Abstract
BACKGROUND
Pauses in chest compressions during cardiopulmonary resuscitation have been shown to correlate with poor outcomes. In an attempt to minimize these pauses, the American Heart Association recommends charging the defibrillator during chest compressions. While simulation work suggests decreased pause times using this technique, little is known about its use in clinical practice.
METHODS
We conducted a multicenter, retrospective study of defibrillator charging at three US academic teaching hospitals between April 2006 and April 2009. Data were abstracted from CPR-sensing defibrillator transcripts. Pre-shock pauses and total hands- off time preceding the defibrillation attempts were compared among techniques.
RESULTS
A total of 680 charge-cycles from 244 cardiac arrests were analyzed. The defibrillator was charged during ongoing chest compressions in 448 (65.9%) instances with wide variability across the three sites. Charging during compressions correlated with a decrease in median pre-shock pause [2.6 (IQR 1.9–3.8) vs 13.3 (IQR 8.6–19.5) s; p < 0.001] and total hands-off time in the 30 s preceding defibrillation [10.3 (IQR 6.4–13.8) vs 14.8 (IQR 11.0–19.6) s; p < 0.001]. The improvement in hands-off time was most pronounced when rescuers charged the defibrillator in anticipation of the pause, prior to any rhythm analysis. There was no difference in inappropriate shocks when charging during chest compressions (20.0 vs 20.1%; p=0.97) and there was only one instance noted of inadvertent shock administration during compressions, which went unnoticed by the compressor.
CONCLUSIONS
Charging during compressions is underutilized in clinical practice. The technique is associated with decreased hands-off time preceding defibrillation, with minimal risk to patients or rescuers.
Keywords: Heart arrest, Cardiopulmonary resuscitation, Defibrillation, Chest, compression
INTRODUCTION
Despite international resuscitation guideline recommendations to minimize chest compression interruptions, cardiopulmonary resuscitation (CPR) in clinical practice is often performed with long and frequent pauses in chest compressions.1–3 These pauses have been shown to correlate with poor outcomes in both animal and clinical studies.4–8 Pauses are particularly detrimental in the time period immediately preceding defibrillation, where prolonged pre-shock pauses have been shown to correlate with defibrillation failure, right ventricular congestion, and decreased rates of return of spontaneous circulation (ROSC) and survival.9–12
In contrast to the European Resuscitation Council (ERC), the American Heart Association (AHA) recommended in 2005 that rescuers resume chest compressions while charging the defibrillator to minimize these pauses.13–15 A mannequin study comparing the two methods demonstrated significantly shorter pre-shock pause durations when utilizing the AHA method of charging concurrently with chest compressions.16 However, participants in this simulation study who utilized the AHA method stated that they felt less safe compared to the ERC method of pausing compressions to charge the defibrillator.
We sought to determine the compliance with this AHA recommendation in three US hospitals and to measure the impact on peri-shock pause duration. In addition, we sought to test the safety of charging during defibrillation by assessing for inadvertent shocks to rescuers and inappropriate shocks to patients.
METHODS
We conducted a multi-center, retrospective study at three US academic teaching hospitals. Approval was granted by the Institutional Review Boards of each participating hospital. Consecutive in-hospital cardiac arrests in which a CPR-sensing monitor/defibrillator (Heartstart MRx, Philips Healthcare, Andover, MA) was used were included if there was at least one instance of defibrillator charging during the resuscitation attempt.
Transcripts from all cardiac arrests at each site between April 2006 and April 2009 were downloaded from the defibrillators by study personnel and analyzed using custom software (QCPR Review, Laerdal Medical, Stavanger, Norway and Matlab, Mathworks, Natick, MA) for any instance in which the defibrillator was charged during a resuscitation attempt. Each charge-cycle was entered into the study database as an individual entry, with some transcripts containing multiple charge-cycles. Charge-cycles were excluded if chest compression data were missing. Cardioversions of perfusing tachycardias were also excluded.
