Abstract
Context:
Yoga as a life-style practice has demonstrated beneficial effects. The role of yoga in the elderly for such benefits merits investigation.
Aims:
The aim of this study is to examine the effects of yoga intervention on quality-of-life (QOL) and sleep quality in the elderly living in old age homes.
Settings and Design:
Single blind controlled study with block randomization of elderly homes.
Materials and Methods:
A total of 120 subjects from nine elderly homes were randomized in to yoga group (n=62) and waitlist group (n=58). Subjects in the yoga group were given yoga intervention daily for 1 month and weekly until 3 months and were encouraged to practice yoga without supervision until for 6 months. Subjects in waitlist group received no intervention during this period. Subjects were evaluated with World Health Organization Quality of Life (WHOQOL)-BREF for measuring QOL and Pittsburgh Sleep Quality Index for sleep quality in the baseline and after 6 months.
Statistical Analysis:
Independent t-test and repeated measures analysis of covariance respectively was used to measure the difference in outcome measures between the two groups at baseline and after the study period.
Results:
Subjects in the yoga group had significantly higher number of years of formal education. Subjects in the yoga group had significant improvement in all the domains of QOL and total sleep quality after controlling for the effect of baseline difference in education between the two groups.
Conclusion:
Yoga intervention appears to improve the QOL and sleep quality of elderly living in old age homes. There is a need for further studies overcoming the limitations in this study to confirm the benefits of yoga for elderly in QOL and sleep quality.
Keywords: Elderly, sleep, quality of life, yoga
INTRODUCTION
Developing countries such as China, India and Indonesia are projected to have the largest number of elderly by 2025. The elderly population in India is expected to grow from 7.6 million in 2001 to 137 million by 2021. Even within the elderly population, people over 80 years of age are increasing rapidly, posing great demands on the health-care services in the coming years.[1]
Ageing is associated with multiple medical conditions mainly due to deteriorating physiological reserves and impaired immune mechanisms. Epidemiological and population ageing studies report that chronic, non-communicable diseases such as diabetes, hypertension, ischemic heart disease and arthritis are integral part of ageing.[1] Multiple health complaints especially pain, fatigue and mobility impairment were reported to predict low quality-of-life (QOL) and especially health related QOL in older adults leading to higher risk of dependency.[2] Epidemiological studies have reported high prevalence of psychiatric disorders such as depression and dementia in elderly ranging from 9% to 35%. Further, increasing age as well as the presence of multiple chronic medical illnesses especially diabetes, vascular risk factors, physical frailty and chronic distress increase the risk of mild cognitive impairment (MCI). MCI is a transitional state between normal aging and dementia.[3] Many elderly individuals may have subsyndromal depressive symptoms and MCI, which can have an adverse impact on the QOL.
Sleep disturbance is another commonly reported problem in elderly. Sleep disturbances can affect daytime function in elderly and have a significant negative effect on the QOL. High prevalence of excessive day-time sleepiness, insomnia, night time awakenings, snoring, restlessness and periodic leg movements during sleep are reported in elderly. These sleep disturbances were strongly associated with respiratory symptoms, physical disabilities, use of non-prescription medications, depressive and anxiety symptoms, cognitive dysfunction and poorer self-perceived health.[4,5]
QOL is recognized as a concept representing individual responses to the physical, mental and social effects of illness on daily living, which influence the extent of personal satisfaction with life circumstances that can be achieved. Measuring QOL is recognized as an important add-on to objectify clinical effectiveness in recent clinical trials.[6,7]
Interestingly recent reports show increasing trends of complementary and alternative medicine usage among elderly especially for insomnia.[8] Yoga is one such mind body intervention which is increasingly being explored for therapeutic potentials in elderly. A survey carried out in the American population indicated that about 15.8 million or 6.9% of its population practice some form of yoga and a sizeable proportion willing to take it up in the future.[9] Yoga, with its roots in ancient Indian philosophy, is used for physical, mental and spiritual well-being. Some studies of yoga-based interventions have shown benefits in sleep and QOL in elderly.[10,11,12]
The current study focuses on the effects of 6-month yoga-based intervention on sleep and QOL in the elderly living in old age homes. Replication of positive benefits with yoga in the improvement of sleep and QOL in elderly will further strengthen the basis for including yoga as a life-style practice in elderly.
