Abstract
Background and purpose
Loss of bone stock remains a challenge in revision hip surgery. Grafting with allograft is well established, but there are problems with availability, cost, infection, antigenicity, reproducibility, and stability of the created construct. BoneSave is a biphasic porous ceramic consisting of sintered 80% tricalcium phosphate and 20% hydroxyapatite. In vitro and in vivo studies, including its use mixed with allograft, have shown good results in impaction grafting. This is the first reported series of its use alone in impaction grafting of the acetabulum.
Methods
Methods We conducted a retrospective review of a cohort of 43 consecutive patients undergoing impaction grafting of contained acetabular defects by multiple surgeons at a single centre. All patients received uncemented acetabular components. They were followed up radiographically, together with self-reported satisfaction scale (SAPS), Oxford hip score (OHS), and Short-Form 12 (SF12) health survey. Kaplan-Meier survivorship analysis was performed with revision of the acetabular component, revision of any part of the construct, and reoperation as endpoints.
Results
The fate of all cases was known. Mean follow-up was 4 years. 5 patients died during follow-up, with their constructs in situ. The survivorship of the acetabular component was 98% (95% CI: 85–100) at 7 years. 1 acetabular component was revised for infection and there was 1 radiographic acetabular failure. The median OHS was 36 (6–48), the median SF12 PCS was 36 (14–57), the median SAPS was 75 (0–100), and the median SF12 MCS was 50 (23–64). The graft material had incorporated in all 3 zones of the acetabulum in 33 out of 37 cases with complete radiographic follow-up.
Interpretation
Medium-term results show that BoneSave alone is a reliable material for impaction grafting of contained defects in the acetabulum at revision surgery.
Impaction grafting to restore bone stock and create a stable construct was made popular by the Exeter and Nijmegen groups (Gie et al. 1993, Slooff et al. 1996). Reported problems with allograft such as infection (Simonds et al. 1992), antigenicity (Friedlaender et al. 1984), lack of availability (Galea et al. 1998), and cost (Tomford et al. 1981) have led to the search for bone graft substitutes. Femoral head allograft has been shown to be more expensive than commercially available bone substitutes (per gram) in some countries (Leung et al. 2010).
Hydroxyapatite and tricalcium phosphates osseointegrate (Itokazu et al. 1996, Ransford et al. 1998) but their ability to maintain structural integrity under load has been questioned (Hanft et al. 1995). In conjunction with Stryker (Newbury, UK), our group has developed a biphasic ceramic bone graft substitute, called BoneSave, specifically for use in impaction grafting in revision hip surgery. Mechanical engineering studies have demonstrated that BoneSave combined with allograft is more stable and more reproducible than allograft alone in an impaction grafting model (Blom et al. 2002). Furthermore, stability and reproducibility are directly proportional to the ratio of BoneSave to allograft. Studies in sheep have shown the clinical effectiveness of BoneSave when used as a bone graft extender (Blom et al. 2005). We have already reported good results using BoneSave combined with allograft in acetabular impaction grafting in revision hip surgery in patients (Blom et al. 2009, Whitehouse et al. 2013). Until now, there have been no reports of BoneSave being used without allograft in impaction grafting. Here we report the medium-term follow-up of a cohort of patients undergoing grafting of acetabular defects with BoneSave only, a biphasic tricalcium phosphate/hydroxyapatite porous ceramic bone graft substitute that is sintered at high temperature to allow the necessary mechanical properties to be used in impaction grafting.
Patients and methods
43 patients (26 female) underwent revision hip arthroplasty with grafting of BoneSave bone substitute alone between July 2004 and October 2010. Before July 2004, BoneSave had been used in our unit for acetabular grafting in combination with femoral head allograft. This was a series of patients presenting with contained acetabular defects that required grafting. Medial defects that were supplemented with a mesh in the floor were included but other uncontained defects that required the use of a rim mesh were excluded.
In 35 cases, the femoral component was also revised at the time of index surgery. In 25 cases, a cemented femoral component was inserted (15 C-stem AMTs (DePuy International, Leeds, UK); 6 CPTs (Zimmer Inc., Warsaw, IN); 4 Exeter stems (Stryker, Newbury, UK), and in 10 cases an uncemented component (9 KAR stems and 1 S-ROM (DePuy). All acetabular defects were grade B according to the classification of Parry et al. (2010). The median percentage of host bone contact with the implanted component was 70% (IQR 55–80, range 0–90). In all cases, the acetabular component inserted was uncemented (28 Pinnacle and 4 Duraloc (DePuy); 3 Trident, 2 ABG, and 3 Omnifit (Stryker); 2 Procotyle (Wright Medical Technology Inc., Arlington, TN) and 1 Trilogy (Zimmer)). In 38 of the cases, supplementary screw fixation was used for the acetabular component following assessment of stability by the treating surgeon. A median of 3 (0–6) screws were used. In 18 cases, a metal-on-polyethylene bearing was used, in 18 a metal-on-metal bearing was used, and in 7 a ceramic-on-ceramic bearing was used.
