Abstract
Objectives
Delirium’s adverse effect on long-term mortality in older hospitalized patients is well documented, while its effect in older emergency department (ED) patients remains unclear. Similarly, the consequences of delirium on nursing home patients seen in the ED are also unknown. As a result, we sought to determine if delirium in the ED was independently associated with 6-month mortality in older patients and if this relationship was modified by nursing home status.
Methods
Our prospective cohort study was conducted at a tertiary care, academic ED using convenience sampling, and included English speaking patients who were 65 years and older and were in the ED for less than 12 hours at the time of enrollment. Patients were excluded if they refused consent, were previously enrolled, were unable to follow simple commands at baseline, were comatose, or had incomplete data. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) was used to determine delirium and was administered by trained research assistants. Cox proportional hazard regression was performed to determine if delirium in the ED was independently associated with 6-month mortality after adjusting for age, comorbidity burden, severity of illness, dementia, functional dependence, and nursing home residence. To test whether the effect of delirium in the ED on 6-month mortality was modified by nursing home residence, an interaction term (delirium*nursing home) was incorporated into the multivariable model. Hazard ratios (HR) with their 95% confidence intervals (95% CI) were reported.
Results
Of the 628 patients enrolled, 108 (17.2%) were delirious in the ED and 58 (9.2%) were from the nursing home. For the entire cohort, the 6-month mortality rate was higher in the delirious group compared to the non-delirious group (37.0% versus 14.3%). Delirium was an independent predictor of increased 6-month mortality (HR = 1.72, 95% CI: 1.04 – 2.86) after adjusting for age, comorbidity burden, severity of illness, dementia, functional dependence, and nursing home residence. The “delirium*nursing home” interaction was non-significant (p=0.86), indicating that place of residence had no effect on the relationship between delirium in the ED and 6-month mortality.
Conclusion
Delirium in older ED patients is an independent predictor of increased 6-month mortality and this relationship appears to be present regardless of nursing home status.
Introduction
Background
Delirium occurs in 8 – 10% of older emergency department (ED) patients.1, 2 This form of brain dysfunction is characterized by an acute change in cognition that cannot be better accounted for by a preexisting or evolving dementia.3 Approximately 1.5 million older patients with delirium will be evaluated in the ED each year in the United States.4 This is similar to the number of annual acute coronary syndromes, a disease with comparable mortality and morbidity.5 Despite the magnitude of this problem, emergency physicians miss delirium in up to 75% of the cases.1, 2, 6
Importance
The lack of delirium recognition may be secondary to a dearth of ED outcomes data. Predominantly from in-hospital literature, delirium has been shown to be a marker for long-term death in non-critically ill and critically ill inpatients.7, 8 Unfortunately, hospital-based studies have limited generalizability to the ED population since they excluded patients discharged from the ED and enrollment typically occurred within 24 to 48 hours after admission.7 In addition, many of these studies included patients who developed delirium during their hospital course,7, 8 and a significant proportion of inpatients who were classified as having delirium may not have been delirious in the ED.
Even less is known about delirium’s effect on mortality in nursing home patients seen in the ED, despite being seven times more likely to be delirious compared to community dwelling elders.9 Conclusions derived from general geriatric datasets have limited external validity to nursing home patients because they have higher rates of dementia, poorer functional status, and higher comorbidity burden.9 There are approximately 1.5 million nursing home residents in the United States and 43% of community dwelling elders will enter a nursing home during their lifetime.10 Because up to 25% of all nursing home patients will visit the ED for an acute illness,11, 12 understanding how delirium affects nursing home patients is crucial.
Goals of This Investigation
Because there is a paucity of data regarding the relationship between delirium in he ED and long term mortality, and little is known about its effect on nursing home patients, we sought to determine if delirium is an independent predictor of 6-month mortality in older ED patients regardless of their admission status, and to assess if this relationship is modified by nursing home residence.
Methods
Study Design and Setting
This was a prospective cohort study conducted at a tertiary care, academic ED with an annual census of approximately 55,000 visits. Approximately 10% were 65 years and older. While no outcomes data from this cohort has been published, portions of this cohort have been used for previous publications which investigated delirium risk factors in ED patients, recognition of delirium by emergency physicians, and delirium in nursing home patients seen in the ED.2, 9 The analysis of delirium in the ED and 6-month mortality was designed a priori. The local institutional review board reviewed and approved this study using verbal consent.
Selection of Participants
This was a convenience sample of patients enrolled from May 2007 to August 2008 between 8AM and 10PM. The enrollment window was based upon availability of funding and personnel. Patients who were 65 years and older and were in the ED for less than 12 hours at the time of enrollment were included. Patients who refused consent, were non-English speaking, were previously enrolled, were unable to follow simple commands prior to their acute illness, were comatose, or did not have a completed delirium assessment performed were excluded. We excluded patients who were present in the ED for greater than 12 hours because we wanted to minimize extraneous factors which would artificially cause new-onset delirium from prolonged exposure to known delirium precipitants (e.g. psychoactive medications). The 12-hour cut-off was based upon typical waiting room times, average duration of an older ED patient evaluation, and research assistant availability. Patients who were unable to follow simple commands prior to their acute illness were determined by surrogate interview or medical record review. These patients were considered to have severe dementia and were excluded because there are no delirium assessments that have been validated for this specific patient population. Comatose patients were excluded because a patient must be arousable to verbal stimuli in order to assess for delirium.13
Methods of Measurement
Delirium, dementia, and functional status were prospectively collected by research assistants who were blinded to this study’s hypothesis. Prior to the start of data collection, all assistants participated in an intense one-week training period where they studied training manuals, received didactic lectures, watched live patient demonstrations, and practiced the study’s assessments using simulated patient scenarios. At the end of the training period, the primary investigator (JHH) observed the research assistants perform these assessments in actual ED patients to determine competency.