Pre-shock pauses were measured from the end of the last chest compression to the time of defibrillation and post-shock pauses were measured from the time of defibrillation to resumption of chest compressions. Total hands-off time, during which no chest compressions were being administered, was calculated by adding the pre-shock pause to any other pauses in compression during the 30s preceding shock delivery. Cardiac rhythms at the time of shock delivery were confirmed manually by study investigators (DPE, DW). Shocks were deemed inappropriate if delivered for any rhythm other than ventricular fibrillation (VF) or ventricular tachycardia (VT). If a transcript included audio data, it was reviewed to determine whether any rescuers were inadvertently shocked.
Analysis of audio data was supplemented by review of resuscitation documentation forms. Patient demographics and outcomes were obtained from clinical records at each site.
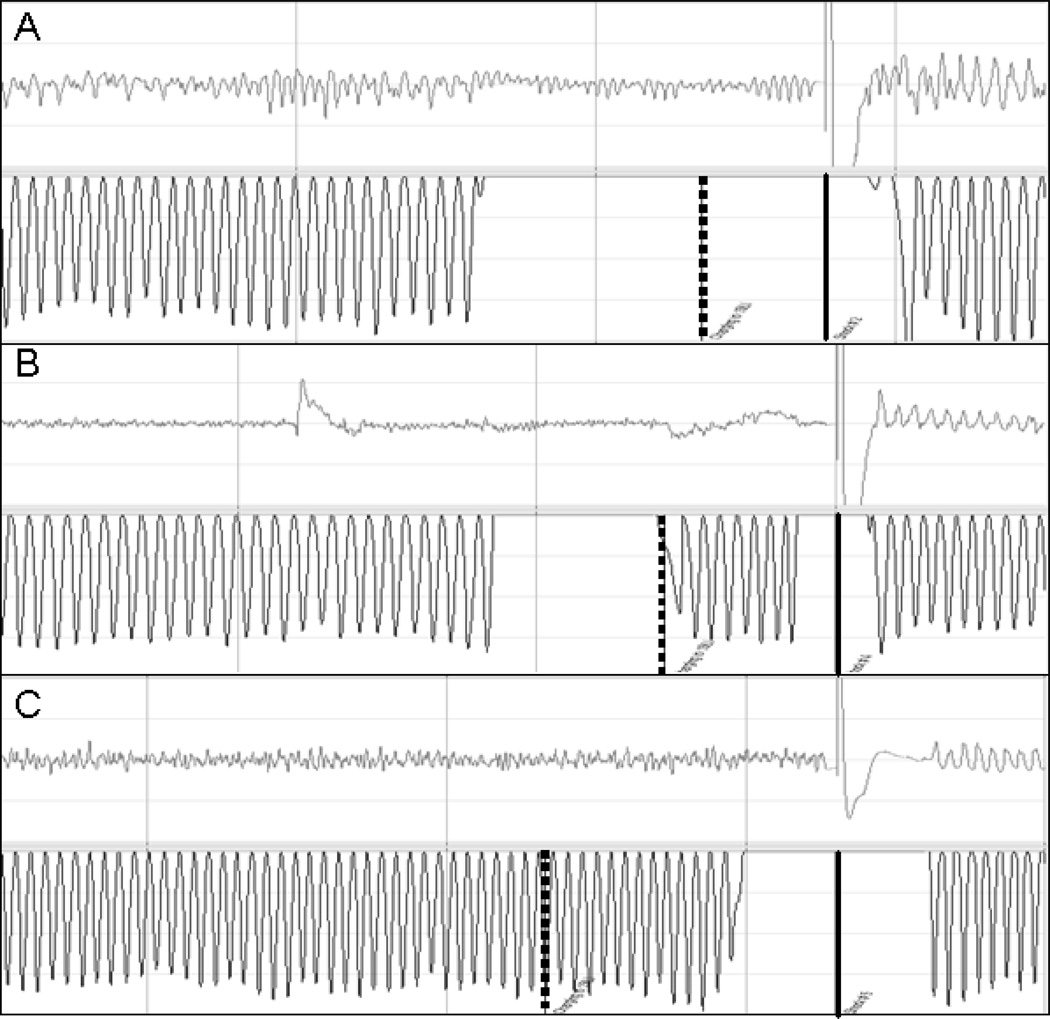
Transcripts were manually reviewed to determine the sequence of defibrillator charging (Figure 1). Charging during compressions was noted to take two different forms. In the first method (the one currently recommended by the AHA), rescuers complete a CPR cycle, pause to analyze the rhythm and then resume chest compressions while charging.13 In the second method, rescuers charge the defibrillator near the end of the compression cycle (in anticipation of a potentially shockable rhythm but prior to actually analyzing the rhythm) and then pause to analyze and either shock or resume CPR if the rhythm is deemed not shockable. In the latter instance, the defibrillator is disarmed either manually, by a rescuer, or automatically, by the defibrillator after 30 seconds.
