Abstract
Background
Measures for pain management after total hip arthroplasty (THA) are important for early improvement in the quality of life after operation and early postoperative rehabilitation. We investigated the analgesic effect of locally injected drugs around the total hip prosthesis.
Methods
54 patients undergoing THA were randomized either to receive a periarticular intraoperative injection of a 30-ml mixture containing morphine hydrochloride 10 mg, 0.5% bupivacaine 20 ml, epinephrine 0.3 mg, and saline 8.7 ml or to receive no injection. The perioperative analgesic regimen was standardized. The evaluation items included assessment of pain using a 100-point visual analog scale (VAS) after the patients awoke on the day of the operation and on postoperative day 1, the dose of diclofenac sodium suppository, the number of days for acquiring assisted ambulation with a walking cane, and side effects.
Results
The VAS score on the day of the operation was significantly low in the injection group. No cardiac or central nervous system toxicity was observed.
Conclusions
Intraoperative periarticular injection with multimodal drugs can significantly reduce pain on the day of the operation, with no apparent risks, following THA.
Keywords: Pain control, Total hip arthroplasty, Periarticular injection
1. Introduction
Total hip arthroplasty (THA) is associated with considerable postoperative pain. Measures for pain management after THA are important for early improvement in the quality of life after operation and early postoperative rehabilitation, and these measures are as follows: continuous epidural anesthesia, continuous femoral nerve block, and intraarticular injection. Epidural analgesia is of proven benefit but is associated with side effects such as spinal headache, neurogenic bladder, hypotension, respiratory depression, pulmonary hypertension, cardiac decompensation, and a risk of spinal infection.1 Continuous infusion of opioids and bupivacaine into the femoral nerve may be associated with prolonged wound drainage.2 We controlled the pain around the surgical wounds that the patients experienced immediately after surgery by intraoperative administration of a periarticular multimodal drug cocktail injection comprising a solution containing several drugs. The purpose of this study was to examine the usefulness of a periarticular multimodal drug cocktail l injection for pain management in THA.
2. Materials and methods
Our prospective study involved 54 patients undergoing unilateral THA, including 11 men and 43 women. We randomly divided the patients into 2 groups: a multimodal drug cocktail injection group and a non-injection group. All they had written informed consent. Exclusion criteria were major psychological problems, previous drug dependency, allergies to any of the ingredients of the injection, renal insufficiency, abnormal liver enzymes, a history of stroke or a major neurological deficit, or uncontrolled angina and bifascicullar blocks with prolonged QT intervals. The multimodal drug cocktail injection group comprised 5 men and 23 women, with a mean age of 65.7 years. Among these patients, 24 had osteoarthritis of the hip, 4 had osteonecrosis of the femoral head. The non-injection group consisted of 6 men and 20 women with a mean age of 65.7 years. Among these patients, 23 had osteoarthritis of the hip, 3 had osteonecrosis of the femoral heads. The multimodal drug cocktail injection group received a periarticular injection of a 30-ml mixture containing morphine hydrochloride 10 mg, 0.5% bupivacaine 20 ml, epinephrine 0.3 mg, and saline 8.7 ml. Operative anesthesia was all general and anesthesia regimen was standardized. We performed the operation through an anterolateral approach developing the interval between the tensor fasciae latae muscle and gluteus medius muscle using minimum invasive instruments.3 The evaluation items included assessment of pain using a 100-point visual analogue scale (VAS) after the patients awoke on the day of the operation and on postoperative day 1, the dose of diclofenac sodium suppository, the number of days for acquiring assisted ambulation with a walking cane, and side effects. Chi-square test and analysis of variance were used for statistical testing, and the level of significance was set at P < 0.05 (Table 1).
Table 1.
