Abstract
Objectives
This study aimed to identify demographic, psychological, health-related, and geographic predictors of adherence to home-based and supervised components of a yoga intervention in breast cancer survivors.
Methods
Participants were the 32 post-treatment breast cancer survivors who were randomized to the Viniyoga intervention arm of a controlled trial. Participants were asked to practice yoga 5 times per week for 6 months, including at least one weekly facility-based session. Adherence was monitored using sign-in sheets and logs. Height and weight were measured; other potential predictors of adherence were obtained from baseline questionnaires.
Results
Participants attended 19.6±13.0 yoga classes and performed 55.8±32.8 home-based yoga sessions. Participants adhered to 58% of the overall yoga practice goal (75% of the goal for yoga classes and 54% of the goal for home based-sessions). Higher class attendance and home practice were predicted by greater self-efficacy for yoga (p=0.004 and 0.06, respectively). Additionally, employment outside the home was associated with greater class attendance (p=0.004), while higher waist circumference was marginally associated with lower adherence to home-based yoga (p=0.05).
Conclusions
High levels of facility- and home-based yoga practice were achieved. Breast cancer survivors who have lower self-efficacy for yoga or who have a higher waist circumference may benefit from additional support or intervention tailoring. Adherence may also be improved by ensuring that class times are convenient to both working and nonworking women.
Introduction
The United States is home to 2.4 million breast cancer survivors,1 many of whom experience long-lasting effects of diagnosis and treatment, including fatigue,2 anxiety, depression,3 weight gain,4 and lymphedema.5 Lifestyle interventions involving yoga are a potential way to help breast cancer survivors manage lingering pain and treatment side-effects. Yoga has been found to reduce fatigue and depression and to improve sleep and overall quality of life among healthy older adults and cancer survivors.6–8 Among breast cancer survivors, yoga has been associated with reduced arthralgia pain,9 reduced fatigue and salivary cortisol levels,10,11 and improved emotional functioning12 and quality of life.13–15
Trials involving lifestyle interventions often achieve lower adherence than trials involving medications, in part because they require extended motivation and effort on the part of participants.16 When adherence is lower than expected, participants may receive an insufficient dose of the intervention, biasing the study results toward the null hypothesis. Consequently, understanding predictors of adherence itself is important to study for yoga and other lifestyle interventions. While most studies of lifestyle interventions report basic adherence statistics, few provide detailed information about adherence rates and predictors of adherence.
Previous studies among breast cancer survivors have found that yoga interventions are generally feasible and safe.7,12,17 Only a few studies have examined adherence to combined facility- and home-based interventions; these have generally reported moderate-to-good adherence. Carson et al. investigated effects of an 8-week trial of the Yoga of Awareness program (a comprehensive program that draws strongly on the Kripalu school of yoga, in which postures are complemented by meditation techniques, breathing exercises, didactic presentations, and group discussions) versus wait-list control in adult survivors (>2 years postdiagnosis) of early-stage (stages IA-IIB) breast cancer with no signs of active breast cancer but ≥1 hot flash/day on ≥4 days per week. In this study, the authors reported that participants (n=17 in the yoga intervention group) attended, on average, six of the eight weekly classes and performed 30 minutes per day of home practice.18 Poorer adherence was observed in a 12-week trial of weekly Hatha yoga classes plus home practice versus wait-list control in a multiethnic, urban sample of patients with breast cancer, in which 31% of intervention group participants did not attend a single class.19 Among those who did attend classes, however, mean attendance was 7.0 (standard deviation [SD]=3.8) of 12 classes. Although low in absolute terms, the adherence rates in this study are encouraging considering that this well-conducted study focused on an underserved and understudied population, who were on average only 1 year postdiagnosis (range: 2 weeks to 5 years), whereas most other studies report on highly selected samples that had subjects who are likely to be more adherent.
The short duration of most yoga studies limits the ability to predict adherence to programs of longer duration, which may be necessary to achieve long-term, sustainable benefits. Of the 10 studies included in a recent systematic review of yoga for patients with cancer,20 six featured interventions lasting ≤8 weeks, one used a 12-week intervention, and three did not report the duration of the intervention. While these studies provide valuable information regarding short-term adherence to yoga, for outcomes such as weight, longer-duration interventions are needed and therefore more information is needed regarding the feasibility of long-term yoga practice.
