Abstract
Context:
Therapeutic effects in depression of yoga adopted from different schools have been demonstrated. The efficacy of a generic module of yoga on depressed patients has not yet been tested in the literature.
Aims:
The study was aimed to compare the therapeutic effect of a generic yoga module with antidepressant drugs in non-suicidal out-patients of major depression attending a psychiatric hospital.
Settings and Design:
The study was outpatient-based using an open-labeled design.
Materials and Methods:
A total of 137 out-patients of depressive disorders received one of the three treatments as they chose – yoga-only, drugs-only or both. The yoga was taught by a trained yoga physician for over a month in spaced sessions totaling at least 12. Patients were assessed before treatment, after 1 and 3 months on depression and Clinical Global Impression Scales. Out of 137, 58 patients completed the study period with all assessments.
Results:
Patients in the three arms of treatment were comparable on demographic and clinical variables. Patients in all three arms of treatment obtained a reduction in depression scores as well as clinical severity. However, both yoga groups (with or without drugs) were significantly better than the drugs-only group. Higher proportion of patients remitted in the yoga groups compared with the drugs-only group. No untoward events were spontaneously reported in the yoga-treated patients.
Conclusion:
Within the limitations of this study, it can be concluded that the findings support a case for prescribing yoga as taught in the study in depressive non-suicidal out-patients.
Keywords: Depression, antidepressant, yoga treatment, non-suicidal
INTRODUCTION
Depression is emerging as a leading cause for global burden from diseases.[1] Prompt treatment is the key to reducing this burden. Antidepressant drugs have remained as standard and effective agents in the treatment.[2] Yet, a sizeable proportion fails to obtain remission.[3] Complementary and alternative medical (CAM) treatments are sought after on cultural/faith reasons or with a different hope. Among the diagnoses that are seen in CAM seekers, depression is most prevalent.[4] Reviews endorse a role for yoga among the CAMs as an effective treatment in depressive disorder patients.[5,6] Yoga practices that are used in treating depression have also carried a tag of influential schools such as Art-of-Living, Iyengar and Sahaja Yoga.[7,8,9,10] These could carry concerns of associated suggestion effects as well as copyright issues. Yoga is a generic discipline that is available as a recognized curriculum in standard college courses (example, a bachelor and post-graduate degree in yoga). There is hence an option to use practices elucidated in traditional texts as a generic yoga module in the treatment of selected ailments, depression being one. In this study, we report use of one such generic yoga module as treatment in depression, developed from traditional texts. We also compared this with medication treatment as usual.
MATERIALS AND METHODS
Patients
Consenting out-patients with a diagnosis of major depression[11] who were not suicidal and scored 2 or less on the suicide item of Hamilton Depression Rating Scale (HRSD),[12] were the subjects of this study. Only patients who were either treatment-naïve or were off any treatment in the last one month were included. None had received yoga as treatment before. Patients were referred by the consultants only when there was no indication for electroconvulsive therapy (catatonia, severe depression). A medical doctor (MGR) with 2 years of psychiatry training made the clinical diagnosis as well as the rating on suicide item on HRSD. Patients were offered three treatment options; drug alone, yoga with drugs or yoga alone. They were also invited to participate in a randomized study to compare addition or not of yoga to routine antidepressant drug treatment. Only 14 patients of the 137 treated during the study period consented for the randomization. The rest (n=123) chose their own option and were unwilling for the randomization. In view of the near total numbers making their treatment choices and that only 14 were treated on the randomization procedure (yoga + drug=6, drug-only=8), in the final tally these 14 were merged with the corresponding groups in the rest of the study with three treatment arms (yoga-only, drug-only and combination). The Institute's Ethics Committee had approved both the randomized and non-randomized study designs.
Treatments
Yogāsana and breathing procedures from traditional texts were identified as those potentially helpful to reduce depressive symptoms. Nine experienced yoga practitioners endorsed most of these procedures used as a module. In a pilot study, this module was found to be acceptable to depressive patients also receiving antidepressant drugs. In the small sample that was treated with this module no spontaneous adverse events were reported. The development of the generic yoga module and the order of the procedures are presented in another paper.[13] Patients were offered yoga as a sole therapy or with the drugs they received. Patients had an option to choose neither but only receive the antidepressant drugs. Only those patients who were available for all three assessments (over 3 months) were included in this analysis (see below).
