Abstract
Ameloblastomas are locally aggressive jaw tumors with a high propensity for recurrence that are believed to arise from remnants of odontogenic epithelium, lining of odontogenic cysts and basal layer of overlying oral mucosa. They can occur in either the maxilla or mandible at nearly any age but most frequently are discovered as a painless expansion in the mandible of patients in their 20s-40s. Histopathologically, the follicular and plexiform patterns are the most common. When extensive squamous metaplasia, often associated with keratin formation occurs in central portions of the epithelial islands of follicular ameloblastoma, the term acanthomatous is sometimes applied. Here we present a case of acanthomatous ameloblastoma in a 20 year old patient.
How to cite this article: Geeta Singh, Rashmi Agarwal, Vimlesh Kumar, Deepak Passi. Acanthomatous Ameloblastoma- A Case Report. J Int Oral Health 2013; 5(2):60-64..
Key words: : Ameloblastoma, Aacanthomatous, Mandibular Tumors
Introduction
Ameloblastoma is a rare odontogenic jaw tumor that is a challenge to pathologists because of its diversity of histological features and to surgeons due to its frequent defiance to complete eradication1. It is described for the first time by Broca (1868) as adamtinoma and then recoined by Churchill (1934)2. The other histological variants of ameloblastoma include follicular, plexiform, acanthomatous, granular cell, desmoplastic and basal cell types.
Acanthomatous ameloblastoma is considered as an aggressive tumor of the canine jaw, characterized by irregular verrucous masses adjacent to the tooth3. In 1993 Gardner and Baker described that acanthomatous epulides were a type of ameloblastoma that developed from the gingival epithelium (peripheral) or from alveolar bone (intraosseous)4. It has an aggressive local behavior and often invades periodontal apparatus, despite that it doesn’t metastasize to other organs. The most curative treatment of choice for acanthomatous ameloblastoma is the surgical excision. However, surgery can be declined owing to health problems or due to cosmetic defects. Radiation therapy has also been the treatment of choice for these tumor types, but this option may not be feasible for financial and logistic reasons. Intralesional chemotherapy is another option for treating acanthomatous ameloblastoma5. We present a case report of acanthomatous ameloblastoma which has been treated with surgical resection.
Case Report
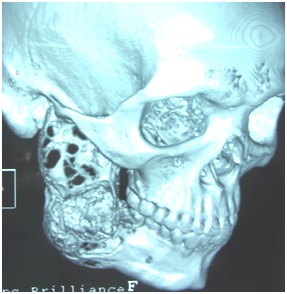
A 20 year old male patient reported to department of Oral & Maxillofacial surgery KGDU, Lucknow with the chief complaint of swelling in the right side of face since one year (Figure 1). The general health and medical history of the patient were not relevant. On clinical examination the swelling was about 6 x 5cm extending anteriorly 1cm from corner of the mouth to ramus of mandible posteriorly and superiorly 2cm from outer canthus of the eye to inferiorly lower border of the mandible. On palpation the swelling was non-tender, firm and fixed. A radiological examination with OPG (Orthopantomogram) and CT scan was done (Figure 2 & 3). The OPG showed multilocular radiolucencies involving angle and ramus of mandible including condyle and coronoid process with root resorption of 1st and 2nd mandibular right molars. CT scan showed marked expansion & distortion of both buccal and lingual plates.
Fig. 1:patient with swelling on right side of face.

Fig. 2:OPG showing multilocular radiolucency.
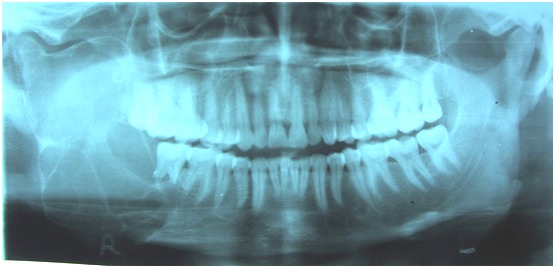
Fig 3:CT SCAN also showing multilocular images in mandible.
Surgical treatment has been planned under general anesthesia. An extended submandibular incision was given and layer wise dissection has been performed to expose pathological bone. The surgical resection of lesion was done with wide normal margin of about 1cm involving soft tissue.
