integrity under load has been questioned (Hanft et al. 1995). In conjunction with Stryker (Newbury, UK), our group developed BoneSave for use in impaction grafting. In vitro work has shown that the mix is more stable than allograft alone in impaction grafting (Blom et al. 2002), and in vivo studies in sheep have demonstrated its successful use as a graft extender (Blom et al. 2005). Our previous report described good results in the short term (mean 2 year follow-up); we now report the medium-term results in the same patient cohort.
Methods
43 patients underwent total hip arthroplasty with a 50:50 mix (by volume) of BoneSave and femoral head allograft. This was a consecutive series of patients presenting with contained acetabular defects.
As the inclusion criteria, all the patients included in the study had to have undergone revision arthroplasty due to aseptic loosening with contained acetabular defects requiring grafting, in whom a mix of BoneSave and femoral head allograft was used, between August 2003 and December 2006. Uncontained superolateral defects that required the use of mesh were considered an exclusion criterion; medial defects that could be converted to a contained defect with medial mesh alone were not excluded.
This study was conducted as a service evaluation (National Patient Safety Agency 2009), and as such was exempt from consideration by the local ethics committee. It was conducted in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975 (revised 2000). A questionnaire consisting of the validated self-administered satisfaction scale (Mahomed et al. 2011), the Oxford hip score (OHS) (Dawson et al. 1996), and the Short-Form 12 health survey (Ware et al. 1996) was sent to each patient with a cover letter, and on a second occasion if necessary. An additional question was asked regarding whether the patient would undergo the same surgery again in light of his/her preoperative and postoperative symptoms and function. If the patients did not respond, the hospital records system, picture archiving system (PACS), and primary care record were examined to determine whether they had undergone further surgery.
The latest follow-up radiograph was assessed for radiolucency around the acetabular components according to the method of DeLee and Charnley (1976) and graft incorporation in each zone according to the system described by the Oswestry group (Aulakh et al. 2009). Component migration was assessed with reference to the teardrop and the trans-ischial line; components were considered to have migrated if there was a change of 3 mm or more (Ritter et al. 1999). The presence of BoneSave or allograft in the soft tissues was assessed, as was the degree of heterotopic ossification (HO) (Brooker et al. 1973).
Statistics
Data were checked for normal distribution with the Kolmogorov-Smirnov test. Where the data were normally distributed, central tendency is described as a mean value with standard deviation (SD). Parametric tests (2-tailed, unpaired Student’s t-test) were used for comparisons. Where the data were not normally distributed, central tendency is described as median value with interquartile range (IQR) and range. A Mann-Whitney test was used for comparison when the data was non parametric. Survivorship was analyzed with the Kaplan-Meier method, with 95% confidence intervals (CIs). The data were analyzed with revision of the acetabular component, revision of any part of the construct (acetabular component, bearing, or stem), and reoperation for any reason as endpoints.
Results
43 patients (27 females) met the inclusion criteria, with an index operation (21 on the left side) performed between August 2003 and December 2006. The median patient age at surgery was 74 years (IQR: 63–79; range: 42–90). 15 patients had died during the follow-up period, at a mean time of 38 months post operation (SD 20). 28 patients remained at the time of follow-up (median 80 months; IQR: 74–85; range 69–106). There was no significant difference in age of surgery between the patients who had died and those who were still alive (p = 0.2).
All acetabular defects were grade B according to the classification of Parry et al. (2010). An uncemented acetabular component was implanted during the revision in 34 cases and a cemented implant in 9 cases. A metal-on-polyethylene articulation was used in 35 cases, a metal-on-metal in 4 cases, and a ceramic-on-ceramic in 4 cases. The femoral component was also revised with impaction grafting at index surgery in 11 cases: a cemented component was used in 10 of them and an uncemented component was used in the other case. The uncemented acetabular components used were Duraloc (DePuy, Leeds, UK), Pinnacle (DePuy), or Procotyle (Wright Medical Technology Inc., Arlington, TN). Cemented components were Ogee cups (DePuy).
Construct-survivorship data were available for all patients. The median time since index surgery for all patients was 80 months (IQR: 73–86; range: 69–106). When this was restricted to patients who remained alive, there was no significant difference (p = 1.0). There were 238 person-years of observation. Of the 28 patients who survived until follow-up, 25 returned completed questionnaires.