MATERIALS AND METHODS
Design
This is a randomized controlled study approved by the Institutional Ethical Committee of the National Institute of Mental Health and Neurosciences. Subjects willing to participate in the trial signed a written consent form after adequate information about the nature of the study. Each old-age home as a block was randomized to either yoga or waitlist group by an independent researcher who was not involved in assessments.
Sample and settings
Consenting older adults aged above 60 years were recruited from the elderly homes in and around Bangalore city, India. 152 subjects were screened across 9 elderly homes for inclusion in the study. Subjects with dementia or other neurodegenerative disorder, stroke, major depressive disorder, psychosis, anxiety disorder, severe hearing and visual impairment and those who had an inability to perform yogic practices were excluded from the study. 120 subjects fulfilling the inclusion and exclusion criteria were recruited for the study. Yoga group included 62 subjects from 3 old age homes with 16, 15 and 31 subjects in the corresponding old age home. Control group included 58 subjects from 6 old age homes with 11, 5, 9, 8, 10 and 15 subjects in the corresponding old age home. Subjects were screened with geriatric depression scale-15 (GDS-15),[13] Hindi Mental State Examination (HMSE)[14] and Mini-International Neuropsychiatric Interview (plus 5.0.0)[15] for excluding dementia, depression and other psychiatric disorders. Short version of World Health Organization Quality of Life (WHOQOL)-BREF[16] was used to measure the QOL of the subjects. WHOQOL-BREF is a self-rated questionnaire. It elicits the perceived physical health, psychological health, social relations and environment-related QOL in an individual. Sleep was assessed using Pittsburg Sleep Quality Index (PSQI),[17] which is an 18 item, self-rated questionnaire eliciting sleep quality. It has 7 subscales namely: Subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, medication use and daytime sleepiness. The score from these seven subscales were added together to derive a total score for PSQI. The old age homes with their subjects were then randomized to receive either yoga intervention or to waitlist control group. Follow-up assessments were repeated after 6 months.
Intervention
The yoga program was developed by reviewing traditional and contemporary yogic texts. This yoga package was sent for validation to ten experts in the field of yoga and integrative medicine for its appropriateness in older adults. Thus, validated yoga program consisted of Sūkṣmavyāyāma, (loosening exercises), Yogāsana (physical postures), Prāṇāyāma (breathing exercises) and meditation in the form of Nādānusandhāna (OM Meditation). Subjects in the yoga group received 60 min yoga training daily for 1 month. Following this they were to practice the same daily until the end of 6 months. However, in the 2nd and 3rd months of the study, they received 1 hour supervisory sessions weekly to reinforce the yoga practice. Subjects in the waitlist control group did not receive any intervention during the study period. Detailed report of development of yoga module is presented as a separate paper in this issue and is available on request.
Statistical analysis
Univariate statistics was used to compare the demographic and other characteristics of two groups. Intent-to-treat (ITT) analysis method by imputing the last observation carried forward (LOCF) data was employed to include all the randomized subjects for analysis. Effect of yoga intervention on QOL and sleep quality was assessed with repeated measures analysis of covariance (RMANCOVA). Statistical significance was fixed at P<0.05.
RESULTS
A total of 120 subjects (yoga=62, waitlist control=58) from 9 elderly homes were recruited in the study. Only 87 (yoga-44, control-43) subjects completed the study. Baseline variables of the drop out subjects (n=33) did not significantly differ from those who completed the study (n=87; data not presented). In order to include all individuals enrolled in the study (both completers and dropouts) for the analysis, ITT approach was employed by LOCF for missing data. Some of the common reasons for drop out were inability to participate in yoga sessions, shift to different elderly homes and/or non-availability for follow-up.
Demographic profile of the participants
Socio-demographic profiles of yoga and waitlist group were comparable except for education [Table 1]. Yoga group were more educated compared with the waitlist controls (P=0.037).
Table 1.