Median age at surgery was 73 (28–92) years. 5 patients died during the follow-up period, at a median age of 84 (80–94) years. The period of follow-up was normally distributed. For patients who remained alive at final follow-up, the mean time was 51 months (SD 19). When patients who had died were included, the mean follow-up until final follow-up or death was 49 months (SD 20). There was a total of 176 person years of observation. Of the 38 patients who remained alive at final follow-up, 36 of them returned completed questionnaires (see below).
This study was conducted as a service evaluation (National Research Ethics Service 2007). A questionnaire consisting of a validated self-administered patient satisfaction scale (SAPS) (Mahomed et al. 2011), an Oxford hip score (OHS) (Dawson et al. 1996), and a Short-Form 12 (SF12) health survey (Ware et al. 1996) was sent to each patient, with a cover letter, on 2 separate occasions. An additional question was asked: whether the patient would undergo the same surgery again in light of their preoperative and postoperative symptoms and function. If patients did not respond, the hospital records system, picture archiving system (PACS), and the primary care records were used to determine whether they had undergone further surgery.
Radiographic analysis was carried out by MRW and AWB. Radiolucencies around the acetabular component on the latest follow-up radiograph were assessed according to the method of DeLee and Charnley (1976). The presence or absence of graft incorporation in each of these zones was recorded according to the system described by the Oswestry group (Aulakh et al. 2009). Components were considered to have migrated if they had moved by 3 mm or more from the inter-tear drop line or trans-ischial line where this was obscured (Ritter et al. 1999). The grade of heterotopic ossification, according to the system of Brooker et al. (1973), and the presence of BoneSave in the soft tissues were recorded.
Statistics
The distribution of data was checked for normality using the Kolmogorov-Smirnov test. Where the data were normally distributed, central tendency is given as mean with SD and parametric tests were used (2-tailed unpaired Student’s t-test). Where the data were not normally distributed, central tendency is given as median with range; and in such cases non-parametric tests were used. Correlation was calculated using a Spearman rank test. Survivorship was analyzed with the Kaplan-Meier method, with 95% confidence intervals (CIs). The data were analyzed with revision of the acetabular component, revision of any part of the construct (acetabular component, bearing, or stem), and reoperation for any reason as endpoints.
Results
The outcome scores were not normally distributed. The median SAPS was 75 (0–100). The median OHS was 36 (6–48). The median SF12 PCS was 36 (14–57) and the median SF12 MCS was 50 (23–64). 30 of the patients said they would have the operation again, 3 were unsure, and 3 said they would not undergo the operation again. There was no correlation between whether the patients would have the operation performed again and their OHS at final follow-up (–0.43).
Radiographic follow-up was available in 37 cases. 1 case had migrated and was considered a radiographic failure, but the patient was not fit to undergo further revision surgery. No osteolysis or accelerated polyethylene wear was observed. Graft incorporation had occurred in all 3 zones in 33 cases. In 2 cases, graft incorporation had not occurred in any zone and in 2 cases graft incorporation had not occurred in zone 2, where the graft was not loaded due to rim fixation of the acetabular component. According to the graft incorporation grading system of Aulakh et al. (2009), the median graft incorporation score was 3—indicating consolidation of the graft material (IQR 2–3, range 0–3) (Figures 1 and 2).
Figure 1.