Similarly, only a few studies13,19,21 have evaluated the demographic and psychosocial factors that may affect adherence of breast cancer survivors to yoga intervention. In one study of Iyengar yoga among post-treatment survivors, demographics were not predictive of 12-week adherence, but participants with more advanced tumors or a history of previous cancer adhered better, as did those reporting less fatigue and more happiness at baseline. Other studies have identified fatigue, age, radiation therapy, and hormonal treatment as relevant to adherence.12,19
In this article, detailed adherence data are presented from the intervention arm of a two-arm randomized trial with the longest-duration yoga trial yet reported among breast cancer survivors. The overall aims of the parent trial22 were to obtain estimates of the time to recruit the sample, levels of retention and adherence, and the efficacy of the yoga intervention on fatigue, quality of life, and weight change. The parent trial found that the yoga intervention was feasible and well accepted among breast cancer survivors. Quality of life and fatigue improved to a greater extent in women in the yoga group compared to the control group, although these differences did not meet statistical significance in the small sample in this study. Waist circumference decreased more among yoga group participants than among those in the control group. No between-group difference in weight change was observed. Full results are reported separately.22 The 26-week intervention consisted of facility- and home-based Viniyoga, a gentle form of Hatha yoga. Demographic, psychologic, health-related, and geographic predictors of adherence are also examined. This study extends the literature by providing new evidence that regular, long-term yoga practice is feasible in this population and addresses issues relevant to maximizing adherence.
Materials and Methods
Participants
Participants were 32 breast cancer survivors aged 47–74 years who were randomized to a 26-week Viniyoga intervention as part of a randomized controlled trial. All participants had a diagnosis of Stage 0–III breast cancer, had completed adjuvant therapy at least 3 months prior to enrollment (continued use of hormonal or biologic therapies was allowed), and had no physical or psychologic conditions that would contraindicate participation in the program. Eligible women had a body mass index (BMI) ≥24.0 kg/m2 (≥23.0 kg/m2 for Asian-American women). This BMI criterion was chosen to facilitate recruitment while targeting only those women who were overweight/obese or at risk for overweight. Women were excluded if they had practiced yoga more than once per month during the past 6 months, were pregnant or planned to become pregnant, were diabetic, or had experienced a myocardial infarction or stroke in the past 6 months.
Recruitment
Study participants were recruited between May 2007 and April 2008 using media placements, flyers, direct mailings, a study website, and referrals. A preliminary eligibility screening was conducted by telephone, after which interested individuals attended an information session and a clinic visit and completed questionnaires. Participants were block randomized to the yoga intervention or a wait-list control group on tumor stage, age, and BMI. Only women randomized to the yoga intervention are included in the current analyses. Written informed consent was obtained following the requirements of the Fred Hutchinson Cancer Research Center Institutional Review Board. Additional details are available elsewhere.22
Assessment of predictor variables
Potential demographic, geographic, cancer-related, psychosocial, and anthropometric predictors of adherence were assessed at baseline. The majority of predictors were collected via self-report on the baseline questionnaire. Height, weight, and waist circumference were measured directly by study staff.
Demographic predictors
The following demographic variables were examined as potential predictors of adherence: age, educational attainment (high school, some college, college graduate, postgraduate degree), and work status (employed outside the home versus not).
Geographic factors
Driving distance (kilometers) and estimated drive time (minutes) from each participant's home address to the facility were calculated using Google's mapping function (http://maps.google.com/).
Physical activity
Baseline leisure-time physical activity (summarized as total metabolic equivalent in minutes/week23) over the past 12 months was assessed using a self-administered version of the Modifiable Activity Questionnaire.24 Twenty-nine (29) activities were listed (e.g., walking at a moderate pace, bicycling, jogging, and t'ai chi) and space for activities not listed was also included.22
Cancer characteristics
Cancer-related predictors included tumor stage at diagnosis (Stage 0, I, II, or III) and years since diagnosis (calculated as years from diagnosis date to randomization).
Psychosocial factors
Sleep was assessed using the following item from the Pittsburgh Sleep Quality Index25: “During the past month, how many hours of actual sleep did you get at night? (This may be different than the number of hours you spend in bed.)”.
Stress was measured using Cohen's 10-item Perceived Stress Scale,26 a reduction of the original 14-item version27 that retains good psychometric properties.26 Potential scores range from 0 to 40, with higher scores reflecting greater perceived stress. Fatigue was assessed using the 13-item Functional Assessment of Chronic Illness Therapy fatigue subscale.28 This measure has a potential score range of 0–160; higher scores reflect less fatigue (i.e. better functioning). The 20-item Centers for Epidemiological Studies Depression Scale29 was used to evaluate depressive symptoms; the range of potential scores is 0–60 with higher scores indicating more depressive symptoms. Social support was assessed using the 12-item version of the Interpersonal Support Evaluation List. This measure produces a score range of 0–36, with high scores reflecting a greater availability of social support.
