Abstract
Aim: Articaine is an amide local anesthetic that differs from other agents of its group due to the presence of thiophene ring instead of a benzene ring. Some researchers claim that articaine is superior to lidocaine in its biologic profile. The aim of the study is to compare the efficacy of articaine with that of lidocaine which has proven efficacy.
Materials and method: This study was done on 50 subjects; 25 of them received 4 % articaine HCl with 1:100000 epinephrine and the next 25 received 2% lignocaine HCl with 1:100000 epinephrine. Time of injection, onset of anesthesia, amount of anesthetic injected were recorded. Efficacy was determined using visual analog scale. The values were statistically analyzed.
Results: The mean onset time of anesthesia in study group was 2.07 ± 0.22 and 2.18 ± 0.26 minutes in comparison group. A mean duration of 4.28 +0.78 hours was seen with articaine group and 3.51 + 0.45 hours with the lignocaine group. No statistical difference between the two groups with regard to pain experience.
Conclusion: Articaine has similar efficacy as that of lignocaine with slightly longer duration and can be used as an alternative to lignocaine in third molar surgeries.
Clinical Significance: Increased availability of local anesthetics has improved interest in research about dental pain control. a quest for new methods of pain reduction is always justified.
How to cite this article: R Shruthi, S N Kedarnath, S Mamatha N, Rajaram P, Dinesh B. Articaine For Surgical Removal of Impacted Third Molar; A Comparison With Lignocaine. J Int Oral Health 2013; 5(1):48-53.
Keywords: : Local anaesthesia, articaine, lignocaine, efficacy, visual analogue scale
Introduction
Local anesthetics are the safest and the most effective drugs available for prevention and management of pain. Indeed, there is no other drug that truly prevent pain; no other drug actually prevent a propagated nociceptive nerve impulse from reaching the central nervous system, where it would be interpreted as pain.1
Carticaine, first prepared by Rusching and colleagues in 1969, had its generic name changed to articaine when it entered clinical practice in Germany in 1976. Its use gradually spread, entering North America in 1983 and United Kingdom in 1998. As with lidocaine articaine is also classified in the group of intermediate duration of action.2
Literature mention that patients treated with articaine will be 'drug free' more quickly than those who receive other local anesthetics. Articaine reported to diffuse better through soft tissue and bone than other local anesthetics, claimed to be superior to lidocaine owing to fast onset of the block, the excellent quality of the anesthesia, the low degree of toxicity but this remains unproven.3
Materials and Methods
A randomized clinical trial was done, articaine being compared with lignocaine for purpose of evaluating the efficacy of articaine. Lignocaine was chosen as a reference substance, as its effects are well documented. The study group consisted of fifty patients who had undergone surgical removal of impacted mandibular third molar. Subjects between age group of 20-30 years with impacted mandibular third molars not associated with acute infection having no concomitant medical problems. Twenty-five subjects received 4% articaine HCl (group 1) and twenty five received 2% lignocaine HCl (group 2) for removal of impacted tooth. All subjected were evaluated preoperatively. Twenty five of them received 4% articaine with 1:100000 epinephrine and next twenty five received 2% lignocaine with 1:100000 epinephrine.
Exclusion Criteria
Known or suspected allergies or sensitivities to sulfites, amide type local anesthetics or any ingredients in the anesthetic solution.
Concomitant cardiac or neurological disease.
Pregnancy / lactation.
Concomitant use of monoamine oxidase inhibitors, tricyclic antidepressants, phenothiazine, vasodepressor drugs or ergot type oxytocic drugs.
Subjects who are on sedatives.
Subjects who had taken aspirin, acetaminophen, NSAIDS 24 hours prior to administration of local anesthetic.
All patients were explained about the visual analog proforma preoperatively and informed to report the numbness of lip and tongue as soon as they feel. Time of injection, onset of anesthesia, amount of anesthetic injected were recorded. The proforma was filled by the patient based on their pain experiences postoperatively. They were told to report to the doctor about time of loss of anesthesia as soon as noticed. All patients were reviewed next day.
