Abstract
Context:
Yoga therapy has been demonstrated to be useful in treatment of negative symptoms and improving the socio-occupational functioning and emotion recognition deficits in antipsychotic-stabilized schizophrenia patients. Oxytocin has been recently implicated in social cognition deficits in schizophrenia. The effect of yoga therapy on oxytocin levels in schizophrenia has not been studied.
Aims:
This study aimed to assess the effect of yoga therapy on symptoms, socio-occupational functioning, facial emotion recognition deficits and plasma oxytocin levels in antipsychotic stabilized schizophrenia patients.
Settings and Design:
Randomized controlled study on 43 consenting, medication stabilized patients with schizophrenia in a tertiary psychiatric center using yoga intervention and waitlisted groups.
Materials and Methods:
A total of 43 schizophrenia patients were randomized to yoga group (n=15) or waitlist group (n=28). Patients in the yoga group received training in a specific yoga therapy module for schizophrenia. Patients in both groups were continued on stable antipsychotic medication. Assessments included scale for assessment of positive symptoms, scale for assessment of negative symptoms, socio-occupational functioning scale and tool for recognition of emotions in neuropsychiatric disorders (TRENDS) and plasma oxytocin levels; performed at baseline and at the end of 1 month.
Results:
A total of 15 patients in the yoga group and 12 in waitlist group completed the study. The yoga therapy group showed a significant improvement in socio-occupational functioning, performance on TRENDS (P<0.001) and plasma increase in oxytocin levels (P=0.01) as compared with the waitlist group.
Conclusion:
The study supported the role of add-on yoga therapy in management of schizophrenia and demonstrated an improvement in endogenous plasma oxytocin levels in schizophrenia patients receiving yoga therapy.
Keywords: Facial emotion recognition deficits, oxytocin, schizophrenia, tool for recognition of emotions in neuropsychiatric disorders, yoga
INTRODUCTION
Schizophrenia is one among the major mental disorders and is an important cause of disability. The disorder is associated with positive symptoms, negative symptoms, deficits in neuro-cognition as well as social-cognition. Among these the negative symptoms, neuro-cognitive and social-cognitive deficits continue to persist throughout the illness despite conventional antipsychotic therapy and contribute to poor socio-occupational functioning. Hence, intervention to improve these deficits and the socio-occupational functioning in antipsychotic stabilized schizophrenia patients is of important clinical relevance.
Social cognition deficits are being increasingly realized to be an independent symptom dimension in schizophrenia.[1] Facial emotion recognition deficits (FERD); an important component of social cognition, have been consistently demonstrated across the various phases during the course of schizophrenia. These deficits may be critical to our understanding of the evolution of psychopathology in schizophrenia and could be trait related deficits that can have a direct impact on patients socio-occupational functioning.[2]
Yoga is a traditional Indian system of alternative and complementary medicine with wide cultural acceptability. The role of yoga therapy has been demonstrated in various stress related disorders.[3,4] We have earlier reported beneficial role of yoga therapy in improving negative symptoms and socio-occupational functioning as an add on treatment in antipsychotic-stabilized patients.[5] In another study, we also reported the role of yoga therapy in improving FERD in schizophrenia.[6] While yoga therapy could potentially be a useful adjunct in the management of residual deficits in schizophrenia, the neurobiological mechanism through which yoga therapy can exert its beneficial effects is poorly understood and is an important area of research. Studies looking at the mechanism of action of yoga therapy have demonstrated it to have a role in modulation of the neuroendocrine axis, immunomodulators such as cytokines and vagal nerve stimulation.[7,8,9]
Oxytocin is a nine amino acid peptide that is synthesized in the magnocellular neurosecretory cells of the supraoptic and paraventricular nuclei of the hypothalamus and is released through the posterior pituitary into the peripheral circulation. Recent studies have demonstrated an increasing role for oxytocin in modulating social cognition abilities. Oxytocin can enhance the processing of positive socio-emotional cues facilitating interpersonal trust and pro-social interactions in humans.[10] It can also modulate neural responses to recognition of faces and enhance the ability to accurately discriminate facial emotions.[11] Studies on patient groups have demonstrated an association of low oxytocin levels with impaired performance on social cognition tasks in autism and schizophrenia.[12,13,14,15] The evidence for the role of oxytocin in mediating social cognition deficits is further strengthened by studies that have demonstrated a role for intra nasal oxytocin supplementation in improving social cognition abilities.[16]
