Abstract
Objectives: The aim of this study was to determine the effect of ageing on the light intensity of quartz-tungsten-halogen (QTH) polymerization units in dental schools and dental clinics.
Materials & Methods: Two dental schools and multiple public health dental clinics were visited and the light intensity of curing units was assessed. The age, make, model and service history were recorded. A calibrated radiometer (range 0-1000 nm) was used to measure the light intensity of 171 QTH units. At the end of each visit, the team members provided each dental clinic with a verbal report of the test results and recommendations on maintenance of light polymerization units.
Results: The 171 units tested were from seven different manufacturers. The mean light intensity was 373.1 mW/cm2, the lowest intensity being 95.3 and the highest 526.60 mW/cm2. Only 29 QTH units recorded more than 500 mW/cm2; 102 units showed readings that ranged between 300 and 500 mW/cm2 and 39 units recorded readings below 300 mW/cm2. It was not able that one unit had light intensity reading of less than 100 mW/cm2. The age distribution was as follows: 35 units were more than 10 years old, 79 were from 5 to 10 years old and 57 were less than 5 years old. There was a high statistical significant relation between the mean light intensity and age (P = 0.001).
Conclusion: Light intensity values used in some dental clinics were to be found lower than what is recommended for optimum polymerization of resin-based composite restorations. Awareness among dentists of the value of QTH light curing units and their commitment to care and maintenance are crucial to achieving optimum restoration properties.
How to cite this article: Al-Samadani KH, Al-Dharrab A, Wahbi MA , Algizani L. Light Intensity Decay in Quartz-Tungsten-Halogen Polymerization Units. J Int Oral Health 2013; 5(1):23-30.
Keywords: : Intensity, Quartz-tungsten, Light unit, Polymerization
Introduction:
Dental composites are important materials extensively used in the restoration of teeth. However, composite resins have some limitations. Factors that determine the final properties of light-activated composite resin include composition, the intensity of the light source and exposure time. The clinical performance of light-cured composite restorations is greatly influenced by the quality of curing light.1,2
Quartz-tungsten-halogen lamps have been widely employed for polymerizing resins, bonding systems, bases and liners, luting agents and some provisional restorative materials. These units have a white halogen bulb with a filter to remove the undesirable wavelengths. However, a considerable number of other wavelengths are still emitted and absorbed by composite resins, inducing heating of the material and the tooth during the polymerization process. The decline of irradiance over time, due to the ageing of the bulb and the filter, has been reported.3,4
The clinical success of composite resins is directly related to the polymerization process. The satisfactory polymerization of a composite resin relies on variables such as hue, translucency, filler particle size, time of light exposure, increment thickness, light intensity and light source distance. Moreover, clinical factors such as the accessibility of the light source, the direction of the light, cavity depth and intervening tooth tissue may limit depth of cure or adequate polymerization, which demands light intensities greater than 280 mW/cm2.5,6,7,8 If the intensity falls to between 200 and 300 mW/cm2, a prolonged time will be required to cure the composite resins, while an intensity below 200 mW/cm2 is inadequate and even harmful, because excess infrared and ultraviolet radiation may be emitted.4
Composite resins polymerized by ineffective equipment may present low mechanical strengths and stains on the outer surface of the material, or even in the bulk of the material, which harms the physical properties of the restoration. Irradiance is an important factor, because it represents the number of photons delivered to the sample per unit of time, regard-less of the area illuminated.4