FIGURE 1. Examples of charging techniques.
Each tracing displays 18 seconds of a resuscitation, involving a defibrillation attempt, with the electrocardiograph waveform above and the accelerometer tracing showing compressions below. The vertical dashed lines represent charge initiation and the solid lines represents shock delivery. (A) Pause to charge technique: compressions are held to analyze, charge and shock; (B) Charging during compression (American Heart Association method): compressions are held to analyze the rhythm, resumed briefly to charge, and then held again to deliver the shock; (C) Charging during compression (anticipatory method): the defibrillator is charged at the end of the compression sequence, without analyzing the rhythm, and then compressions are paused to analyze and shock.
Resuscitation care is supervised by physicians certified in Advanced Cardiovascular Life Support (ACLS) with assistance from respiratory technicians, nurses, and medical students at each of the three sites. Two of the sites (A and B) have physician champions who train the rescuers at their institutions, and specifically stress the minimizing of pre- shock pauses and the importance of charging during ongoing chest compressions.17 Site C does not specifically stress the technique but many of the physician rescuers are members or graduates of the Site A training program.
All calculations were performed using a statistical software application (Stata Version 10.0, Statacorp, College Station, TX). Each charge cycle was treated independently. Normally distributed variables were described using means and standard deviations and skewed data, such as times, were described in terms of medians with interquartile ranges. Categorical variables were compared via chi-squared analysis. Analysis of variance was used to compare mean age, as well as charges and shocks per resuscitation across the sites. Linear regression was used to adjust for potential confounding by individual resuscitation, hospital, cardiac arrest location, time of day, shock number, and presence of a shockable rhythm. Significance was set at p < 0.05 for all values. As this manuscript represents a post-hoc study of a collected data set, there were no interim analyses and all charge-cycles which met inclusion criteria were analyzed.
RESULTS
A total of 680 charge-cycles from 244 in-hospital cardiac arrests involving 225 distinct patients were examined. Patient and arrest demographics are described in Table 1 for each of the three sites. The sites were similar with respect to patient sex, time of arrest and arrest outcomes but significantly different from one another with regard to patient age, race, and arrest location.
Table 1.