Hence, the above studies support a role for oxytocin in mediating social cognition deficits in schizophrenia. Yoga therapy could potentially exert its beneficial effect on improving social cognition deficits in schizophrenia by increasing endogenous oxytocin levels, which in turn could modulate the neural circuits involved in emotion processing.[17]
On this background, the present study was conducted with the following aims: (1) To study the effect of yoga therapy on FERD, negative symptoms and social-occupational functioning as add on treatment in antipsychotic stabilized schizophrenia patients as compared to a waitlist group. (2) To study the effect of yoga therapy on plasma oxytocin levels and its correlation with FERD. The hypothesis proposed was that (1) Patient group receiving yoga therapy would show a significant improvement in FERD, negative symptoms and socio-occupational functioning. (2) There would be a significant increase in plasma oxytocin levels in the yoga therapy group as compared with the wait list group.
MATERIALS AND METHODS
Study subjects
A total of 43 subjects with a diagnosis of schizophrenia[18] who were between the ages of 18 and 45 years, on stable dosage of antipsychotics for at least last 6 weeks prior to recruitment, with clinical global impression[19] score of ≤3 and consenting to participate in the study were recruited from out-patient and in-patient services of the Department of Psychiatry, National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore. Diagnosis of Schizophrenia was made based on the DSM-IV criteria and confirmed independently by two qualified psychiatrists based on clinical interview and by administering mini-international neuropsychiatric interview plus.[20] Patients with psychoactive substance dependence (except nicotine) within the past 6 months or substance abuse within the past 1 month or those with comorbid neurological or medical disorders were excluded from the study. After obtaining informed consent, the subjects were randomized to either yoga group (N=15) or waitlist group (N=28). The antipsychotic treatment was decided by the treating psychiatrist and continued during the course of study. The study was approved by the institutional ethics committee.
Procedure
At baseline psychopathology was assessed using the scale for assessment of positive symptoms (SAPS)[21] and the scale for assessment of negative symptoms (SANS).[22] socio-occupational functioning was assessed using Socio-occupational functioning scale (SOFS).[23] Emotion recognition abilities were assessed using the tool for recognition of emotions in neuropsychiatric disorders (TRENDS).[24] Blood sample was drawn to assess the plasma oxytocin levels. The patients in the yoga group received yoga therapy along with antipsychotic medication for a period of 1 month while patients in the waitlist group continued antipsychotic medication alone without any additional intervention. Assessments performed at baseline were repeated after a period of 1 month in all subjects. Patients in the waitlist group were offered yoga therapy after their follow-up assessment. All patients who completed the study were adherent on medications and no antipsychotic medications were changed during the study period.
TRENDS
The TRENDS consists of a set of 52 validated images of four actors balanced for gender and age expressing six basic emotions of happy, sad fear, anger, surprise and disgust at two intensities along with a neutral expression. The tool used to assess emotion recognition abilities in this study; called the E-TRENDS was constructed using images from the TRENDS. E-PRIME software (Psychology Software Tools, Inc.) was used to display the images on a computer and record keystroke responses. The images consisted of fear, anger, happy, surprise and neutral images. The emotions were classified into threatening emotions (fear and anger), non-threatening emotions (happy, surprise) and neutral images (four actors × {two threatening emotions [fear, anger], + two non-threatening emotions [happy, surprise] + two neutral images} × two runs=48 stimuli). The test was administered in a quiet environment with the subjects placed at 50 cm from the computer screen. The 48 stimuli were presented in random order. Target stimulus depicting the image of facial expression appeared on screen for 3000 ms followed by a blank screen for 1000 ms before the next image.