Self-efficacy for yoga was evaluated using a 6-item modified version of Bandura's Exercise Self-Efficacy Scale.30 The items assessed the participant's confidence in her ability to perform yoga despite specific barriers (e.g., when too busy, tired, in a bad mood, on vacation, experiencing cancer-related pain/symptoms). Participants responded on an 11-point Likert scale (0=not at all confident, 10=very confident); item scores were then averaged to produce a total score ranging from 0 to 10.
Anthropometrics
Height, weight, and waist circumference were measured by study staff at the baseline clinic visit. Height without shoes was measured twice to the nearest 0.1 cm on a stadiometer; the two measures were averaged. Weight was measured to the nearest 0.1 kg on a balance beam scale. BMI was calculated as kg/m2. Waist circumference was measured twice at the end of normal expiration at the narrowest location on the torso, to the nearest 0.1 cm; the two measures were averaged.
Intervention
The facility- and home-based intervention consisted of Viniyoga, a gentle, therapeutic style of Hatha yoga that is appropriate for various fitness and skill levels, including overweight and obese individuals. Viniyoga involves physical stretches and poses, breath control, and meditation and emphasizes individualization of postures to meet the abilities and needs of the individual. As a consequence, it is well suited for use in therapeutic settings. Viniyoga is characterized by the use of repetition into and out of postures in addition to holding postures. Gary Kraftsow evolved this approach to yoga from the teachings transmitted by T. Krishnamacharya and T.K.V. Desikachar of Madras, India.31
Classes
Participants were asked to attend at least one of three weekly Viniyoga classes at the study site (Fred Hutchinson Cancer Research Center, Seattle, WA. The Instructor Manual is part of Supplementary Data (Supplementary Data are available online at www.liebertpub.com/acm). These 75-minute classes, developed specifically for the intervention, were designed to be easily modified for differing levels of ability and physical function. Each yoga practice opened with a 5–10-minute “check-in” period to allow participants to introduce themselves, discuss their current status, ask questions, or share concerns about their home practice or physical pain/tightness that instructors could address during the class. After sounding three oms, 5–8 minutes was allotted for breathing and body awareness exercises, including cultivating an intention for their practice. During this time, the teacher instructed the participants to focus on abdominal breathing and drew their attention to their breath. Next, instructors led the students through a total of 11–16 postures, including a mixture of supine, prone, quadruped, and standing poses. Each pose was repeated 6–8 times, alternating sides. The class was structured to gradually prepare students for the pinnacle pose or poses (e.g., triangle, lunge/warrior variations, standing forward bend, and standing twists) with preparatory poses (e.g., cat/cow, cobra, chakravakasana, wide leg-forward bends). Following the pinnacle pose, counter poses were performed that were specific to the pinnacle pose(s) (e.g., child's pose, bow/locust, lunge/warrior variations, apanasana, bridge, knee circles, and bound angle pose [baddha konasana]). Next, approximately 5 minutes was allotted for corpse pose (savasana). To conclude the practice, instructors led the participants in a seated silent meditation for approximately 5 minutes. They encouraged students to repeat the following mantra (Inhale “I calm my body”; Exhale “I smile, cultivating [fill in the blank] in this moment”). Participants were instructed to fill in the blank with a word (e.g., peace, healing, wholeness, etc.) that held meaning for them. All participants received a yoga mat and strap; blankets, blocks, and chairs were available in class. The classes were taught by local yoga instructors who had previous experience leading yoga classes for populations with special needs (e.g., cancer, multiple sclerosis). A manual with detailed class guidelines and descriptions of how poses are performed and can be modified was developed to standardize delivery of the intervention and is available by contacting the corresponding author.
Home practice
In addition to attending facility-based yoga classes, participants were also asked to perform 15–30-minute sessions of yoga at home, to achieve a total goal of 5 days per week (e.g., one class + four home sessions; two classes + three home sessions). Each participant received a DVD containing four different yoga practices as well as a yoga booklet with descriptions and photographs depicting each of the poses used in the DVD. The Home Practice Guide is part of Supplementary Data (Supplementary Data are available online at www.liebertpub.com/acm).
The DVDs were developed specifically for the study, and included instruction and modeling of poses by the class instructors. These practices mirrored the facility-based classes in both content and style, with fewer poses and breathing exercises in order to keep the practice to less than 30 minutes.