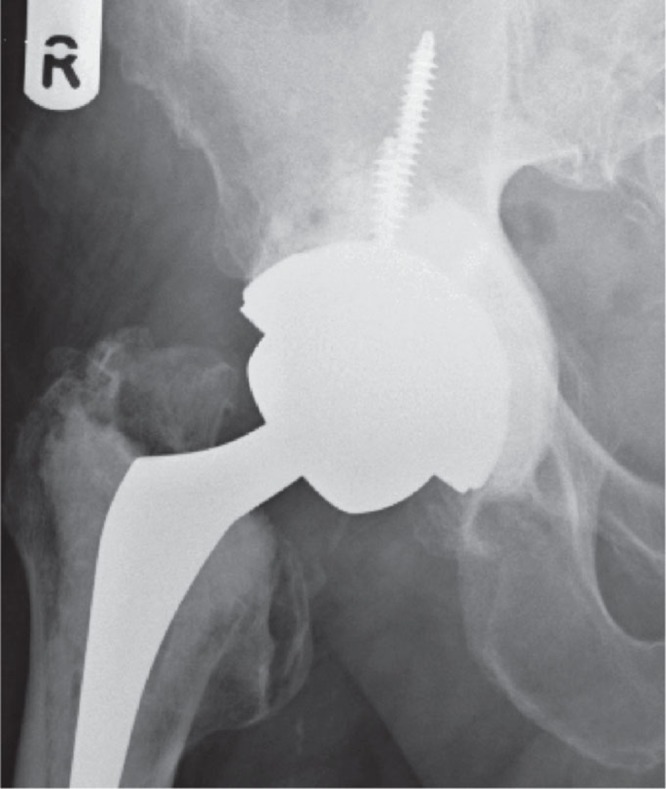
Radiograph of an illustrative case 1 year post operation.
Figure 2.

Radiograph of an illustrative case 4 years post operation.
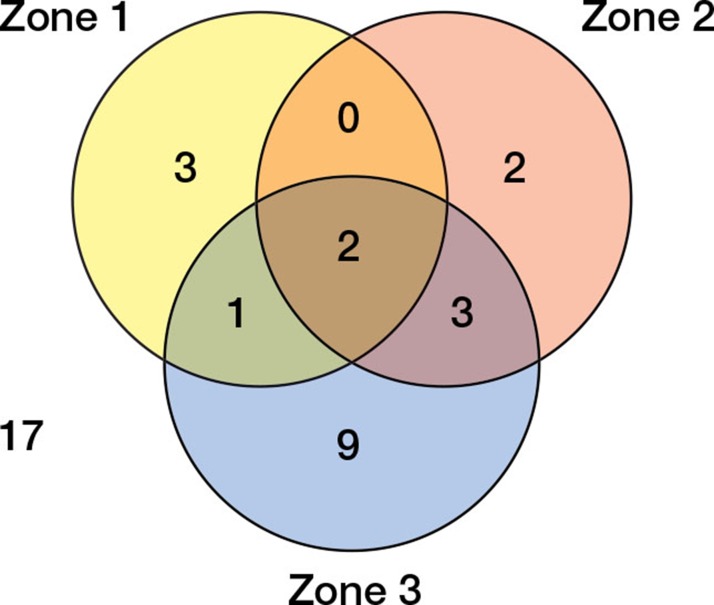
Brooker grade 0 was recorded in 21 cases, grade 1 in 12 cases, grade 2 in 2 cases, and grade 3 in 2 cases. In 4 cases, the Brooker grade was worse than preoperatively and in 2 cases the grade had decreased. Graft was visible in the soft tissues in 2 cases: 1 was Brooker grade 0 and 1 was grade 1, and had been preoperatively. Of the 37 cases with radiographic follow-up, no radiolucency was observed in 17 cases (Figure 3). 1 of the 2 cases with radiolucency in all 3 zones was the radiographic failure already described; the other case had an OHS of 29.
Figure 3.
Distribution of radiolucencies by acetabular zone.
1 acetabular component was revised for infection during the follow-up period (16 months after the index operation). 1 patient required revision of the femoral stem only for aseptic loosening (5.5 years). 6 patients required reoperations that did not involve revision of any part of the construct. 2 radical debridements were performed for infection (at 1 week and 3 weeks), 2 femurs required supplementary strut grafting of the femur (at 2 weeks and 5.5 years), 1 patient required closed reduction for dislocation following a fall (at 1 week), and 1 patient underwent an examination under anesthetic to assess subluxation (at 1.5 years); the hip was found to be stable.