The subjects were instructed to identify the emotion depicted in the image and to press one of the three specified buttons of the keyboard corresponding to the threatening (right arrow key), non-threatening (left arrow key) and neutral images (down arrow key). Pressing a button other than the one corresponding to the displayed image was considered as a misidentification error. The software recorded the response keystroke automatically.
Yoga therapy
Patients in the yoga group received training in a specific yoga therapy module for schizophrenia, by a professional yoga therapist at the Advanced Center for Yoga in NIMHANS for a period of 1 month. This yoga module was developed by the Swami Vivekananda Yoga Anusandhana, which is a Deemed University of Yoga at Bangalore; it consisted of loosening exercises, breathing practices, Suryanamaskāra, sitting and supine and prone posture Āsanas along with Prāṇāyāma and relaxation techniques. For further details regarding the yoga techniques please see Appendix.
Plasma oxytocin assessment
Blood sample was collected between 8 am and 9 am. After overnight fasting 10 cc of blood was drawn and collected into chilled ethylenediaminetetraacetic acid (1 ml/ml of blood) tubes containing aprotinin (500 KIU/ml). Sample was centrifuged at 1600 g for 15 min at 2-8°C. Plasma sample was immediately frozen and kept at −70°C until analysis. Plasma oxytocin levels were measured by using MILLIPLEX MAP multiplex assay kit (Millipore Life sciences, MA), analyzed by Luminex xMAP technology. (CV=6.25%).
Analysis
For assessing the performance on E-TRENDS the following scores were calculated. (1) TRENDS accuracy score (TRACS) defined as the total number of images, which were correctly identified as threatening, non-threatening or neutral (out of 48 stimuli). (2) TRENDS over identification score (TOI) defined as the total number of non-threatening or neutral images that were misidentified as neutral or threatening (out of 32 stimuli). Analysis using the Kolmogrov-Smirnov test indicated that the data was not normally distributed and hence non-parametric statistical tests were used. Mann-Whitney test was used to compare baseline variables between the two patient groups. Wilcoxon signed rank test was performed to compare the scores on SAPS, SANS, SOFS, TRENDS and plasma oxytocin levels between baseline and follow-up in each patient group.
RESULTS
In the yoga group, all 15 patients completed baseline and follow-up assessments. In the waitlist group, 12 patients completed both the assessments and were included in the final analysis. The 16 patients who dropped out in the waitlist group did so primarily due to logistic reasons.
The socio-demographic and clinical variables are described in Table 1. The yoga and waitlist group did not significantly differ in their baseline characteristics. The patients in waitlist group who did not complete follow-up assessments did not differ significantly in their demographic and clinical profile. On comparison of baseline and follow-up variables, both groups showed significant improvement in negative symptoms and positive symptoms (P<0.001). However only the yoga group showed a significant improvement in SOFS scores (P<0.001), TRACS (P<0.001), TOI (P=0.03) and plasma oxytocin level (P=0.01) [Table 2 and Figure 1]. On correlation analysis no significant correlation was found between plasma oxytocin levels and TRACS or TOI.
Table 1.
Demographic status and clinical characteristics of yoga group in comparison with waitlist group
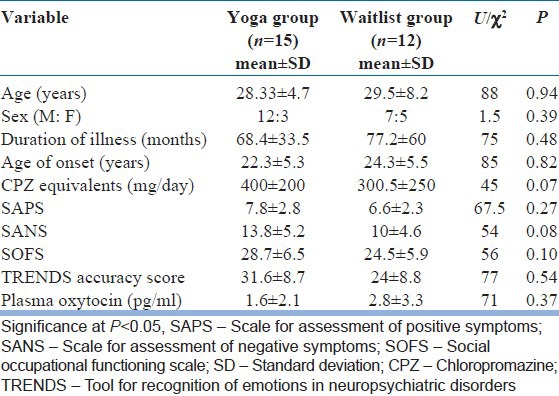
Table 2.