The most common dental curing light used today is the QTH lamp. The relatively broad emission spectrum of QTH curing lights allows them to initiate the polymerization of all known composite resin materials. The principal output from these lamps is infrared energy, with the generation of considerable heat. Filters are used to reduce the transfer of heat energy to the oral structures and to provide further restriction of visible light to the narrower spectrum of photoinitiators. Additionally, these filters are intended to remove the major part of the radiation outside the blue range, in particular in the red and infrared range. Finally, a silver-coated dichroic reflector passes infrared energy out at the back and reflects and focuses the light forward to provide a focal area of energy at a defined distance. Ultimately, 99.5% of the original radiation is eliminated. Because of their high operating temperatures, QTH bulbs have a limited lifetime. The reflector, bulb and filters tend to deteriorate over time, reducing the curing effectiveness.9
The intensity and frequency of the radiation source must be sufficient to cure the material to the depth necessary for proper solidification and bonding of the polymer. To ensure proper curing, many dentists apply and cure the polymer in thin layers until the fill area is completed. Effective curing requires correct maintenance of the radiation device, proper control of the duration of exposure and the use of an appropriate type of restorative material. Other factors found to be important in effective curing include the shade of composite, the wavelength and bandwidth of the radiation, the distance of the instrument from the composite and the intensity and duration of the curing radiation.10,11
Incomplete polymerization may increase water sorption and solubility, adversely affecting the aesthetics of the restoration. In the region of the material where curing is not effective, the possible consequences include postoperative sensitivity, microleakage, premature failure of the restoration and high toxicity to the pulp. On the other hand, polymerization units themselves create a temperature rise during operation and this risk increases when these units are used with a high energy output and for prolonged operation times.12,13,14,15
Aim of the study:
The aim of the study was to determine the effect of ageing on the light intensity of QTH polymerization units used in two dental schools and multiple public dental clinics.
Methods and Materials:
The study was conducted in dental clinics at King Abdul Aziz University and Taibah University and at public dental clinics in Jeddah, Saudi Arabia. The research team members were trained to check the radiation intensity of QTH light sources used in the clinics to polymerize resin-based composite restorations. Data including age, make, model and service history were recorded for a total of 250 QTH light curing units, of which 79 were excluded as having been installed less than 12 months before the study, while 171 units were selected as fulfilling the inclusion criteria. The clinicians were contacted and the study requirements were explained to them, as was the purpose of the study. Curing radiometer, Model 100, Demetron, Kerr, was used to measure the optical radiation intensity given off by each QTH source. Before visiting the dental clinics, the team members checked the light radiometers to ensure consistency of readings, according to manufacturer's instructions. At each site, after a specific warm-up period, the team members recorded three measurements at intervals of 5-10 minutes of light intensity for each light unit in the clinic. At the end of each visit, the team members provided a report of the intensity test results.
The data collected were entered into a database after averaging the three readings of light intensity for each unit. Using the SPSS 15 statistical analysis program, a chi-squared test was used to establish the significance of any relation between the age of the units and their mean light intensity. The implications of the findings were discussed and recommendations made.
Results:
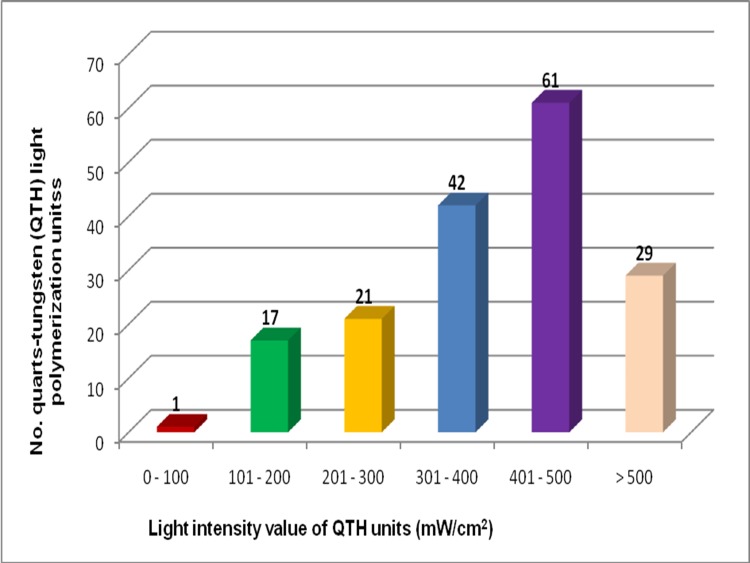
The 171 QTH light curing units examined were of even different makes and had a mean light intensity of 373.10 mW/cm2. The output varied widely among the units tested, as Figure 1 shows: one of the units recorded < 100 mW/cm2, 17 units showed readings of 100-200 mW/cm2 and 21 units 200-300 mW/cm2; thus a total of 39 units registered < 300 mW/cm2, while a further 42 units had an output < 400 mW/cm2, 61 more units < 500 mW/cm2 and only 29 units > 500 mW/cm2.