Parameters
Drug volume: Amount of anesthetic used (volume in ml) in each case and any additional injections required were recorded.
Onset of anesthesia: Time of onset of anesthesia is calculated by recording the time of injection and time of patient first report of numbness of the lower lip and tongue. Patient is immediately checked for objective signs.
Time of soft tissue anesthesia - time of injection = time of onset.
Duration of anesthesia: Calculated by recording the time of injection and patient reporting the loss of numbness.
Time of loss of anesthesia - time of injection =duration of anesthesia
Pain ratings: Efficacy is determined on gross scale immediately after the procedure using the visual analog scale or VAS ranging from 0= no pain to 10= worst pain imaginable.
Any post operative complication like paresthesia, trismus and others were noted.
Results:
We randomized 50 patients and treated 25 with articaine and 25 with lignocaine.
11 male and 14 female patients with mean age group of 22.5 years in articaine group and 10 male and 15 female patients with mean age group of 24 years in lignocaine group were included in the study.
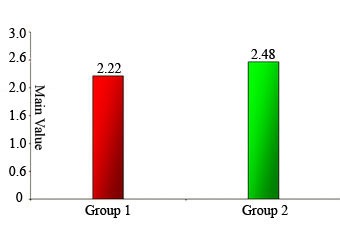
Drug volume: We administered as much of the drug as necessary to achieve adequate anesthesia. The mean volume of articaine administered was 2.22 ± 0.49 ml and mean volume of lignocaine was 2.46 ± 0.69 ml. Though the volume used is slightly less in articaine group, it is not statistically significant.
Fig. 1: Dutribution amount of local Anesthesia is used among the study group.
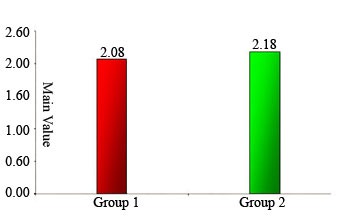
Time of onset: The study showed the onset period ranging between 1.4 to 2.4 minutes in articaine group and between 1.5 to 2.4 minutes in lignocaine group. The mean onset time of anesthesia in study group was 2.07 + 0.22 and 2.18 + 0.26 minutes in comparison group.
Fig. 2: Distribution On set of Anesthesia among the study group.
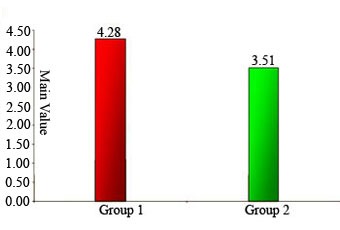
Duration of anesthesia: A mean duration of 4.28 ±0.78 hours was seen with articaine group and 3.51 ± 0.45 hours with the lignocaine group. The difference is statistically significant (P=0.0004) giving an inference that the articaine has longer duration of anesthesia compared to that of control group.
Fig. 3: Distribution duration of Anesthesia among the study group.
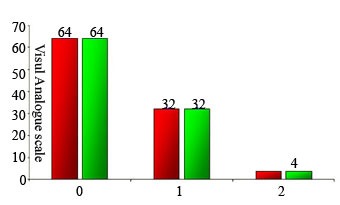
Pain ratings: We included VAS evaluation for efficacy analysis. We found no statistical difference between the two groups (P=1).
Fig. 4: Distribution Visual Analogue Scale among the Study Group.
The most common complaint was trismus in 9 subjects, four cases of articaine and five in lignocaine group, and followed by swelling in operated area clinically, we did not find any difference between the two groups even though objective measures were not done.