Antidepressant medications were prescribed by the treating psychiatrists and these were continued at doses decided by them in the 3- month study period. As part of the standard practice, the treating psychiatrists, who were not necessarily part of the research team, gradually built the doses of each antidepressant based on clinical judgment. We noted the type of antidepressants and their dosage. In the drugs-alone group 7, 6 and 3 patients received fluoxetine (20-40 mg/day), escitalopram (10-15 mg/day) and amitriptyline (100 mg/day) respectively. In the yoga + drugs group 6, 19, 1 and 1 patient received fluoxetine (20-40 mg/day), escitalopram (10-15 mg/day), amitriptyline (100 mg/day) and mirtazapine (15 mg/day) respectively.
All patients agreeing to be treated with yoga were given training by the same therapist. The yoga therapist was formally trained with a graduate degree (5 years) in yoga (NH). They were requested to attend the therapy sessions on a daily basis for 2 weeks and again at weekly intervals for next 2 weeks. “Booster” sessions were provided once each in the 1st weeks of 2nd and 3rd months of the study. Each session of training/practice lasted one hour. On all other days patients were encouraged to practice yoga at home daily. Where available (in nearly all), a relative staying with the patient was spoken to with a purpose of confirming the patients’ accounts of yoga practice. Adherence to treatment was operationally defined as doing 50 or more yoga sessions in the 3 month period and/or using drugs for at least 2 months on the doses prescribed. Patients receiving yoga were encouraged to report any untoward event that they experienced (apart from the adverse effects of the drugs they received as informed by their treating psychiatrist).
Assessments
The severity of depression was rated on 17-item HRSD[12] by a clinician blind to the therapy (MGR). Same clinician recorded the severity and improvement on the Clinical Global Impression (CGI) Scale.[14] Assessments were conducted before starting the treatments and after 1st and 3rd months. A responder at each assessment was operationally defined as one who achieved a HRSD score of 7 or less. A remitted patient had such score both at 1 and 3 month assessments. The yoga therapist was unaware of the clinical ratings until the end of the study. The primary outcome variable was the reduction in HRSD scores. CGI ratings and numbers of patients responding/remitting formed secondary outcome variables.
Statistics
The three groups’ variables were compared using ANOVA or Chi-square tests. Changes in the symptom severity over the assessment sessions in the three groups were tested using two-way repeated measure analysis of variance (RMANOVA) with Scheffe's post-hoc test to detect intergroup differences. Statistical significance was set at P<0.05.
RESULTS
A total of 137 patients eligible for yoga were included at the outset. A minority accepted yoga as the sole treatment (n=23). A higher number (n=36) opted drugs with yoga. Majority (n=78) wished only medicines. The most common reason for opting out of yoga was the inability to attend daily sessions of therapy in the first 2 weeks of treatment. Only 58 patients were available for assessments at the time points required for this study. These 58 were not significantly different from the 79 who did not complete the study requirements as regards age, initial HRSD total scores, duration of illness and proportion of recurrent depressive disorder (RDD) patients (data not presented). However, significantly more female patients did not complete the assessments and so also those with fewer years of literacy. More patients in the drugs-only group failed to complete the study requirements.
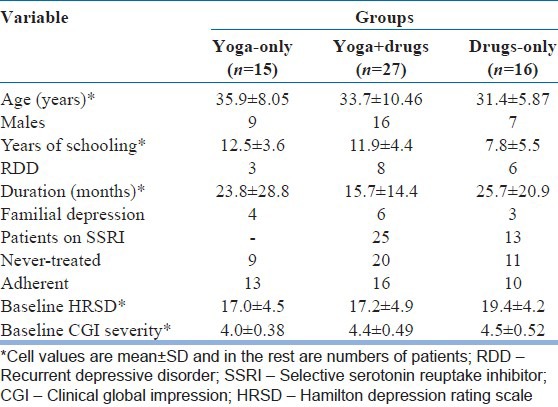
The clinical demographic details of the three groups of patients who completed the study are provided in Table 1. They were comparable on most parameters. More literates had opted for yoga. The three groups differed in baseline HRSD (P=0.023) and CGI severity (P=0.013), but without pair wise inter group differences (Scheffe's test).