Overall goal
Participants were asked to attend at least one facility-based yoga class per week, supplemented by home-based yoga practice to meet an overall goal of five sessions per week. Thus, there were various ways to meet the goal (e.g., one class plus four home-based sessions; two classes plus three home-based sessions).
Monitoring of adherence
Adherence to facility-based yoga classes was tracked by attendance sign-in sheets collected by instructors at each class. Adherence to home-based yoga practice was determined from paper log sheets completed by participants and turned in to yoga instructors each week. Telephone counseling was used to encourage adherence and help participants navigate specific barriers. A participant received a call if she (1) failed to attend class for 2 consecutive weeks, (2) failed to meet the overall goal of five yoga sessions/week for 2 consecutive weeks, and/or (3) fell behind on returning her weekly logs.
Outcome measures
Given that the factors that influence attendance at yoga classes may be very different from those that predict at-home yoga, two adherence variables were calculated and separate analyses were conducted for them: (1) total number of facility-based classes attended during the 26-week intervention, and (2) total number of home yoga sessions performed during the intervention as assessed from weekly logs. If no log was turned in, it was assumed that the participant did not practice yoga that week.
Statistical analyses
The distributions of each potential predictor variable were examined to identify outliers and to determine appropriate measures for categorization and/or transformation. Variables for age, BMI, waist circumference, baseline physical activity, sleep, perceived stress, self-efficacy, driving time to class site, and distance to class site were left in their original form. For years since diagnosis, depressive symptoms, fatigue, and social support, a transformation was applied to reduce the impact of outliers on the correlation coefficients. The authors log transformed years since diagnosis and depressive symptoms and used a square root transformation for fatigue. Because neither of these transformations led to a normal distribution, the authors categorized social support as high (>25) versus low (<25). Due to outliers in the adherence outcomes, a log transformation was applied to both number of classes attended and number of home yoga sessions performed.
Associations between baseline variables and each of the adherence measures were next assessed using Pearson correlations (for continuous predictors) and regression (for categorical predictors). Variables that were univariately associated with an adherence measure based on having a p-value<0.10 were then entered in a multiple regression model. In cases where two or more correlated measures with overlapping constructs (e.g., BMI and waist circumference) met the p<0.10 criterion, only one was chosen for entry into the model. All participants were included in adherence analyses, regardless of whether they completed the study. Data analyses were performed using SAS 9.1 (SAS Institute Inc., Cary, NC) and all tests were two-sided.
Results
Sample characteristics
Participants were, on average, 60.3 (SD=7.2) years of age with a BMI of 29.8 kg/m2 (SD=4.0, Table 1). Ninety-four percent (94%) were overweight or obese (BMI≥25.0 kg/m2). Ninety-one percent (91%) were non-Hispanic white, 41% had a postgraduate degree, and 56% were employed outside the home. Participants reported low-to-moderate perceived stress and depressive symptoms, sleeping just under 7 hours per night on average, and moderate-to-high levels of social support. The majority was diagnosed at an early stage of breast cancer (44% at Stage 0, 22% at Stage I, and 34% at Stage II–IIIA). Time since breast cancer diagnosis ranged from 0.6 to 18.1 years; 31% had been diagnosed in the previous 3 years. They lived, on average, 10.3 km (SD=7.7) from the facility with an estimated mean drive time of 14 minutes (SD=6.5).
Table 1.
Baseline Characteristics of Participants (n=32)
| % or Mean (SD) (range) | |
|---|---|
| Age (yrs) | 60.3 (7.2) (47–74) |
| Non-Hispanic white | 91% |
| Postgraduate degree | 41% |
| Employed | 56% |
| Weight (kg) | 82.4 (13.6) (63.5–119.4) |
| BMI (kg/m2) | 29.8 (4.0) (24.7–41.3) |
| Waist circumference (cm) | 93.6 (7.4) (85.0–112.8) |
| Perceived stressa | 13.5 (5.9) (0.0–30.0) |
| Depressive symptomsb,c | |
| <7 | 38% |
| 7–10 | 28% |
| 11+ | 34% |
| Fatiguec,d | |
| <124 | 31% |
| 124–137 | 31% |
| 137+ | 38% |
| Sleep (hours/night) | 6.8 (1.0) (4.0–9.0) |
| Social supportc,e | |
| Low (<29) | 38% |
| High (≥29) | 62% |
| Self-efficacy for yogaf | 8.2 (1.3) (5.7–10.0) |
| Total physical activity (MET–hours/week) | 23.6 (24.0) (0.0–120.4) |
| Tumor stage | |
| 0 (in situ) | 44% |
| I | 22% |
| II–IIIA | 34% |
| Years since diagnosisc | |
| 0.6–<3 | 31% |
| 3–6 | 38% |
| 7–18 | 31% |
| Distance to facility (km) | 10.3 (7.7) (1.6–34.3) |
| Drive time to facility (min) | 14.0 (6.5) (3.0–34.0) |
Assessed by the Perceived Stress Scale, score range 0–40.
