Abstract
Background:
Numerous cross-sectional studies have suggested that chronic periodontitis is a risk factor for cardiovascular diseases. There is evidence that periodontitis and cardiovascular diseases are linked by inflammatory factors including C-reactive protein. The purpose of the study was to investigate the levels of CRP and PNM cells as a marker of inflammatory host response in the serum of chronic periodontitis patients and in patients with CVD.
Materials and Methods:
Study population included 75 patients; both male and female above 35 years were included for the study. The patients were divided into three groups of 25 each – Group I: Chronic periodontitis patients with CVD, Group II: Chronic periodontitis patients without CVD and Group III: Control subjects (without chronic periodontitis and CVD). Patients with chronic periodontitis had ≥8 teeth involved with probing depth (PD) ≥5 mm involved. The control group had PD ≤ 3 mm and no CVD. Venous blood was collected from the patients and C-reactive protein levels were analyzed by immunoturbidimetry. PMN was recorded by differential count method.
Results:
On comparison, OHI-S Index, GI, mean PD, CRP and PMN values showed significant difference from Group I to III. CRP level was highly significant in Group I when compared with Group II and Group III. PMN level was highly significant in Group I when compared with Group III PMN level which was not significant.
Conclusion:
This study indicated that periodontitis may add the inflammation burden of the individual and may result in increased levels of CVD based on serum CRP levels. Thus, controlled prospective trials with large sample size should be carried out to know the true nature of the relationship if indeed one exists.
Keywords: Chronic periodontitis, C-reactive proteins, cardiovascular disease, polymorphonuclear leukocytes
INTRODUCTION
Periodontitis is a common chronic infection of the supporting tissue of the teeth, epidemiologically associated with cardiovascular disease.[1] Periodontitis has been proposed as having an etiological or modulating role in cardiovascular and cerebrovascular diseases, diabetes, respiratory diseases and adverse pregnancy outcome.[2] Patients suffering from severe periodontitis have increased local production of inflammatory cytokines (IL-7β, TNF and IL-6) and moderate systemic inflammatory response (defined by raised concentration of CRP, fibrinogen and moderate leukocytosis).[3] C-reactive proteins (CRP) is a strong, type-I acute phase protein, which is synthesized by hepatocytes and other cell types, including monocytes, endothelial cells, fibroblast and adipocytes.[4] Chronic periodontitis is shown to raise inflammatory markers such as CRP in the blood, which is also risk indication for cardiovascular disease.[5,6] Therefore, a cross-sectional study was carried for the assessment of relationship between chronic periodontitis and cardiovascular disease by using PMN and serum CRP as a potential marker.
MATERIALS AND METHODS
This project was reviewed by the board of ethical committee for the dental college and the project envisaged, then the clearance was obtained. Participation of the subjects in this study did not affect any treatment decisions regarding medical care. The subjects were divided into three groups of 25 each – Group I: Cardiovascular diseases patients with chronic periodontitis, Group II: Chronic periodontitis without cardiovascular diseases and Group III: Control subjects (without cardiovascular diseases and chronic periodontitis). Chronic periodontitis patients and controls were included from Department of Periodontics, H.K.E. Society's S. Nijalingappa Institute of Dental Sciences and Research, Gulbarga. Cardiovascular disease patients were included from Basaveshwar Hospital Gulbarga.
Periodontal condition
Both males and females of age group ≥35 years were selected for the study. Patient with chronic generalized periodontitis had ≥8 teeth, with probing depth (PD) >5 mm were involved. The control group PD ≤ 3 mm had no cardiovascular diseases (CVDs).
Cardiovascular criteria
The diagnosis was based on chest pain associated with typical electrocardiogram (ECG) changes.
Exclusion criteria
Patient with chronic inflammatory or immunological conditions such as arthritis, chronic obstructive airway diseases, type 1 and type 2 diabetic, pregnant and lactating women, patient receiving antibiotic therapy from past 6 months and patient who had periodontal therapy in past 3 months and with increased BMI were excluded from the study.
Armamentarium used in the study
Mouth mirror, Williams graduated periodontal probe, tweezers, kidney tray, gloves, mouth mask, cotton swab, gauze strips, disposable syringe and needle, sterilium, tourniquet, test tube and Dettol solution were used. A detailed medical and dental history was taken from each patient in the prepared proforma.
Clinical parameters
The periodontal examination included clinical measurements of OHI-S Index by Green and Vermillion (1964), Gingival Index by Loe and Sillness (1963) and probing depth or loss of attachment.
C-reactive protein
Sample collection
2 ml of venous blood was collected and transferred to a sterilized test tube and sent to lab for analysis as early as possible.
Content
Reagent-1: Tri buffer (pH 6.7), Reagent-2: Anti-CRP antibody calibration solution (41 mg/L).