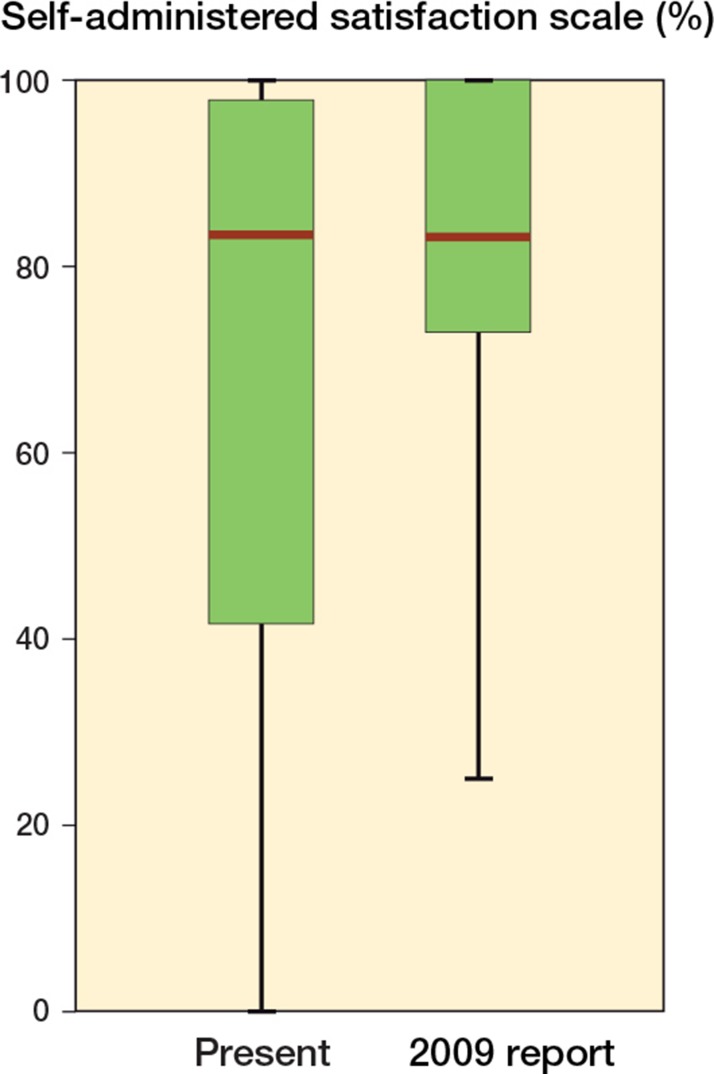
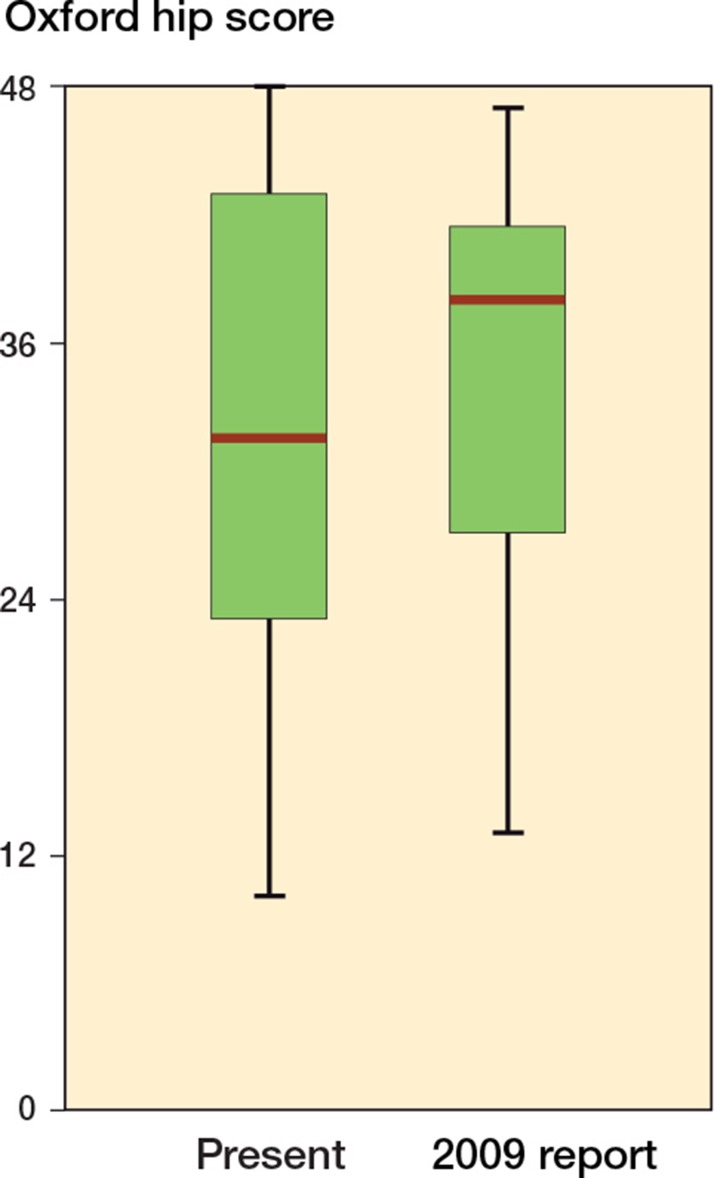
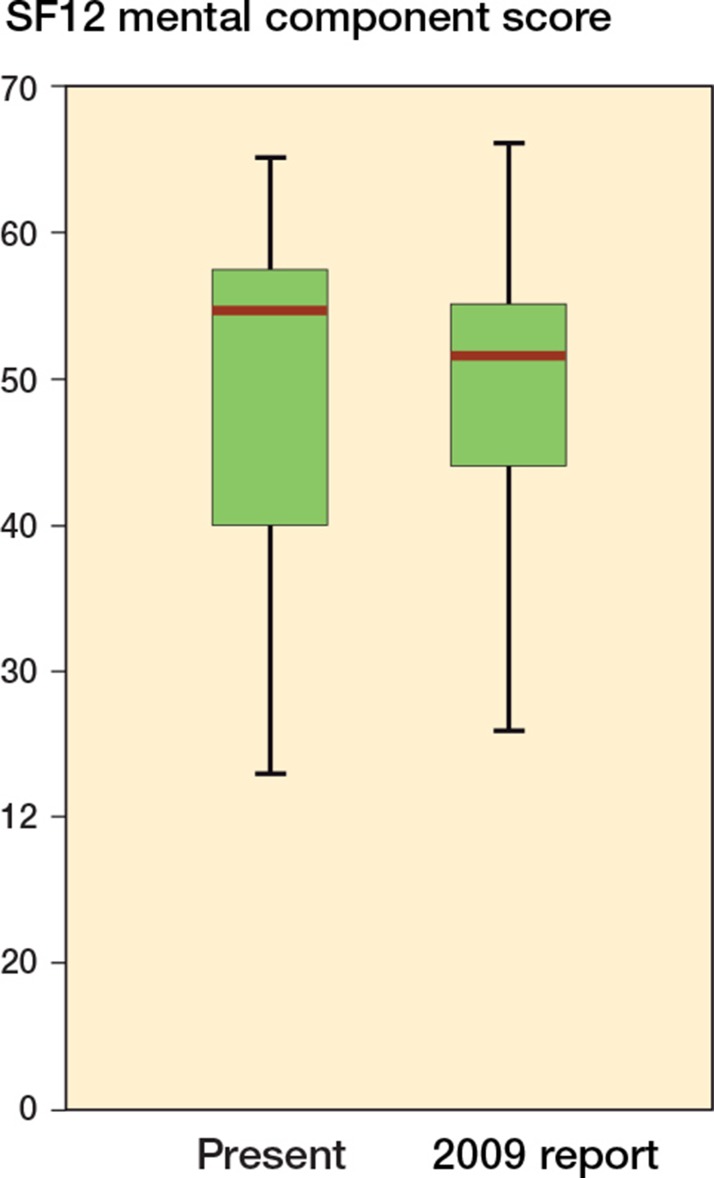
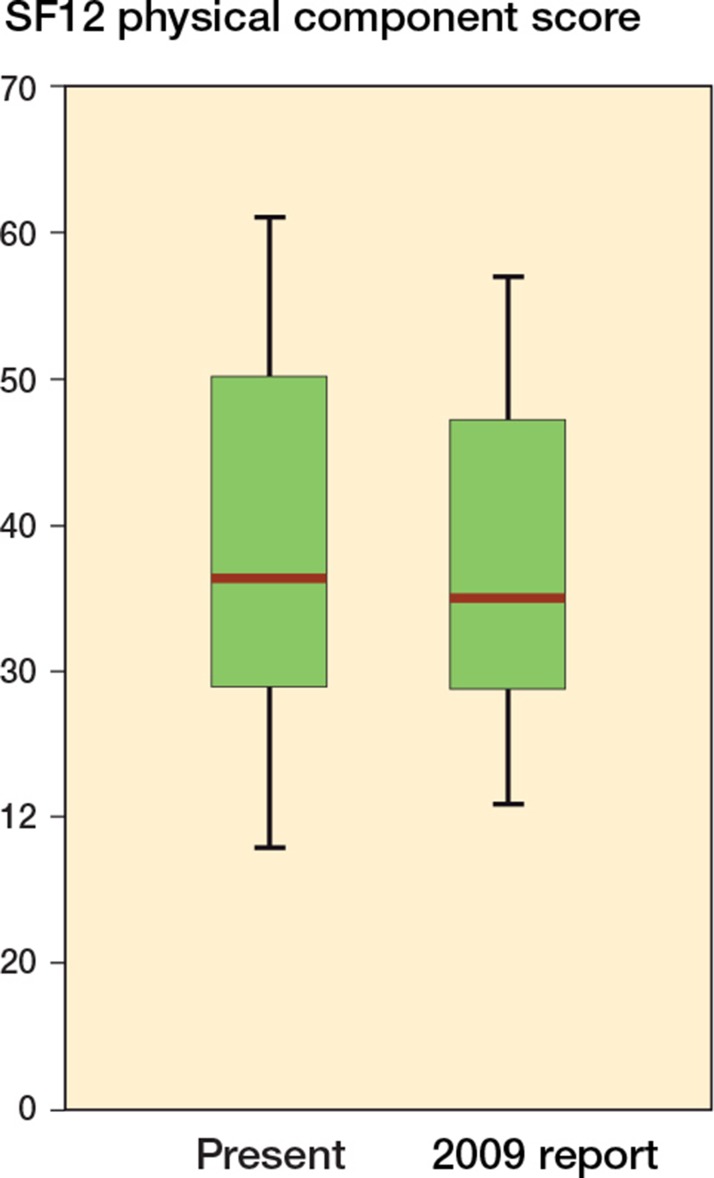
The SAPS and the SF12 mental-component score (MCS) were not normally distributed, but the OHS and the SF12 physical-component score (PCS) were. The mean OHS was 31 (SD 12) and the mean SF12 PCS was 38 (SD 13). The median SAPS was 83 (IQR: 41–98; range: 0–100) and the median SF12 MCS was 55 (IQR: 40–58; range: 23–65). Box-and-whisker plots of the data from this time point and the original report are shown in Figures 1–4. There were no significant differences between the outcome scores from the original report (Blom et al. 2009) and the present report on medium-term follow-up (p-value for SAPS, 0.7; for OHS, 0.7; for SF12 MCS, 0.5; and for SF12 PCS, 0.4). Of the 25 patients who returned questionnaires, 23 stated that they would have the operation performed again, 1 was unsure, and 1 said that he would not. Given the small number of patients who were unsure whether they would have the operation performed again, it was not considered informative to perform correlation calculations. The OHS of the patient who did not want to have the operation performed again was 10 (28 in the previous report) and the patient who was unsure had an OHS of 11 (25 in the previous report).
