Recurrent vertigo is one of the most common and incapacitating complaints reported by patients in a clinical ENT practice. Numerous pathologic diseases can result in vertigo, with or without associated auditory and neurologic symptoms. In 1952, Dix and Hallpike identified vestibular neuronitis (or neuritis) as an association of characteristic signs occurring predominantly in middle age and composed of a sudden severe and prolonged vertigo, with reduced or absent caloric response in 1 ear and preceded or concomitant to an upper respiratory tract infection (1). The presence of any auditory or neurologic symptoms would point to a differential diagnosis such as Ménière’s disease, a cerebellar infarction, or an acoustic tumor.
Inflammation has long been thought to be the cause of vestibular neuronitis. However, several temporal bone evaluations have shown histologic changes, which are suggestive of a viral herpetic infection. Moreover, the common association with an upper respiratory infection and the anatomical proximity of the meatal and vestibular ganglions to the upper respiratory tract provides support for the virus theory. After the first contact with a neurotropic virus, the human body cannot rid itself of it, and the virus will remain latent in the ganglion cells, waiting for a reactivation. The contiguity of the meatal and vestibular ganglions can explain, in some cases, the movement of the virus from the meatal ganglion, in the fundal segment of the facial nerve, to the vestibular nerve but not the auditory nerve owing to the lack of continuity of the two. Thus, the neurotropic viruses can spread after an anterograde flow, so that hearing loss does not occur (2).
CASE REPORT
A 96-year-old woman with a 65-year history of tinnitus and progressive hearing loss due to otosclerosis reported 2 sudden unprovoked attacks of vertigo, 42 and 26 years before her death. During these episodes, no auditory symptoms were reported, and the recovery was complete over several days. She had also undergone stapes surgery on both ears. Histological findings of an atrophic superior nerve and ganglion and the history of a dizzy spell 26 years before death suggest vestibular neuronitis.
HISTOPATHOLOGY
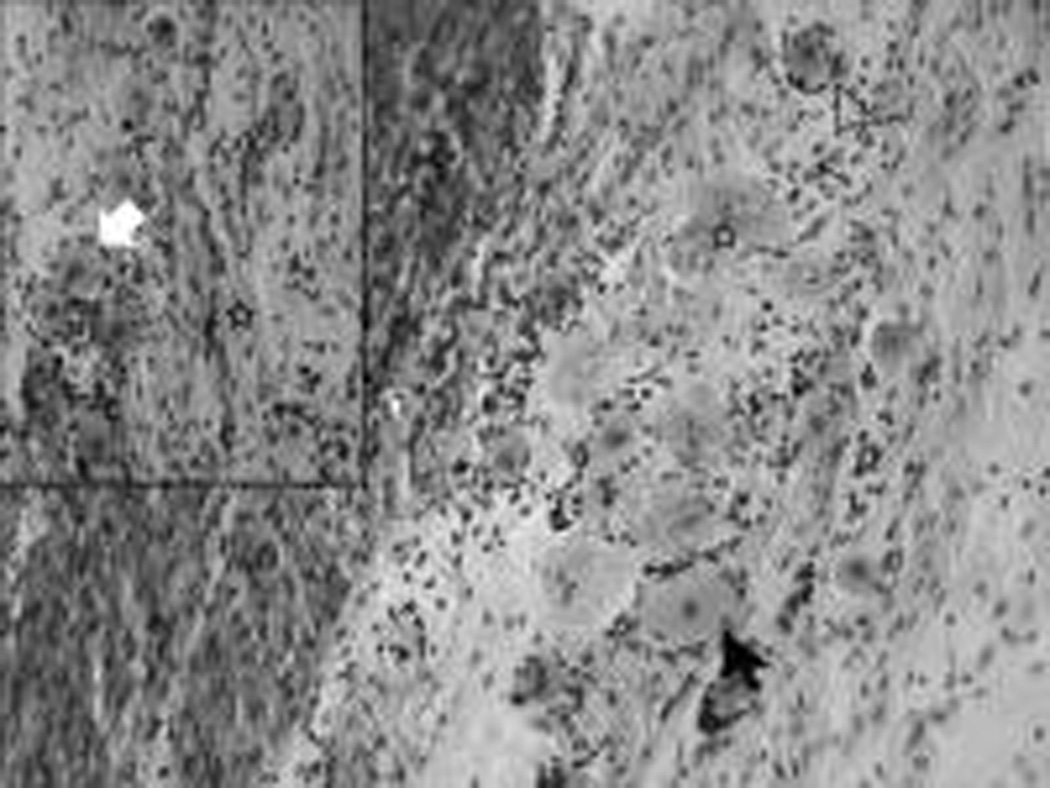
The right superior vestibular nerve is devoid of most of its neurites, with paler and smaller ganglion than those of the inferior nerve (Fig. 1). These degenerated cells are replaced by a material that has been previously described as a collagen-like material (2) (Fig. 2).
Fig 1.

Fig 2.
Acknowledgments
This study was supported by Grant U 24 DC 011962 HO 1 from the National Institutes of Health and Perspectives ORL 2010 from décerné avec le soutien de Sanofi-aventis.
Footnotes
The authors disclose no conflicts of interest.
REFERENCES
- 1.Dix M, Hallpike C. The pathology, symptomatology, and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol. 1952;61:987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- 2.Gacek RR, Gacek MR. Viral neuropathies in the temporal bone [review] Adv Otorhinolaryngol. 2002;60:VII–IX. doi: 10.1159/isbn.978-3-318-00764-0. [DOI] [PubMed] [Google Scholar]