Procedure
CRP examination was done manually by immuno-turbidimetry method using biosino kit in semi-auto Analyzer Erba Chem 7 by absorbance made using microcuvettes. Bring reagent to room temperature and add 560 microliters of reagent-1 into a microcuvettes, after this add 24 microliter serum or calibrator into microcuvette and mix them well and incubate for 5 minutes at 37 °C. Then measure absorbance of mixture at 340 nm in the semi autoanalyzer and record absorbance as (A1) and 140 microliter of reagent-2 added into the microcuvette. Mix the mixture well, incubated at 37°C for 5 minutes. Measure absorbance of the mixture (solution) at 340 nm in semiautoanalyzer and record absorbance as (A2).
ΔA = A2 – A1, for calculation.
Reference value
<5 mg/L (according to IFCC/CRMA470 Protein standardized).
RESULTS
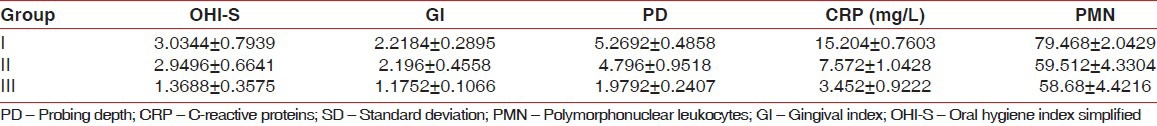
Figure 1 and Table 1 shows student t-test and mean ± standard deviation. On comparison, Group-I and Group-II showed no statistical significance between OHI-S, GI but PD was statistically significant in Group- I. The CRP and PMN values were highly statistically significant in Group-I when compared with Group-II. All the clinical parameter such as OHI-S, GI, PD, CRP and PMN values were highly significant in Group-I when compared with Group-III. The PMN value was not statistically significant between Group-II and Group-III but other parameters such as OHI-S, GI; PD and CRP were statistically highly significant in Group-II when compared with Group-III.
Figure 1.
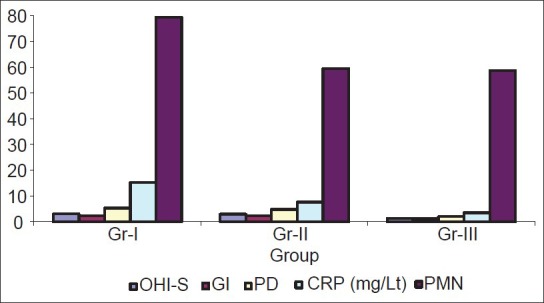
Comparison of study parameters (mean ± SD)
Table 1.
Comparison of study parameters (mean±SD)
DISCUSSION
Periodontal disease is characterized by inflammation and destruction of the supporting tissues of the affected teeth. CRP in particular has been the focus of attention as a key marker of atherosclerosis, and elevated levels (e.g., 2.1 mg/L) constitutes a risk predictor for cardiovascular disease (CVD). CRP is currently regarded as a biomarker of systemic inflammation. In the present study, subjects with CVDs and chronic periodontitis and only chronic periodontitis without CVD showed a significant association between the number of mean Probing depth (PD) and increased (CRP) when compared with control. This finding is in correlation with studies conducted by Aluto et al.,[7] who showed periodontitis had significant increased odds of being at above average risk for CVD. Recently Salzberg et al.[8] reported that patients with aggressive periodontitis had increased serum concentrations of CRP. Similar to these previous finding, our results showed that serum CRP levels were higher in periodontitis patients with or without CVD than healthy subjects. Recently, a study done by Gulay Tuter et al.[9] showed patients with chronic periodontitis and with coronary artery disease had statistically significant elevation in serum HsCRP levels compared to healthy subjects. Statistical significant elevations of mean CRP were noted in subjects with both CVDs and chronic periodontitis and only chronic periodontitis without CVD. In the present study, CRP levels were increased three-fold in condition with both cardiovascular diseases and chronic periodontitis and was increased by two-fold with chronic periodontitis without CVD when compared with controls and is correlated with the study done by Ingrid Glurich et al.[10] Deposition of CRP was documented along carotid arterial walls in association with atheromatous plaque. Zhu et al.[11] recently demonstrated that the total pathogen burden was a significant predictor of levels of CRP and postulated that increased levels of CRP contribute to the development of CVD through modulation of the inflammatory response. In the present study, the values of PMN were highly significant in Group-I (CVDs with chronic periodontitis) when compared with Group-II (chronic periodontitis without CVDs) and Group-III Control (without chronic periodontitis and cardiovascular diseases) and was consistent with Syrajnen et al.[12] study. Loesche[13] reviewed studies suggested that periodontal disease is a risk factor for heart diseases’ he postulated that oral diseases lead to low-level bacteremia and elevated WBC as well as systemic endotoxemia, which affects endothelial integrity metabolism of plasma lipoprotein, blood coagulation functioning of platelets. From these studies the systemic consequences of periodontal infections proposed to risk for vascular thromboembolic events. C-reactive protein (CRP) is a marker of nonspecific inflammation, which has been found to predict cardiovascular events. It is known that factors such as stress, inflammatory diseases, smoking, and diet, lack of physical exercise, obesity and atherosclerotic lesions increase CRP levels (Labarrere and Zaloga 2004).[14]
This study has certain limitations. First, CRP assaying method was not done by high-sensitivity CRP measurements the detection limit for CRP measurements was 5 mg/l in the present study. According to recent meta-analysis on CRP in relation to periodontitis done by Paraskevas et al.,[15] only high-sensitivity CRP measurements were accepted and therefore several studies were excluded.