Table 1.
Demographic and clinical comparison of the three treatment groups
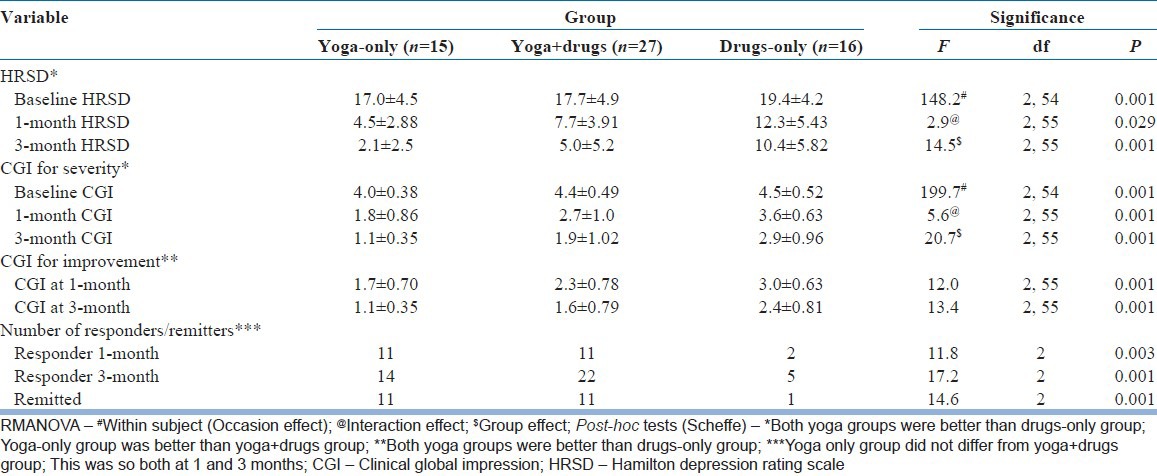
Significant reduction in HRSD scores occurred in all treatment groups. However, this difference was better in both yoga groups than drug-only group, with the yoga-only group performing best [Figure 1]. On CGI measures too, both yoga groups were better than drugs-only group. The proportions of patients responding at 1 and 3 months were higher in the yoga groups [Table 2]. No patient in the yoga groups spontaneously reported any adverse event. Analyses of the subgroup that was adherent to treatments, revealed similar significant findings with respect to reductions in HRSD and CGI, as well as proportions with responder/remission status. In the smaller subgroup of those who were not adherent, the treatment group differences on these measures were not detectable (data not presented).
Figure 1.
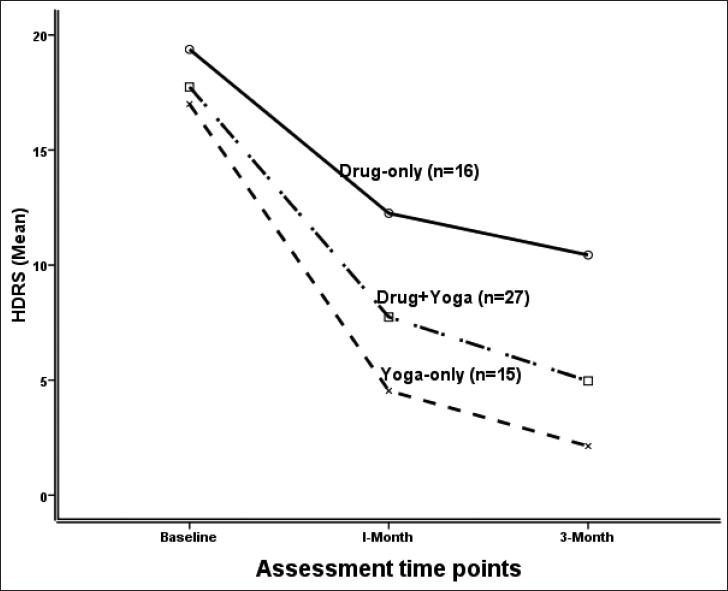
Graphical representation of the hamilton depression rating scale scores from Table 2
Table 2.