Comparative profile of psychopathology scores, TRENDS scores and plasma oxytocin between baseline and the follow-up
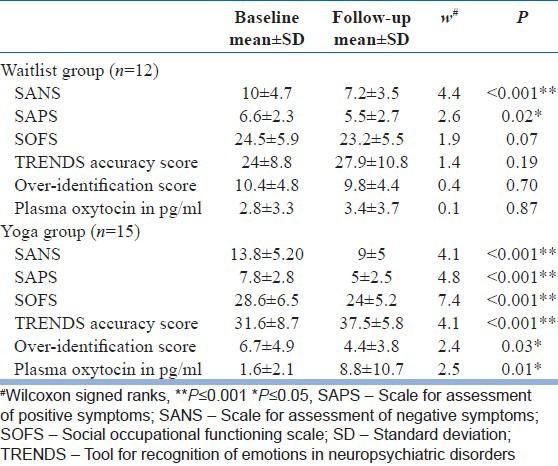
Figure 1.
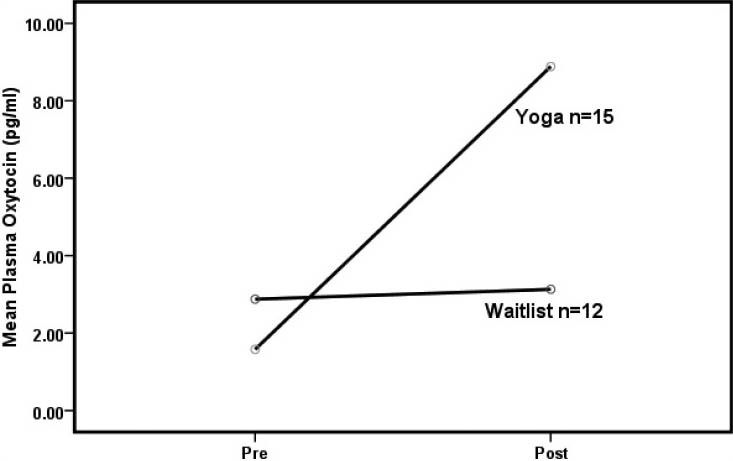
Change in plasma oxytocin from baseline to follow-up
DISCUSSION
The results of this study support a role for add on yoga therapy in improving symptoms, socio-occupational functioning and FERD in schizophrenia. We had earlier reported a beneficial effect of yoga on above dimensions in schizophrenia. This supports the earlier reported findings as we were able to replicate the results in an independent sample of patients. More importantly this study for the first time demonstrated the beneficial effect of yoga therapy on improving plasma oxytocin levels.
Enhanced emotional threat perception; as demonstrated by misidentification of neutral or non-threatening stimuli as threatening, has been described to possibly underlie the development of paranoia in patients with schizophrenia.[25] This misinterpretation of facial emotions can lead to impairment in behavior in response to social cues and situations and hence can adversely affect the socio-occupational functioning. Oxytocin has been demonstrated to be associated with pro-social behavior such as development of trust.[6]
In schizophrenia, patients’ deficits in oxytocin levels have been independently demonstrated to be associated with impairment in performance on tasks of social cognition. The role of oxytocin in mediation of social cognition is further strengthened by studies that have demonstrated a beneficial role for intra nasal oxytocin supplementation in improving social cognition deficits.[16] Hence, yoga therapy by increasing endogenous oxytocin levels can possibly exert its beneficial effects on FERD and functioning in schizophrenia. In this study, no correlation was found between change in oxytocin levels and change in TRACS score. A positive correlation would have supported a direct role of change in plasma oxytocin levels in improving FERD. Probably studies with a larger sample size are required to consistently demonstrate this effect.
One of the mechanism by which yoga therapy can modulate oxytocin synthesis is through its action on the vagal nerve. Yoga therapy increases vagal activity by stimulation of dermal and/or subdermal pressure receptors that are innervated by vagal afferent fibers, which ultimately project to the limbic system and are directly or indirectly connected to neuroendocrine outputs.[9,26] In an earlier study on “OM” chanting, we had postulated the role of vagal nerve stimulation by yoga practices in causing deactivation of limbic areas.[27] Interestingly, evidence from animal studies has shown that stimulation of vagal afferents increases plasma oxytocin levels.[28] Hence, indirect evidence from the above mentioned studies support a possible vagal nerve mediated mechanism for yoga therapy in improving oxytocin levels.