Socio-demographic and clinical variables comparisons between yoga and control groups
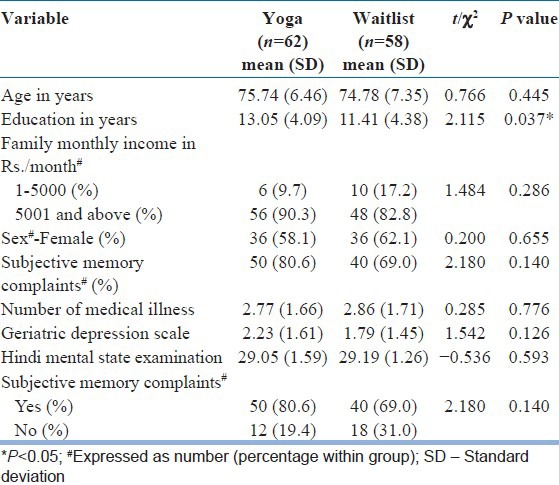
Majority of the study population (yoga - 91.9%, waitlist control - 91.4%) had one or more medical illness. Median number of medical illness in both groups was three. Hypertension was the most common medical illness in both groups (69.4% in the yoga group and 60.3% in the control group). There was no significant difference in the number of medical illness or the frequency of individual medical illness between the two groups. The scores on the screening instruments namely GDS and HMSE were not different between the groups.
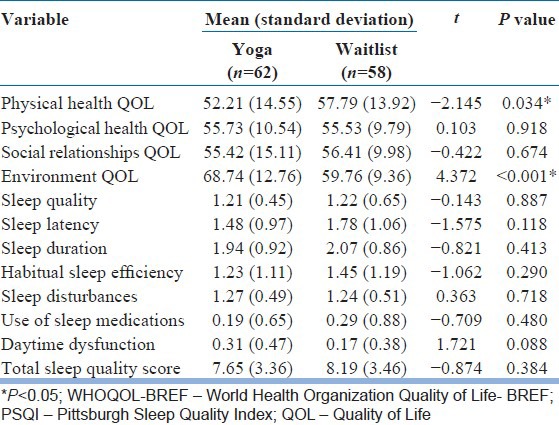
The comparison of baseline QOL scores across the subjects recruited from different old age homes showed a significant difference in all the domains of WHOQOL-BREF (data not shown). The comparison of baseline QOL scores between the yoga group and control group revealed significantly better QOL score in physical health domain for waitlist group and in environment domain for yoga group [Table 2]. There was no baseline difference between the two groups in total sleep quality as well as any of the subscales of PSQI [Table 2].
Table 2.
Baseline comparison of WHOQOL-BREF and PSQI scores
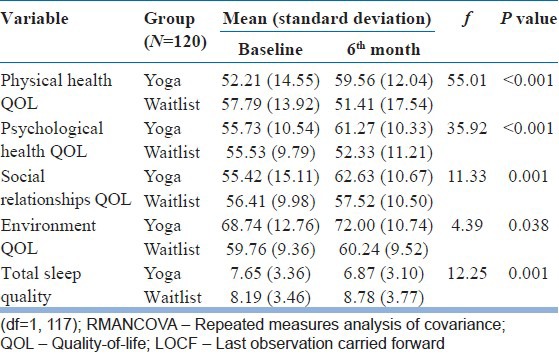
We analyzed the difference in QOL and sleep quality over time (baseline and at 6 months) across the two groups using the RMANCOVA. As there was baseline difference in education between the two groups, we used education as a covariate. There was no significant change over time for the entire sample (occasion effect) for total sleep quality (f=0.30, df=1, 117, P=0.584) measured with PSQI, physical health QOL (f=0.93, df=1, 117, P=0.338), psychological health QOL (f=0.02, df=1, 117, P=0.895) and environment QOL (f=3.12, df=1, 117, P=0.08). There was a significant change over time for the QOL domain of social relationships (f=11.00, df=1, 117, P=0.001). However, there was a significant group X occasion interaction effect, suggesting that the change in the total sleep quality and QOL scores in all the domains was significantly greater in the yoga group than in the waitlist group [Table 3]. For RMANCOVA analysis, Bonferronni correction for multiple comparisons was applied and P value for statistical significance was set as 0.01. After correction for multiple comparisons, the yoga group was significantly better in total quality of sleep and all dimensions of QOL except the environment related QOL.
Table 3.