Clinical outcome in the three groups
DISCUSSION
In this study, we compared the treatment effects of yoga-only, drugs-only and a combination in outpatients of depression choosing one of these options. Patients were not “suicidal” as operationally defined (HRSD suicide item scoring two or less). The yoga groups with or without drugs obtained better antidepressant effects than drugs-only group. Randomization being unsuccessful in the majority, the treatment was by patient's choice and the groups occurred by a naturalistic design. The hospital being primarily an allopathic treatment center, it is likely that most would have come with the expectation of being treated by such approaches (mainly drugs). Yoga was offered to all (as an alternative or complementary) and a minority chose this option and even fewer opted for yoga as the sole treatment. Such choice is expected in yoga research in a center that is not a primary yoga therapy center.[15,16]
The study has all the limitations of a non-randomized study. For instance, practical considerations, rather than random allocation, determined the choice of treatment. Though the patients in the three groups were comparable with regards to age, sex, illness duration, RDD status, adherence to treatments and prior treatment-naïve status, they differed on symptom severity. At baseline, the drugs-only group of patients had the highest average HRSD score. It is known that placebo-effect is less so in severely ill depressives.[17] It is likely that the placebo-effect (that is common to all groups) was less in this group. Only the motivated may have chosen yoga. More in the yoga groups completed the study and only a minority in the drug-only group remained in all three assessments. Patients may have perceived addition of yoga or yoga itself as a special intervention adding to higher expectation/suggestion effects. This is more so a concern as yoga as treatment is unusual in this well-known allopathic hospital. By adopting a generic module of yoga sans the names of influential/popular yoga groups/centers, the expectation/suggestion effect from yoga therapy was minimized. A placebo yoga group as a comparator is ideal, but is difficult to implement.[16] Absence of a no-treatment group too is a serious limitation that precludes inference regarding the efficacy of yoga therapy. Potential biological markers of either depression or treatment effects may have helped in finding an answer to this argument of the placebo effect. For example in an earlier study, P300 changes with a yoga-only treatment occurred after successful antidepressant effects.[18]
Antidepressant drug class as well as its dose was neither standardized nor uniform. It is likely that higher doses of the drug are required for some patients. The proportion of patients obtaining response/remission with drug-only is lower than reported in the literature.[19] This vindicates the suboptimal drug therapy. It is highly likely that in this design the drug-only group was at a serious disadvantage. The yoga groups were to keep therapy appointments at scheduled (though spaced) intervals throughout the 3 months. Higher number of patients irrespective of the clinical need (having been improved) therefore met appointments. In the drug-only group, patients had to come for assessments while they were receiving drugs. It is likely that only those who were symptomatic enough to seek help came for follow-ups. The highest number of patients left the study in this group. The education status was lower in drug groups as compared with the yoga-only group. This may also have contributed to lower follow-ups in these groups.
The doses of antidepressants used were close to the recommended ones and the majority may have indeed responded. This left out the responded/remitted patients in the drug-only group. Therefore, the comparative finding should be viewed with caution. However, the response rates in yoga-only group compares with similar figures in other studies.[10,20] Some side-effects of the drugs may also have contributed for higher depression ratings; although, no serious adverse side-effects were spontaneously reported nor observed by the treating psychiatrists. Though no spontaneous report of side-effects occurred, it may be premature as well as unsafe to conclude that yoga group experienced none of these. More systematic probing may bring out if yoga did or did not produce adverse effects. No information of the choice of treatment after the study period and/or long-term outcome was recorded that may have thrown more light on the viability of yoga as a treatment option in outpatient depressives.
Knowledge about the reason for dropout would have yielded further useful information with regard to the efficacy and side-effects of the three treatments. However, as patients who dropped out could not be contacted, this information is unavailable – this forms another limitation in the interpretation of these results.
In summary, out-patients with non-suicidal depression choosing yoga obtained significant therapeutic effects and perhaps better than conventional drugs over 3 months of treatment. A generic module of yoga has potential for routine prescription in out-patients of depression who are not suicidal. However, this being a non-randomized study precludes a firm conclusion.
ACKNOWLEDGMENT
We would like to thank Dr. R. Nagaratna, Dean, Life Sciences, SVYASA, Bangalore for her support, encouragement and guidance.