DISCUSSION
Articaine is not exactly a new drug. Identified in the older (mostly German) literature as articaine or carticain. Articaine is unique among available amide local anesthetics because it is based on a thiophene moiety rather than the typical benzene group. Articaine unlike other amide local anesthetics undergoes biotransformation in both liver and plasma thus cleared more quickly from the body.4
We should be aware that articaine delivers nearly twice the concentration of active anesthetic to the patient; as compared to lignocaine, thus one half of the amount should achieve similar anesthetic delivery. The dose required to achieve adequate anesthesia were 2.5 ml of articaine for a simple procedure (compared to 2.6 ml of lignocaine) and 4.2 ml for complex procedure (compared to 4.5ml of lignocaine) according to study conducted by Malamed5 and others. In our study, the mean volume of articaine administered was 2.22 + 0.49 ml and mean volume of lignocaine was 2.46 + 0.69 ml.
Costa6 et al found shorter onset and longer duration of pulpal anesthesia with articaine for maxillary infiltration. The mean values for pulpal onset were 2.8, 1.6 and 1.4 minutes and for pulpal duration were 39. 2, 56.7 and 66.3 minutes, respectively for 2% lignocaine with 1:100000 epinephrine, 4% articaine with 1:100000 epinephrine and 4% articaine with 1:200000 epinephrine. The present study comparable to study by Costa6 et.al has found slight early onset period of 2.07 minutes for articaine and 2.18 for lignocaine but is statistically not significant and mean duration of anesthesia of 4.28 hour of soft tissue anesthesia and 3.31 hrs which statistically confirms that 4% articaine with 1:100000 epinephrine produces longer duration of anesthesia. The study included only the subjective recordings of loss of soft tissue anesthesia but not an objective finding.
The duration of anesthesia cited for each drug is an approximation. Factors exist that affect both the depth and duration of a drug's anesthetic action, either prolonging or decreasing it. These factors include individual response to drug, accuracy in deposition of local anesthetic, status of tissue at the site of drug deposition, anatomical variation and volume of anesthetic used. Deposition of the local anesthetic close to the nerve provides greater depth and duration of anesthesia compared with local anesthetic deposited at a greater distance from the nerve to be blocked.7
We found VAS scores between 0 to 2 and no significant difference in pain experience with articaine or lignocaine. 64% patient reported no pain, 32% mild pain and 4% moderate pain ratings in both group. Pain measurement is difficult to establish, because its perception and intensity are multifactorial, encompassing sensorial and affective factors. Although VAS may show deficiencies regarding understanding and perception, it provides a validated and meaningful measure of anesthetic efficiency.
Van Eden and Patel8 reported that four patients complained of persistent, long standing lingual paraesthesia following routine dentistry performed using and inferior alveolar block with articaine. Haas and Lennon9 indicated articaine with a higher incidence of paraesthesia compared with other anesthetics. In our study there were no reports of paraesthesia.
Multiple variable factors exist like technique variability, anatomic variations, complexity of procedure and reporting error. Pain itself is multifactorial; perception and pain reaction varies greatly varies among individuals. Further controlled clinical trials are necessary to evaluate the safety and efficacy of articaine.
A prospective, randomized and clinical study was done on patients submitted to third molar surgery. Duration of surgery, latency, the amount of anesthetic used and analgesic consumption showed clinical differences with highlights of articaine, though statistical significance was not observed (P<0.05). The pain scores indicated similar anesthetic efficacy with both solutions which is comparable to our study10
A recent study has shown that 4% articaine with 1:100,000 epinephrine showed faster onset, longer duration of action and better diffusion in the tissues of the palate when compared with 2% lidocaine with 1:100,000 epinephrine and 60% of procedures with aritcaina 4% had no need for anesthesia of the palate11.
Puchades et al have compared bupivacine with articaine in third molar surgeries. Authors suggest that Bupivacaine could be a valid alternative to articaine especially due to its early postoperative pain prevention ability12.