Delirium was assessed using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). The CAM-ICU was chosen because of its brevity (< two minutes), ease of use, and excellent interrater reliability.14 This delirium assessment uses the exact same construct as the Confusion Assessment Method (CAM) and utilizes four features: 1) acute onset of mental status changes or a fluctuating course, 2) inattention, 3) disorganized thinking, and 4) altered level of consciousness.15 Like the CAM, a patient must possess both features 1 and 2, and either 3 or 4 in order to meet criteria for delirium. The CAM-ICU has been validated in both mechanically ventilated and non-mechanically ventilated patients. This assessment is highly sensitive (93% – 100%) and specific (89% – 100%), and has excellent interrater reliability between physicians and nurses (kappa = 0.84 – 0.96).14, 16 Because the CAM-ICU’s ease of use and excellent interrater reliability in non-physicians, no reliability testing was performed during the study.
Patients were considered to have dementia if they had one of the following: (1) documented dementia in the medical record prior to the index ED visit, (2) a Mini-Mental State Examination (MMSE) less than 24,17 or (3) a short form Informant Questionnaire on Cognitive Decline in the Elderly score (IQCODE) greater than 3.38.18 All three were used to be conservative and because no single dementia assessment was valid for the entire cohort. The MMSE is widely used to measure cognitive impairment and has very good test-retest reliability (r = 0.83).17 A cutoff of less than 24 out of a possible 30 points is 85% sensitive and 98% specific.19 The MMSE was not performed in patients with delirium because it would not have accurately reflected premorbid cognitive status. The short form IQCODE is an informant questionnaire with 16-items and is highly reliable (alpha = 0.95) with moderately high test-retest reliability (r = 0.75).20 A cut-off of 3.38 out of 5.00 is 79% sensitive and 82% specific.21 In patients without a surrogate present in the ED, the IQCODE was not completed. Twenty eight (2.9%) patients did not have a MMSE, IQCODE, and a documented history of dementia in the medical record. We assumed that these patients did not have dementia.
Premorbid functional status was determined by the Katz Activities of Daily Living (Katz ADL). This widely used assessment is a 0 to 6 scale (0 being completely dependent) and is based upon the patient’s level of independence in bathing, dressing, toileting, transferring, continence, and feeding.22 Patients with a score less than or equal to 4 were considered to be functionally dependent. Ten patients (1.6%) did not have a Katz ADL measured; these patients were considered not to be functionally dependent.
The Charlson Comorbidity Index, which is the sum of a weighted index that takes into account the number and seriousness of preexisting comorbid conditions, was used to measure comorbid burden.23 A modified Acute Physiology and Chronic Health Evaluation II (APACHE II) score was used quantify illness severity.24 The APACHE II score is a continuous variable based upon age and the initial values of 12 routine physiologic measurements. However, age, Glasgow Coma Scale, and serum potassium were removed from its calculation. Age was not used in the APACHE II because we planned to incorporate this covariate into the multivariable model. Glasgow coma scale was not included because it was not collected, and we had other measures of cognitive status. Serum potassium was not recorded. The Charlson Comorbidity Index and modified APACHE II were obtained from the medical record severalmonths after patient enrollment.
Outcome Measures
Death within six months after enrollment was the primary outcome variable and was ascertained by medical record review or searching the Social Security Death Index using the following algorithm: (1) The electronic medical record was searched, looking for date of death based upon death certificates or clinical communications between the patients’ families and their physicians. (2) Patients who had a documented ED visit, outpatient clinic visit, or hospitalization after 6-months were considered to be alive at 6 months. (3) For the remaining patients whose survival status could not be determined from the medical records, date of death was searched in the Social Security Death Index (SSDI). (4) Patients without a death recorded in the Social Security Death Index one year after the index visit were considered to be alive at 6-months. The SSDI is 88.2% sensitive for death for the general population.25 Its sensitivity improves in patients who are older and born in the United States, who comprise the vast majority of our patient population.25 Five hundred twenty four (83.4%) patients had a recorded death in the medical record or SSDI, or had an ED or hospital visit documented in their medical record 6 months after the index visit.