Figure 1.
Distribution of data on the self-administered satisfaction scale (SAPS). “2009 report” refers to our short-term follow-up report (Blom et al. 2009). The whiskers represent the minimum and maximum values (range).
Figure 2.
Oxford hip score.
Figure 3.
SF12 mental-component score (MCS).
Figure 4.
SF12 physical-component score (PCS).
Radiographic follow-up was available in 24 cases. 1 acetabular construct had failed with excision arthroplasty performed due to deep infection. The 3 patients who did not wish to complete a questionnaire had not had a radiograph performed in the previous 12 months; 1 other patient was too frail to attend for radiography.
In no case had the acetabular component migrated by more then 3 mm. No osteolysis was detectable on the radiographs. Graft material was visible in the soft tissues in 2 of the cases, neither of which had developed HO (grade 0). 17 cases were Brooker grade 0, 3 were grade 1, and 4 were grade 3. The Brooker grade had worsened in comparison to the preoperative radiographs in 3 cases. Graft incorporation was visible in all 3 zones in 23 cases. Graft had not incorporated in zone 2 in 1 case, in which the graft was not loaded medially by the construct. According to the scoring system of Aulakh et al. (2009), the median grade of graft incorporation was 3, indicating consolidation of the graft material (IQR: 1–3; range 1–3). There was no radiolucency in 15 cases. 2 cases had a radiolucency in zone 1 only, 3 cases had a radiolucency in zone 3 only, 1 case in zones 1 and 3, 1 case in zones 2 and 3, and 2 cases had radiolucencies in all 3 zones. The 2 patients with radiolucencies in all 3 zones had OHS of 23 and 27 respectively. In 3 cases, the radiolucency had progressed since the last radiograph.
1 patient who remained alive had undergone revision of the acetabular component since the index revision. This was the previously mentioned excision arthroplasty for deep infection (32 months after the index operation). 1 patient who had died before final follow-up had undergone a further revision of both (acetabular and femoral) components 21 months after implantation of the ceramic bone graft substitute/femoral head allograft mixture. 3 other patients who were still alive had undergone revision of part of the construct. A femoral stem was revised for aseptic loosening at 67 months, a femoral stem was revised for fracture of the stem at 24 months, and there was a revision of the acetabular liner and abductor repair for recurrent dislocation at 3 months. 1 patient who died had undergone a liner exchange due to polyethylene wear at 62 months. There had been no pending revisions for the patients who died.
There had been 5 reoperations not involving part of the construct in patients who were alive at the final follow-up. The reasons for reoperation were a radical debridement for infection (at 1 month, no recurrence), 2 open reductions and internal fixation of traumatic Vancouver C femoral periprosthetic fractures (at 4 and 12 months), and 2 strut graftings of the femur (both at 67 months). There had been 1 reoperation in a patient who had died by the time of the final follow-up; this was a closed reduction for dislocation following a fall (at 4 days, no recurrence).
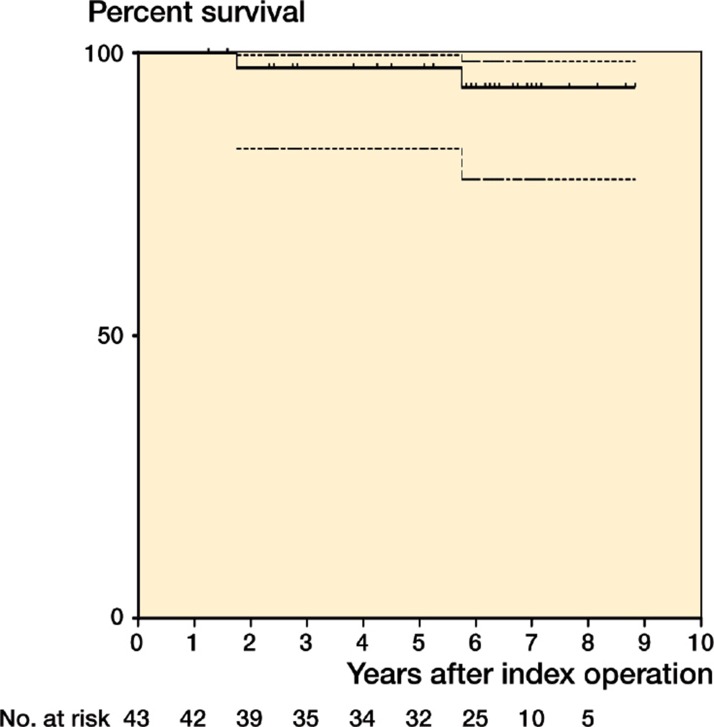
The survivorship of the acetabular component with grafting was 94% (CI 99–78) at 84 months. The numbers at risk are shown below the x-axes in Figures 5–7.