Certain limitations are inherent in an intervention of this nature. It is not possible to achieve blinding to treatment received in the patient group. Hence a possible placebo effect due to an expectation of outcome from treatment, meeting a professional on a regular basis can be expected. Further increased social interactions during the yoga session may have also contributed to elevated plasma oxytocin levels. Hence further studies need to control these factors possibly by including an arm of physical exercise in which patients attend similar number of sessions and are exposed to similar avenues of social interaction.
CONCULSION
This study demonstrated the beneficial role of add-on yoga therapy in antipsychotic stabilized schizophrenia patients in improving symptoms, socio-occupational functioning and FERD. Importantly, the study also demonstrated a significant improvement in plasma oxytocin levels in the yoga group. This finding can have important implications in intervention to improve socio-occupational functioning in schizophrenia. Further studies are required to replicate the findings as well as elucidate the potential neurobiological mechanisms by which yoga therapy can exert its beneficial effects in schizophrenia.
ACKNOWLEDGMENTS
The authors are grateful to the subjects who kindly consented to be a part of the study. The authors would like to thank the anonymous reviewers whose comments were very useful in enhancing the quality of the manuscript.
We thank Mr. Sushrutha and Mr. Bhagath of Swami Vivekananda Yoga Anusandhana Samsthana for their help with transliteration.
Footnotes
Source of Support: The research was done under the Advanced Centre for Yoga - Mental Health and Neurosciences, a collaborative centre of NIMHANS and the Morarji Desai Institute of Yoga, New Delhi
Conflict of Interest: None declared.
REFERENCES
- 1.Brüne M. Emotion recognition, ‘theory of mind,’ and social behavior in schizophrenia. Psychiatry Res. 2005;133:135–47. doi: 10.1016/j.psychres.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Grady CL, Keightley ML. Studies of altered social cognition in neuropsychiatric disorders using functional neuroimaging. Can J Psychiatry. 2002;47:327–36. doi: 10.1177/070674370204700403. [DOI] [PubMed] [Google Scholar]
- 3.Malathi A, Damodaran A. Stress due to exams in medical students – Role of yoga. Indian J Physiol Pharmacol. 1999;43:218–24. [PubMed] [Google Scholar]
- 4.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I-neurophysiologic model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 5.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia: A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 6.Behere RV, Arasappa R, Jagannathan A, Varambally S, Venkatasubramanian G, Thirthalli J, et al. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123:147–53. doi: 10.1111/j.1600-0447.2010.01605.x. [DOI] [PubMed] [Google Scholar]
- 7.Bowman AJ, Clayton RH, Murray A, Reed JW, Subhan MM, Ford GA. Effects of aerobic exercise training and yoga on the baroreflex in healthy elderly persons. Eur J Clin Invest. 1997;27:443–9. doi: 10.1046/j.1365-2362.1997.1340681.x. [DOI] [PubMed] [Google Scholar]
- 8.Kuntsevich V, Bushell WC, Theise ND. Mechanisms of yogic practices in health, aging, and disease. Mt Sinai J Med. 2010;77:559–69. doi: 10.1002/msj.20214. [DOI] [PubMed] [Google Scholar]
- 9.Field T. Yoga clinical research review. Complement Ther Clin Pract. 2011;17:1–8. doi: 10.1016/j.ctcp.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Domes G, Heinrichs M, Michel A, Berger C, Herpertz SC. Oxytocin improves “mind-reading” in humans. Biol Psychiatry. 2007;61:731–3. doi: 10.1016/j.biopsych.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Marsh AA, Yu HH, Pine DS, Blair RJ. Oxytocin improves specific recognition of positive facial expressions. Psychopharmacology (Berl) 2010;209:225–32. doi: 10.1007/s00213-010-1780-4. [DOI] [PubMed] [Google Scholar]