Assessed by the Centers for Epidemiologic Diseases Depression Scale, score range 0–40.
Categories presented because variable distribution was skewed.
Assessed by the Functional Assessment of Chronic Illness Therapy Fatigue, score range 0–160.
Assessed by the Interpersonal Support Evaluation, score range 0–36.
Assessed by a modified version of Bandura's Exercise Self-Efficacy scale, score range 0–10.
SD, standard deviation; BMI, body–mass index; MET, metabolic equivalent task.
Overall adherence
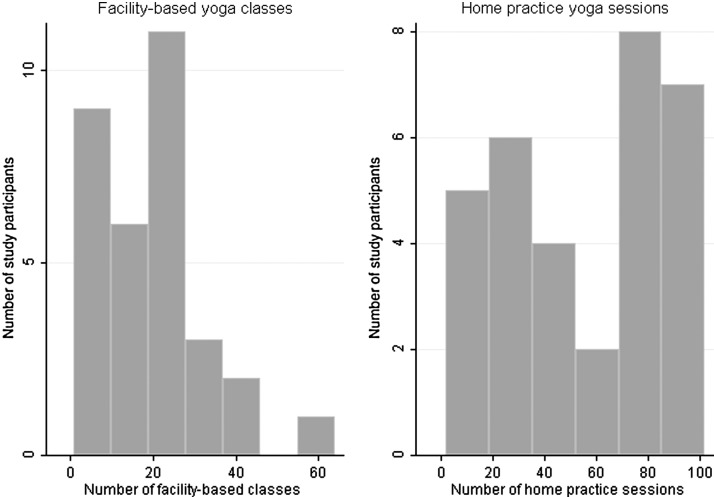
Over the 26-week intervention, participants attended, on average, 19.6 yoga classes (SD=13.0; range 1–61) and completed 55.8 home yoga sessions (SD=32.8; range 2–102). A more detailed breakdown of the distribution of facility- and home-based practice is shown in Figure 1. Participants were asked to practice yoga 5 times per week, including at least one facility-based session. Overall, participants adhered to 58% of that goal (75% of the goal for yoga classes and 54% of home-based sessions based on a conservative criterion of 4 home-based sessions per week) (Table 2). Fifty-nine percent (59%) of women achieved at least half the total number of goal sessions across the 26-week intervention; 72% of women achieved at least half of the goal for yoga classes and 53% achieved at least half of the goal for home-based practice.
FIG. 1.
Distribution of facility-based and home-based yoga practice.
Table 2.
Percent of Yoga Goal Achieved
| Total yoga | Facility-based yoga classes | Home-based yoga sessions | |
|---|---|---|---|
| Percent of goal sessions completeda | |||
| Mean | 58% | 75% | 54% |
| Range | 4–119% | 4–235% | 2–98% |
| Percent of participants adhering to criterion: | |||
| ≥90% of goal | 16% | 31% | 13% |
| ≥75% of goal | 41% | 53% | 41% |
| ≥50% of goal | 59% | 72% | 53% |
| ≥25% of goal | 78% | 78% | 75% |
Participants were asked to complete one yoga class plus four home-based sessions per week, or an equivalent combination totaling 5 days of yoga (e.g., two classes and three home sessions). Percents for home-based yoga are conservatively based on the maximum goal of four home-based sessions.
Predictors of adherence
Associations between various factors and facility-based attendance and home practice are shown in Table 3. The number of facility-based yoga classes attended during the 6-month intervention was inversely associated with BMI (p=0.09) and waist circumference (p=0.04) and positively associated with self-efficacy (p=0.06), being employed (p=0.07), and tumor stage (p=0.02). Home yoga practice was inversely associated with BMI (p=0.03) and waist circumference (p=0.01) and positively associated with self-efficacy (p=0.01). Because waist circumference and BMI were highly intercorrelated (r=0.61, p=0.002), only waist circumference was entered in the multivariable models as it had a stronger correlation with the outcomes than did BMI. Perceived stress, depressive symptoms, fatigue, and sleep were not statistically significantly associated with either facility-based or home-based yoga practice.
Table 3.