Baseline characteristics
| Site A | Site B | Site C | p value | |
|---|---|---|---|---|
| Patients, n | 153 | 35 | 37 | N/A |
| Male sex, n/total (%) | 78/153 (51.0) | 20/35 (57.1) | 22/37 (59.5) | 0.58 |
| Race, n/total (%) | 0.002 | |||
| Black | 87/153 (56.9) | 13/35 (37.1) | 9/37 (24.3) | |
| White | 44/153 (28.8) | 15/35 (42.9) | 23/37 (62.2) | |
| Hispanic | 5/153 (3.3) | 0/35 (0.0) | 3/37 (8.1) | |
| Asian | 2/153 (1.3) | 1/35 (2.9) | 1/37 (2.7) | |
| Other/unknown | 15/153 (9.8) | 6/35 (17.1) | 1/37 (2.7) | |
| Age, mean (SD), years | 59.3 (16.2) | 61.9 (17.5) | 67.5 (20.2) | 0.03 |
| Arrests, n | 164 | 37 | 43 | N/A |
| Time of day, n/total (%) | 0.08 | |||
| 7am–3pm | 45/164 (27.4) | 19/37 (51.4) | 13/43 (30.2) | |
| 3pm–11pm | 49/164 (29.9) | 9/37 (24.3) | 12/43 (27.9) | |
| 11pm–7am | 70/164 (42.7) | 9/37 (24.3) | 18/43 (41.9) | |
| Location, n/total (%) | <0.001 | |||
| ICU | 109/164 (66.5) | 20/37 (54.1) | 23/43 (53.5) | |
| Ward | 47/164 (28.7) | 3/37 (8.1) | 17/43 (39.5) | |
| Other | 8/164 (4.9) | 14/37 (37.8) | 3/43 (7.0) | |
| Total charges, n | 471 | 104 | 105 | N/A |
| Charges per resuscitation, median (range), n | 2 (1–14) | 3 (1–11) | 2 (1–11) | 0.66 |
| Total shocks, n | 369 | 93 | 100 | N/A |
| Shocks per resuscitation, median (range), n | 2 (1–13) | 3 (1–11) | 2 (1–11) | 0.22 |
| ROSC, n/total (%) | 74/164 (45.1) | 17/35 (48.6) | 22/40 (55.0) | 0.53 |
| Survival to discharge, n/total (%) | 18/153 (11.8) | 4/35 (11.4) | 2/37 (5.4) | 0.53 |
SD, standard deviation; ICU, intensive care unit; ROSC, return of spontaneous circulation.
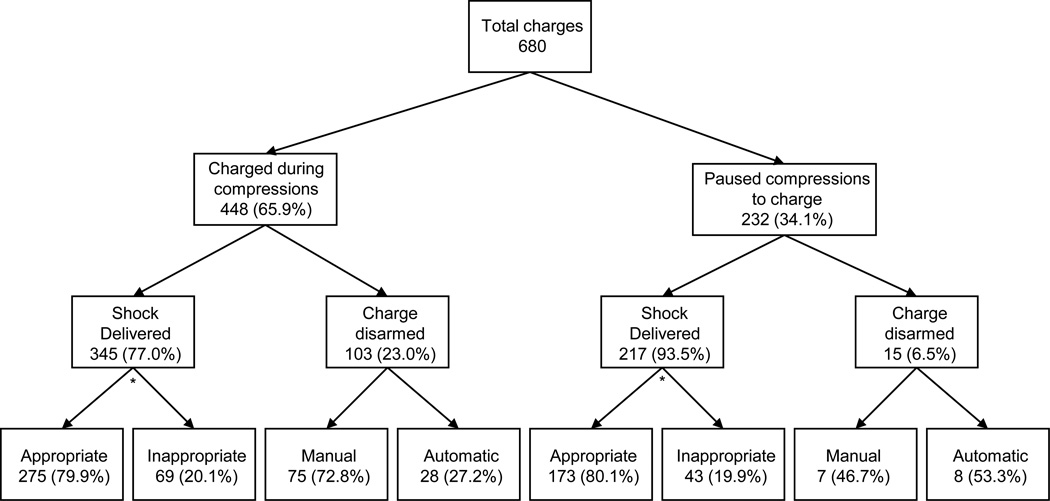
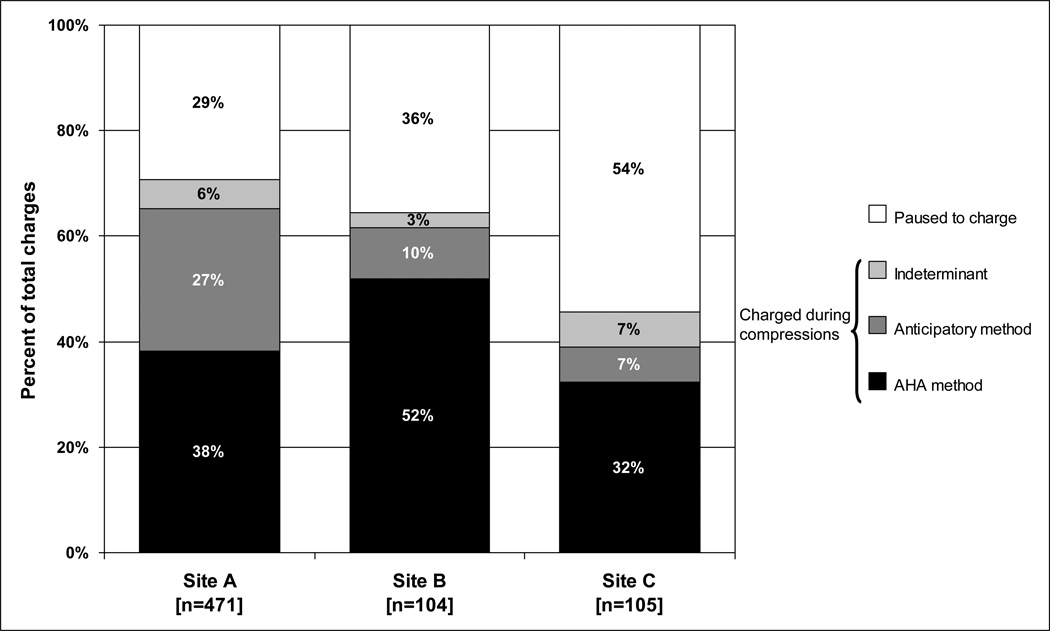
