Abstract
Context:
Attention deficit-hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders. Stimulant medication is frequently used in management, with significant adverse effects. There is a growing interest in complementary treatments like yoga.
Aims:
To study the effects of yoga as a complementary therapy in children with moderate to severe ADHD.
Settings and Design:
The study was performed on children (consent was taken from parents) admitted in a child psychiatry unit using an open-label exploratory study.
Materials and Methods:
Children between 5 and 16 years of age diagnosed with ADHD and co-operative for yoga were included. Subjects with other serious psychiatric and medical illnesses were excluded. The participants were given yoga training daily during their in-patient stay. They were rated on Conners’ abbreviated rating scale – (CARS), ADHD-rating scale–IV (ADHD - RS IV) and clinical global impression (CGI)-Severity, at the beginning of study, at discharge and subsequently at the end of 1st, 2nd and 3rd month by a research associate not involved in yoga instruction. Paired t-test was employed to compare the means of scores between baseline and follow-ups.
Results:
A total of 9 children (8 males, 1 female) were recruited into the study. All, but one were on medications. An average of 8 yoga training sessions was given to subjects. They were able to learn yoga reasonably well. There was a significant improvement in the ADHD symptoms as assessed on CARS (P-0.014), ADHD-RS IV (P=0.021) and CGI- S scales (P=0.004) at the time of discharge.
Keywords: Attention deficit-hyperactivity disorder, children, inpatients, yoga
INTRODUCTION
Attention deficit-hyperactivity disorder (ADHD) is the most common neurobehavioral developmental disorder among school-age children, affecting about 8-12% of children world-wide.[1] An epidemiological study by Srinath et al. showed the prevalence of ADHD to be 1.6% in children less than 16 years, posing costly demands on medical, psychological and societal resources in India.[2] The child with ADHD will have difficulty in concentrating on a task, at home and school. This, predictably, leads to considerable distress among the care givers.[3]
Stimulant medication is one of the widely used treatments in the management of ADHD.[4] The frequently reported adverse effects are decreased appetite, headaches, abdominal discomfort, problems falling asleep and irritability, to name a few.[5,6] Daly et al. have questioned the evidence for long-term use of stimulant medications to improve the learning disabilities and peer relationships in children with ADHD.[7] Though 70-80% of children respond positively to a stimulant regimen, poor compliance to treatment, particularly while in school,[8] often leads parents to seek alternate approaches like behavioral interventions in the form of parent training, classroom, academic and peer-related interventions. Large randomized trials, which compared behavioral interventions with pharmacological therapy, showed that any one of the former is less effective than pharmacological therapy.[4,8,9] Multimodal intervention, which is viewed as the gold standard among ADHD treatment also falls short in terms of cost-effectiveness.[10] In recent years, several complementary and alternative medicine techniques have been used in the management of ADHD with encouraging results.[11]
Yoga is one such complementary intervention. Yoga as therapy uses physical postures (āsanas), breathing exercises (Prāṇāyāma) and meditation techniques. Independently and/or comprehensively, these have been shown to improve several physiological functions and improve cognitive domains such as executive functions, attention, intelligence, memory and concentration.[12,13,14,15,16,17,18,19,20,21,22,23] Evidence suggests that yoga-based interventions are effective in the management of anxiety,[24,25] neuroticism,[26] obsessive compulsive disorder[27] and depression.[28,29] These conditions are common co-morbid disorders found in children with ADHD.[30]
Previous studies have shown improvement in attention and other core symptoms of ADHD with once/twice weekly yoga sessions in school-going children stabilized with medication. In addition to improving ADHD symptoms, a family treatment approach for children with ADHD in the form of Sahaj yoga meditation made parents feel happier, less stressed and better able to manage their child's behavior, thereby improving the quality of child-parent relationship.[31,32,33,34]
The major query that any psychiatrist would face when recommending yoga for a child with ADHD is whether the child can cooperate, concentrate, learn and practice yoga; in other words, the feasibility of yoga. Most of the earlier studies primarily focused on school going children who are mildly or moderately ill. The effect of yoga in children with severe ADHD needing inpatient care has not been investigated as yet.