Second, smoking has also been suggested as possible confounding effect, which was not recorded, higher CRP levels in smokers than in nonsmoker have been reported by Ridker and Russell et al.[16]
This study indicated that periodontitis may add to the inflammation burden of the individual and may result in increased levels of CVD based on serum CRP levels. As both, the disease CVD and chronic periodontitis share several risk factors including smoking, age, diabetes and socioeconomic status. The epidemiological evidence to data shows a significant but modest relationship between periodontitis and CVD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Loos BG, Craandijk J, Hoek FJ, Wertheim-van Dillen PM, van der Velden U. Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. J Periodontol. 2000;71:1528–34. doi: 10.1902/jop.2000.71.10.1528. [DOI] [PubMed] [Google Scholar]
- 2.Ide M, McPartlin D, Coward PY, Crook M, Lumb P, Wilson RF. Effect of treatment of chronic periodontitis on levels of serum markers of acute-phase inflammatory and vascular responses. J Clin Periodontol. 2003;30:334–40. doi: 10.1034/j.1600-051x.2003.00282.x. [DOI] [PubMed] [Google Scholar]
- 3.Ebersole JL, Machen RL, Steffen MJ, Willmann DE. Systemic acute-phase reactants, c-reactive protein and haptoglobin, in adult periodontitis. Clin Exp Immunol. 1997;107:347–52. doi: 10.1111/j.1365-2249.1997.270-ce1162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebersole JL, Cappelli D. Periodontitis Humans and Non-Human Primates: Oral systemic linkage inducing acute phase proteins. Periodontal. 2000;23:19–49. doi: 10.1902/annals.2002.7.1.102. [DOI] [PubMed] [Google Scholar]
- 5.Shishehbor MH, Bhatt DL, Topol EJ. Using C-reactive protein to assess cardiovascular disease risk. Cleve Clin J Med. 2003;70:634–40. doi: 10.3949/ccjm.70.7.634. [DOI] [PubMed] [Google Scholar]
- 6.Shklair IL, Loving RH, Leberman OF, Rau CF. C-reactive protein and periodontal diseases. J Periodontol. 1968;39:93–5. doi: 10.1902/jop.1968.39.2.93. [DOI] [PubMed] [Google Scholar]
- 7.Blum A, Front E, Peleg A. Periodontal care may improve systemic inflammation. Clin Invest Med. 2007;30:E114–7. doi: 10.25011/cim.v30i3.1079. [DOI] [PubMed] [Google Scholar]
- 8.D’Aiuto F, Parkar M, Andreou G, Suvan J, Brett PM, Ready D, et al. Periodontitis and systemic inflammation: Control of the local infection is associated with a reduction in serum inflammatory markers. J Dent Res. 2004;83:156–60. doi: 10.1177/154405910408300214. [DOI] [PubMed] [Google Scholar]
- 9.Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA. C-reactive protein levels in patients with aggressive periodontitis. J Periodontol. 2006;77:933–9. doi: 10.1902/jop.2006.050165. [DOI] [PubMed] [Google Scholar]
- 10.Romero-Corral A, Sierra-Johnson J, Lopez-Jimenez F, Thomas RJ, Singh P, Hoffmann M, et al. Relationships between leptin and C-reactive protein with cardiovascular disease in the adult general population. Nat Clin Pract Cardiovasc Med. 2008;5:418–25. doi: 10.1038/ncpcardio1218. [DOI] [PubMed] [Google Scholar]
- 11.Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: The heart of the matter. J Am Dent Assoc. 2006;137:14–20. doi: 10.14219/jada.archive.2006.0402. [DOI] [PubMed] [Google Scholar]
- 12.Slade GD, Ghezzi EM, Heiss G, Beck JD, Riche E, Offenbacher S. Relationship between periodontal disease and C-reactive protein among adults in the Atherosclerosis Risk in Communities study. Arch Intern Med. 2003;163:1172–9. doi: 10.1001/archinte.163.10.1172. [DOI] [PubMed] [Google Scholar]
- 13.Gortney JS, Sanders RM. Impact of C-reactive protein on treatment of patients with cardiovascular disease. Am J Health Syst Pharm. 2007;64:2009–16. doi: 10.2146/ajhp060542. [DOI] [PubMed] [Google Scholar]
- 14.Yasunari K, Maeda K, Nakamura M, Yoshikawa J. Oxidative stress in leukocytes is a possible link between blood pressure, blood glucose, and C-reacting protein. Hypertension. 2002;39:777–80. doi: 10.1161/hy0302.104670. [DOI] [PubMed] [Google Scholar]
- 15.Loesche WJ. Periodontal disease as a risk factor for heart disease. J Periodontol. 1994;15:978–82. [PubMed] [Google Scholar]
- 16.Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J Clin Periodontol. 2008;35:277–90. doi: 10.1111/j.1600-051X.2007.01173.x. [DOI] [PubMed] [Google Scholar]