CONCLUSION
The following conclusions can be drawn from the data obtained in our study The efficacy of 4% articaine is comparable to 2% lignocaine.Onset of action and amount of local anesthetic solution required is similar to lignocaine .4% articaine has longer duration of action than lignocaine The efficacy of 4% articaine based on VAS is similar to 2% lignocaine, indicating that articaine provides adequate analgesia for the procedure to be performed. Articaine can be used as an alternative to lignocaine in third molar surgeries.
Footnotes
Source of Support: Nil
Conflict of Interest: None Declared
Contributor Information
R Shruthi, Department of Oral and Maxillofacial Surgery Rajarajeshwari Dental College and Hospital, Ramohalli Cross, Mysore Road, Bangalore - 560 005, Karnataka, India.
NS Kedarnath, Oral Pathology, Maratha Mandal's N.G.H.I.D.S & R.C. Belgaum, India.
NS Mamatha, Department of Oral and Maxillofacial Surgery Rajarajeshwari Dental College and Hospital, Ramohalli Cross, Mysore Road, Bangalore - 560 005,Karnataka, India.
Prashanth Rajaram, Department of Oral and Maxillofacial Surgery VS dental college and hospital, Bangalore , Karnataka ,India.
Dinesh BhadraShetty, Department of Oral and Maxillofacial Surgery Al Jabal Al Ghardi University, Al zawia Libia.
REFERENCES:
- 1.Malamed SF. Handbook of local anesthesia. 5. St Louis; Mosby: 2004. p. 5. [Google Scholar]
- 2.Costa CG, Tortamano IP, Rocha RG, Francischone CE. Onset and duration periods of articaine and lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- 3.Vree TB, Gielen MJ. Clinical pharmacology and the use of articaine for local and regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19(2):293–308. doi: 10.1016/j.bpa.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Chaffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2004;30(8):568–571. doi: 10.1097/01.don.0000125317.21892.8f. [DOI] [PubMed] [Google Scholar]
- 5.Malamed SF, Gagnon S, Leblanc D. Efficacy of articaine: a new amide local anesthetic. J Am Dent Assoc. 2000;131(5):635–642. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 6.Luo YC. Sex determination from the pubis by discriminant function analysis. Forensic Sci. Int. 1995;74:89–98. doi: 10.1016/0379-0738(95)01739-6. [DOI] [PubMed] [Google Scholar]
- 7.Muller WP, Weiser P, Scholler KL. Pharmacokinetics of articaine in mandibular nerve block. Regional-Anaesthesie. 1991;14:52–55. [PubMed] [Google Scholar]
- 8.Van Eden SP, Patel MF. Prolonged paraesthesia following inferior alveolar nerve block using articaine. J Oral Maxillofac Surg. 2002;40:519–521. doi: 10.1016/s0266435602002231. [DOI] [PubMed] [Google Scholar]
- 9.Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc. 1995;61:319–330. [PubMed] [Google Scholar]
- 10.Silva LC, Santos Td, Santos TJ, Maia MC, Mendonca CM. Articaine versus lidocaine for third molar surgery: A randomized clinical study. Med Oral Patol Oral Cir Bucal. 2012 Jan;17(1):e140–e145. doi: 10.4317/medoral.17148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barcelos KC, Salim M, Cabral A, Prado R. Comparison of Articaina4% versus Lidocaina2% in Third Molar Surgery The Preliminary Program for IADR/AADR/CADR 89th General Session and Exhibition. http/iadr.confex.com/iadr2011sandiego/index.html Dental Anesthesiology Research. 2011 Mar; [Google Scholar]
- 12.Puchades MS, Vilchez-Perez MA, Castellon EV, Garcia JP. Bupivacaine 0.5 % versus articaine 4 % for the removal of lower third molars. A crossover randomized controlled trial med Oral Patol Oral Cir Bucal. med Oral Patol Oral Cir Bucal. 2012 May;17(3):e462–e468. doi: 10.4317/medoral.17628. [DOI] [PMC free article] [PubMed] [Google Scholar]