The aim of this study was to test the feasibility and effects of yoga as an add-on intervention in children with ADHD admitted as in-patients at a tertiary psychiatric hospital. We hypothesized that yoga therapy would reduce the severity of symptoms in children practicing it.
MATERIALS AND METHODS
This was an open-label exploratory study approved by the institutional ethical committee. Children were recruited from the in-patient services of child and adolescent psychiatry unit. All children were reviewed by a qualified child psychiatrist to confirm the diagnosis of ADHD according to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition criteria.[35] The diagnosis was made after a detailed interview with parent and the child as well as teachers’ inputs, wherever available. Children aged between 5 and 16 years willing to participate in yoga were included in the study after obtaining a written consent from the caregiver and the child's assent whenever possible.
Children with co-morbid substance abuse or dependence, psychosis, suicidal and self-injurious behavior, moderate mental retardation, severe physical ailments such as congenital heart disease, fracture or an episode of seizure in the past 1 month were excluded from the study. Since the study needed the caregivers also to learn yoga, children with caregivers having severe heart disease such as coronary artery disease or history of myocardial infarction, cerebrovascular accident, fracture and other conditions limiting the practice of yoga were also excluded from the study.
The subjects were rated by the research associate who was not involved in yoga instruction, on ADHD rating scale-IV (ADHD-RS),[36] Conners’ abbreviated rating scale (CARS)[37] and clinical global impression (CGI) Severity[38] at the beginning of study, at the time of discharge and subsequently at the end of the 1st, 2nd and 3rd month of follow-up. The subjects’ ability to perform yoga was rated on a yoga performance questionnaire [Appendix 1] by the instructor who taught the yoga.
Appendix 1.
Details of Yoga Intervention
Yoga performance questionnaire
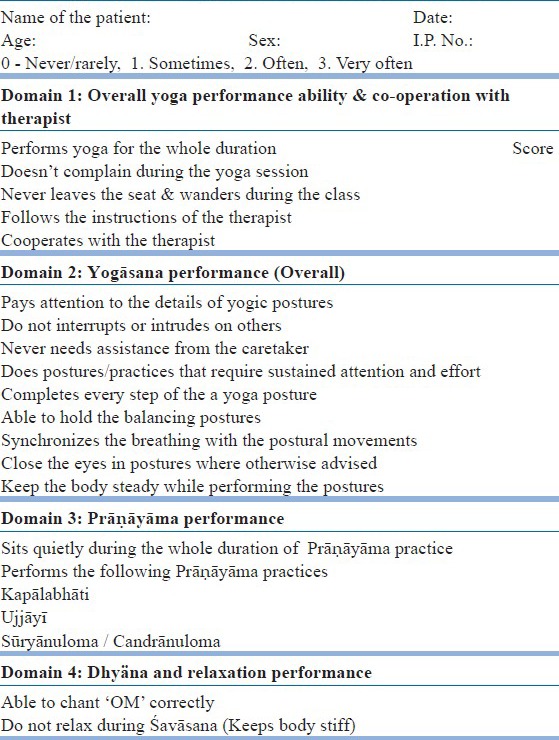
This is a 20-item, yoga instructor rated scale exclusively designed for the current study. This scale rates the performance of subject's practice during the supervised yoga sessions. The scale in divided into four domains namely:
Overall yoga performance ability and co-operation with the therapist
Yogāsana, performance (overall)
Prāṇāyāma performance
Relaxation and Nādānusandhāna performance.
The scores for each domain were added and the total scores at pre- and post-assessments were compared.