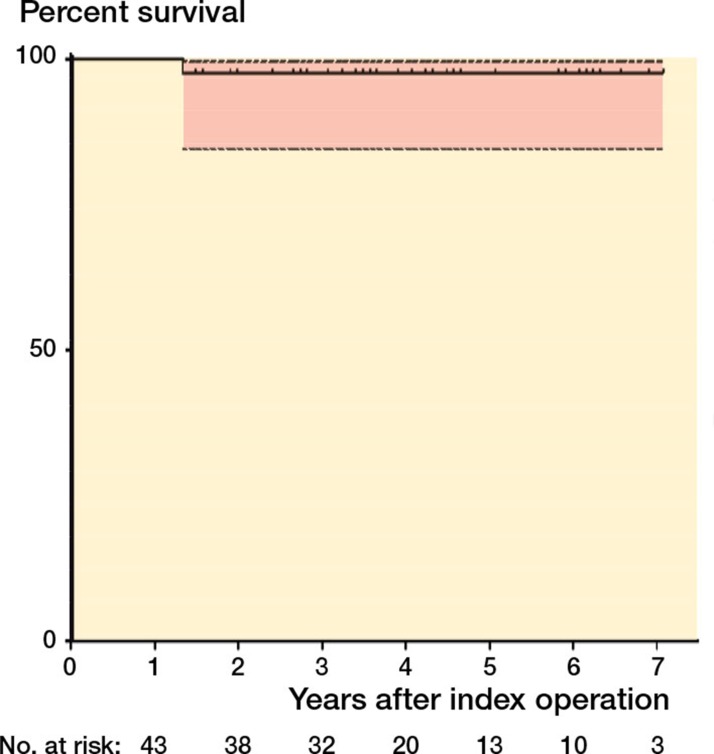
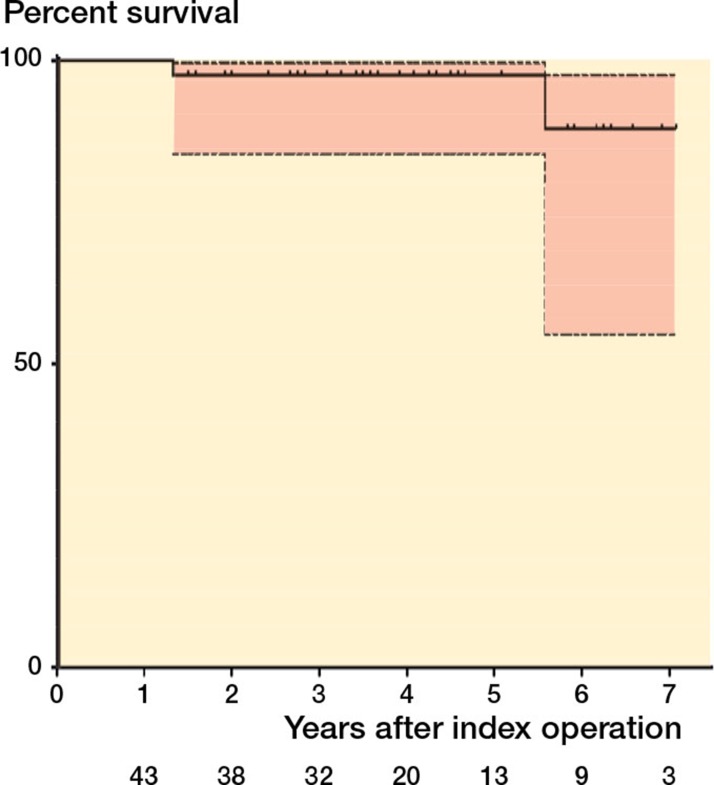
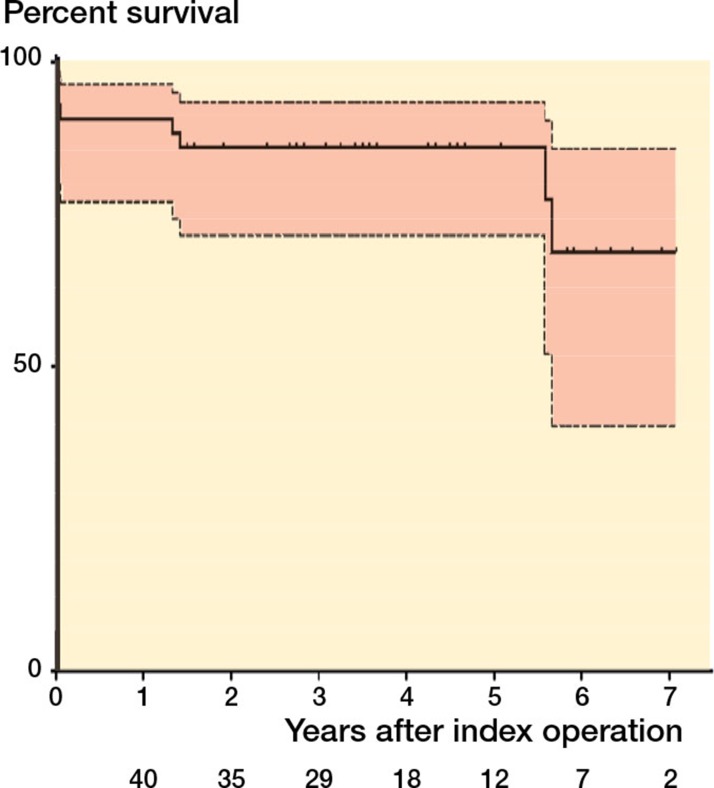
The survivorship of the acetabular component with grafting was 98% (CI: 85–100) at 85 months (Figures 4–6).