The flow diagram for included charge-cycles is shown in Figure 2. Rescuers charged the defibrillator during ongoing chest compressions in 65.9% of all charge-cycles. However, there was significant variance in the use of the technique between the three sites, with a range of 45.7% in Site C to 70.7% in Site A (Figure 3). Shocks were delivered in 562 (82.6%) of the 680 charge cycles. The remaining 118 charge cycles were disarmed either manually by the rescuers (69.5%) or automatically by the defibrillator (30.5%). Of the 562 shocks, 112 (20.0%) were deemed inappropriate, having been delivered for PEA (n=100), asystole (n=9), or perfusing rhythms (n=3). The defibrillator was disarmed most often in response to PEA (92/118; 78.0%). However, in 16 instances, the charge was disarmed in the presence of a shockable rhythm.
FIGURE 2. Flowchart of included charge cycles.
Shocks were deemed inappropriate if delivered for any rhythm other than ventricular fibrillation or ventricular tachycardia. *Rhythm could not be analyzed prior to shock in two cases, and therefore appropriate and inappropriate shocks do not sum to shock delivered totals.
FIGURE 3. Hospital variation in utilization of different charging techniques.
P < 0.001 for the differences. AHA; American Heart Association.
Charging during compressions was associated with a significant decrease in measured pause times (Table 2). There was no difference in compression depth between the two techniques but the rate of compressions was higher for the group that charged during compressions [109±11 vs 106±12/min; p=0.002]. Median pre-shock pause time decreased from 13.3 s (IQR 8.6–19.5 s) to 2.6 s (IQR 1.9–3.8 s) when rescuers charged during compressions (p < 0.001). This technique also correlated with a significant decrease in total hands-off time in the 30 s preceding defibrillation [14.8 (IQR 11.0–19.6) vs 10.3 (IQR 6.4–13.8) s; p < 0.001]. After adjusting for potential confounders, including clustering at the level of the patient, charging during chest compressions was associated with a 13.1 s decrease in pre-shock pause and 5.1s decrease in total hands-off time in the 30 s preceding defibrillation.
Table 2.