Yoga intervention
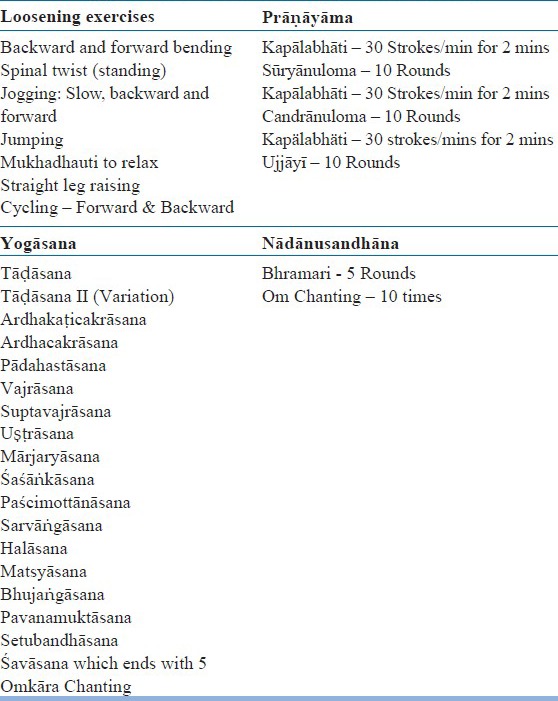
The yoga program was developed from the publication “yoga in education.”[39] Yogic practices that are challenging promote relaxation, concentration and balance, improve attention, breath and body awareness were selected. The yoga program consisted of Sukṣmavyayāma (loosening exercises), Yogāsana (physical postures), Prāṇāyāma (breathing exercises) and meditation in the form of Nādānusandhāna (OM chanting) [Appendix 2].
Appendix 2.
Yoga Performance Questionnaire
The subjects, along with their caregiver, received training in the above yoga module daily (barring holidays) during the period of admission in the child and adolescent psychiatry ward from a certified yoga instructor who had more than 2 years of experience in teaching yoga. An attempt was made to give individual attention to each dyad. Since the caregiver would have to supervise the child at home, it was hoped that the parent/caregiver would volunteer to learn yoga. Such of the caregivers who did not learn yoga were trained in supervising their child's yoga practice at home. Caregivers were asked to maintain a log of attendance and the number of days of yoga sessions subjects practiced post-discharge. The yoga instructor rated the subjects’ performance of the different yoga components on the yoga performance questionnaire [Appendix 1] at the end of 1 week of the program and at the time of discharge. Each training session lasted 1 h and each subject received at least six sessions of training.
RESULTS
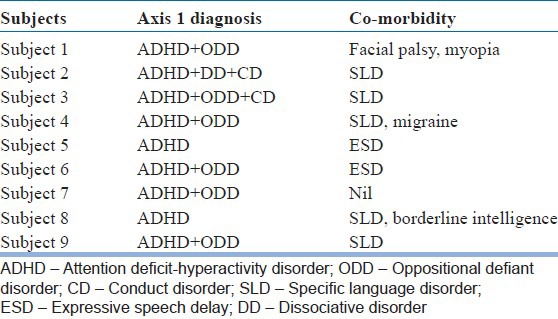
A total of 20 children were screened, of which 11 were excluded from the study due to age less than 6 years, co-morbid severe mental retardation, autism spectrum disorders, cardio vascular abnormality and epilepsy. A total of 9 children (8 males, 1 female) who met the inclusion criteria were recruited into the study. They were between 6 and 13 years of age (mean 8.6 years, standard deviation (SD) ±2.4 years) and had a mean of 3.7 years (SD 2.4) of schooling. Five children were on Methylphenidate, two on Clonidine, three on Atomoxetine and two were on multiple medications while only one subject was drug naïve. They were on regular medications and received other interventions routinely administered in the ward. The diagnostic features of the nine children are mentioned in Table 1.
Table 1.
Subjects axis 1 diagnosis and co-morbidity
All the subjects practiced yoga at least for 8 days during their stay at the hospital. All the subjects practiced yoga at least thrice a week out of which five of them had continued practicing yoga daily at home during the 1st month under the supervision of the mother. Only three of them practiced yoga at the end of second follow-up. None had practiced yoga at the end of 3rd month. In the 2nd and 3rd month, the frequency had come down to almost nil.
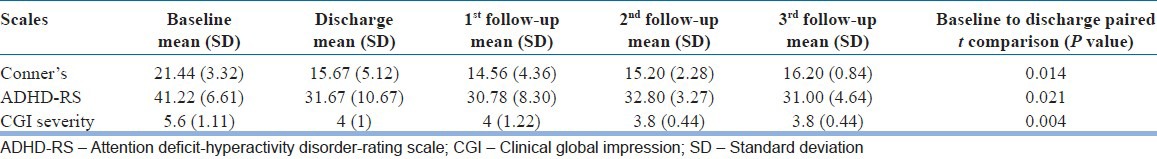
The scores obtained on CARS, ADHD-RS and CGI are depicted in Table 2. There is a reduction in scores from baseline to discharge in all the scales. Further reduction in scores occurred in follow-ups, predominantly in the 1st month. In 2nd and 3rd month there was a slight increase in scores. Paired t-test was employed to compare the means of scores between baseline and discharge; discharge and1st follow-up; 1st follow-up and 2nd follow-up and; 2nd follow-up and 3rd follow-up. The reduction was statistically significant for scores between baseline and discharge (P=0.014 on CARS and P=0.021 on ADHD-RS and 0.004 on CGI). There was no significant reduction in the scores later on.