Figure 4.
Kaplan–Meier analysis with 95% confidence intervals and number at risk with revision of the acetabular component as the endpoint.
Figure 5.
Kaplan–Meier analysis with 95% confidence intervals and number at risk with revision of any part of the construct as the endpoint.
Figure 6.
Kaplan–Meier analysis with 95% confidence intervals and number at risk with reoperation for any cause as the endpoint.
Discussion
The results presented here are short- to medium-term, and must therefore be interpreted with caution. The heterogeneous case mix makes generalization of the results to patients undergoing revision hip replacement complex, but this is a reflection of the patient population that presents for such procedures, as has been observed in other reports. In the medium to long term, good results have been reported for impaction grafting of allograft in the acetabulum in conjunction with the use of cemented components in primary hip replacement (Somford et al. 2008), primary and revision surgery (Schreurs et al. 2004, Busch et al. 2011), and revision with supplementation by use of autologous marrow and uncemented components (Deakin and Bannister 2007), but there may a limit to the size of the defect that can be grafted (van Haaren et al. 2007).
We have previously reported our experience of the use of BoneSave in a 1:1 combination with allograft (Blom et al. 2009, Whitehouse et al. 2013), at a mean follow-up of 24 months and 7 years. There were no revisions or migration, with high patient satisfaction at the first follow-up. There were 2 revisions at the later follow-up, 1 for aseptic loosening and 1 for infection. Fujishiro et al. (2008) reported a series of 15 patients grafted with a 1:1 mix of allograft and a graft substitute with a much higher proportion of hydroxyapatite than used in BoneSave; 2 failures were reported, 1 at 16 months and 1 at 33 months. McNamara et al. (2010) did not report any revisions, but improved function and graft incorporation in 60% of hips grafted with a 1:1 mix of allograft and pure hydroxyapatite in a series of 48 patients with a mean follow-up period of 5 years. Migration was observed in 2 acetabular components. Kawanabe et al. (1998) used an apatite-wollastonite glass ceramic in combination with autograft or allograft in a series of 13 patients. Migration was seen in 1 out of 11 acetabular revisions and 1 out of 4 femoral revisions. The findings of Englbrecht et al. (2000) were similar in a series of 45 graftings with a mix of allograft and a granulate glass ionomer cement. Loosening was observed in 10 patients at a mean time of 30 months after revision in a series of 45 patients followed for a mean of 42 months.
A number of authors have reported the results of the use of bone graft substitutes on their own, rather than in combination with allograft or autograft. Oonishi et al. (1997) used hydroxyapatite granules to graft massive acetabular bone deficiencies in 40 patients undergoing revision. 3 patients had loosening and migration, with the remaining 37 showing good outcomes and bonding of the hydroxyapatite to bone. Schwartz and Bordei (2005) reported the use of biphasic phosphor-calcium ceramics for void filling (granules) and reconstruction of segmental defects (preformed shapes). At a mean of 5.5 years of follow-up, integration of ceramic with host bone was observed in all 32 hips. Femoral component subsidence of between 5 and 14 mm was observed in 8 cases. At 1-year follow-up, Egawa et al. (2009) found substantial new mineralization in 10 patients with symptomatic osteolysis who were treated with calcium sulfate bone graft substitute.
The OHS achieved by our patients was similar to those in published large series when adjustment was made for the different scoring method for the OHS used (Field et al. 2005). The proportion of patients who stated that they would undergo the operation again is satisfying, and reflects the SAPS achieved. It is surprising to note that there was a negative correlation between OHS and whether a patient would undergo the operation again, but this is probably a reflection of individual patient variation and of the relatively small sample size.
There was 1 case of revision of part of the construct—for infection—in this series, which is consistent with our previously reported experience (Blom et al. 2003). When soft tissue debridements for infection were taken into account, the incidence in this series was higher than in our previous experience. The use of bone graft substitute alone does not eliminate the risk of infection in this high-risk group of patients, which is not surprising. The rates of infection in our series are similar to those reported by authors for similar-sized series (Engelbrecht et al. 2000, McNamara et al. 2010).