Associations Between Demographic, Anthropometric, Cancer, Health, and Geographic Factors and Adherence to Supervised Yoga Classes and Home-Based Yoga Over 6 Months (N=32)
| Facility-based yoga classesa | Home-based yogab | |
|---|---|---|
| Continuous variables | Correlationc(p-value) | Correlationc(p-value) |
| Age (years) | −0.15 (0.41) | −0.06 (0.74) |
| BMI (kg/m2) | −0.31 (0.09) | −0.38 (0.03) |
| Waist circumference (cm) | −0.37 (0.04) | −0.44 (0.01) |
| Perceived stress | −0.03 (0.88) | −0.007 (0.97) |
| Depressive symptomsd | 0.02 (0.90) | −0.005 (0.98) |
| Fatiguee | 0.13 (0.46) | 0.09 (0.62) |
| Sleep (typical h/night) | 0. 17 (0.36) | 0.22 (0.23) |
| Self-efficacy | 0.34 (0.06) | 0.42 (0.01) |
| Baseline physical activity (MET-h/week) | 0.12 (0.52) | 0.14 (0.44) |
| Years since diagnosisd | −0.11 (0.57) | 0.07 (0.69) |
| Driving time to facility (min) | −0.21 (0.24) | −0.00 (0.98) |
| Distance to facility (km) | −0.19 (0.29) | −0.01 (0.95) |
| Categorical variables | βf (p-value) | βf (p-value) |
| Postgraduate degree vs. college degree or less | 1.55 (0.18) | 0.91(0.81) |
| Employed vs. not employed | 1.80 (0.07) | 1.77 (.21) |
| Tumor stage I-IIIA vs. 0 | 2.05 (0.02) | 1.67 (0.17) |
| High vs. low social support | 1.07 (0.85) | 1.23 (0.60) |
Bolded values have a p<0.1.
Number of yoga classes attended, as recorded on attendance sheets.
Number of home-based yoga sessions, as recorded on participant logs.
Pearson's r.
Log transformed to reduce effect of outliers on the correlation analysis.
Square-root transformed to reduce effect of outliers on the correlation analysis.
Outcome variables were log-transformed for all analyses. Beta values have been back-transformed.
Results of the multivariable models are shown in Table 4, including all variables that were entered. In the final model for facility-based yoga practice, higher yoga self-efficacy (p=0.004) and employment outside the home (p=0.004) were associated with greater class attendance. In the model for home-based yoga, higher waist circumference was marginally associated with less home yoga practice (p=0.05) and higher self-efficacy was marginally associated with more home practice (p=0.06).
Table 4.
Results of Multivariable Regression to Predict Adherence to Yoga (N=32)
| Variable | βa(95% CI) | p | |
|---|---|---|---|
| Class attendancea | Waist circumference (1-cm increase) | −1.49 (0.80, 2.75) | 0.62 |
| Self-efficacy (1-pt change) | 1.34 (1.04, 1.74) | 0.004 | |
| Work status (employed vs. not employed) | 1.94 (0.97, 3.88) | 0.004 | |
| Tumor stage (0 vs. I-IIIA) | 0.99 (0.95, 1.03) | 0.20 | |
| Home practicea | Waist circumference (cm) | −0.95 (0.91, 1.00) | 0.05 |
| Self-efficacy (1-pt change) | 1.29 (0.99, 1.69) | 0.06 |
Outcome variables were log-transformed for all analyses. Beta values have been back-transformed.
CI, confidence interval.
Discussion
This pilot study provides detailed adherence data from a 6-month randomized trial of yoga among breast cancer survivors and includes a quantitative analysis of predictors of adherence. The trial was notable both for the duration of the intervention, which is longer than those previously reported in this population, as well as the large amount of yoga that participants were asked to perform (5 days of yoga practice per week, including at least one facility-based class).
Consistent with a report of a 6-month yoga intervention among healthy older adults,32 it was found that demographic characteristics did not predict adherence. Perceived stress, fatigue, and social support were also not predictive of adherence. However, several easy-to-assess factors, including self-efficacy, waist circumference, and work status were predictive of class attendance and/or home practice.
The finding that self-efficacy for yoga was a significant or near-significant predictor of adherence to both supervised and home-based practice is supportive of similar results reported by Speed-Andrews et al.21 and lends credence to the utility of self-efficacy in the study of yoga adoption. The current results showing a nearly significant inverse association of waist circumference and adherence to home-based yoga are consistent with observational data showing that higher levels of obesity are associated with lower uptake of yoga among breast cancer survivors.33 Although the unadjusted association between higher waist circumference and lower class attendance was significant, waist circumference was not found to be predictive of class attendance in the final multivariable model.