Table 2.
Scores on CGI, ADHD-RS and Conner's scales from baseline to 1st, 2nd and 3rd follow-up and P value of comparison between baseline scores and scores at discharge
Since the follow-up assessments were carried out through telephonic interview for some of the subjects, yoga performance assessments carried out only at the time of discharge is elaborated in the following results.
The participants’ ability to practice yoga according to the domains at the time of discharge is depicted in Figure 1. There is a significant improvement in the participants’ performance in all four domains from baseline to discharge. Subjects’ duration of yoga practice and co-operation with the yoga instructor improved. Subjects started paying attention to the details of the yogic practices; some even attempted completing each step of the individual yogic practices. They needed lesser support from their caregivers in the yoga session. However, most of the subjects were unable to perform advanced yogic practices such as Matsyāsana, (n=9), Uṣṭāsana, (n=8), Halāsana, (n=7), Sarvāṅgāsana (n=4) and there were difficulties in performing the Prāṇāyāma and relaxation practices.
Figure 1.
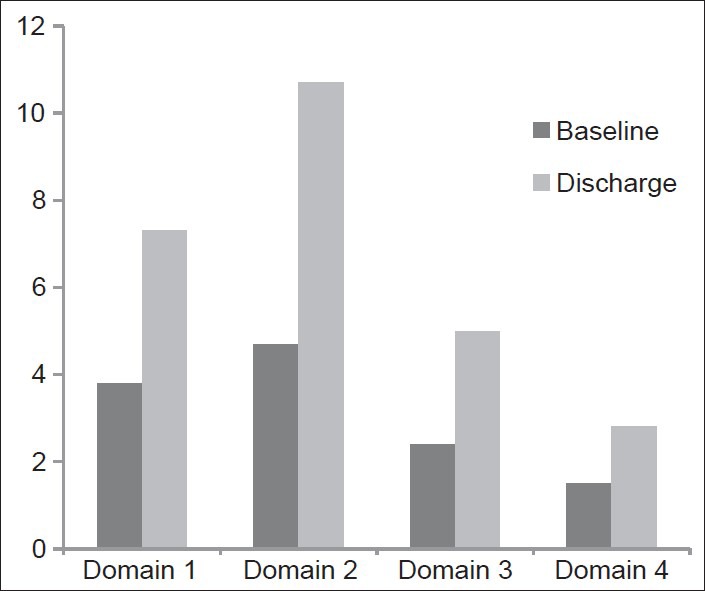
The improvement in scores on four domains (Domain 1: Overall yoga performance ability and co-operation with the therapist, Domain 2: Yoga äsana performance (overall), Domain 3: Präëäyäma performance, Domain 4: Relaxation and Nädänusandhäna performance)
The caregivers cited “disinterest for yoga practice,” “inability to make children practice yoga,” “homework,” “attends yoga class once/twice weekly at school” and “family problems” as the main reasons for non-adherence among children to yoga practice at home post-discharge.
DISCUSSION
This was an open-label exploratory study investigating the feasibility and effectiveness of yoga as an add-on therapy in subjects diagnosed with ADHD receiving in-patient care. All the subjects were receiving pharmacological treatment and/or behavioral interventions as a part of their in-patient care. Yoga was included as a complementary therapy to the subjects consenting to participate in the present study. Having excluded co-morbid conduct disorder (CD), oppositional defiant disorder (ODD) and Learning disorders, most of the subjects in previous studies were mainly school going out-patients well-maintained on medication. Little information about their yoga performance is available in most of these studies except for the duration of the yoga intervention.[31,32,33,34] Mehta et al. in a pilot study, showed that yoga could be taught successfully in high school volunteers with ADHD irrespective of their age and type of ADHD.[40] In the current study, the severity of the illness ranged from moderate to severe with several co-morbidities such as CD, SLD and borderline intelligence.