RMANCOVA for QOL and total sleep quality (intent-to-treat analysis after imputation by LOCF method) between yoga and waitlist group
DISCUSSION
Results of the current study indicate beneficial effects of 6 month yoga-based intervention on physical health, psychological health, social relationships and environment domains of QOL in elderly living in old age homes. Furthermore, the subjects in the yoga group had significant improvement in total sleep quality score. Previously Manjunath and Telles have reported that 6 months of yogic program in elderly involving physical postures, relaxation techniques, voluntarily-regulated breathing and lectures on yoga philosophy had improved sleep latency, sleep duration and feeling of being rested in the morning.[10] In agreement with the similar earlier studies, yoga-intervention had improved the total sleep quality in elderly living in old age home.[11,12] Similar to a previous randomized controlled study, this study also demonstrates favorable effects of yoga intervention on QOL.[18] In addition to multiple health complaints, subjective memory problems and disturbed sleep were reported to predict low QOL especially health related QOL in older adults. Yogic techniques improve bodily physiological functions such as cardiovascular and respiratory efficiency;[19] so also biochemical parameters like blood sugar, lipid levels, serum triglycerides[20] and cognition[21,22,23] in the elderly. Yoga program in elderly was also reported to improve the muscle strength, active range of motion, gait and balance, mobility, physical and emotional well-being.[24,25,26] Gentle yogic postures and controlled breathing techniques reduce activity of sympathetic nervous system resulting in parasympathetic dominance and physiological reactivity to stress[27,28] among both healthy subjects and in patients suffering from various psychosomatic illnesses. Though we did not measure these in our own sample, such changes could have contributed to improvement in sleep as well as QOL. The subjects indicated the outcome on scales that did not require clinician's rating. Self-rating scales minimized the subjective bias as the same yoga therapist obtained the participant's rating on these scales. Subjects were randomized in a block fashion. Less number of blocks may be unsuitable for this procedure. That the randomization was unsatisfactory is borne out by the subject groups being incomparable on education as well as baseline QOL measures in physical health and environment domains. It would have been better if the randomization was performed with more number of blocks with a smaller number of subjects in each block. Significant baseline difference in QOL measure across all domains between the blocks of old age homes suggest that factors intrinsic to the old age home itself could have contributed to the QOL. It would be important to recruit subjects from homogenous old age homes to minimize such baseline differences in future studies. Ideally subjects in each center/home should have been randomized into two groups. This could have reduced the role of other confounds like the facilities in each home, non-specific effects of staff and peers, physical comforts in each home, etc., Logistic reasons of conducting sessions to only some (experimental group) prevented in implementing such a strategy. The dropout rate was high in the current study. Since the elderly population in this study belonged to residential care, generalization of the results may be limited. Though randomized, the patients knew what intervention they received. This could have biased the self-ratings on these instruments. Blinding in yoga research is a challenge.[29] Including an active comparative group like aerobic exercise would have controlled for the effects of socialization and/or exercise component of yoga.
CONCLUSION
This study suggests potential benefits of yoga therapy for elderly in improving the QOL and sleep quality. However, considering the limitations in the design of this study, the findings of the study needs to be considered as preliminary and there is a need for future studies overcoming the methodological limitations of this study to further establish the efficacy of yoga therapy in elderly in improvement of QOL and sleep quality.
ACKNOWLEDGMENTS
We thank Mr. Sushrutha and Mr. Bhagath of Swami Vivekananda Yoga Anusandhana Samsthana for their help with transliteration.
Footnotes
Source of Support: The research was done under the Advanced Centre for Yoga - Mental Health and Neurosciences, a collaborative centre of NIMHANS and the Morarji Desai Institute of Yoga, New Delhi
Conflict of Interest: None declared.
REFERENCES
- 1.Dhar HL. Emerging geriatric challenge. J Assoc Physicians India. 2005;53:867–72. [PubMed] [Google Scholar]
- 2.Borglin G, Jakobsson U, Edberg AK, Hallberg IR. Self-reported health complaints and their prediction of overall and health-related quality of life among elderly people. Int J Nurs Stud. 2005;42:147–58. doi: 10.1016/j.ijnurstu.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: Clinical characterization and outcome. Arch Neurol. 1999;56:303–8. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 4.Ancoli-Israel S. Sleep and aging: Prevalence of disturbed sleep and treatment considerations in older adults. J Clin Psychiatry. 2005;66(Suppl 9):24–30. [PubMed] [Google Scholar]
- 5.Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult-A mini-review. Gerontology. 2010;56:181–9. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaplan RM. The significance of quality of life in health care. Qual Life Res. 2003;12(Suppl 1):3–16. doi: 10.1023/a:1023547632545. [DOI] [PubMed] [Google Scholar]
- 7.Eiser C, Jenney M. Measuring quality of life. Arch Dis Child. 2007;92:348–50. doi: 10.1136/adc.2005.086405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gooneratne NS. Complementary and alternative medicine for sleep disturbances in older adults. Clin Geriatr Med. 2008;24:121–38. doi: 10.1016/j.cger.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoga journal releases 2008 “Yoga in America” Market study: Practitioner spending grows to nearly $6 billion a year. 2008. [Cited on 2012 Dec 25]. Available from: http://www.yogajournal.com/advertise/press_releases/10 .