The observation that employment outside the home was associated with better class attendance is likely due to the fact that two of the three classes were scheduled either early in the morning or early in the evening on a weekday. While convenient for women who worked outside the home, many retired or nonworking women found these times to be difficult as they required navigating rush-hour traffic. The associations reported in this study require replication in a larger and more diverse sample. They do, however, provide an initial guide for maximizing adherence in future studies. For example, programs could facilitate attendance by using self-efficacy assessments to identify those participants who may benefit from additional support and/or including specific intervention modules focused on improving self-efficacy. The lower observed adherence to home-based yoga among women with larger waist circumference is an interesting finding that may be related to physiologic factors (e.g., higher levels of joint pain from excess weight) and/or psychological factors (e.g., more difficulty with self-directed practice). Additional research is needed to better understand and address the specific issues related to yoga participation among obese women.
In contrast to others' findings,12,19,21 higher levels of fatigue were not associated with poorer adherence to either facility- or home-based yoga in our study. This may be due to differences in fatigue measure used, the type of yoga intervention, the study population, or other factors. Similar to the findings in the study by Speed-Andrews and colleagues, class attendance was associated with advanced tumor stage; however, this association weakened and was no longer statistically significant, after controlling for waist circumference, self-efficacy, and work status.
Strengths of this pilot study include the use and assessment of both supervised and home-based yoga, detailed adherence tracking including class sign-in sheets and daily logs of home practice, and an intervention that is longer than those previously reported in this population. The study also had several limitations. Similar to most other trials in this area, the current study had a relatively small sample size, limiting statistical power. Additionally, a relatively large number of factors were examined, so it is possible that some statistically significant associations were observed due to chance. The use of self-report logs to assess adherence to home-based yoga is subject to participant error or misrepresentation of the frequency of yoga practice. Finally, this sample was homogeneous in terms of ethnicity and education level, which reduced our ability to examine these factors as predictors of adherence.
Conclusions
Our study confirms and extends previous findings showing that both class-based and home-based yoga is feasible and well accepted among survivors of breast cancer. Useful topics for future study include adherence in interventions longer than 6 months, comparison of adherence to different types of yoga, and the use of larger samples to enable more powerful analyses of correlates of adherence.
Supplementary Material
Acknowledgments
We gratefully acknowledge the study participants; Laura Yon Brooks and Christy Fisher, for assistance designing the yoga protocol and teaching classes; Ann Enomoto, Lisa Yeager, and Linda Heuertz, for teaching classes. This work was supported by the National Cancer Institute's research grant U54 CA116847 and the Biobehavioral Cancer Prevention Training Program (R25CA92408).
Disclosure Statement
No competing financial interests exist.
References
- 1.Gold EB. Flatt SW. Pierce JP. Bardwell WA, et al. Dietary factors and vasomotor symptoms in breast cancer survivors: The WHEL Study. Menopause. 2006;13:423–433. doi: 10.1097/01.gme.0000185754.85328.44. [DOI] [PubMed] [Google Scholar]
- 2.Bower JE. Ganz PA. Desmond KA. Rowland JH, et al. Fatigue in breast cancer survivors: Occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 3.Burgess C. Cornelius V. Love S. Graham J, et al. Depression and anxiety in women with early breast cancer: Five year observational cohort study. BMJ. 2005;330:702. doi: 10.1136/bmj.38343.670868.D3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroenke CH. Chen WY. Rosner B. Holmes MD. Weight, weight gain, and survival after breast cancer diagnosis. J Clin Oncol. 2005;23:1370–1378. doi: 10.1200/JCO.2005.01.079. [DOI] [PubMed] [Google Scholar]
- 5.Erickson VS. Pearson ML. Ganz PA. Adams J, et al. Arm edema in breast cancer patients. J Natl Cancer Inst. 2001;93:96–111. doi: 10.1093/jnci/93.2.96. [DOI] [PubMed] [Google Scholar]
- 6.Oken BS. Zajdel D. Kishiyama S. Flegal K, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–47. [PMC free article] [PubMed] [Google Scholar]
- 7.Culos-Reed SN. Carlson LE. Daroux LM. Hately-Aldous S. A pilot study of yoga for breast cancer survivors: Physical and psychological benefits. Psychooncology. 2006;15:891–897. doi: 10.1002/pon.1021. [DOI] [PubMed] [Google Scholar]