The main findings are reductions in the ADHD scores as measured by ADHD-RS IV and CPRS in the group of children at discharge. In the follow-up months, they practiced yoga irregularly and scores on these scales had worsened. Jensen et al. report similar findings.[32] The important finding of this study is that the yoga module can be taught to symptomatic inpatients with ADHD and these children were able to learn the yoga procedures. This is demonstrated by the assessment of yoga performance showing that there were improvements on all four domains of the yoga performance during the hospital stay. The finding also indicates that as they reduced/stopped the yoga practice, the symptoms worsened. This may suggest a therapeutic benefit from yoga. It is important to note that in the hospital, the children received yoga training on an individual basis from the yoga teacher along with their parents, which was not available at home. An earlier study[32] that was a randomized controlled trial (RCT) reported significant benefits from add-on yoga in ADHD that was not seen in those who did not receive yoga. Furthermore, benefits of yoga were associated with more home practice. There is a suggestion from this study that home yoga practice is also feasible and may benefit ADHD. The current study also reports the barriers for caregivers to teach yoga at home such as “disinterest for yoga practice” and “inability to make children practice yoga.” Some of these may be attributed to the co-morbid ODD since it is seen as an important moderator for treatment adherence in children with ADHD. Furthermore, inability to devote time and interpersonal problems among caregivers may explain reporting of reasons such as “family problems.”
This study carries all the other limitations of a single arm design. For example, Jensen and Kenny found that a control (no intervention) arm too obtained some improvements in children with ADHD.[32] It could be that pre-post differences found in our study were incidental. An argument against this, though weak, is that upon reducing/stopping yoga, the scores on symptoms rose in the follow-up. As in any yoga study, patient blinding was not possible. Faith in an Indian system of intervention could have contributed to improvement: Although, it is difficult to accept that a condition like ADHD would have faith-related response. We did not control all non-drug interventions that may have contributed during their in-patient stay; although, these would have been uniform to all. These and medication continuation may have had an effect in lowering the ADHD symptom scores. An early relapse may have discouraged the patients from continuing yoga. Clearly, we need to have a comparison group. However, relapse or increase in symptom score occurred when yoga was stopped, despite remaining on medications.
Furthermore, a small sample size of nine precludes the generalizability of these encouraging findings. Another issue to be considered is that whether the children were on medications prior to admission. Only one of the children was drug naïve and the rest were on medication at the time of before and during the yoga training and assessment. Hence, the effects of yoga appear to have been independent of the starting of medications in the ward. A limitation in the study is that the children's behavior in school was not taken into consideration; however, the rating scales that were used confirmed the diagnosis of ADHD.
Within these limitations, we may conclude that in-patients with ADHD can be taught a package of yoga along with other medical treatments. There were no adverse events reported that could implicate yoga. The children learnt the procedures well and also obtained improvements at the time of discharge. Failing to be regular with yoga at follow-up was also associated with symptom relapse. The findings encourage RCT of yoga intervention in in-patients with ADHD.
ACKNOWLEDGMENTS
We acknowledge Prof. Satish Girimaji and Prof. Shekar Seshadri of the Department of Child and Adolescent Psychiatry for their guidance. We also acknowledge Dr. Vishal V, Program Coordinator, Advanced Centre for Yoga, National Institute of Mental Health and Neurosciences for help in editing the manuscript.
We thank Mr. Sushrutha and Mr. Bhagath of Swami Vivekananda Yoga Anusandhana Samsthana for their help with transliteration.
Footnotes
Source of Support: The research was done under the Advanced Centre for Yoga - Mental Health and Neurosciences, a collaborative centre of NIMHANS and the Morarji Desai Institute of Yoga, New Delhi
Conflict of Interest: None declared.
