Abstract
Multiple myeloma is a malignant neoplasm that is characterized by a monoclonal proliferation of plasma cells. Oral and maxillofacial manifestations as an initial sign or symptom of multiple myeloma are rare. A 58-year-old male patient presented with generalized gingival enlargement for last 6 months. Based on clinical presentation, a diagnosis of gingival hyperplasia was made. After Phase I therapy, excisional biopsy was taken in anterior mandibular region and excised tissue was sent for histopathological examination. The histopathology report revealed a lining of stratified squamous epithelium with foci of ulceration. The subepithelial zone showed infiltration by sheets of mainly binucleate and multinucleate plasma cells, few cells being less differentiated. Rounded cytoplasmic inclusion bodies were identified in many of these cells. After a series of clinical investigations, a case of “multiple myeloma” was diagnosed. Patient presenting with generalized gingival hyperplasia should be worked up for systemic disease like multiple myeloma.
Keywords: Gingival enlargement, multiple myeloma, plasma cells
INTRODUCTION
Multiple myeloma is a malignant neoplasm that is characterized by a monoclonal proliferation of plasma cells. It is the most common primary malignancy of bone. The cause of this disease is unknown. It occurs most frequently in older age group and in men (2:1). The clinical manifestations of the disease occur as a result of an expanding plasma cell mass in the bone marrow and other factors produced by these cells such as monoclonal immunoglobulin, Bence-Jones proteins and osteoclast activating factors.[1] The common clinical signs and symptoms of multiple myeloma include pain in the bone, fatigue, anemia and infectious diseases. Radiography frequently shows the typical “punched-out” osteolytic lesions.[2]
Oral and maxillofacial manifestations as an initial sign or symptom of multiple myeloma are rare.[2] In 12-15% of cases, oral manifestations are the initial presenting sign.[3,4,5] Oral involvement can be apparent as swelling, orofacial pain, mobility of teeth, numbness and paresthesia, hemorrhage, fracture and root resorption.[6] We hereby present a case of multiple myeloma with first clinical manifestation as generalized gingival enlargement.
CASE REPORT
A 58-year-old male patient was referred to our department because of the generalized enlargement of gingiva. The enlargement was first noted by the patient 6 months prior to the referral, and progressed steadily since then. Patient also complained of weakness, fatigue and anorexia. The intraoral examination revealed soft, granular, friable, non-tender, and red/magenta enlargement that bled spontaneously. The growth was painless in nature. Purulent discharge from some areas of the enlargement was also noted. The enlargements were present on both buccal and lingual/palatal sides [Figure 1]. On physical examination, Grade III mobility was observed in 16, 17, 18, 36, 37. General examination showed signs of pallor and poor nourishment. The medical history of the patient included epilepsy for which he took prescribed medication with no occurrence of seizure for last 10 years. Based on clinical presentation, a provisional diagnosis of inflammatory gingival enlargement, plasma cell gingivitis or Wegener's granulomatosis was made. Routine blood investigations were done along with HIV and Hepatitis B and sputum examination to rule out any leukemic infiltration and enlargement associated with tuberculosis. Orthopantomography was advised, which revealed severe bone loss in 16, 17, 18 and 36, 37 regions. Oral hygiene status of the patient was good. After Phase I therapy and consultation with the physician, gingivectomy was performed in anterior mandibular region and excised tissue was sent for histopathological examination. Periodontal dressing was given after performing gingivectomy. The patient was followed up every week [Figure 2] but after 1 month the clinical examination revealed recurrence of enlargement in the anterior mandibular region [Figure 3]. The histopathology report revealed a lining of stratified squamous epithelium with foci of ulceration. The subepithelial zone showed infiltration by sheets of plasma cells mainly mature with few being less differentiated [Figure 4]. Binucleate and multinucleate plasma cells were also noted [Figure 5]. Presence of rounded cytoplasmic inclusion bodies was identified in many of these cells. Based on these findings, serum protein electrophoresis and urine analysis for Bence-Jones proteins was carried out. Serum protein electrophoresis revealed monoclonal increase in immunoglobulin G levels. No Bence-Jones proteins were detected in urine. Subsequently, patient was advised to undergo cranial and pelvic radiography [Figures 6 and 7]. The radiographs revealed small punched out osteolytic lesions in the cranium and pelvic region. The patient was referred to an oncologist for systemic screening. Bone marrow aspiration was done, which showed a marginal prominence of plasma cells. The biochemistry revealed high values of alkaline phosphatase and lowered albumin/globulin ratio. Bone marrow biopsy also revealed a patchy prominence of plasma cells. The patient was diagnosed as a case of multiple myeloma and chemotherapy was started with thalidomide. The patient reported for follow-up after 1 month. The gingiva appeared normal after the start of chemotherapy [Figure 8].
Figure 1.

