Abstract
Context:
Hypercortisolemia is well-known in depression and yoga has been demonstrated earlier to reduce the parameters of stress, including cortisol levels.
Aim:
We aimed to find the role of yoga as an antidepressant as well as its action on lowering the serum cortisol levels.
Settings and Design:
An open-labeled study consisting of three groups (yoga alone, yoga along with antidepressant medication and antidepressant medication alone) was conducted at a tertiary care psychiatry hospital.
Methodology:
Out-patient depressives who were not suicidal were offered yoga as a possible antidepressant therapy. A validated yoga module was used as therapy taught over a month and to be practiced at home daily. Patients were free to choose the drugs if their psychiatrist advised. Patients (n=54) were rated on Hamilton Depression Rating Scale (HDRS) with serum cortisol measurements at baseline and after 3 months. In 54 patients, assessments and blood test results were both available. 19 each received yoga alone or with drugs and 16 received drugs only. Healthy comparison subjects (n=18) too underwent morning cortisol measurements once.
Results:
Serum cortisol was higher in depressives compared with controls. In the total sample, the cortisol level dropped significantly at the end of treatment. More patients in the yoga groups had a drop in cortisol levels as compared to drug-only group. In the yoga-only group, the cortisol drop correlated with the drop in HDRS score (antidepressant effect).
Conclusion:
The findings support that yoga may act at the level of the hypothalamus by its ‘anti-stress’ effects (reducing the cortisol), to bring about relief in depression.
Keywords: Cortisol, depression, hypercortisolemia, stress, yoga
INTRODUCTION
Depression is well-recognized to be associated with hypercortisolemia as a result of hyperfunctioning of hypothalamo-pituitary-adrenal axis.[1,2] Increased cortisol is also a well-known response to stress, acute or chronic.[3,4] Stress caused mainly by negative/exit life events are known to precipitate depression.[4] Yoga has been used as an effective intervention in stress as well as depressive illness.[5] Yoga is also associated with lowering of cortisol.[6] In this study, we investigated yoga in relation to antidepressant effects and serum cortisol.
METHODOLOGY
Subjects
The data for this research comes from a study comparing the clinical and laboratory outcome of patients with depression who were treated with yoga therapy alone, antidepressant medications alone or a combination of both (Naveen et al., this issue). Consenting out-patients from a research and clinical care hospital with a diagnosis of major depression according to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition[7] criteria were invited to participate in the study. The diagnosis was confirmed by the Mini-International Neuropsychiatric Interview.[8] In 58 patients serum sample for cortisol level estimation could be obtained before the initiation of treatment (at 8 am); the same could be obtained in 54 patients who came for follow-up at 3 months (at 8 am). Healthy volunteers from the hospital staff were contacted to participate as controls and serum sample was collected in 18 of them. All subjects provided written informed consent and the Institute Ethics Committee accorded permission to conduct this study.
Treatment
Out of the 58 patients, 38 were never treated and 20 were medication-free for at least a month. Patients got to choose one of the three treatments, antidepressant medication alone (n=16), yoga-alone (n=19) or a combination of both (n=19). Four of these patients were not available for follow-up. Antidepressant medications offered by the treating psychiatrist included fluoxetine (20-40 mg/day), escitalopram (10-15 mg/day), sertraline (50-100 mg/day) or mirtazapine (15-30 mg/day). Severity of depression was measured before start of treatment (baseline) and at the end of 3 months using the Hamilton Depression Rating Scale (HDRS) by a rater blind to the treatment group status of the patients.[9]
All patients agreeing to be treated with yoga were trained in yoga practices by the same therapist. They were requested to attend the training sessions on a daily basis for 2 weeks and again at weekly intervals for next 2 weeks. “Booster” sessions were provided once each in the 1st weeks of 2nd and 3rd months of the study. Each session of training/practice lasted one hour. On all other days patients were encouraged to practice yoga at home daily. The same was reinforced through telephonic contacts. A relative staying with the patient confirmed the patients’ accounts of yoga practice at home. Adherence to treatment was operationally defined as doing 50 or more yoga sessions in the 3 month period and/or using medications for at least 2 months.