Given the small numbers, formal testing of correlation was not determined to be useful. It is interesting to note that in the 2 cases with graft material visible in the soft tissues, the Brooker grade had not changed from before revision. Given that BoneSave is capable of incorporation and is osteoconductive but not osteogenic, and does not contain growth factors capable of osteoinduction other than those present in the host tissue, this finding fits with our understanding of the properties of bone graft materials.
There was a high incidence of graft incorporation in this series (33 of 37 cases with complete radiographic follow-up). Failure of graft incorporation in all 3 zones was not necessarily associated with clinical failure, with 1 case being determined to have failed but the other being clinically successful. The need to create a stable construct with loading of the grafted material is emphasized by the lack of incorporation of the graft in the 2 cases where rim fit had been achieved with the acetabular component. The incidence of graft incorporation was better than in other reported series (McNamara et al. 2010) and similar to the best reported results (Oonishi et al. 1997). The incidence of radiolucencies around the acetabular components in our series remains a cause for concern that we will continue to monitor with further follow-up. Although it is reassuring that implant migration has not occurred in these implants at medium-term follow-up—whereas in series where catastrophic failure has been reported with impaction grafting, this has occurred within a year of surgery (Eldridge et al. 1997, Charalambides et al. 2005)—it is possible that these radiolucencies could represent an interface that is not sealed, and therefore be susceptible to ingress of wear debris (Schmalzried et al. 1992) or be predictive of future migration (Ritter et al. 1999).
Limitations of our study include the lack of comparator groups without grafting and with the use of graft substitute mixed with autograft or allograft. We hope that surgeons will find our data useful to inform practice in the choice of graft material and add to the body of available evidence. The lack of standardized components and the range of follow-up is a reflection of the patients that present for revision surgery with bone loss, and the variety of surgical techniques required to address this. Acetabular defects were classified according to the system of Parry et al. (2010); we find this system useful, as it helps to guide our treatment strategy. We have not attempted to classify the defects in this series using other recognized classification systems. The lack of correlation with intraoperative findings (Gozzard et al. 2003) limits the usefulness of such classification in a study of this nature. A high proportion of our patients received metal-on-metal bearing surfaces, and this may bias towards worse outcomes (Smith et al. 2012).
In summary, we have found that BoneSave, a biphasic tricalcium phosphate/hydroxyapatite porous ceramic bone graft substitute, when used without augmentation with autograft, allograft, or autologous marrow, to be reliable for grafting of contained defects of the acetabulum. It is associated with a low rate of failure and complications and it osseointegrates when suitably loaded by the construct.
Acknowledgments
MRW: data collection, radiographic analysis, and statistical analysis. PJD: data collection and statistical analysis. JCJW: surgery. AWB: data collection, radiographic analysis, and surgery. All the authors were involved in the study design and in conducting the study, and in manuscript preparation.
No competing interests declared.
References
- Aulakh TS, Jayasekera N, Kuiper J-H, Richardson JB. Long-term clinical outcomes following the use of synthetic hydroxyapatite and bone graft in impaction in revision hip arthroplasty. Biomaterials. 2009;30(9):1732–8. doi: 10.1016/j.biomaterials.2008.12.035. [DOI] [PubMed] [Google Scholar]
- Blom AW, Grimm B, Miles AW, Cunningham JL, Learmonth ID. Subsidence in impaction grafting: the effect of adding a ceramic bone graft extender to bone. Proc Inst Mech Eng H. 2002;216(4):265–70. doi: 10.1243/09544110260138754. [DOI] [PubMed] [Google Scholar]
- Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg (Br) 2003;85(7):956–9. doi: 10.1302/0301-620x.85b7.14095. [DOI] [PubMed] [Google Scholar]