Effect of charging during compressions on pause times and inappropriate shocks
| All [n=562] |
Pause to Charge [n=217] |
Charging During Compressions [n=345] |
p value |
|
|---|---|---|---|---|
| Compression depth prior to shock†, mean (SD), mm | 47.3 (10.3) | 47.1 (10.6) | 47.3 (10.0) | 0.81 |
| Compression rate prior to shock†, mean (SD), /min | 108 (11) | 106 (12) | 109 (11) | 0.002 |
| Pre-shock pause, median (IQR), s | 3.8 (2.2–10.0) | 13.3 (8.6–19.5) | 2.6 (1.9–3.8) | <0.001* |
| Post-shock pause, median (IQR), s | 2.0 (1.4–3.0) | 2.3 (1.7–3.9) | 1.9 (1.3–2.7) | 0.01* |
| Hands-off time 30s preceding shock, median (IQR), s | 11.7 (8.1–16.3) | 14.8 (11–19.6) | 10.3 (6.4–13.8) | <0.001* |
| Inappropriate shocks‡, n/total (%) | 112/560 (20.0) | 43/216 (20.0) | 69/344 (20.1) | 0.97 |
| Shocks to rescuers, n/total (%) | 1/562 (0.2) | 0/217 (0.0) | 1/345 (0.3) | 0.43 |
IQR, interquartile range
Adjusted for individual resuscitation, hospital, cardiac arrest location, time of day, shock number, and presence of a shockable rhythm.
There was no compression data prior to shock in 17 pause-to-charge cases. Compression depth could not be analyzed in two additional cases, and compression rate could not be analyzed in one additional case.
Rhythm could not be analyzed prior to shock in two cases.
There was only one incident where a shock was delivered while a rescuer was actively performing chest compressions. However, the compression transcript continued without any visible change to CPR administration, suggesting that the rescuer was unaffected by the event. Review of clinical records and audio transcripts revealed no evidence of inadvertent shocks to rescuers. In addition, there was no significant difference in the incidence of inappropriate shocks to patients associated with charging during compressions (20.0% vs 20.1%; p=0.97).
Of the 345 instances of charging during compressions which were followed by a shock, 255 used the AHA recommended method of analyzing the rhythm then resuming compressions to charge, while 67 used the anticipatory charging method (Figure 1). In 23 cases the charging scheme could not be determined. Table 3 shows that while the two methods had similarly short pre-shock pauses (median 2.5 s vs 3.8 s; p=0.08) the total pause times in the 30 s preceding defibrillation was significantly longer when the AHA method was employed [11.5 (IQR 9.1–14.5) vs 3.9 (2.4–5.6) s; p < 0.001]. There was no significant difference between charging during compressions and anticipatory charging in terms of compression depth or compression rate. These differences were not associated with any increase in inappropriate shocks to patients but the one shock administered during chest compressions occurred in a case of anticipatory charging.
Table 3.
Effect of method of charging during compressions on pause times and inappropriate shocks
| Charging During Compression (AHA Recommended) [n=255] |
Charging During Compression (Anticipatory) [n=67] |
p value | |
|---|---|---|---|
| Compression depth prior to shock, mean (SD), mm | 47.6 (9.9) | 46.5 (9.1) | 0.41 |
| Compression rate prior to shock, mean (SD), /min | 109 (11) | 108 (11) | 0.42 |
| Pre-shock pause, median (IQR), s | 2.5 (1.8–3.3) | 3.8 (2.4–5.4) | 0.08* |
| Post-shock pause, median (IQR), s | 1.7 (1.3–2.5) | 2.2 (1.6–3.5) | 0.39* |
| Hands-off time 30s preceding shock, median (IQR), s | 11.5 (9.1–14.5) | 3.9 (2.4–5.6) | <0.001* |
| Inappropriate shocks, n/total (%) | 45/255 (17.7) | 13/67 (19.4) | 0.74 |
| Shocks to rescuers, n/total (%) | 0/255 (0.0) | 1/67 (1.5) | 0.05 |
IQR, interquartile range.