Serum cortisol estimation
The serum samples were stored at - 80°C and were analyzed in one batch by laboratory staff unaware of the clinical details related to the samples. Serum cortisol was measured using the enzyme-linked immunosorbent assay technique with commercially available kits Globe Diagnostics SRL, Milan, Italy.
We used Chi-square test and independent-sample t-test for between-subject comparisons and paired t-test for within-subject comparisons. Pearson's r was used to examine the correlations between serum cortisol levels and HDRS scores.
RESULTS
The 58 patients and 18 healthy volunteers were comparable as regards age and gender (patients: 54.3±8.6 years and 23 females; controls: 34.0 ± 9.7 years and 10 females; t=0.95; P=0.34 and Chi-square=0.16; P=0.69). The serum cortisol was significantly higher in patients (105.6 ng/ml ± 58.7) than in controls (68.4 ng/ml ± 31.5; t=2.6, P=0.012). Current drug status (never-treated n=38 or drug-free for at least 1 month n=20) had no influence on baseline serum cortisol (103.2 ng/ml ± 63.5 and 110.1 ng/ml ± 49.8 respectively; t=0.42; P=0.68).
Following treatment the total scores on depression HDRS dropped significantly (n=54; baseline: 17.8±4.5; 3-month: 5.3±5.0; t=15.6; P=0.001). However, the drop in serum cortisol level was not statistically significant (n=54; baseline: 107.19 ng/ml±59.38; 3-month: 97.99 ng/ml±48.25; t=1.24; P=0.22). In the adherent patients (n=40, including all three treatment groups), the drop in cortisol level (baseline value=109.9 ng/ml±63.8 and 3-month value=96.3 ng/ml±48.5) reached a trend level of significance (t=1.79; P=0.08) compared with those who were non-adherent (n=14; the values were respectively 99.1 ± 45.6 and 102±48.9; t=0.21; P=0.8). In all patients who received yoga with or without medications (n=38), the change in serum cortisol level was significant (111.9 ng/ml±58.4-91.7 ng/ml±47.3; t=2.94; P=0.006); it was not so in those who received only medications (95.7 ng/ml±62.1-113 ng/ml±48.5; t=0.99; P=0.34).
Serum cortisol did not correlate with the baseline depression scores on HDRS (Pearson's r=0.031, P=0.82). There was a significant direct correlation between the drop in HDRS score (baseline-3-month HDRS total score) and drop in serum cortisol level (baseline - 3-month) in the treatment-adherent sample (n=40; r=0.5, P=0.001); it was not so in those who were not adherent (n=14; r=0.28, P=0.34). The treatment groups presented differential correlations, with patients in yoga-only group showing highly significant correlation between the drop in HDRS and drop in serum cortisol (medication-only: r=0.39, P=0.13; medication + yoga: r=−0.28, P=0.25; yoga-only r=0.59, P=0.008) [Figure 1].
Figure 1.
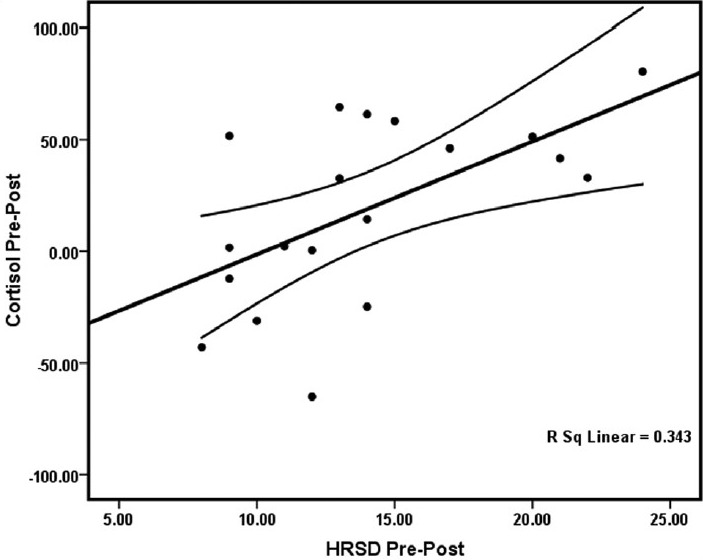
The drop in depression scores correlated significantly with the drop in cortisol levels for yoga-only treatment group (n=19)
There was a reduction of serum cortisol level in 32 patients; in the 22 remaining, there was an increase. The reductions in HDRS scores too occurred differentially in patients who had decrease (mean±SD HDRS change=13.87±5.37) or increase in cortisol (mean±SD HDRS change=10.5±6.11; t=2.14; P=0.037) [Figure 2].