REFERENCES
- 1.Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: Is it an American condition? World Psychiatry. 2003;2:104–13. [PMC free article] [PubMed] [Google Scholar]
- 2.Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P, et al. Epidemiological study of child and adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res. 2005;122:67–79. [PubMed] [Google Scholar]
- 3.Musa RS, Shafiee Z. Depressive, anxiety and stress levels among mothers of ADHD children and their relationships to ADHD symptoms. ASEAN J Psychiatr. 2007;8:20–8. [Google Scholar]
- 4.Rappley MD. Clinical practice. Attention deficit-hyperactivity disorder. N Engl J Med. 2005;352:165–73. doi: 10.1056/NEJMcp032387. [DOI] [PubMed] [Google Scholar]
- 5.Greydanus DE. Pharmacologic treatment of attention-deficit hyperactivity disorder. Indian J Pediatr. 2005;72:953–60. doi: 10.1007/BF02731672. [DOI] [PubMed] [Google Scholar]
- 6.Elia J, Ambrosini PJ, Rapoport JL. Treatment of attention-deficit-hyperactivity disorder. N Engl J Med. 1999;340:780–8. doi: 10.1056/NEJM199903113401007. [DOI] [PubMed] [Google Scholar]
- 7.Daly BP, Creed T, Xanthopoulos M, Brown RT. Psychosocial treatments for children with attention deficit/hyperactivity disorder. Neuropsychol Rev. 2007;17:73–89. doi: 10.1007/s11065-006-9018-2. [DOI] [PubMed] [Google Scholar]
- 8.Pelham WE, Jr, Carlson C, Sams SE, Vallano G, Dixon MJ, Hoza B. Separate and combined effects of methylphenidate and behavior modification on boys with attention deficit-hyperactivity disorder in the classroom. J Consult Clin Psychol. 1993;61:506–15. doi: 10.1037/0022-006X.61.3.506. [DOI] [PubMed] [Google Scholar]
- 9.The MTA Cooperative Group. Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: The multimodal treatment study of children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56:1088–96. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- 10.Jensen PS, Garcia JA, Glied S, Crowe M, Foster M, Schlander M, et al. Cost-effectiveness of ADHD treatments: Findings from the multimodal treatment study of children with ADHD. Am J Psychiatry. 2005;162:1628–36. doi: 10.1176/appi.ajp.162.9.1628. [DOI] [PubMed] [Google Scholar]
- 11.Sadiq AJ. Attention-deficit/hyperactivity disorder and integrative approaches. Pediatr Ann. 2007;36:508–15. doi: 10.3928/0090-4481-20070801-13. [DOI] [PubMed] [Google Scholar]
- 12.Selvamurthy WN, Nayar HS, Joseph NT, Joseph S. Physiological effects of yogic practices. NIMHANS J. 1983;1:71–80. [Google Scholar]
- 13.Udupa K, Madanmohan, Bhavanani AB, Vijayalakshmi P, Krishnamurthy N. Effect of pranayam training on cardiac function in normal young volunteers. Indian J Physiol Pharmacol. 2003;47:27–33. [PubMed] [Google Scholar]
- 14.Nayar HS, Mathur RM, Kumar RS. Effects of yogic exercises on human physical efficiency. Indian J Med Res. 1975;63:1369–76. [PubMed] [Google Scholar]
- 15.Mandanmohan, Jatiya L, Udupa K, Bhavanani AB. Effect of yoga training on handgrip, respiratory pressures and pulmonary function. Indian J Physiol Pharmacol. 2003;47:387–92. [PubMed] [Google Scholar]
- 16.Yadav RK, Das S. Effect of yogic practice on pulmonary functions in young females. Indian J Physiol Pharmacol. 2001;45:493–6. [PubMed] [Google Scholar]
- 17.Sahay BK, Sadasivudu B, Yogi R, Bhaskaracharyulu C, Raju PS, Madhavi S, et al. Biochemical parameters in normal volunteers before and after yogic practices. Indian J Med Res. 1982;76(Suppl):144–8. [PubMed] [Google Scholar]
- 18.Manjunath NK, Telles S. Improved performance in the Tower of London test following yoga. Indian J Physiol Pharmacol. 2001;45:351–4. [PubMed] [Google Scholar]
- 19.Rani JR, Rao KPV. Meditation and attention regulation. J Indian Psychol. 1996;14:26–30. [Google Scholar]
- 20.Sridevi K, Sitamma M. Yoga training and cognitive task performance. J Indian Psychol. 1998;16:34–9. [Google Scholar]