Pre-operative view
Figure 2.

Gingiva 10 days after excisional biopsy was taken
Figure 3.

Recurrence after 1 month of biopsy
Figure 4.
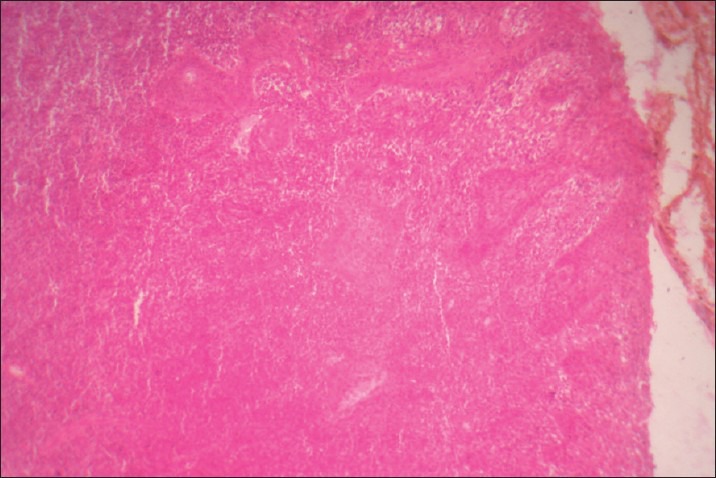
Areas of ulceration and sheets of plasma cells
Figure 5.
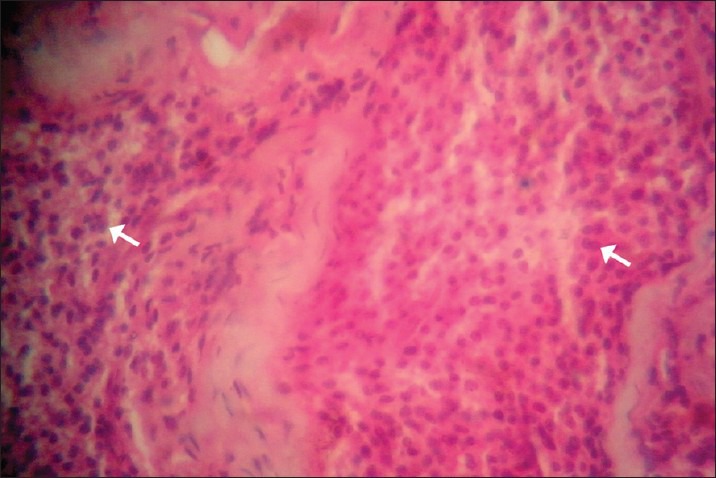
Multinucleate and binucleate plasma cells
Figure 6.

Pelvic radiograph showing osteolytic lesions
Figure 7.
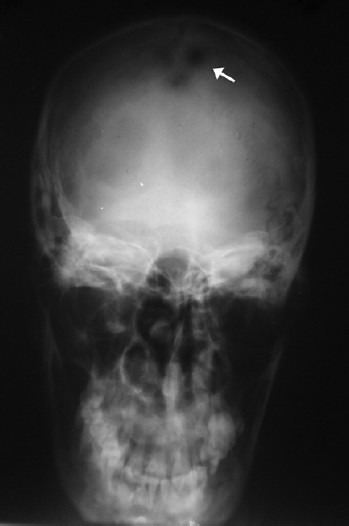
Skull radiograph showing osteolytic lesions
Figure 8.