Patient characteristics.
| Objectives | Cocktail injection group | Control group |
|---|---|---|
| No of patients | 28 | 26 |
| Male/Female | 5/23 | 6/20 |
| Average age | 65.7 ± 11.7 | 65.7 ± 9.0 |
| Osteoarthritis of the hip | 24 | 23 |
| Osteonecrosis of the femoral head | 4 | 3 |
3. Results
The multimodal drug cocktail injection group had a mean VAS score of 38.1 points after awakening on the day of the operation and 33.0 points on postoperative day 1. The non-injection group had a mean VAS score of 58.3 points after awakening on the day of the operation and 35.0 points on the postoperative day 1. The VAS score on the day of the operation was significantly low in the injection group, but that on postoperative day 1 was not significantly different between the 2 groups. Moreover, the dose of diclofenac sodium suppository on the day of the operation and on postoperative day 1 and the number of days for acquiring assisted ambulation with a walking cane were not significantly different between the 2 groups. Side effects included nausea in 12 of the 28 patients in the cocktail injection group and in 3 of the 26 patients in the non-injection group. There were no cases of delayed wound healing, prolonged wound drainage, or wound infections. There were no cases of deep vein thrombosis, and no cardiac or central nervous system toxicity was observed (Fig. 1 and Table 2).
Fig. 1.
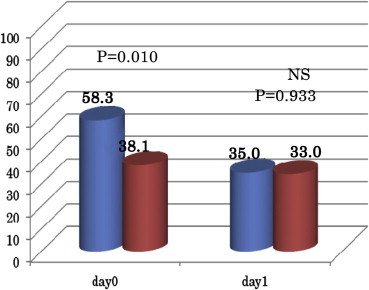
VAS average.
Table 2.
Dosage of diclofenac sodium suppository.
| Cocktail group | Control group | ||
|---|---|---|---|
| POD 0 | 28.8 mg | 22.3 mg | NS P = 0.385 |
| POD 1 | 22.1 mg | 29.5 mg | NS P = 0.334 |
4. Discussion
In the present study, the VAS score on the day of the operation was significantly lower in the multimodal drug cocktail injection group than in the non-injection group, but that on postoperative day 1 was not significantly different between the 2 groups. Moreover, no significant difference was observed in the dose of postoperative analgesics administered after the operation and the number of days required for acquiring assisted ambulation with a walking cane between the 2 groups. According to a report by Andersen, et al., injection of ropivacaine and ketorolac immediately after surgery and 24 h after surgery improved pain for up to 2 weeks after the operation.4 Although our study indicated no significant difference in pain improvement on postoperative day 1 between the 2 groups, the administration methods, drugs, evaluation items, and evaluation time should be reconsidered. Some patients had nausea as a side effect. The mechanism of occurrence of nausea due to morphine involves a complicated mechanism of the autonomous nervous system because of the stimulating action of morphine on the vomiting center in the floor of the fourth ventricle. Prochlorperazine, a centrally acting drug, and metoclopramide which enhances the gastrointestinal function as well as has a central action, are useful as antiemetic drugs.5 In this study, however, nausea occurred in 6 out of the 12 patients in the non-prochlorperazine treatment group and in 6 out of the 16 patients in the prochlorperazine treatment group. Thus, measures against nausea and vomiting are required to be considered in future studies (Table 3).
Table 3.
The day until T-cane gait.
| Cocktail group | Control group | ||
|---|---|---|---|
| Days | 10.5 | 8.8 | NS P = 0.490 |
5. Conclusion
VAS score on the day of the operation was significantly low in the multimodal drug cocktail injection group. Measures against nausea and vomiting should be considered in the future.
Conflicts of interest
All authors have none to declare.
References
- 1.Mahoney O.M., Noble P.C., Davidson J., Tullos H.S. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total hip knee arthroplasty. Clin Orthop Relat Res. 1990;260:30–37. [PubMed] [Google Scholar]
- 2.Deweese F.T., Akbari Z., Carline E. Pain control after knee: intraarticular versus epidural anesthesia. Clin Orthop Relat Res. 2001;392:226–231. doi: 10.1097/00003086-200111000-00028. [DOI] [PubMed] [Google Scholar]
- 3.Nakai T., Kakiuchi M. Minimally invasive anterolateral total hip arthroplasty on a standard operative table using a two-tined retractor and a double offset broach handle. J Orthop. 2009;6(3):e10. [Google Scholar]
- 4.Andersen L.J., Poulsen T., Krogh B., Nielsen T. Postoperative analgesia in total hip arthroplasty: A randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop. 2007;78(2):187–192. doi: 10.1080/17453670710013663. [DOI] [PubMed] [Google Scholar]
- 5.Gan T.J., Meyer T., Apfel C.C. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71. doi: 10.1213/01.ane.0000068580.00245.95. [DOI] [PubMed] [Google Scholar]