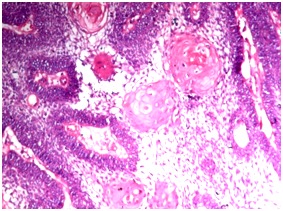
Reconstruction was done with 2.5mm titanium reconstruction plate; which was incorporated with cancellous iliac crest and alloplast hydroxyappatite collagen graft using PRP (Platelet Rich Plasma). The resected specimen was sent for histopathological examination which revealed solid epithelial cell nests with peripheral palisading ameloblastic cells and central squamous cells with the diagnosis of ameloblastoma acanthomatous type. During postoperative follow up, patient revealed no untoward complications (Figure 4).
Fig 4: Histopathological picture showing acanthomatous changes.
Discussion
Ameloblastomas account for 1% of all tumors of the jaw encountered during the 3rd to 5th decades of life which was not consistent with our case as the patient in our case was in 2nd decade of life. Schafer et al reported that ameloblastomas of oral cavity, except sinonasal type typically occur in younger age patients (15-25 years younger) without gender predilection6. About 80% of all cases occur in mandible, of which 70% cases are seen in the ramus1. The same location was seen in our case as he reported the swelling in the right mandibular region. Ameloblastomas have been classified in both human and veterinary literature and have been defined as benign, locally invasive and clinically malignant lesions. Metastasis has never been documented in dogs; however, in humans, malignant ameloblastomas and ameloblastic carcinomas have been noted to metastasize to the lungs, pleura, orbit, skull and brain. In human ameloblastomas, histopathological categories include Plexiform, Unicystic, Acanthomatous, Granular and follicular4.
Acanthomatous type is a benign tumor, but is locally aggressive and frequently invades the alveolar bone or recurs after marginal surgical excision. It is classified as an ameloblastoma; however controversies exist as to whether this tumor should be classified as a basal cell carcinoma, epulis or an odontal origin tumor5.
Patients may complian or present with the history of a slow growing mass, malocclusion, loose teeth or more rarely paresthesia and pain, however many lesions are detected incidentally on radiographic studies in asymptomatic patients. The lesions usually progress slowly but if left untreated can resorb the cortical plate and extend into adjacent tissue7. In our case the patient only reported regarding slowly progressive swelling and difficulty in mastication.
The OPG and CT scan in our case showed multilocular radiolucencies involving angle and ramus of mandible including condyle and coronoid process with root resorption of 1st and 2nd molar which was consistent with the radiographic features7, reported that most of ameloblastoma cases showed expansile, radiolucent, multiloculated cystic lesion with a characteristic "soap bubble" appearance7. Factors which have been notified regarding the aggressive behavior of ameloblastomas are; increase in the proliferative potential and changes in the expression of tumor suppressor genes and their protein products8. Calculus and oral sepsis (which could be the source of chronic irritation) have also been suggested to play a role in etiology of ameloblastoma9.
Although odontogenic tumors have particular histological characteristics, it is not uncommon for them to be misdiagnosed by pathologists who are not familiar with oral pathology. For ameloblastomas that do not show the obvious characteristic features of dental epithelium or when they are predominated by squamous component with invasive growth pattern, the diagnosis is sometimes difficult. This is particularly eminent for acanthomatous ameloblastoma since squamous metaplasia may be present10, which is same as our histopathological report of the presented case. According to Adebiyi et al follicular ameloblastoma is the most prevalent histological variant followed by plexiform, desmoplastic and acanthomatous varieties9.
The treatment of choice is complete surgical resection. If possible, conservative surgery can be used if an assured complete removal can be performed6. In the present case, surgical resection of the lesion was done. In addition to low sensitivity of this neoplasm, the intraosseous location of the ameloblastoma prevents the use of radiotherapy as an effective therapeutic option because radiation induces the potential development of secondary tumors. Therefore, in all types of ameloblastomas, a thorough long term clinical and radiographic follow up is always recommended11.