Fig. 1: Distribution of light intensity value of QTH units (mW/cm2).
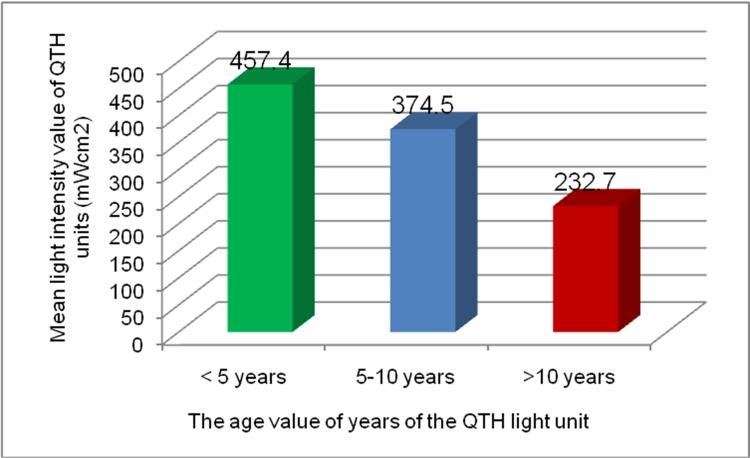
Table 1 and Figure 2 show the distribution of time in years since purchase of the QTH light units, which was > 10 years for 35 units (20.5%), 5-10 years for 79 units (46.2 %) and < 5 years for 57 units (33.3 %). The mean light intensity decreased with increasing age, as shown in Table 1; this association of age with light intensity is plotted in Figure 2. The age of the units was found to have a high significant relation with mean intensity of light output (P = 0.001).
Table 1: The age value of years, age value % and Mean light intensity value of QTH units (mW/cm2).
| Age in years | Number | % | Mean light intensity |
| < 5 | 57 | 33.3 | 457.4 |
| 5 - 10 | 79 | 46.2 | 374.5 |
| > 10 | 35 | 20.5 | 232.7 |
| Total | 171 | ||
| Chi squire at 2 df 15.08 P = 0.001 | |||
Fig. 2: Distribution of mean light intensity value (mW/cm2) vs. the age value of years of the QTH light unit.
Discussion:
There have been three major evolutions in dental composite curing lights since they were studied in 1991. At that time, the majority of practitioners used QTH units with power densities in the 400-600 mW/cm2 range. The relatively simple guidelines for clinicians involved three variables: light intensity, exposure duration and incremental layering of the composite material. Restorative dentists were instructed to monitor the output of their lights routinely to ensure that the intensity was above 300 mW/cm2, to cure the composite in increments less than 2 mm in thickness and to cure each increment for at least 40 seconds.10
Successful use of a polymerization unit depends on correct functioning of the instrument. For adequate polymerization, sufficient radiant intensity, correct wavelength of the visible light and sufficient polymerization time are essential. Unfortunately, halogen light-curing units have some specific negative characteristics, such as light output which decreases with time, which may result in a reduced degree of monomer conversion of composites; the generation of heat due to the ageing of bulbs and filters has also been reported.3
Visible light curing units are also required for most other bonding systems. Adequate polymerization requires sufficient intensity (or power density), appropriate wavelength and sufficient exposure duration. All three of these parameters must be adequate to achieve complete polymerization. Typically, these polymers are activated by a diketone photoinitiator that responds to radiation by creating free radicals which, in turn, initiate