- 21.Sharma VK, Das S, Mondal S, Goswami U, Gandhi A. Effect of Sahaj Yoga on neuro-cognitive functions in patients suffering from major depression. Indian J Physiol Pharmacol. 2006;50:375–83. [PubMed] [Google Scholar]
- 22.Verma IC, Jayashanka rappa BS, Palani M. Effect of transcendental meditation on the performance of some cognitive psychological tests. Indian J Med Res. 1982;76(Suppl):136–43. [PubMed] [Google Scholar]
- 23.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 24.Sahasi G, Mohan D, Kacker C. Effectiveness of yogic techniques in the management of anxiety. J Pers Clin Stud. 1989;5:51–55. [Google Scholar]
- 25.Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50:41–7. [PubMed] [Google Scholar]
- 26.Naug R. Yoga therapy in neurotic disorders. Indian J Clin Psychol. 1975;2:87–90. [Google Scholar]
- 27.Shannahoff-Khalsa DS, Beckett LR. Clinical case report: Efficacy of yogic techniques in the treatment of obsessive compulsive disorders. Int J Neurosci. 1996;85:1–17. doi: 10.3109/00207459608986347. [DOI] [PubMed] [Google Scholar]
- 28.Sharma VK, Das S, Mondal S, Goswampi U, Gandhi A. Effect of Sahaj Yoga on depressive disorders. Indian J Physiol Pharmacol. 2005;49:462–8. [PubMed] [Google Scholar]
- 29.Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M. Yoga as a complementary treatment of depression: Effects of traits and moods on treatment outcome. Evid Based Complement Alternat Med. 2007;4:493–502. doi: 10.1093/ecam/nel114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drabick DA, Gadow KD, Sprafkin J. Co-occurrence of conduct disorder and depression in a clinic-based sample of boys with ADHD. J Child Psychol Psychiatry. 2006;47:766–74. doi: 10.1111/j.1469-7610.2006.01625.x. [DOI] [PubMed] [Google Scholar]
- 31.Haffner J, Roos J, Goldstein N, Parzer P, Resch F. The effectiveness of body-oriented methods of therapy in the treatment of attention-deficit hyperactivity disorder (ADHD): Results of a controlled pilot study. Z Kinder Jugendpsychiatr Psychother. 2006;34:37–4. doi: 10.1024/1422-4917.34.1.37. [DOI] [PubMed] [Google Scholar]
- 32.Jensen PS, Kenny DT. The effects of yoga on the attention and behavior of boys with attention-deficit/hyperactivity disorder (ADHD) J Atten Disord. 2004;7:205–16. doi: 10.1177/108705470400700403. [DOI] [PubMed] [Google Scholar]
- 33.Grosswald SJ, Stixrud WR, Travis F, Bateh MA. Use of the transcendental meditation technique to reduce symptoms of attention deficit hyperactivity disorder (ADHD) by reducing stress and anxiety: An exploratory study. Curr Issues Educ. 2008;10:1–16. [Google Scholar]
- 34.Harrison LJ, Manocha R, Rubia K. Sahaja yoga meditation as a family treatment programme for children with attention deficit-hyperactivity disorder. Clin Child Psychol Psychiatry. 2004;9:479–97. [Google Scholar]
- 35.American Psychiatric Association. Text Revision. 4th ed. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 36.DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. New York: Guilford Press; 1998. ADHD Rating Scale—IV: Checklists, Norms, and Clinical Interpretation. [Google Scholar]
- 37.Conners CK. Rating scales for use in drug studies with children. Psychopharmacology Bulletin (Special Issue: Pharmacotherapy of children) 1973:24–84. [Google Scholar]
- 38.Guy W. Rockville (MD): National Institute of Mental Health; 1976. ECDEU Assessment Manual for Psychopharmacology; pp. 218–22. [Google Scholar]
- 39.Nagendra H, Mohan T, Shriram A, editors. Bangalore, India: Vivekananda Kendra Yoga Anusandhana Samsthana; 2010. Yoga in Education. [Google Scholar]
- 40.Mehta S, Mehta V, Shah D, Motiwala A, Vardhan J, Mehta N, et al. Multimodal behavior program for ADHD incorporating yoga and implemented by high school volunteers: A pilot study. ISRN Pediatr 2011. 2011 doi: 10.5402/2011/780745. 780745. [DOI] [PMC free article] [PubMed] [Google Scholar]