Figure 2.
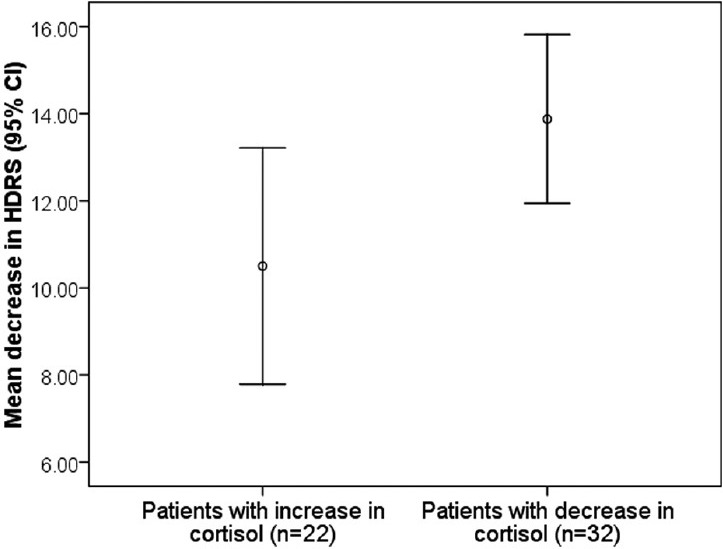
The change in hamilton depression rating scale scores in both cortisol-response groups
DISCUSSION
In this study, depressed out-patients had higher levels of serum cortisol level than the healthy controls. Adherence to treatment, irrespective of the treatment method, was associated with drop in cortisol level. Moreover, treatment with yoga was associated with a significant drop in cortisol. Those who received yoga-only as a treatment showed a high correlation between reduction of serum cortisol level and antidepressant response.
The findings in this clinical sample are in keeping with other reports of hypercortisolemia in depressive disorder that “correct” after treatment.[10] Treatment adherence tended to be associated with higher drop in cortisol levels suggesting a cause effect relationship. Patients getting yoga therapy either with drugs or solely had better reductions in cortisol levels. Higher proportion of yoga patients obtained decrease in cortisol levels. This is in keeping with yoga reducing cortisol in healthy and in other psychiatric disorders. For example, alcohol dependent subjects undergoing detoxification obtained a robust drop in cortisol levels when yoga was added.[6] Like in the earlier studies, cortisol reductions paralleled reductions in depressive syndrome.[11] This effect was the best observed with yoga. We had a little control over the medication subtypes or their doses. It is possible that the drug effects may confound cortisol response. Indeed, some antidepressant medications are known to increase cortisol levels upon acute administration.[12] Lack of a significant decrease in cortisol levels in antidepressant-treated patients may have been confounded by this effect. Yoga-only group was devoid of this biological confound. Therefore, the effects of yoga in reducing the cortisol level could be detected robustly. Even better, the relationship between the cortisol-lowering effect and the antidepressant effect was best demonstrated in this (yoga-only) group. Consistent with our findings, it has been observed that greater reduction of cortisol occurs in depressed patients who receive psychological treatment along with antidepressant medication than those who receive antidepressant medication alone.