Figure 5.
Survivorship of grafted acetabular constructs, with 95% CI.
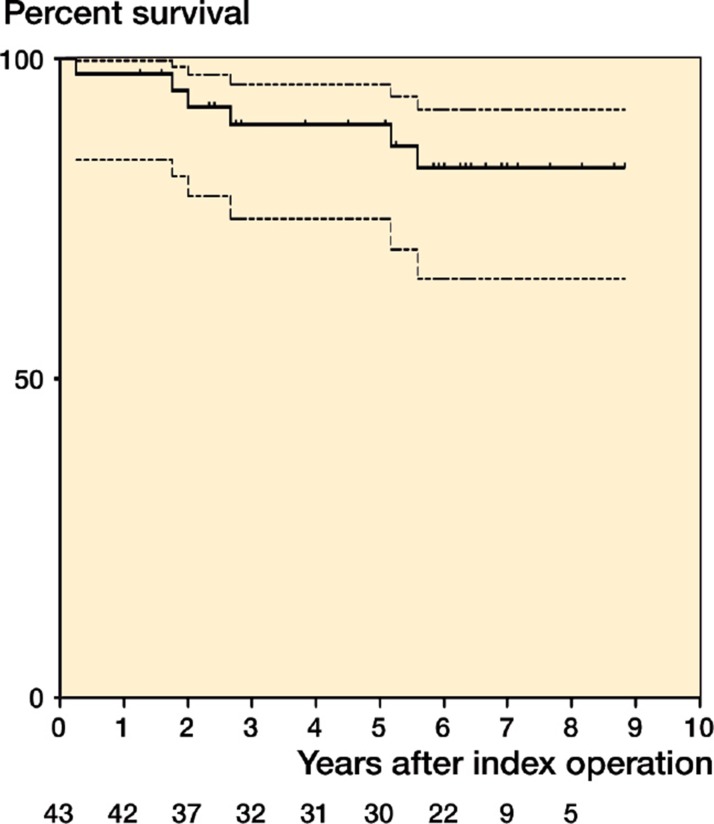
Figure 6.
Survivorship of revision hip replacement constructs, with 95% CI.
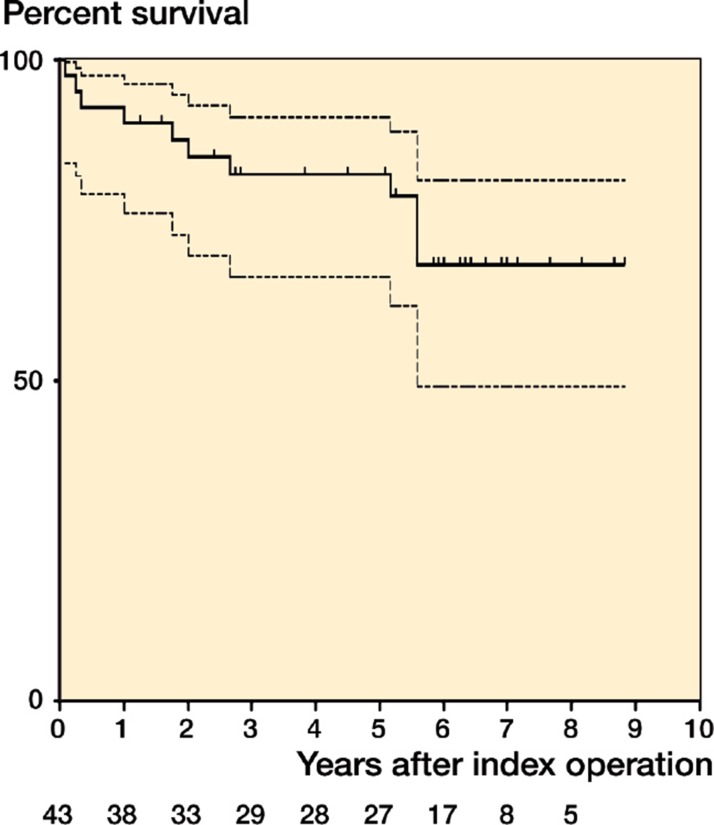
Figure 7.
Survivorship with reoperation for any cause as the endpoint, with 95% CI.