- Blom AW, Cunningham JL, Hughes G, Lawes TJ, Smith N, Blunn G, Learmonth ID, et al. The compatibility of ceramic bone graft substitutes as allograft extenders for use in impaction grafting of the femur. J Bone Joint Surg (Br) 2005;87(3):421–5. doi: 10.1302/0301-620x.87b3.14337. [DOI] [PubMed] [Google Scholar]
- Blom AW, Wylde V, Livesey C, Whitehouse MR, Eastaugh-Waring S, Bannister GC, Learmonth ID. Impaction bone grafting of the acetabulum at hip revision using a mix of bone chips and a biphasic porous ceramic bone graft substitute. Acta Orthop. 2009;80(2):150–4. doi: 10.3109/17453670902884767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973;55(8):1629–32. [PubMed] [Google Scholar]
- Busch V J JF, Gardeniers J WM, Verdonschot N, Slooff T J JH, Schreurs BW. Acetabular Reconstruction with Impaction Bone-Grafting and a Cemented Cup in Patients Younger than Fifty Years Old: A Concise Follow-up, at Twenty to Twenty-eight Years, of a Previous Report. J Bone Joint Surg (Am) 2011;93(4):367–71. doi: 10.2106/JBJS.I.01532. [DOI] [PubMed] [Google Scholar]
- Charalambides C, Beer M, Cobb AG. Poor results after augmenting autograft with xenograft (Surgibone) in hip revision surgery. Acta Orthop. 2005;76(4):544–9. doi: 10.1080/17453670510041547. [DOI] [PubMed] [Google Scholar]
- Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg (Br) 1996;78(2):185–90. [PubMed] [Google Scholar]
- Deakin DE, Bannister GC. Graft incorporation after acetabular and femoral impaction grafting with washed irradiated allograft and autologous marrow. J Arthroplasty. 2007;22(1):89–94. doi: 10.1016/j.arth.2006.02.162. [DOI] [PubMed] [Google Scholar]
- DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;(121):20–32. [PubMed] [Google Scholar]
- Egawa H, Ho H, Huynh C, Hopper RH, Engh CA, Engh CA. A. Three-dimensional Method for Evaluating Changes in Acetabular Osteolytic Lesions in Response to Treatment. Clin Orthop. 2009;(468)(2):480–90. doi: 10.1007/s11999-009-1050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;12(5):535–40. doi: 10.1016/s0883-5403(97)90176-5. [DOI] [PubMed] [Google Scholar]
- Engelbrecht E, Foerster von G, Delling G. Ionogran in revision arthroplasty. J Bone Joint Surg (Br) 2000;82(2):192–9. [PubMed] [Google Scholar]
- Field RE, Cronin MD, Singh PJ. The Oxford hip scores for primary and revision hip replacement. J Bone Joint Surg (Br) 2005;87(5):618–22. doi: 10.1302/0301-620X.87B5.15390. [DOI] [PubMed] [Google Scholar]
- Friedlaender GE, Strong DM, Sell KW. Studies on the antigenicity of bone. II. Donor-specific anti-HLA antibodies in human recipients of freeze-dried allografts. J Bone Joint Surg (Am) 1984;66(1):107–12. [PubMed] [Google Scholar]
- Fujishiro T, Nishikawa T, Takahiro N, Takikawa S, Saegusa Y, Kurosaka M, Bauer TW. Histologic analysis of allograft mixed with hydroxyapatite-tricalcium phosphate used in revision femoral impaction bone grafting. Orthopedics. 2008;31(3):277. doi: 10.3928/01477447-20080301-12. [DOI] [PubMed] [Google Scholar]
- Galea G, Kopman D, Graham BJ. Supply and demand of bone allograft for revision hip surgery in Scotland. J Bone Joint Surg (Br) 1998;80(4):595–9. doi: 10.1302/0301-620x.80b4.8240. [DOI] [PubMed] [Google Scholar]
- Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg (Br) 1993;75(1):14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- Gozzard C, Blom A, Taylor A, Smith E, Learmonth I. A comparison of the reliability and validity of bone stock loss classification systems used for revision hip surgery. J Arthroplasty. 2003;2003;18(5):638–42. doi: 10.1016/s0883-5403(03)00107-4. [DOI] [PubMed] [Google Scholar]
- Hanft JR, Sprinkle RW, Surprenant MS, Werd M B. Implantable bone substitute materials. Clin Podiatr Med Surg 1995. 1995;12(3):437–55. [PubMed] [Google Scholar]
- Itokazu M, Matsunaga T, Ishii M, Kusakabe H, Wyni Y. Use of arthroscopy and interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Arch Orthop Trauma Surg. 1996;115(1):45–8. doi: 10.1007/BF00453217. [DOI] [PubMed] [Google Scholar]
- Kawanabe K, Iida H, Matsusue Y, Nishimatsu H, Kasai R, Nakamura T. A-W glass ceramic as a bone substitute in cemented hip arthroplasty: 15 hips followed 2-10 years. Acta Orthop. 1998;69(3):237–42. doi: 10.3109/17453679809000922. [DOI] [PubMed] [Google Scholar]