Conclusion
Ameloblastomas are uncommon benign odontogenic neoplasms that rarely become malignant. In most cases, radical surgery is the treatment of choice. Although several articles have been published on this subject, little is known regarding the biological behavior of this tumor. Careful clinical examination combined with thorough imaging investigation to evaluate the general aspects of the lesions and the margins, as well as its internal architecture and its relationship to adjacent anatomical structures can be assisted in treatment planning. This information coupled with histopathological confirmation of the diagnosis will allow for the selection of the best individual therapeutic approaches, increasing the treatment efficacy in patients diagnosed with this tumor.
Footnotes
Source of Support: Nil
Conflict of Interest: None Declared
Contributor Information
Geeta Singh, Department of Oral & Maxillofacial Surgery, King George Dental University, Lucknow, Uttar Pradesh, India.
Rashmi Agarwal, Department of Oral & Maxillofacial Surgery, Chandra Dental College & Hospital, Barabanki, Uttar Pradesh, India.
Vimlesh Kumar, Department of Oral & Maxillofacial Surgery, B.R.D Medicall College, Gorakhpur, Uttar Pradesh, India.
Deepak Passi, Department of Oral & Maxillofacial Surgery, King George Dental University, Lucknow, Uttar Pradesh, India.
References
- 1.VA Walke, MM Munshi, WK Raut, SK Bobahate. cytological diagnosis of acanthomatous ameloblastoma. Journal of cytology. 2008;25(2):62–64. [Google Scholar]
- 2.Bansal M, Chaturvedi TP, Bansal R, kumar M. Acanthomatous ameloblastoma of anterior maxilla. Journal of Indian society of pedodontics and preventive dentistry. 2010;28(3):209–211. doi: 10.4103/0970-4388.73797. [DOI] [PubMed] [Google Scholar]
- 3.Mortano M, Damiano S, Restucci B, Paciello O, Russo V, Maiolino P. Nuclear morphometry in canine acanthomatous ameloblastomas and squamous cell carcinoma. European journal of histocehmistry. 2006;50(2):125–130. [PubMed] [Google Scholar]
- 4.Murray RL, Aitken ML, Gottfried SD. The use of rim excision as a treatment for canine acanthomatous ameloblastoma . Journal of the American animal hospital association. 2010;46(2):91–96. doi: 10.5326/0460091. [DOI] [PubMed] [Google Scholar]
- 5.Kelly JM, Belding BA, Schaefer AK. Acanthomatous ameloblastoma in dogs treated with intralesional bleomycin. Veterinary and comparative oncology. 2010;8(2):81–86. doi: 10.1111/j.1476-5829.2010.00208.x. [DOI] [PubMed] [Google Scholar]
- 6.Schafer DR, Thompson LDR, Smith BC, Wenig BM. Primary ameloblastoma of the sinonasal tract. Cancer. 1998;82(4):667–674. doi: 10.1002/(sici)1097-0142(19980215)82:4<667::aid-cncr8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 7.A Bhargava, S Saigal, M Chalishazar. Acanthomatous ameloblastoma of mandible. Journal of dental sciences & Research. 2(2):1–5. [Google Scholar]
- 8.J salehinejad, RZ Mahmoodabadi, S Saghafi, AH Jafarian, N Ghazi, AR Rajaei, P Marouzi. immunohistochemical detection of p53 & PCNA in ameloblastoma and adenomatoid odontogenic tumor. Journal of oral science. 2011;53(2):213–217. doi: 10.2334/josnusd.53.213. [DOI] [PubMed] [Google Scholar]
- 9.Adebiyi KE, Ugboko VI, GO Esan, KC Ndukwe, FO Oginni. clinicopathological analysis of histological variants of ameloblastoma in a suburban Nigerian population. Head & Face medicine. 2006;24(2):42. doi: 10.1186/1746-160X-2-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.YW Chen, WY Li, SY Kao. synchronous oral squamous cell carcinoma and ameloblastoma in a patient and using CK8 expression as an aid to differential diagnosis – case analysis. Taiwan J Oral Maxillofac surg. 2008;19:170–178. [Google Scholar]
- 11.LR Olieira, BH Matos, PR Dominguete, VA Zorgetto, AR Silva. Ameloblastoma: Report of two cases and a brief literature review. Int.J. Odontostomat. 2011;5(3):293–299. [Google Scholar]