Primary Data Analysis
Patient’s baseline characteristics were presented using proportions for categorical variables and medians and interquartile ranges for continuous variables. Cumulative probabilities of survival were estimated within six months from enrollment date using the Kaplan-Meier method. The survival curves were stratified by delirium status and further categorized by nursing home status. Because the Proportional Hazards assumption was met using the Schoenfeld residuals method,26 Cox proportional hazards regression was performed to determine if delirium in the ED was independently associated with 6-month mortality after controlling for age, comorbidity burden (Charlson Comorbidity Index), severity of illness (modified APACHE II), dementia, functional dependence (Katz ADL ≤ 4), and nursing home residence. Given the number of events (81 deaths) present, we limited the Cox proportional hazards regression model to seven or eight covariates in order to avoid overfitting.27 The selection of covariates was made a priori based on expert opinion and previous literature. In addition, we incorporated a two-factor interaction term (delirium * nursing home) in order to assess the effect modification of nursing home residence on the relationship between delirium in the ED and 6-month mortality. A p-value < .05 was considered statistically significant. The reliability of the final regression model was internally validated using the Bootstrap method.27 Two thousand sets of bootstrap samples were generated by re-sampling the original data and the optimism was estimated to determine the degree of overfitting.27 An optimism value > 0.80 indicated no evidence of overfitting.27 Variance Inflation factors were used to determine collinearity. Schoenfeld residuals were also analyzed to determine goodness-of-fit and assess for outliers. Hazard ratios (HRs) with their 95% confidence intervals (95% CIs) were reported.
In the main analysis, we assumed that patients who were lost to follow-up and without a recorded death in the Social Security Death Index were alive at 6 months. Thus we conducted a sensitivity analysis to assess if there was any potential bias introduced by making this assumption. In the sensitivity analysis, the Cox proportional regression model was re-run while censoring these patients when they were “last seen alive” in the medical record. Cox proportional hazards regression model was performed with the same covariates mentioned in the previous paragraph. All statistical analyses were performed using Open source R statistical software, version 2.9.2 (http://www.r-project.org/).
Results
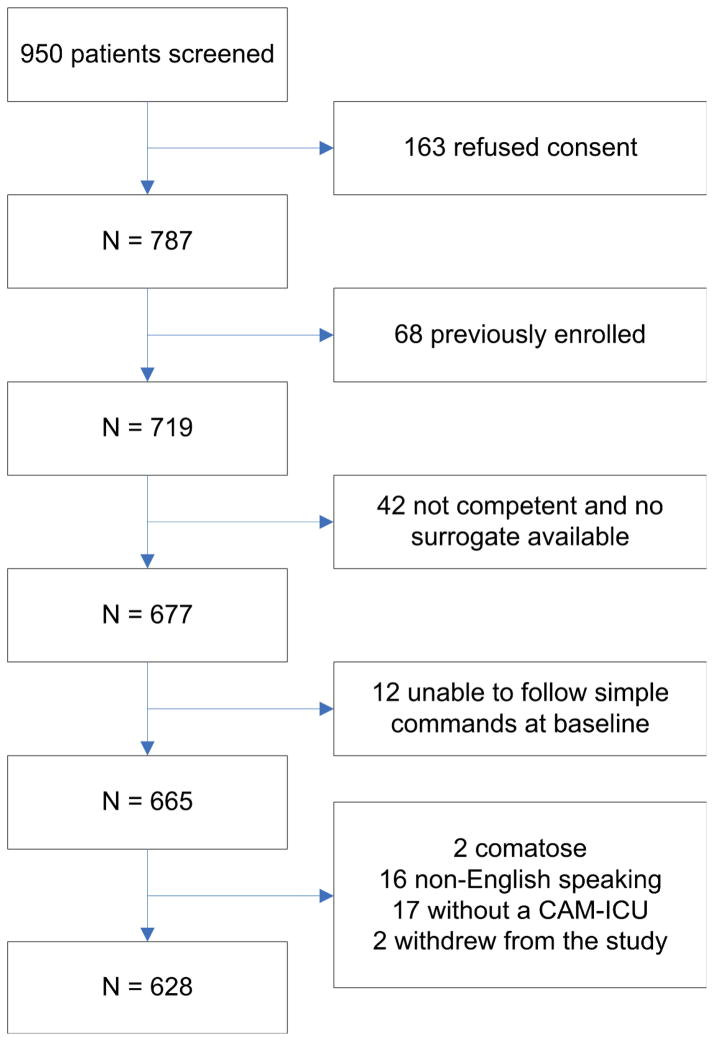
A total of 628 patients met enrollment criteria (Figure 1) and of these, 351 (55.9%) were admitted to the hospital, 58 (9.2%) were from the nursing home, 108 (17.2%) met criteria for delirium, and 81 (12.9%) died within 6-months. Patient demographics and characteristics stratified by delirium status are listed in Table 1. Patients who were delirious in the ED were more likely to be older and severely ill, and have higher comorbidity burden. In addition, delirious patients were more likely to have dementia, premorbid functional impairment, hearing impairment, and reside in a nursing home. In regards to emergency physician diagnosis categorized by organ system, patients who were delirious in the ED were less likely to have cardiovascular and gastrointestinal diagnoses, but were more likely to have neurologic diagnoses.
Figure 1.
Patients meeting inclusion and exclusion criteria.
Table 1.