- 8.Cohen L. Warneke C. Fouladi RT. Rodriguez MA, et al. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253–2260. doi: 10.1002/cncr.20236. [DOI] [PubMed] [Google Scholar]
- 9.Galantino ML. Desai K. Greene L. Demichele A, et al. Impact of yoga on functional outcomes in breast cancer survivors with aromatase inhibitor-associated arthralgias. Integr Cancer Ther. 2012;11:313–320. doi: 10.1177/1534735411413270. [DOI] [PubMed] [Google Scholar]
- 10.Banasik J. Williams H. Haberman M. Blank SE, et al. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23:135–142. doi: 10.1111/j.1745-7599.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- 11.Bower JE. Garet D. Sternlieb B. Yoga for persistent fatigue in breast cancer survivors: Results of a pilot study. Evid Based Complement Alternat Med. 2011;2011:623168. doi: 10.1155/2011/623168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danhauer SC. Mihalko SL. Russell GB. Campbell CR, et al. Restorative yoga for women with breast cancer: Findings from a randomized pilot study. Psychooncology. 2009;18:360–368. doi: 10.1002/pon.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Speed-Andrews AE. Stevinson C. Belanger LJ. Mirus JJ, et al. Pilot evaluation of an Iyengar yoga program for breast cancer survivors. Cancer Nurs. 2010;33:369–381. doi: 10.1097/NCC.0b013e3181cfb55a. [DOI] [PubMed] [Google Scholar]
- 14.Chandwani KD. Thornton B. Perkins GH. Arun B, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8:43–55. [PubMed] [Google Scholar]
- 15.Vadiraja HS. Rao MR. Nagarathna R. Nagendra HR, et al. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Complement Ther Med. 2009;17:274–280. doi: 10.1016/j.ctim.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 16.DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 17.Rao MR. Raghuram N. Nagendra HR. Gopinath KS, et al. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complement Ther Med. 2009;17:1–8. doi: 10.1016/j.ctim.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Carson JW. Carson KM. Porter LS. Keefe FJ, et al. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: Results from a randomized trial. Support Care Cancer. 2009;17:1301–1309. doi: 10.1007/s00520-009-0587-5. [DOI] [PubMed] [Google Scholar]
- 19.Moadel AB. Shah C. Wylie-Rosett J. Harris MS, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J Clin Oncol. 2007;25:4387–4395. doi: 10.1200/JCO.2006.06.6027. [DOI] [PubMed] [Google Scholar]
- 20.Smith KB. Pukall CF. An evidence-based review of yoga as a complementary intervention for patients with cancer. Psychooncology. 2009;18:465–475. doi: 10.1002/pon.1411. [DOI] [PubMed] [Google Scholar]
- 21.Speed-Andrews AE. Stevinson C. Belanger LJ. Mirus JJ, et al. Predictors of adherence to an Iyengar yoga program in breast cancer survivors. Int J Yoga. 2012;5:3–9. doi: 10.4103/0973-6131.91693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Littman AJ. Cadmus Bertram L. Ceballos R. Ulrich C, et al. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: Effects on quality of life and anthropometric measures. Supportive Care Cancer. 2012;20:267–277. doi: 10.1007/s00520-010-1066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ainsworth BE. Haskell WL. Whitt MC. Irwin ML, et al. Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 24.Taylor HL. Jacobs DR., Jr Schucker B. Knudsen J, et al. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 25.Buysse DJ. Reynolds CF., 3rd Monk TH. Berman SR, et al. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S. Williamson G. Spacapan S. Oskamp S. The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988. Perceived stress in a probability sample of the United States. [Google Scholar]
- 27.Cohen S. Kamarck T. Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 28.Cella D. Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System Center on Outcomes, Research and Education (CORE), Version 4. Evanston Northwestern Healthcare and Northwestern University; 1997. [Google Scholar]
- 29.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Psycholog Measur. 1977;1:385–401. [Google Scholar]
- 30.Bandura A. Guide for creating self-efficacy scales. Self-Efficacy Beliefs of Adolescents. In: Pajares F, editor; Urdan T, editor. Vol. 2006. Information Age Publishing; pp. 307–337. [Google Scholar]
- 31.Kraftsow G. Penguin Books; 1999. Yoga for Wellness: Healing with the Timeless Teachings of Viniyoga. [Google Scholar]
- 32.Flegal KE. Kishiyama S. Zajdel D. Haas M, et al. Adherence to yoga and exercise interventions in a 6-month clinical trial. BMC Complement Altern Med. 2007;7:37. doi: 10.1186/1472-6882-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desai K. Bowman MA. Galantino ML. Hughes-Halbert C, et al. Predictors of yoga use among patients with breast cancer. Explore. 2010;6:359–363. doi: 10.1016/j.explore.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.