Reduction in stress may be expected to lower the cortisol levels. The effect of yoga on reduction of cortisol may be attributable to the reduction of stress-related consequences. However, how does cortisol reduction produce antidepressant effects? Does cortisol reduction trigger yet another mechanism? There is evidence to suggest a reciprocal role for stress and cortisol on brain-derived neurotrophic factor (BDNF).[13,14,15] Further, impaired hypothalamo-pituitary-adrenal axishas been associated with reduced hippocampal volumes, suggesting its interference with neuroplasticity.[16,17,18] It is hence likely that lowered cortisol levels facilitate neurotropism. Increase in levels of BDNF could be one such evidence, which, if demonstrated to associate with cortisol reduction, have the potential to explain these observations. Increased BDNF levels related to antidepressant drugs have been interpreted as neuroplastic mechanisms in the relief of depressive symptoms. Alternatively, it is known that “de-stressing” effects of some treatments, including yoga, reduce cortisol. The direct effect of cortisol on certain steroid receptors in selected brain areas (hippocampus being one), causing depression, could hence be thwarted by antidepressant treatments, including yoga. This finding could be a link to newer molecules for antidepressant action, based on cortisol/steroid receptor blockade.
A few additional possible mechanisms of reduction of cortisol with yoga are worth discussing: Yoga is known to result in enhancement of parasympathetic (vagal) tone.[19] Increased parasympathetic activity may cause reduced firing of paragigantocellular nucleus of medulla to locus ceruleus. Decreased stimulation of locus ceruleus could decrease norepinephrine output, resulting in relaxation, quiescence and reduced respiratory and heart rates. Reduced input of norepinephrine to paraventricular nucleus of hypothalamus may explain the decreased corticotropin-releasing hormone and cortisol.[19] Enhanced parasympathetic tone and the resultant drop in blood pressure could relax arterial baroreceptors, leading to decreased γ-aminobutyric acid-ergic inhibition of supraoptic nucleus of hypothalamus, which in turn could cause the release of arginine vasopressin (AVP). AVP is known to cause positive affect.[20,21] Finally, yoga may cause activation of prefrontal cortex and enhanced glutamate transmission in the arcuate nucleus of the medial hypothalamus resulting in the release of beta-endorphin[22] – the latter causes anxiolysis,[23] which, in turn, may cause a reduction of cortisol.
In summary, out-patients with depression have increased levels of cortisol. The latter is associated with severity of depression only poorly. However, treatments that lower the cortisol levels, e.g., yoga produced antidepressant effects. Yoga had a significant and direct influence on cortisol response that correlated with yoga's antidepressant effects.
ACKNOWLEDGMENT
We would like to thank Dr. R. Nagaratna, Dean, Life Sciences, Swami Vivekananda Yoga Anusandhana Samsthana, Bangalore for her support, encouragement and guidance.
We thank Mr. Sushrutha and Mr. Bhagath of Swami Vivekananda Yoga Anusandhana Samsthana for their help with transliteration.
Footnotes
Source of Support: The research was done under the Advanced Centre for Yoga - Mental Health and Neurosciences, a collaborative centre of NIMHANS and the Morarji Desai Institute of Yoga, New Delhi
Conflict of Interest: None declared.