Patient demographics and characteristics stratified by delirium status. Continuous variables are represented as median (interquartile range), and categorical variables are represented as absolute number (proportion).
| Variable | Delirium N=108 | No Delirium N=520 |
|---|---|---|
| Median Age (IQR) | 78 (72, 84) | 74 (69, 80) |
| Female | 65 (60.2) | 300 (57.7) |
| Non-white | 23 (21.3) | 88 (16.9) |
| Dementia | 68 (63.0) | 213 (41.0) |
| Katz ADL ≤ 4 | 52 (48.2) | 85 (16.4) |
| Nursing Home Residence | 20 (18.5) | 38 (7.3) |
| Median Modified APACHE II (IQR) | 3 (2, 5) | 2 (1, 4) |
| Median Charlson (IQR) | 3 (2, 4) | 2 (1, 4) |
| Triage ESI | ||
| 1 | 0 (0.0) | 0 (0.0) |
| 2 | 69 (63.9) | 313 (60.2) |
| 3 | 36 (33.3) | 193 (37.1) |
| 4 | 3 (2.8) | 13 (2.5) |
| 5 | 0 (0.0) | 1 (0.2) |
| Hearing Impairment | 58 (53.7) | 133 (25.6) |
| Emergency Physician Diagnosis Categorized by Organ System* | ||
| Cardiovascular | 13 (12.0) | 116 (22.3) |
| Drug Toxicity/Withdrawal | 13 (12.0) | 50 (9.6) |
| Gastrointestinal | 11 (10.2) | 81 (15.6) |
| Genitourinary | 11 (10.2) | 35 (6.7) |
| Neurologic | 17 (15.7) | 41 (7.9) |
| Hemato-oncologic | 3 (2.8) | 15 (2.9) |
| Pulmonary | 14 (13.0) | 49 (9.4) |
| Trauma/Musculoskeletal | 21 (19.4) | 104 (20.0) |
| Other | 5 (4.6) | 29 (5.6) |
IQR, interquartile range; ADL, activities of daily living; ESI, emergency severity index
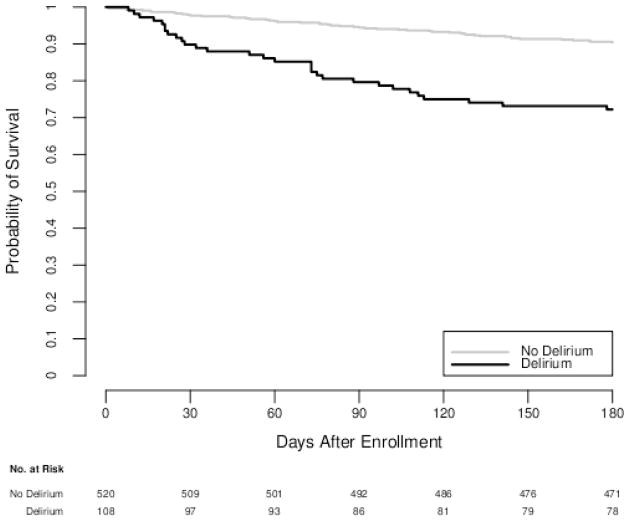
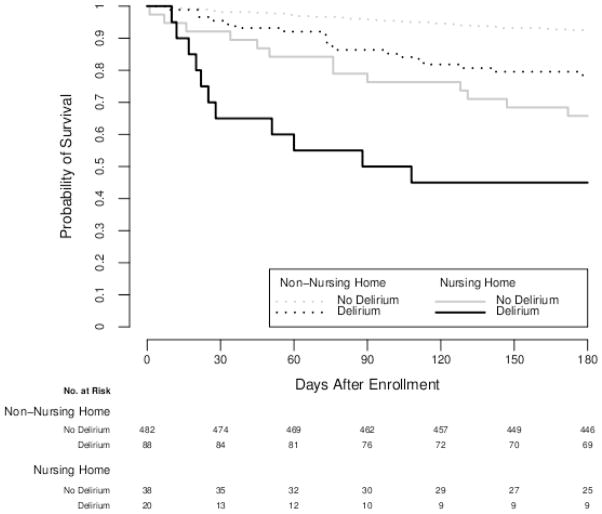
Older ED patients with delirium were more likely to die within 6-months (37.0% versus 14.3%) compared to those without delirium. The Kaplan-Meier survival curves for delirious and non-delirious ED patients can be seen in Figure 2; the survival curve declined more slowly in patients without delirium compared to those with delirium. The Kaplan-Meier survival curves for delirious patients and non-delirious patients stratified by nursing home residence can be seen in Figure 3. Within the non-nursing home patient subgroup, those with delirium were more likely to die than those without delirium (33.3% versus 13.5%). In the nursing home patient subgroup, those with delirium were also more likely to die than nursing home patients without delirium (45.8% versus 26.5%). Of note, the survival curve of non-nursing home ED patients with delirium appeared to be similar to the survival curve of nursing home ED patients without delirium.
Figure 2.
Kaplan-Meier survival curves in older emergency department patents with and without delirium. Hazard ratio of delirium on 6-month mortality is (HR = 1.72, 95% CI: 1.04 – 2.86) adjusted for age, dementia, functional dependence, comorbidity burden, severity of illness, hearing impairment, and nursing home residence. This indicates that older emergency department patients with delirium are 67% more likely to die compared to those patients without delirium.
Figure 3.