the polymerization process. A common diketone photoinitiator now used is camphorquinone (CQ) which is sensitive to blue light and the most suitable wavelengths are within the range of 450-490 nm. A visible-light-sensitive diketone photoinitiator is responsible for initiating free-radical polymerization. CQ absorbs energy in the visible range with a peak at 468 nm. Photons associated with this frequency range will be absorbed by CQ, raising it from the ground state to an excited, but short-lived, activated triplet state. When the excited triplet collides with an amine co-initiator, an aminoalkyl free radical will form, which is capable of initiating polymerization.16-18 Thus, any source of light with a reasonable irradiance within this range can be employed as a curing device. However, to obtain the correct irradiance of blue light to polymerize resins, a reasonable interval of time of around 40 seconds and a powerful light intensity emitted by the halogen lamp will be necessary (depending on the brand of the material), both related to the light density that reaches the resin.4
The formulation of dental composite selected by the clinician is an important variable when considering composite polymerization. Manufacturers continually refine the formulation of their materials in an effort to improve their physical properties, handling characteristics and available shades. In response to professional demands to reduce the polymerization time of composites and to produce "bleaching friendly" lighter shades, manufacturers began to substitute alternative photoinitiators for CQ, whose bright yellow colour makes it aesthetically incompatible for incorporation into the lighter shade composites. The alternative photoinitiators, phenyl-propanedione (PPD) and trioctylphosphine oxide (TPO) are used by the manufacturers of some newer composites because they are colour neutral and therefore tend not to exhibit the yellowing associated with CQ. These new photoinitiators absorb light energy in lower regions of the visible-light spectrum.18,19
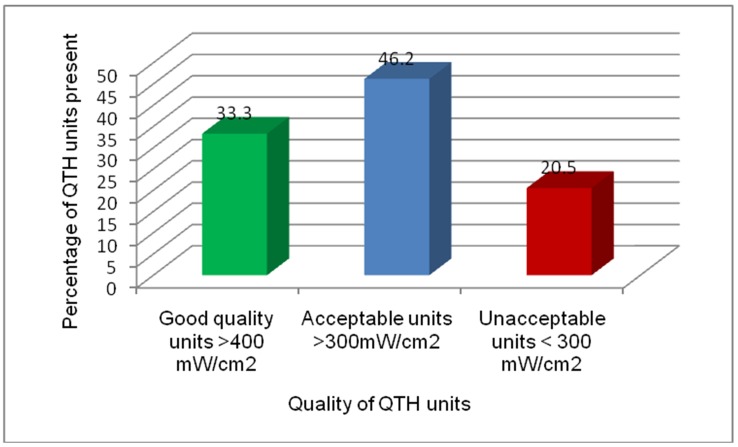
Since university clinics seek a high quality assurance standard and to meet the ISO standard, the suggested limit of irradiance for QTH units used in dental practices is 300 mW/cm2.3,8,10 We found that 20.5% units were unacceptable (< 300 mW/cm2), 46.2% were acceptable (>300 mW/cm2) and only 33.3% were of good quality (>400 mW/cm2) for use in dental clinics. The acceptability of the light units is presented in Figure 3.
Fig. 3: Acceptability of QTH units regarding light intensity value in mW/cm2.