REFERENCES
- 1.Gillespie CF, Nemeroff CB. Hypercortisolemia and depression. Psychosom Med. 2005;67(Suppl 1):S26–8. doi: 10.1097/01.psy.0000163456.22154.d2. [DOI] [PubMed] [Google Scholar]
- 2.Christensen MV, Kessing LV. The hypothalamo-pituitary-adrenal axis in major affective disorder: A review. Nord J Psychiatry. 2001;55:359–63. doi: 10.1080/080394801317080873. [DOI] [PubMed] [Google Scholar]
- 3.Miller GE, Rohleder N, Stetler C, Kirschbaum C. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67:679–87. doi: 10.1097/01.psy.0000174172.82428.ce. [DOI] [PubMed] [Google Scholar]
- 4.Raison CL, Miller AH. When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. 2003;160:1554–65. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- 5.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 6.Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249–53. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Text Revision. 4th ed. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 8.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 9.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schüle C, Baghai TC, Eser D, Zwanzger P, Jordan M, Buechs R, et al. Time course of hypothalamic-pituitary-adrenocortical axis activity during treatment with reboxetine and mirtazapine in depressed patients. Psychopharmacology (Berl) 2006;186:601–11. doi: 10.1007/s00213-006-0382-7. [DOI] [PubMed] [Google Scholar]
- 11.Hinkelmann K, Moritz S, Botzenhardt J, Muhtz C, Wiedemann K, Kellner M, et al. Changes in cortisol secretion during antidepressive treatment and cognitive improvement in patients with major depression: A longitudinal study. Psychoneuroendocrinology. 2012;37:685–92. doi: 10.1016/j.psyneuen.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Schüle C, Baghai T, Schmidbauer S, Bidlingmaier M, Strasburger CJ, Laakmann G. Reboxetine acutely stimulates cortisol, ACTH, growth hormone and prolactin secretion in healthy male subjects. Psychoneuroendocrinology. 2004;29:185–200. doi: 10.1016/s0306-4530(03)00022-2. [DOI] [PubMed] [Google Scholar]
- 13.Smith MA, Makino S, Kvetnansky R, Post RM. Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNAs in the hippocampus. J Neurosci. 1995;15:1768–77. doi: 10.1523/JNEUROSCI.15-03-01768.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schaaf MJ, de Jong J, de Kloet ER, Vreugdenhil E. Downregulation of BDNF mRNA and protein in the rat hippocampus by corticosterone. Brain Res. 1998;813:112–20. doi: 10.1016/s0006-8993(98)01010-5. [DOI] [PubMed] [Google Scholar]
- 15.Bravo JA, Díaz-Veliz G, Mora S, Ulloa JL, Berthoud VM, Morales P, et al. Desipramine prevents stress-induced changes in depressive-like behavior and hippocampal markers of neuroprotection. Behav Pharmacol. 2009;20:273–85. doi: 10.1097/FBP.0b013e32832c70d9. [DOI] [PubMed] [Google Scholar]
- 16.Lupien SJ, de Leon M, de Santi S, Convit A, Tarshish C, Nair NP, et al. Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci. 1998;1:69–73. doi: 10.1038/271. [DOI] [PubMed] [Google Scholar]
- 17.Knoops AJ, Gerritsen L, van der Graaf Y, Mali WP, Geerlings MI. Basal hypothalamic pituitary adrenal axis activity and hippocampal volumes: The SMART-Medea study. Biol Psychiatry. 2010;67:1191–8. doi: 10.1016/j.biopsych.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 18.Gold SM, Kern KC, O’Connor MF, Montag MJ, Kim A, Yoo YS, et al. Smaller cornu ammonis 2-3/dentate gyrus volumes and elevated cortisol in multiple sclerosis patients with depressive symptoms. Biol Psychiatry. 2010;68:553–9. doi: 10.1016/j.biopsych.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohandas E. Neurobiology of spirituality. Mens Sana Monogr. 2008;6:63–80. doi: 10.4103/0973-1229.33001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Renaud LP. CNS pathways mediating cardiovascular regulation of vasopressin. Clin Exp Pharmacol Physiol. 1996;23:157–60. doi: 10.1111/j.1440-1681.1996.tb02589.x. [DOI] [PubMed] [Google Scholar]
- 21.Pietrowsky R, Braun D, Fehm HL, Pauschinger P, Born J. Vasopressin and oxytocin do not influence early sensory processing but affect mood and activation in man. Peptides. 1991;12:1385–91. doi: 10.1016/0196-9781(91)90224-d. [DOI] [PubMed] [Google Scholar]
- 22.Yadid G, Zangen A, Herzberg U, Nakash R, Sagen J. Alterations in endogenous brain beta-endorphin release by adrenal medullary transplants in the spinal cord. Neuropsychopharmacology. 2000;23:709–16. doi: 10.1016/S0893-133X(00)00152-4. [DOI] [PubMed] [Google Scholar]
- 23.Janal MN, Colt EW, Clark WC, Glusman M. Pain sensitivity, mood and plasma endocrine levels in man following long-distance running: Effects of naloxone. Pain. 1984;19:13–25. doi: 10.1016/0304-3959(84)90061-7. [DOI] [PubMed] [Google Scholar]