- 12.Hollander E, Novotny S, Hanratty M, Yaffe R, DeCaria CM, Aronowitz BR, et al. Oxytocin infusion reduces repetitive behaviors in adults with autistic and Asperger's disorders. Neuropsychopharmacology. 2003;28:193–8. doi: 10.1038/sj.npp.1300021. [DOI] [PubMed] [Google Scholar]
- 13.Modahl C, Green L, Fein D, Morris M, Waterhouse L, Feinstein C, et al. Plasma oxytocin levels in autistic children. Biol Psychiatry. 1998;43:270–7. doi: 10.1016/s0006-3223(97)00439-3. [DOI] [PubMed] [Google Scholar]
- 14.Goldman M, Marlow-O’Connor M, Torres I, Carter CS. Diminished plasma oxytocin in schizophrenic patients with neuroendocrine dysfunction and emotional deficits. Schizophr Res. 2008;98:247–55. doi: 10.1016/j.schres.2007.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubin LH, Carter CS, Drogos L, Jamadar R, Pournajafi-Nazarloo H, Sweeney JA, et al. Sex-specific associations between peripheral oxytocin and emotion perception in schizophrenia. Schizophr Res. 2011;130:266–70. doi: 10.1016/j.schres.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pedersen CA, Gibson CM, Rau SW, Salimi K, Smedley KL, Casey RL, et al. Intranasal oxytocin reduces psychotic symptoms and improves Theory of Mind and social perception in schizophrenia. Schizophr Res. 2011;132:50–3. doi: 10.1016/j.schres.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 17.Petrovic P, Kalisch R, Singer T, Dolan RJ. Oxytocin attenuates affective evaluations of conditioned faces and amygdala activity. J Neurosci. 2008;28:6607–15. doi: 10.1523/JNEUROSCI.4572-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Text Revision. 4th ed. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 19.Guy W. Rockville (MD): National Institute of Mental Health; 1976. ECDEU Assessment Manual for Psychopharmacology; pp. 218–22. [Google Scholar]
- 20.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 21.Andreasen NC. Iowa City: University of Iowa; 1984. Scale for the Assessment of Positive Symptoms (SAPS) [Google Scholar]
- 22.Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS): Conceptual and theoretical foundations. Br J Psychiatry Suppl. 1989;7:49–58. [PubMed] [Google Scholar]
- 23.Saraswat N, Rao K, Subbakrishna DK, Gangadhar BN. The Social Occupational Functioning Scale (SOFS): A brief measure of functional status in persons with schizophrenia. Schizophr Res. 2006;81:301–9. doi: 10.1016/j.schres.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Behere RV, Raghunandan V, Venkatasubramanian G, Subbakrishna D, Jayakumar P, Gangadhar B. TRENDS-A tool for recognition of emotions in neuropsychiatric disorders. Indian J Psychol Med. 2008;30:2. [Google Scholar]
- 25.Behere RV, Venkatasubramanian G, Arasappa R, Reddy NN, Gangadhar BN. First rank symptoms and facial emotion recognition deficits in antipsychotic naïve schizophrenia: Implications for social threat perception model. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1653–8. doi: 10.1016/j.pnpbp.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Arora S, Bhattacharjee J. Modulation of immune responses in stress by Yoga. Int J Yoga. 2008;1:45–55. doi: 10.4103/0973-6131.43541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalyani BG, Venkatasubramanian G, Arasappa R, Rao NP, Kalmady SV, Behere RV, et al. Neurohemodynamic correlates of ‘OM’ chanting: A pilot functional magnetic resonance imaging study. Int J Yoga. 2011;4:3–6. doi: 10.4103/0973-6131.78171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stock S, Uvnäs-Moberg K. Increased plasma levels of oxytocin in response to afferent electrical stimulation of the sciatic and vagal nerves and in response to touch and pinch in anaesthetized rats. Acta Physiol Scand. 1988;132:29–34. doi: 10.1111/j.1748-1716.1988.tb08294.x. [DOI] [PubMed] [Google Scholar]