Kaplan-Meier survival curves in older emergency department patents stratified by delirium and nursing home status. In the Cox proportional hazard regression model, the “delirium*nursing home” interaction was non-significant (p=0.86), delirium in the ED’s effect on 6-month mortality was similar in nursing home and non-nursing home patients.
Using Cox proportional hazards regression (Table 2), the relationship between delirium in the ED and 6-month mortality persisted (HR =1.72, 95% CI: 1.04 – 2.86) even after adjusting for age, Charlson Comorbidity Index, modified APACHE II, dementia, functional dependence, and nursing home residence. The “delirium*nursing home” interaction was non-significant (p=0.86), providing no evidence that nursing home status modified the relationship between delirium in the ED and 6-month mortality. The regression model was internally validated and the estimated optimism was 0.92 indicating that there was no evidence of overfitting. The Variance Inflation Factor did not exceed 10 for all variables, indicating that there was no evidence of substantial collinearity. We graphically examined the Schoenfeld residuals and found overall good model fit and no significant outliers.
Table 2.
Cox proportional hazard regression model to determine delirium is independently associated with 6-month mortality.
| Variable | HR (95% CI) |
|---|---|
| Delirium | 1.72 (1.04 – 2.86) |
| Age | 1.51 (1.05 – 2.16) |
| Charlson | 1.53 (1.24 – 1.87) |
| Dementia | 1.29 (0.78 – 2.15) |
| Katz ADL ≤ 4 | 3.46 (1.45 – 8.23) |
| Modified APACHE II | 1.31 (1.10 – 1.55) |
| Nursing Home | 2.44 (1.38 – 4.29) |
ADL, activities of daily living; APACHE II, Acute Physiology and Chronic Health Evaluation II
In the main analysis, we assumed that 104 (16.6%) patients who were lost to follow-up and without a recorded death in the Social Security Death Index were alive at 6 months. In order to determine how this assumption biased our findings, we performed a sensitivity analysis and censored these patients at the date when they were “last seen alive” in the medical record. Using this assumption, the Cox proportional hazard regression was re-run. Delirium in the ED remained associated with 6-month mortality (HR = 1.67, 95% CI: 1.01 – 2.77) after adjusting for age, Charlson Comorbidity Index, modified APACHE II, dementia, functional dependence, and nursing home residence.
Limitations
Our study has several notable limitations. First, there are several potential sources of selection bias. This was a convenience sample and we did not enroll older patients who presented to the ED during early morning or late evening. Because patients who present during these times tend to be sicker, the proportion of deaths and patients with delirium may have been underestimated. There were also 163 (17.2%) patients who refused to participate in the study and 19 (2.0%) patients who did not have a CAM-ICU completed or withdrew from the study. These patients more likely to be from a nursing home compared to enrolled patients (Appendix A), and may have been more cognitively or functionally impaired. In addition, the proportion of delirious patients is higher than previously reported in literature.1, 2 This is most likely from our high proportion of nursing home patients enrolled, but it is also possible that delirious patients may have been inadvertently oversampled. However, our multivariable model adjusted for covariates that are well known to be associated with long-term mortality and should have mitigated these potential sources of selection bias.
Second, given the demanding ED environment and limited length of stays (~5 hours), we had to balance feasibility against the amount of prospective data collected. As a result, unmeasured confounders may have biased our multivariable model. We also chose to use the CAM-ICU to assess for delirium because of its ease of use, brevity, and high reliability. Though this instrument has not been formally validated in the ED setting, its validation studies included patients who were older and younger, intubated and non-intubated patients, as well as patients with and without mild dementia. Third, the CAM-ICU was performed once at the time of enrollment. Because of its fluctuating course, a small proportion of non-delirious patients may have become delirious later in the ED course. However, this misclassification would have likely biased our findings towards the null.
Fourth, we excluded patients who were unable to follow simple commands because they most likely had severe dementia and there are no delirium assessments that have been validated for this patient population.14, 15 Though the bias introduced from this exclusion is unclear, patients with severe dementia are probably more susceptible to developing delirium and may have higher mortality.9, 28 Thus, their exclusion would most likely have biased our results towards the null. Fifth, we did not perform phone follow-up to ascertain death status. In patients who were lost to follow-up, we assumed them to be alive if they had no death record in the SSDI one year after the index ED visit. However, the SSDI is highly sensitive, especially in older patients born in the United States.21 Because a minority (16.6%) were lost to follow-up before 6-months and did not have a death record in the SSDI, this bias was likely to be minimal. Additionally, we performed a sensitivity analysis and censored patients when they were “last seen alive” in the medical record. The HR from the Cox proportional hazards regression model did not change and delirium in the ED remained independently associated with 6-month mortality. Lastly, this study was performed at a single center and our findings may not be generalizable to rural or non-academic EDs.