Discussion
The survivorship of the grafted acetabulum in this series is encouraging and appears to confirm our previous findings that a mix of BoneSave and allograft has mechanical properties that are suitable for use in impaction grafting. The median follow-up time of 7 years confirms that our earlier findings were still valid in the medium term.
The case mix in this series was heterogeneous, with a variety of different implants, a variety of fixation strategies, and varying degrees of revision. This reflects the case mix that presents requiring such surgery, and we have therefore not tried to limit our consideration to subgroups. Good results have previously been reported with use of allograft alone in impaction grafting of the acetabulum at primary surgery (Somford et al. 2008), primary and revision surgery (Schreurs et al. 2004, Busch et al. 2011), and revision supplemented with autologous marrow (Deakin and Bannister 2007). High failure rates have been observed in the grafting of larger defects, related to the mechanical properties of the graft (van Haaren et al. 2007).
Since our original report of this cohort (Blom et al. 2009), there were 2 acetabular failures: 1 was for mechanical reasons or reasons relating to failure of the construct, with revision due to aseptic loosening of both the femoral component and the acetabular component, and the other case was a deep infection. The number of revisions involving the construct but not the acetabulum and the number of reoperations not involving the construct has risen since the original report, but this is not surprising given the case mix. Histological analysis of 2 failures from a series of 15 cases impacted with a mixture of allograft and HA/TCP (in a 70:30 ratio) showed little in the way of new bone formation with residual HA/TCP, necrotic bone, viable bone graft, and fibrous tissue. The failures occurred at 16 and 33 months, respectively; data on the surviving cases was not presented (Fujishiro et al. 2008). McNamara et al. (2010) described a mixed series of 48 primary and revision patients who underwent grafting with a 50:50 mixture of allograft and pure HA, with a mean follow-up of 5 years. No failures were reported, but 2 cases had migrated with incorporation of the graft seen in 29 of the cases radiographically. These 2 papers raise the possibility that if HA is mainly used as the graft material, then graft incorporation may not be optimal. The use of apatite-wollastonite glass ceramic in combination with autograft or allograft in a series of 13 patients resulted in migration of 1 out of 11 acetabular components and 1 in 4 femoral components (Kawanabe et al. 1998). The findings were similar in a series of 45 grafts performed with a mixture of allograft and a granulate glass ionomer cement (Engelbrecht et al. 2000). Mean follow-up in this series was 42 months with loosening observed in 10 patients at a mean of 30 months. We feel that these 2 series highlight the critical nature of the mechanical properties of the material used in impaction grafting (Blom et al. 2002).
The OHS values achieved in our series are similar to those reported for a large series of all-revision hips with patients of similar age (Field et al. 2005) when adjusted for the different methods of scoring the OHS (Murray et al. 2007). There was a non-significant decline in OHS from our first report. The satisfaction as recorded by the SAPS and the proportion of patients who stated that they would undergo the operation again (23 of 25) is encouraging. Although there did appear to be an association between those who had poor OHS scores and those who would not, or were unsure of whether they would have the operation again, the subgroups were too small to allow meaningful comparison.
The incidence of infection in our series (1 deep infection requiring excision arthroplasty and 1 superficial infection requiring soft tissue debridement only) was similar to that in other published series of similar size (Engelbrecht et al. 2000, McNamara et al. 2010). Given the nature of revision hip replacement, complete eradication of infection will always prove difficult, if not impossible, but we feel that this incidence of infection is not excessive in this difficult group of patients—although it is higher than our previously reported incidence for all revision hip replacements (Blom et al. 2003).
There was a high incidence of graft incorporation in patients for whom radiographs were available in our series, which was similar to the best results previously reported (Oonishi et al. 1997). The pore size of the material used has been shown to be optimal for osseoconduction (Tsuruga et al. 1997). The failure of incorporation of the graft medially in a patient in whom this area of graft was not loaded shows that loading of the graft remains essential for incorporation to occur. The incidence of radiolucencies in our series remains the subject of continuous follow-up and observation. While the presence of radiolucency suggests that the interface has not been sealed (Schmalzried et al. 1992b) at medium-term follow-up, this does not appear to have been a cause of failure. Given that we usually used polyethylene articulations, we would expect to see a rising incidence of failure of the acetabular components if this is indeed a pathway for the ingress of wear debris (Schmalzried et al. 1992a).
The present study does have limitations; we have no control or comparator group to allow us to determine the effect of our use of this graft material on the results observed. Similarly, the use of standardized components for revision surgery would have allowed us to more accurately determine the influence of the graft material.
In summary, BoneSave—a biphasic tricalcium phosphate/hydroxyapatite porous ceramic bone graft substitute—is a satisfactory material when used in combination with femoral head allograft during acetabular impaction grafting at revision hip surgery. It is associated with low rates of revision of the host bone-graft-acetabular component construct, with low rates of infection, and with high rates of graft incorporation when the graft is appropriately loaded by the construct.
Acknowledgments
MRW: data collection, radiographic analysis, and statistical analysis. PJD: data collection and statistical analysis. JCJW: surgery. AWB: data collection, radiographic analysis, and surgery. All the authors were involved in the design and performance of the study, and in manuscript preparation.