Normal gingiva 1 month after chemotherapy
DISCUSSION
Multiple myeloma is the most aggressive plasma cell neoplasia and most common primary malignancy of bone.[7] It is characterized by monoclonal proliferation of neoplastic plasma cells at multiple intrabony sites. It has a predilection for areas of active hematopoiesis such as the lumbar spine, ribs, and pelvic bones.[1,8,9] The malignancy was first described in 1848. Jawbone involvement in multiple myeloma is common and often occurs in the advanced stages of the disease. Jaw involvement in multiple myeloma was reported by Bruce and Royer[9] to have a prevalence rate of 28.8% (17 of 59 total cases). Epstein et al.,[6] reported that 14.1% of 783 multiple myeloma cases had oral manifestations. Maxillofacial manifestations as an initial sign or symptom of multiple myeloma are rare. Lesions such as swelling, orofacial pain, mobility of teeth, numbness and paresthesia, hemorrhage, fracture and root resorption are more frequently found in the mandible than in the maxilla, especially in the posterior third and angle of the jaw, perhaps because of greater hematopoietic activity in these areas.[6,10] A radiographic survey of patients with multiple myeloma reveals multiple well-defined “punched out” radiolucencies involving bone. These radiolucent areas of bone contain the abnormal plasma cell proliferations that characterize the disease. In our case, a generalized gingival enlargement appeared as a presenting manifestation of multiple myeloma. Type 2 bone involvement was seen, which is by far, the most common presentation of multiple myeloma.[6]
In conclusion, oral manifestation is a common phenomenon seen in many malignancies including multiple myeloma. It may be the initial or early sign of the disease. Dental surgeons can play an important role in the early recognition of oral lesions with underlying systemic disease, thus preventing the morbidity and mortality associated with such pathologies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lee SH, Huang JJ, Pan WL, Chan CP. Gingival mass as the primary manifestation of multiple myeloma: Report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:75–9. doi: 10.1016/s1079-2104(96)80380-5. [DOI] [PubMed] [Google Scholar]
- 2.Shibata M, Kodani I, Doi R, Takubo K, Kidani K, Sakai H, et al. Multiple myeloma presenting symptoms in the oral and maxillofacial region. Yonago Acta medica. 2003;46:77–81. [Google Scholar]
- 3.Henderson D, Rowe NL. Myelomatosis affecting the jaws. Br J Oral Surg. 1968;6:161–72. doi: 10.1016/s0007-117x(68)80031-9. [DOI] [PubMed] [Google Scholar]
- 4.Lewin RW, Cataldo E. Multiple myeloma discovered from oral manifestation: Report of case. J Oral Surg. 1967;25:69–72. [PubMed] [Google Scholar]
- 5.Miller CD, Goltry RR, Shenasky JH. Multiple myeloma involving the mandible: Report of a case. Oral Surg Oral Med Oral Pathol. 1969;28:603–9. doi: 10.1016/0030-4220(69)90270-9. [DOI] [PubMed] [Google Scholar]
- 6.Epstein JB, Voss NJ, Stevenson MP. Maxillofacial manifestations of multiple myeloma. Oral Surg Oral Med Oral Pathol. 1984;57:267–71. doi: 10.1016/0030-4220(84)90182-8. [DOI] [PubMed] [Google Scholar]
- 7.Lesmes D, Laster Z. Plasmacytoma in the temperomandibular joint: A case report. Br J Oral Maxillofac Surg. 2008;46:322–4. doi: 10.1016/j.bjoms.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Kyle RA. Diagnostic criteria of multiple myeloma. Hematol Oncol Clin North Am. 1992;6:347–58. [PubMed] [Google Scholar]
- 9.Bruce KW, Royer RQ. Multiple myeloma occurring in the jaws-a study of 17 cases. Oral Surg Oral Med Oral Pathol. 1953;6:729–44. doi: 10.1016/0030-4220(53)90199-6. [DOI] [PubMed] [Google Scholar]
- 10.Lambhertenghi-Deliliers G, Bruno E, Cortellezzi A, Fumagalli L, Morosini A. Incidence of jaw lesions in 193 patients with multiple myeloma. Oral Surg Oral Med Oral Pathol. 1988;65:533–7. doi: 10.1016/0030-4220(88)90135-1. [DOI] [PubMed] [Google Scholar]