Discussion
There are paucity of data regarding delirium in the ED and its relationship to long term outcomes. To address this deficiency, we enrolled a large cohort of older ED patients and observed that patients with delirium were more likely to die at 6-months compared to those without delirium. This relationship persisted after adjusting for age, comorbidity burden, severity of illness, dementia, functional dependence, and nursing home residence. To our knowledge, our study is also the first to evaluate how delirium affects ED patients from the nursing home setting and found that delirium had a similar impact on 6-month mortality in this unique patient population. These findings add to the existing literature and provide further evidence of the independent relationship between delirium and death across different clinical settings in non-nursing home and nursing home patients.7, 8, 29
To our knowledge, only two studies have investigated delirium and its effect on long-term mortality in the ED setting. Lewis et al. found that patients with delirium were significantly more likely to die at 3-months (14% versus 8%), but they did not adjust for potential confounders.30 Kakuma et al. observed that delirium was independently associated with higher 6-month mortality (HR = 7.2, 95% CI: 1.6 – 32.3), but their study excluded ED patients admitted to the hospital, which constitute a significant proportion of the older ED patient population.31 Our study addresses these deficiencies by adjusting for potential confounders using Cox proportional hazards regression and by enrolling patients regardless of admission status. In addition to mortality, delirium has also been linked to accelerated functional and cognitive decline, prolonged hospitalization, nursing home placement, and increased health care costs in hospitalized patients.32 Though these studies have limited generalizability to the ED setting, it is likely that these same consequences will occur in older ED patients with delirium. Additional outcome-based studies conducted in ED patients must be performed to confirm these hypotheses.
Nursing home patients are frequent users of the ED and are disproportionately more susceptible to developing delirium.9 However, little is known about delirium’s affect on their outcomes.9 We observed that nursing home patients with delirium in the ED were more likely to die within 6 months compared to those without delirium. Nursing home patients have a significant financial impact on an already burdened US health care system,33 because they have higher rates of hospitalization compared to community dwelling elders.34 It is likely that delirium in nursing home patients drive a large proportion of such hospitalizations which further increases health care costs.35 In nursing home patients, health care expenditures also markedly increase around the time of death,36 which is an event that occurs with a high degree of frequency in patients with delirium. Additional research is required to better elucidate how delirium in nursing home patients affect outcomes and health care costs.
Despite being a marker of death, delirium is missed by emergency physicians in up to 75% of the cases.1, 2 This has been characterized as a serious quality of care issue,37 and may lead to higher mortality in older ED patients.31 Though the mechanisms for this are unclear, ED patients with unrecognized delirium may receive incomplete diagnostic workups and an underlying life-threatening illness may remain undiagnosed. These patients may also receive inappropriate interventions known to exacerbate delirium such as medications with anticholinergic properties or benzodiazepines.38, 39 Additionally, delirious patients who are discharged from the ED may be less likely to comprehend their discharge instructions,40 leading to poor adherence, return ED visits, and potentially increased mortality and morbidity.41, 42
The ED is ideally positioned to perform delirium surveillance because it is at the nexus of geriatric health care and serves as the gateway for the majority of hospital admissions. Consequently, the Society for Academic Emergency Medicine Geriatrics Task Force recently recommended that delirium surveillance in the ED be a key quality indicator for emergency geriatric care.43 Because the majority of delirium is the hypoactive “quiet” subtype,2 the clinical presentation can be subtle and is often missed without performing a delirium assessment.44 Currently, the Confusion Assessment Method (CAM) is the only delirium assessment validated for the ED setting. When performed by lay interviewers, this instrument is 86% sensitive and 100% specific compared to a geriatrician’s assessment.45 However, the CAM can take up to 10 minutes to perform which can be challenging in a demanding ED environment.46 Performing the CAM in high risk patients only (dementia, functional impairment, hearing impairment, or nursing home residence) may improve screening efficiency.2, 9 The CAM-ICU may be a more suitable alternative because it takes less than 2 minutes to perform, is highly reliable in physicians and nurses, is easy to use, and requires minimal training. Using only a 20-minute educational session, Pun et al. reported that bedside nurses were able to perform the CAM-ICU with a high degree of concordance with research staff raters (kappa = 0.92).47 However, the CAM-ICU still requires validation in the ED setting and delirium screening strategies that maximize accuracy yet minimize burden to the ED staff must be developed. These studies are currently ongoing.
Once delirium is diagnosed in the ED, the diagnostic evaluation should then focus on uncovering the underlying etiology.48 Infections, such as a urinary tract infection or pneumonia, dehydration, electrolyte abnormalities, central nervous system insults, and medication reactions are common causes.32 If admitted, physicians at the next level of care should be notified of the patient’s delirium status. Other than these interventions, however, the optimal management of delirium is still unclear, especially within the ED setting. Several multi-component delirium interventions have been developed for hospitalized patients and can be tailored for the ED,49, 50 but their efficacy is questionable.51 Because many of these interventions were started 24 to 48 hours after admission, early detection and early intervention of delirium in the ED may improve their effectiveness similar to what has been observed in sepsis and ST-elevation myocardial infarction care.52, 53 A multi-faceted line of research must be undertaken to develop delirium interventions specifically tailored for the ED setting and determine their cost-effectiveness using randomized control trial methodology.
Conclusion
In older ED patients, delirium is an independent predictor for death, even after adjusting for age, comorbidity burden, severity of illness, dementia, functional dependence, and nursing home residence. This relationship is present regardless of nursing home residence. Future studies are needed to determine optimal screening and management strategies for delirium in the ED, and to determine if earlier detection and intervention of delirium in the ED improves patient outcomes.