Another important factor associated with the photopolymerization of composite resins is the relationship between the distance of the light tip from the material being cured and the dispersion of the light beam. Light dispersion can be of particular importance when trying to polymerize composite increments located at the gingival floor of a deep interproximal preparation. In this clinical scenario, the curing tip/composite increment distance could reach 6-7mm. Within these parameters, lights may lose up to 50% of their intensity; to overcome this phenomenon clinically, it has been recommended to limit the thickness of the initial composite increments in deep boxes to no more than 1 mm, then after matrix removal to attempt transillumination from various angles of approach.10
Photopolymerization has become an integral component of the practice of dentistry. A better appreciation of the photopolymerization process as well as its potential and limitations may aid the dentist in the delivery of both aesthetic and restorative dental care.18
The basic principle of light conversion in QTH bulbs has proven to be inefficient, as the light power output is less than 1% of the electrical power consumed, while the bulbs have a limited effective useful life of approximately 100 hours due to degradation of their components caused by the large amount of heat they generate.20 It should be considered that when a composite resin restoration does not receive sufficient energy at an appropriate wavelength because of an inadequately performing QTH unit, the effects on wearing may be significant, deterioration of the restoration margins may increase and the tooth-material adhesive strength, microhardness and Young modulus may all decrease. Therefore, dentists must use QTH units that allow high doses at the correct wavelength for polymerization.21
An additional hazard is that problems arising from inadequate light-curing of resin-based composite materials (partially cured resins) include enhanced toxicity.22 The direct toxicity of restorative materials largely results from the elution of compounds, particularly from partially cured resin-based materials.23 Ferracane24 found that ensuring full photopolymerization by adding more photoinitiator to increase the rate of polymerization reduced the availability of monomers to be leached.
Conclusions:
Within the limitations of this study, the following conclusions can be drawn:
A radiometer is useful for measuring the light intensity of the curing unit as the amount of energy on a given surface area (mW/cm2) and for clinicians to monitor the output of a curing unit periodically to maximize the cure of composite resins.
Regulatory bodies should consider the need for obligatory testing of light polymerization units used by dentists in all dental offices, including private practice.
Commitment to care and maintenance is crucial to achieve optimum restoration properties.
Footnotes
Source of Support: Nil
Conflict of Interest: None Declared
Contributor Information
Khalid H Al-Samadani, Department of Restorative Dental Science, College of Dentistry, Taibah University, Al Madinah Al Munawwarah - 43353, Kingdom of Saudi Arabia.
Al-Dharrab Ayman, Department of Oral and Maxillofacial Rehabilitation, Faculty of Dentistry, King Abdulaziz University, Jeddah - 21589, Kingdom of Saudi Arabia.
A Wahbi Mohammed, Conservative Dentistry, Makkah Dental Centre, PO. Box - 3381, Makkah, Kingdom of Saudi Arabia.
I Algizani Loay, Faculty of Dentistry, King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia.
References:
- 1.El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Kermalli J, Soliman O. Intensity of quartz-tungsten-halogen light-curing units used in private practice in Toronto. . J Am Dent Assoc. 2005;136(6):766–773. doi: 10.14219/jada.archive.2005.0260. [DOI] [PubMed] [Google Scholar]
- 2.Jadhav S, Hegde V, Aher G, Fajandar N. Influence of light curing units on failure of direct composite restorations. Journal of Conservative Dentistry. 2011;14(3):225–227. doi: 10.4103/0972-0707.85793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin FE. A survey of the efficiency of visible light curing units. J Dent Mater. 1998;26:239–243. doi: 10.1016/s0300-5712(97)00004-3. [DOI] [PubMed] [Google Scholar]