No competing interests declared.
References
- Anon National Patient Safety Agency, National Research Ethics Service: Defining research. http://www.nres.nhs.uk/EasySiteWeb/GatewayLink.aspx?alId=355 2009 Dec; 0987. Available at:
- Aulakh TS, Jayasekera N, Kuiper J-H, Richardson JB. Long-term clinical outcomes following the use of synthetic hydroxyapatite and bone graft in impaction in revision hip arthroplasty. Biomaterials. 2009;30(9):1732–8. doi: 10.1016/j.biomaterials.2008.12.035. [DOI] [PubMed] [Google Scholar]
- Blom AW, Grimm B, Miles AW, Cunningham JL, Learmonth ID. Subsidence in impaction grafting: the effect of adding a ceramic bone graft extender to bone. Proc Inst Mech Eng (Part H) 2002;216(4):265–70. doi: 10.1243/09544110260138754. [DOI] [PubMed] [Google Scholar]
- Blom AW, Taylor AH, Pattison G, Whitehouse SL, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg (Br) 2003;85(7):956–9. doi: 10.1302/0301-620x.85b7.14095. [DOI] [PubMed] [Google Scholar]
- Blom AW, Cunningham JL, Hughes G, Lawes TJ, Smith N, Blunn G, Learmonth ID, Goodship AE. The compatibility of ceramic bone graft substitutes as allograft extenders for use in impaction grafting of the femur. J Bone Joint Surg (Br) 2005;87(3):421–5. doi: 10.1302/0301-620x.87b3.14337. [DOI] [PubMed] [Google Scholar]
- Blom AW, Wylde V, Livesey C, Whitehouse MR, Eastaugh-Waring S, Bannister GC, Learmonth ID. Impaction bone grafting of the acetabulum at hip revision using a mix of bone chips and a biphasic porous ceramic bone graft substitute. Acta Orthop. 2009;80(2):150–4. doi: 10.3109/17453670902884767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker AF, Bowerman JW, Robinson BG, Riley L. Jr. Ectopic ossification following total hip replacement: Incidence and a method of classification. J Bone Joint Surg (Am) 1973;55(8):1629–32. [PubMed] [Google Scholar]
- Busch V J JF, Gardeniers J WM, Verdonschot N, Slooff T J JH, Schreurs BW. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old: a concise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg (Am) 2011;93(4):367–71. doi: 10.2106/JBJS.I.01532. [DOI] [PubMed] [Google Scholar]
- Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg (Br) 1996;78(2):185–90. [PubMed] [Google Scholar]
- Deakin DE, Bannister GC. Graft incorporation after acetabular and femoral impaction grafting with washed irradiated allograft and autologous marrow. J Arthroplasty. 2007;22(1):89–94. doi: 10.1016/j.arth.2006.02.162. [DOI] [PubMed] [Google Scholar]
- DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;(121):20–32. [PubMed] [Google Scholar]
- Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;12(5):535–40. doi: 10.1016/s0883-5403(97)90176-5. [DOI] [PubMed] [Google Scholar]
- Engelbrecht E, Foerster von G, Delling G. Ionogran in revision arthroplasty. J Bone Joint Surg (Br) 2000;82(2):192–9. [PubMed] [Google Scholar]
- Field RE, Cronin MD, Singh PJ. The Oxford hip scores for primary and revision hip replacement. J Bone Joint Surg (Br) 2005;87(5):618–22. doi: 10.1302/0301-620X.87B5.15390. [DOI] [PubMed] [Google Scholar]
- Friedlaender GE, Strong DM, Sell KW. Studies on the antigenicity of bone. II. Donor-specific anti-HLA antibodies in human recipients of freeze-dried allografts. J Bone Joint Surg (Am) 1984;66(1):107–12. [PubMed] [Google Scholar]
- Fujishiro T, Nishikawa T, Takahiro N, Takikawa S, Saegusa Y, Kurosaka M, Bauer TW. Histologic analysis of allograft mixed with hydroxyapatite-tricalcium phosphate used in revision femoral impaction bone grafting. Orthopedics. 2008;31(3):277. doi: 10.3928/01477447-20080301-12. [DOI] [PubMed] [Google Scholar]
- Galea G, Kopman D, Graham BJ. Supply and demand of bone allograft for revision hip surgery in Scotland. J Bone Joint Surg (Br) 1998;80(4):595–9. doi: 10.1302/0301-620x.80b4.8240. [DOI] [PubMed] [Google Scholar]
- Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg (Br) 1993;75(1):14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- Hanft JR, Sprinkle RW, Surprenant MS, Werd MB. Implantable bone substitute materials. Clin Podiatr Med Surg. 1995;12(3):437–55. [PubMed] [Google Scholar]
- Kawanabe K, Iida H, Matsusue Y, Nishimatsu H, Kasai R, Nakamura T. A-W glass ceramic as a bone substitute in cemented hip arthroplasty: 15 hips followed 2-10 years. Acta Orthop Scand. 1998;69(3):237–42. doi: 10.3109/17453679809000922. [DOI] [PubMed] [Google Scholar]
- Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Kärrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg (Am) (Suppl 3) 2007;89:144–51. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- Leung H-B, Fok M W-M, Chow L C-Y, Yen C-H. Cost comparison of femoral head banking versus bone substitutes. J Orthop Surg (Hong Kong) 2010;18(1):50–4. doi: 10.1177/230949901001800111. [DOI] [PubMed] [Google Scholar]
- Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:1–6. doi: 10.1155/2011/591253. DOI: 10.1155/2011/591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara I, Deshpande S, Porteous M. Impaction grafting of the acetabulum with a mixture of frozen, ground irradiated bone graft and porous synthetic bone substitute (Apapore 60) J Bone Joint Surg (Br) 2010;92(5):617–23. doi: 10.1302/0301-620X.92B5.23044. [DOI] [PubMed] [Google Scholar]
- Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J. The use of the Oxford hip and knee scores. J Bone Joint Surg (Br) 2007;89(8):1010–4. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- Oonishi H, Iwaki Y, Kin N, Kushitani S, Murata N, Wakitani S, Imoto K. Hydroxyapatite in revision of total hip replacements with massive acetabular defects: 4- to 10-year clinical results. J Bone Joint Surg (Br) 1997;79(1):87–92. doi: 10.1302/0301-620x.79b1.1290. [DOI] [PubMed] [Google Scholar]
- Parry MC, Whitehouse MR, Mehendale SA, Smith LK, Webb JC, Spencer RF, Blom AW. A comparison of the validity and reliability of established bone stock loss classification systems and the proposal of a novel classification system. Hip Int. 2010;20(1):50–5. doi: 10.1177/112070001002000108. [DOI] [PubMed] [Google Scholar]
- Ransford AO, Morley T, Edgar MA, Webb P, Passuti N, Chopin D, Morin C, Michel F, Garin C, Pries D. Synthetic porous ceramic compared with autograft in scoliosis surgery. A prospective, randomized study of 341 patients. J Bone Joint Surg (Br) 1998;80(1):13–8. doi: 10.1302/0301-620x.80b1.7276. [DOI] [PubMed] [Google Scholar]
- Ritter MA, Zhou H, Keating CM, Keating EM, Faris PM, Meding JB, Berend ME. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg (Br) 1999;81(6):982–6. doi: 10.1302/0301-620x.81b6.9634. [DOI] [PubMed] [Google Scholar]
- Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg (Am) 1992a;74(6):849–63. [PubMed] [Google Scholar]
- Schmalzried TP, Kwong LM, Jasty M, Sedlacek RC, Haire TC, O’Connor DO, Bragdon CR, Kabo JM, Malcolm AJ, Harris WH. The mechanism of loosening of cemented acetabular components in total hip arthroplasty. Analysis of specimens retrieved at autopsy. Clin Orthop. 1992b;274:60–78. [PubMed] [Google Scholar]
- Schreurs BW, Busch V J JF, Welten ML, Verdonschot N, Slooff T J JH, Gardeniers J WM. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old. J Bone Joint Surg (Am) 2004;86(11):2385–92. doi: 10.2106/00004623-200411000-00004. [DOI] [PubMed] [Google Scholar]
- Schreurs BW, Arts J JC, Verdonschot N, Buma P, Slooff TJ, Gardeniers JWM. Femoral component revision with use of impaction bone-grafting and a cemented polished stem. Surgical technique. J Bone Joint Surg (Am) (Suppl 1 Pt 2) 2006;88:259–74. doi: 10.2106/JBJS.F.00340. [DOI] [PubMed] [Google Scholar]
- Simonds RJ, Holmberg SD, Hurwitz RL, Coleman TR, Bottenfield S, Conley LJ, Kohlenberg SH, Castro KG, Dahan BA, Schable CA. Transmission of human immunodeficiency virus type 1 from a seronegative organ and tissue donor. N Engl J Med. 1992;326(11):726–32. doi: 10.1056/NEJM199203123261102. [DOI] [PubMed] [Google Scholar]
- Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop. 1996;(324):108–15. doi: 10.1097/00003086-199603000-00013. [DOI] [PubMed] [Google Scholar]
- Somford MP, Bolder S BT, Gardeniers J WM, Slooff T J JH, Schreurs BW. Favorable survival of acetabular reconstruction with bone impaction grafting in dysplastic hips. Clin Orthop. 2008;466(2):359–65. doi: 10.1007/s11999-007-0048-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop. 2009;467(1):166–73. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuruga E, Takita H, Itoh H, Wakisaka Y, Kuboki Y. Pore size of porous hydroxyapatite as the cell-substratum controls BMP-induced osteogenesis. J Biochem. 1997;121(2):317–24. doi: 10.1093/oxfordjournals.jbchem.a021589. [DOI] [PubMed] [Google Scholar]
- van Haaren EH, Heyligers IC, Alexander F GM, Wuisman P I JM. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg (Br) 2007;89(3):296–300. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller SD. A. 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]