We thank Mr. Sushrutha and Mr. Bhagath of Swami Vivekananda Yoga Anusandhana Samsthana for their help with transliteration
Footnotes
Source of Support: The research was done under the Advanced Centre for Yoga - Mental Health and Neurosciences, a collaborative centre of NIMHANS and the Morarji Desai Institute of Yoga, New Delhi
Conflict of Interest: None declared.
REFERENCES
- 1.Deswal BS, Pawar A. An epidemiological study of mental disorders at Pune, Maharashtra. Indian J Community Med. 2012;37:116–21. doi: 10.4103/0970-0218.96097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA. A systematic review of comparative efficacy of treatments and controls for depression. PLoS One. 2012;7:e41778. doi: 10.1371/journal.pone.0041778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kupfer DJ, Frank E, Phillips ML. Major depressive disorder: New clinical, neurobiological, and treatment perspectives. Lancet. 2012;379:1045–55. doi: 10.1016/S0140-6736(11)60602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barner JC, Bohman TM, Brown CM, Richards KM. Use of complementary and alternative medicine for treatment among African-Americans: A multivariate analysis. Res Social Adm Pharm. 2010;6:196–208. doi: 10.1016/j.sapharm.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: The research evidence. J Affect Disord. 2005;89:13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 6.da Silva TL, Ravindran LN, Ravindran AV. Yoga in the treatment of mood and anxiety disorders: A review. Asian J Psychiatr. 2009;2:6–16. doi: 10.1016/j.ajp.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M. Yoga as a complementary treatment of depression: Effects of traits and moods on treatment outcome. Evid Based Complement Alternat Med. 2007;4:493–502. doi: 10.1093/ecam/nel114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michalsen A, Jeitler M, Brunnhuber S, Lüdtke R, Büssing A, Musial F, et al. Iyengar yoga for distressed women: A 3-armed randomized controlled trial. Evid Based Complement Alternat Med 2012. 2012 doi: 10.1155/2012/408727. 408727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manocha R, Black D, Sarris J, Stough C. A randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers. Evid Based Complement Alternat Med 2011. 2011 doi: 10.1155/2011/960583. 960583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Text Revision. 4th ed. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 12.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naveen GH, Rao MG, Vishal V, Thirthalli J, Varambally S, Gangadhar BN. Development and feasibility of yoga therapy module for out-patients with depression in India. Indian J Psychiatry. 2013;55:S350–6. doi: 10.4103/0019-5545.116305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guy W. Rockville (MD): National Institute of Mental Health; 1976. ECDEU Assessment Manual for Psychopharmacology; pp. 218–22. [Google Scholar]
- 15.Baspure S, Jagannathan A, Kumar S, Varambally S, Thirthalli J, Venkatasubramanain G, et al. Barriers to yoga therapy as an add-on treatment for schizophrenia in India. Int J Yoga. 2012;5:70–3. doi: 10.4103/0973-6131.91718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gangadhar B, Varambally S. Yoga as therapy in psychiatric disorders: Past, present, and future. Biofeedback. 2011;39:60–3. [Google Scholar]
- 17.Nelson JC, Mazure CM, Jatlow PI. Does melancholia predict response in major depression? J Affect Disord. 1990;18:157–65. doi: 10.1016/0165-0327(90)90032-4. [DOI] [PubMed] [Google Scholar]
- 18.Murthy PJ, Gangadhar BN, Janakiramaiah N, Subbakrishna DK. Normalization of P300 amplitude following treatment in dysthymia. Biol Psychiatry. 1997;42:740–3. doi: 10.1016/s0006-3223(97)00296-5. [DOI] [PubMed] [Google Scholar]
- 19.Rush AJ, Fava M, Wisniewski SR, Lavori PW, Trivedi MH, Sackeim HA, et al. Sequenced treatment alternatives to relieve depression (STAR*D): Rationale and design. Control Clin Trials. 2004;25:119–42. doi: 10.1016/s0197-2456(03)00112-0. [DOI] [PubMed] [Google Scholar]
- 20.Rohini V, Pandey RS, Janakiramaiah N, Gangadhar BN, Vedamurthachar A. A comparative study of full and partial Sudarshan Kriya Yoga (SKY) in major depressive disorder. NIMHANS J. 2000;18:53–7. [Google Scholar]