- 4.Small BW. A review of devices used for photo curing resin-based composites. J Gen Dent. 2001;49:457–460. [PubMed] [Google Scholar]
- 5.Burgess JO, Walker R, Davidson JM. Posterior resin-based composite: review of the literature. J Pediatr Dent. 2002;24:465–479. [PubMed] [Google Scholar]
- 6.Prince RB, Felix CA, Andreou P. Effects of resin composite composition and irradiation distance on the performance of curing lights. Biomat. 2004;25:4465–4477. doi: 10.1016/j.biomaterials.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Rueggeberg FA, Caughman WF. Curtis JWJr. Effect of light intensity and exposure duration on cure of resin composites. Oper Dent. 1994;19:26–32. [PubMed] [Google Scholar]
- 8.Shortall A, Harrington E. Guidelines for the selection, use, and maintenance of visible light activation units. Br Dent J. 1996;181:383–387. doi: 10.1038/sj.bdj.4809265. [DOI] [PubMed] [Google Scholar]
- 9.Rueggeberg FA. Contemporary issues in photocuring. Compend. 1999;25:S4–S15. [PubMed] [Google Scholar]
- 10.Caughman WF, Rueggeberg FA, Curtis JW. Curtis J.W. Clinical Guidelines for Photocuring Restorative Resins. J Am Dent Associ. 1995;126:1280–1286. doi: 10.14219/jada.archive.1995.0364. [DOI] [PubMed] [Google Scholar]
- 11.Fan PL, Schumacher RM, Azzolin K, Geary R, Eichmiller FC. Curing light intensity and depth of cure of resin based composites tested according to international standards. J Am Dent Assoc. 2002;133:429–434. doi: 10.14219/jada.archive.2002.0200. [DOI] [PubMed] [Google Scholar]
- 12.Dunne SM, Davies BR, Millar BJ. A survey of the effectiveness of dental light-curing units and comparison of light testing devices. Br Dent J. 1996;180(1):411–416. doi: 10.1038/sj.bdj.4809107. [DOI] [PubMed] [Google Scholar]
- 13.Mehl A, Hickel R, Kunzelmann KH. Physical properties and gapformation of light-cured omposites with and without 'softstartpolymerization'. J Dent. 1997;25(3-4):321–330. doi: 10.1016/s0300-5712(96)00044-9. [DOI] [PubMed] [Google Scholar]
- 14.Munksgaard E, Peutzfeldt A, Asmussen E. Elution of TEGDMA and BisGMA from a resin composite cured with halogen or plasma light. Eur J Oral Sci. 2000;108:341–345. doi: 10.1034/j.1600-0722.2000.108004341.x. [DOI] [PubMed] [Google Scholar]
- 15.Knezevic A, Tarle Z, Meniga A, Sutalo J, Pichler G. Influence of light intensity from different curing units upon composite temperature rise. J Oral Rehabil. 2005;32:362–367. doi: 10.1111/j.1365-2842.2004.01418.x. [DOI] [PubMed] [Google Scholar]
- 16.Nomoto R. Effect of light wavelength on polymerization of light-cured resins. J Dent Mater. 1997;16(1):60–73. doi: 10.4012/dmj.16.60. [DOI] [PubMed] [Google Scholar]
- 17.Cook WD. Photopolymerization kinetics of dimethacrylates using camphoroquinone amine initiator system. Polymer. 1992;33:600–609. [Google Scholar]
- 18.Stansbury JW. Curing dental resins and composites by photopolymerization. J Esthet Dent. 2000;12:300–308. doi: 10.1111/j.1708-8240.2000.tb00239.x. [DOI] [PubMed] [Google Scholar]
- 19.Burtscher P, Rheinberger V. Efficiency of various light initiators after curing with different light-curing units. J Dent Res. 2003 [Google Scholar]
- 20.Rueggeberg FA, Twiggs SW, Caughman WF, Khajotia S. Lifetime intensity profiles of light-curing units. J Dent Res. 1996;75:380. [Google Scholar]
- 21.Price RBT, Felix CA, Andreou P. Evaluation of a second generation LED curing light. J Can Dent Assoc. 2003;69(10):666–666h. [PubMed] [Google Scholar]
- 22.Quinlan CA, Zisterer DM, Tipton KF, O'Sullivan MI. In vitro cytotoxicity of a composite resin and compomer. Intern Endod J. 2002;35:47–55. doi: 10.1046/j.1365-2591.2002.00456.x. [DOI] [PubMed] [Google Scholar]
- 23.Geurtsen W, Spahl W, Leyhausen G. Residual monomer/additive release and variability in cytotoxicity of light-curing glass-ionomer cements and compomers. J of Dent Res. 1998;77:2012–2019. doi: 10.1177/00220345980770121001. [DOI] [PubMed] [Google Scholar]
- 24.Ferracane JL. Elution of leachable components from composites. J of Oral Rehab. 1994;21:441–452. doi: 10.1111/j.1365-2842.1994.tb01158.x. [DOI] [PubMed] [Google Scholar]