- 10.Manjunath NK, Telles S. Influence of Yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–90. [PubMed] [Google Scholar]
- 11.Chen KM, Chen MH, Chao HC, Hung HM, Lin HS, Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: Cluster randomized trial. Int J Nurs Stud. 2009;46:154–63. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Chen KM, Chen MH, Lin MH, Fan JT, Lin HS, Li CH. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. 2010;18:53–61. doi: 10.1097/JNR.0b013e3181ce5189. [DOI] [PubMed] [Google Scholar]
- 13.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 14.Ganguli M, Ratcliff G, Chandra V, Sharma S, Gilby J, Pandav R. A Hindi version of the MMSE: The development of a cognitive screening instrument for a largely illiterate rural elderly population in India. Int J Geriatr Psychiatry. 1995;10:367–77. [Google Scholar]
- 15.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 16.Szabo S. The World Health Organisation quality of life (WHOQOL) assessment instrument. In: Spilker B, editor. Quality of Life and Pharmaeconomics in Clinical Trials. 2nd ed. Philadelphia, New York: Lippincott-Raven Publishers; 1996. [Google Scholar]
- 17.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–21. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 18.Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–7. [PMC free article] [PubMed] [Google Scholar]
- 19.Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, et al. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: A randomised controlled trial. BMJ Open. 2011;1:e000085. doi: 10.1136/bmjopen-2011-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park HS, Kim YJ, Kim YH. The effect of yoga program on reduced blood pressure in elderly's essential hypertension. J Korean Acad Nurs. 2002;32:633–42. [Google Scholar]
- 21.Newberg AB, Wintering N, Khalsa DS, Roggenkamp H, Waldman MR. Meditation effects on cognitive function and cerebral blood flow in subjects with memory loss: A preliminary study. J Alzheimers Dis. 2010;20:517–26. doi: 10.3233/JAD-2010-1391. [DOI] [PubMed] [Google Scholar]
- 22.Vestergaard-Poulsen P, van Beek M, Skewes J, Bjarkam CR, Stubberup M, Bertelsen J, et al. Long-term meditation is associated with increased gray matter density in the brain stem. Neuroreport. 2009;20:170–4. doi: 10.1097/WNR.0b013e328320012a. [DOI] [PubMed] [Google Scholar]
- 23.Koparde V. MD Thesis. Bangalore, India: National Institute of Mental Health and Neurosciences (NIMHANS); 2011. Short term effects of yoga therapy in elderly. [Google Scholar]
- 24.Vogler J, O’Hara L, Gregg J, Burnell F. The impact of a short-term iyengar yoga program on the health and well-being of physically inactive older adults. Int J Yoga Therap. 2011;21:61–72. [PubMed] [Google Scholar]
- 25.Sierpowska A, Ciechanowicz I, Cywinska-Wasilewska G. Functional fitness assessment among elderly women (60+) participating in yoga or swimming exercises. Stud Phys Cult Tourism. 2006;13:81–3. [Google Scholar]
- 26.Zettergren KK, Lubeski JM, Viverito JM. Effects of a yoga program on postural control, mobility, and gait speed in community-living older adults: A pilot study. J Geriatr Phys Ther. 2011;34:88–94. doi: 10.1519/JPT.0b013e31820aab53. [DOI] [PubMed] [Google Scholar]
- 27.Pratap V. Difference in magnitude of response to yogic and non yogic conditions: A synopsis of an exploratory study. Yoga Mimamsa. 1969;12:9–18. [Google Scholar]
- 28.Panjwani U, Gupta HL, Singh SH, Selvamurthy W, Rai UC. Effect of Sahaja yoga practice on stress management in patients of epilepsy. Indian J Physiol Pharmacol. 1995;39:111–6. [PubMed] [Google Scholar]
- 29.Gangadhar B, Varambally S. Yoga as therapy in psychiatric disorders: Past, present, and future. Biofeedback. 2011;39:60–3. [Google Scholar]