Acknowledgments
We would like to thank Karen Miller, RN, MPA for her coordination of the study. We would also like to thank Amanda Laun, RN for her assistance in editing the final draft. The authors also acknolwedge Nathan Cutler, BS; Eli Zimmerman, BA; Suzanne Bryce, BA; Sara Beth Sayler, BA; Dennis Reed, EMT-P; Robert Brooks, EMT-P, and Larry Hinsley EMT-P for their assistance in data collection.
Dr. Han received support from the Vanderbilt Physicians Scientist Development grant. This study was also partially supported by the Emergency Medicine Foundation. Dr. Ely was supported in part by the National Institutes of Health AG01023 and the Veterans Affairs Tennessee Valley Geriatric Research, Education, and Clinical Center (GRECC).
Appendix A
Appendix A.
Patient demographics in enrolled patients and compared to patients who refused to participate in the study, did not have the CAM-ICU completed, or withdrew from the study. Continuous variables are represented as median (interquartile range), and categorical variables are represented as absolute number (proportion). IQR, interquartile range.
Of these screened, 182 (19.2%) refused consent, did not have a delirium assessment, or withdrew from the study. Median ages were similar between the refusal and enrolled groups. Patients who refused to participate were more likely to be female, non-white, and from a nursing home.
| Refusals and Incompletes N=182 | Enrolled N=628 | |
|---|---|---|
| Median Age (IQR) | 76 (70, 82) | 75 (69, 81) |
| Female | 116 (63.7) | 365 (58.1) |
| Non-White | 44 (24.2) | 111 (17.7) |
| Nursing Home | 29 (15.9) | 58 (9.2) |
Footnotes
Reprints not available from the authors.
This abstract was an oral presentation at the Society for Academic Emergency Medicine National Meeting, May 2009, New Orleans, LA.
References
- 1.Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;41:678–684. doi: 10.1067/mem.2003.152. [DOI] [PubMed] [Google Scholar]
- 2.Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16:193–200. doi: 10.1111/j.1553-2712.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association., American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. Task Force on DSM-IV. [Google Scholar]
- 4.McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2002 emergency department summary. Adv Data. 2004:1–34. [PubMed] [Google Scholar]
- 5.Braunwald E, Zipes D, Libby P, et al. Heart disease: a textbook of cardiovascular medicine. 7. Philadelphia: Elsevier Saunders; 2005. [Google Scholar]
- 6.Elie M, Rousseau F, Cole M, et al. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;163:977–981. [PMC free article] [PubMed] [Google Scholar]
- 7.McCusker J, Cole M, Abrahamowicz M, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162:457–463. doi: 10.1001/archinte.162.4.457. [DOI] [PubMed] [Google Scholar]
- 8.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 9.Han JH, Morandi A, Ely W, et al. Delirium in the nursing home patients seen in the emergency department. J Am Geriatr Soc. 2009;57:889–894. doi: 10.1111/j.1532-5415.2009.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kemper P, Murtaugh CM. Lifetime use of nursing home care. N Engl J Med. 1991;324:595–600. doi: 10.1056/NEJM199102283240905. [DOI] [PubMed] [Google Scholar]
- 11.Bergman H, Clarfield AM. Appropriateness of patient transfer from a nursing home to an acute-care hospital: a study of emergency room visits and hospital admissions. J Am Geriatr Soc. 1991;39:1164–1168. doi: 10.1111/j.1532-5415.1991.tb03568.x. [DOI] [PubMed] [Google Scholar]
- 12.Gabrel CS. Characteristics of elderly nursing home current residents and discharges: data from the 1997 National Nursing Home Survey. Adv Data. 2000:1–15. [PubMed] [Google Scholar]
- 13.Ely EW, Pun BT. The Confusion Assessment Method for the ICU Training Manual. Nashville, TN: Vanderbilt University; 2005. [Google Scholar]
- 14.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 16.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Holsinger T, Deveau J, Boustani M, et al. Does this patient have dementia? JAMA. 2007;297:2391–2404. doi: 10.1001/jama.297.21.2391. [DOI] [PubMed] [Google Scholar]
- 19.Hogervorst E, Combrinck M, Lapuerta P, et al. The Hopkins Verbal Learning Test and screening for dementia. Dement Geriatr Cogn Disord. 2002;13:13–20. doi: 10.1159/000048628. [DOI] [PubMed] [Google Scholar]
- 20.Jorm AF, Jacomb PA. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med. 1989;19:1015–1022. doi: 10.1017/s0033291700005742. [DOI] [PubMed] [Google Scholar]
- 21.Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145–153. doi: 10.1017/s003329170002691x. [DOI] [PubMed] [Google Scholar]
- 22.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 23.Murray SB, Bates DW, Ngo L, et al. Charlson Index is associated with one-year mortality in emergency department patients with suspected infection. Acad Emerg Med. 2006;13:530–536. doi: 10.1197/j.aem.2005.11.084. [DOI] [PubMed] [Google Scholar]