- Leung H-B, Fok M W-M, Chow L C-Y, Yen C-H. Cost comparison of femoral head banking versus bone substitutes. J Orthop Surg (Hong Kong) 2010;18(1):50–4. doi: 10.1177/230949901001800111. [DOI] [PubMed] [Google Scholar]
- Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011:p. 591253. doi: 10.1155/2011/591253. DOI 10.1155/2011/591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara I, Deshpande S, Porteous M. Impaction grafting of the acetabulum with a mixture of frozen, ground irradiated bone graft and porous synthetic bone substitute (Apapore 60) J Bone Joint Surg (Br) 2010;92(5):617–23. doi: 10.1302/0301-620X.92B5.23044. [DOI] [PubMed] [Google Scholar]
- National Research Ethics Service ed. 3. 2007. National Patient Safety Agency, National Research Ethics Service: Defining research. http://www.nres.nhs.uk/EasySiteWeb/GatewayLink.aspx?alId=355 Available from:
- Oonishi H, Iwaki Y, Kin N, Kushitani S, Murata N, Wakitani S, Imoto K. Hydroxyapatite in revision of total hip replacements with massive acetabular defects: 4- to 10-year clinical results. J Bone Joint Surg (Br) 1997;79(1):87–92. doi: 10.1302/0301-620x.79b1.1290. [DOI] [PubMed] [Google Scholar]
- Parry MC, Whitehouse MR, Mehendale SA, Smith LK, Webb JC, Spencer RF, Blom AW. A comparison of the validity and reliability of established bone stock loss classification systems and the proposal of a novel classification system. Hip Int. 2010;20(1):50–5. doi: 10.1177/112070001002000108. [DOI] [PubMed] [Google Scholar]
- Ransford AO, Morley T, Edgar MA, Webb P, Passuti N, Chopin D, Morin C, et al. Synthetic porous ceramic compared with autograft in scoliosis surgery. A prospective, randomized study of 341 patients. J Bone Joint Surg (Br) 1998;1998;80(1):13–8. doi: 10.1302/0301-620x.80b1.7276. [DOI] [PubMed] [Google Scholar]
- Ritter MA, Zhou H, Keating CM, Keating EM, Faris PM, Meding JB, Berend ME. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg (Br) 1999;81(6):982–6. doi: 10.1302/0301-620x.81b6.9634. [DOI] [PubMed] [Google Scholar]
- Schmalzried TP, Kwong LM, Jasty M, Sedlacek RC, Haire TC, O’Connor DO, Bragdon CR, et al. The mechanism of loosening of cemented acetabular components in total hip arthroplasty. Analysis of specimens retrieved at autopsy. Clin Orthop. 1992;(274):60–78. [PubMed] [Google Scholar]
- Schreurs BW, Busch V J JF, Welten ML, Verdonschot N, Slooff T J J H and Gardeniers J WM. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old. J Bone Joint Surg (Am) 2004;86(11):2385–92. doi: 10.2106/00004623-200411000-00004. [DOI] [PubMed] [Google Scholar]
- Schwartz C, Bordei R. Biphasic phospho-calcium ceramics used as bone substitutes are efficient in the management of severe acetabular bone loss in revision total hip arthroplasties. Eur J Orthop Surg Traumatol. 2005;15(3):191–6. [Google Scholar]
- Simonds RJ, Holmberg SD, Hurwitz RL, Coleman TR, Bottenfield S, Conley LJ, Kohlenberg SH, et al. Transmission of Human Immunodeficiency Virus Type 1 from a Seronegative Organ and Tissue Donor. N Engl J Med. 1992;326(11):726–32. doi: 10.1056/NEJM199203123261102. [DOI] [PubMed] [Google Scholar]
- Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop. 1996;(324):108–15. doi: 10.1097/00003086-199603000-00013. [DOI] [PubMed] [Google Scholar]
- Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199–204. doi: 10.1016/S0140-6736(12)60353-5. [DOI] [PubMed] [Google Scholar]
- Somford MP, Bolder S BT, Gardeniers J WM, Slooff T J JH, Schreurs BW. Favorable survival of acetabular reconstruction with bone impaction grafting in dysplastic hips. Clin Orthop. 2008;466(2):359–65. doi: 10.1007/s11999-007-0048-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomford WW, Starkweather RJ, Goldman MH. A study of the clinical incidence of infection in the use of banked allograft bone. J Bone Joint Surg (Am) 1981;63(2):244–8. [PubMed] [Google Scholar]
- van Haaren EH, Heyligers IC, Alexander F GM, Wuisman P I JM. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg (Br) 2007;89(3):296–300. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller SD. A. 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Whitehouse MR, Dacombe PJ, Webb J CJ, Blom AW. Impaction grafting of the acetabulum with ceramic bone graft substitute mixed with femoral head allograft: High survivorship in 43 patients with a median follow-up of 7 years. A follow-up report. Acta Orthop. 2013;84(4):365–70. doi: 10.3109/17453674.2013.792031. [DOI] [PMC free article] [PubMed] [Google Scholar]