- 24.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 25.Schisterman EF, Whitcomb BW. Use of the Social Security Administration Death Master File for ascertainment of mortality status. Popul Health Metr. 2004;2:2. doi: 10.1186/1478-7954-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hess KR. Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat Med. 1995;14:1707–1723. doi: 10.1002/sim.4780141510. [DOI] [PubMed] [Google Scholar]
- 27.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 28.Sampson EL, Blanchard MR, Jones L, et al. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry. 2009;195:61–66. doi: 10.1192/bjp.bp.108.055335. [DOI] [PubMed] [Google Scholar]
- 29.Cacchione PZ, Culp K, Laing J, et al. Clinical profile of acute confusion in the long-term care setting. Clin Nurs Res. 2003;12:145–158. doi: 10.1177/1054773803012002003. [DOI] [PubMed] [Google Scholar]
- 30.Lewis LM, Miller DK, Morley JE, et al. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13:142–145. doi: 10.1016/0735-6757(95)90080-2. [DOI] [PubMed] [Google Scholar]
- 31.Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51:443–450. doi: 10.1046/j.1532-5415.2003.51151.x. [DOI] [PubMed] [Google Scholar]
- 32.Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12:7–21. [PubMed] [Google Scholar]
- 33.Spillman BC, Lubitz J. The effect of longevity on spending for acute and long-term care. N Engl J Med. 2000;342:1409–1415. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- 34.Barker WH, Zimmer JG, Hall WJ, et al. Rates, patterns, causes, and costs of hospitalization of nursing home residents: a population-based study. Am J Public Health. 1994;84:1615–1620. doi: 10.2105/ajph.84.10.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fick DM, Kolanowski AM, Waller JL, et al. Delirium superimposed on dementia in a community-dwelling managed care population: a 3-year retrospective study of occurrence, costs, and utilization. J Gerontol A Biol Sci Med Sci. 2005;60:748–753. doi: 10.1093/gerona/60.6.748. [DOI] [PubMed] [Google Scholar]
- 36.Bercovitz A, Gruber-Baldini AL, Burton LC, et al. Healthcare utilization of nursing home residents: comparison between decedents and survivors. J Am Geriatr Soc. 2005;53:2069–2075. doi: 10.1111/j.1532-5415.2005.00489.x. [DOI] [PubMed] [Google Scholar]
- 37.Sanders AB. Missed delirium in older emergency department patients: a quality-of-care problem. Ann Emerg Med. 2002;39:338–341. doi: 10.1067/mem.2002.122273. [DOI] [PubMed] [Google Scholar]
- 38.Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153:231–237. doi: 10.1176/ajp.153.2.231. [DOI] [PubMed] [Google Scholar]
- 39.Tune LE, Bylsma FW. Benzodiazepine-induced and anticholinergic-induced delirium in the elderly. Int Psychogeriatr. 1991;3:397–408. doi: 10.1017/s1041610291000832. [DOI] [PubMed] [Google Scholar]
- 40.Bryce SN, Han JH, Kripilani S, et al. Cognitive Impairment and Comprehension of Emergency Department Discharge Instructions in Older Patients. Ann Emerg Med. 2009;54:S80–81. [Google Scholar]
- 41.Clarke C, Friedman SM, Shi K, et al. Emergency department discharge instructions comprehension and compliance study. Cjem. 2005;7:5–11. doi: 10.1017/s1481803500012860. [DOI] [PubMed] [Google Scholar]
- 42.Hastings SN, Barrett A, Hocker M, et al. Older patients’ understanding of emergency department discharge information and its relationship with adverse outcomes. J Am Geriatr Soc. 2009;57:S71. doi: 10.1097/PTS.0b013e31820c7678. (Abstract) [DOI] [PubMed] [Google Scholar]
- 43.Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16:441–449. doi: 10.1111/j.1553-2712.2009.00382.x. [DOI] [PubMed] [Google Scholar]
- 44.Inouye SK, Foreman MD, Mion LC, et al. Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161:2467–2473. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 45.Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23:20–25. doi: 10.1016/s0163-8343(00)00116-x. [DOI] [PubMed] [Google Scholar]
- 46.Inouye SK. The Confusion Assessment Method (CAM): Training Manual and Coding Guide. Yale University School of Medicine; 2003. [Google Scholar]
- 47.Pun BT, Gordon SM, Peterson JF, et al. Large-scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centers. Crit Care Med. 2005;33:1199–1205. doi: 10.1097/01.ccm.0000166867.78320.ac. [DOI] [PubMed] [Google Scholar]
- 48.Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156:1–20. [PubMed] [Google Scholar]
- 49.Cole MG, McCusker J, Bellavance F, et al. Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial. CMAJ. 2002;167:753–759. [PMC free article] [PubMed] [Google Scholar]
- 50.Pitkala KH, Laurila JV, Strandberg TE, et al. Multicomponent geriatric intervention for elderly inpatients with delirium: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2006;61:176–181. doi: 10.1093/gerona/61.2.176. [DOI] [PubMed] [Google Scholar]
- 51.Milisen K, Lemiengre J, Braes T, et al. Multicomponent intervention strategies for managing delirium in hospitalized older people: systematic review. J Adv Nurs. 2005;52:79–90. doi: 10.1111/j.1365-2648.2005.03557.x. [DOI] [PubMed] [Google Scholar]
- 52.Rivers E, Nguyen B, Havstad S, et al. Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 53.Antman EM, Hand M, Armstrong PW, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]