Adjusted for individual resuscitation, hospital, cardiac arrest location, time of day, shock number, and presence of a shockable rhythm.
DISCUSSION
We have demonstrated that defibrillator charging during on-going chest compressions is safe and associated with decreased hands-off time prior to defibrillation during actual in- hospital resuscitations. However, the employment of this strategy varied considerably among the three hospitals we studied, despite AHA guidelines recommending its use.13
Interruptions in chest compressions have been shown to result in poor outcomes in both clinical and animal settings.4–12, 18, 19 In the current study, charging during compressions decreased median pre-shock pause by over 10 s, which previous studies suggest could have a dramatic effect on clinical outcomes. We previously reported an almost two-fold increase in the chances of successful defibrillation for every 5 s reduction in the pre- shock pause.9 Similarly, Eftestøl et al found that a 10 s hands-off period prior to defibrillation would roughly halve the probability of obtaining ROSC.6
This study supports prior work by Perkins and colleagues in a simulated setting.16 In that study, the authors found a decrease in pre-shock pause from 7.0 s to 0.9 s and a decrease in total pause time from 7.0 s to 3.8 s when charging during compressions using a hands-free set-up, the method of defibrillation at all three of our sites. Both the pauses and the decreases identified in the current study are greater, however Perkins speculated that their results, derived in mannequins, could underestimate the length of pre-shock pauses during actual resuscitations. Our findings are consistent with that hypothesis.
Though the 2005 guidelines of the AHA and ERC both repeatedly stress the minimization of hands-off time, only the AHA specifically recommends charging during compressions: “When a rhythm check reveals VF/VT, rescuers should provide CPR while the defibrillator charges (when possible), until it is time to ‘clear’ the victim for shock delivery.”20 However, this is the only written mention of the technique in the entirety of the AHA guidelines and the point is not emphasized in the training materials. As such, it may be easily overlooked.
Interestingly, we found that the most efficient technique with regard to minimizing pauses was not the AHA recommended method of pausing to analyze, resuming CPR to charge, and then pausing again to defibrillate. Rather, charging at the end of every 2 minute CPR cycle in anticipation of a shockable rhythm and then pausing only once, briefly, to both analyze and either shock or disarm was associated with significantly shorter total pause duration in the thirty seconds preceding defibrillation.
An important criticism of charging during compressions involves concerns over the safety of the technique. In the Perkins study, rescuers rated the AHA technique of charging during compression to be significantly (p=0.001) less safe than the ERC method of pausing once to analyze, charge and shock. However, several recent studies suggest that these fears may be exaggerated. In a systematic review, Hoke et al summarized 29 reports of accidental defibrillator discharges, of which only 15 occurred during resuscitation attempts.21 Symptoms included tingling sensations, discomfort, and minor burns, but no long term effects or major consequences were reported. In another study, Lloyd and colleagues suggested that as long as polyethylene gloves are worn, it is possible for CPR to be continued even during the moment of defibrillation.22 Rescuers in this clinical investigation experienced a mean leakage current of 283±140 microamperes from 36 reported shocks, a value below the International Electrotechnical Commission standard for leakage current of 500 microamperes.23 Our study found only one incident of a defibrillator being discharged prior to fully clearing the field. The rescuer performing chest compressions at the instant the shock was delivered did not recoil in response to the voltage and no pause in chest compressions occurred following the shock, suggesting that it went unnoticed by that rescuer, which would support the Lloyd findings. Also, despite shortening the pre-shock pause and therefore rhythm analysis time, we found no evidence to support the risk of inappropriate shock decisions by rescuers. This study has prompted debate over whether a pause to defibrillate is even necessary. 24, 25
There are several important limitations to our study. First, we were unable to assess the effect that charging during compressions had on patient or even shock outcomes. Inclusion of multiple charge-cycles per arrest, as well as per patient, limited the ability of each charge cycle to be an independent predictor of ROSC and survival. The surrogate marker of shock success (ie removal of VF for five seconds following defibrillation) could also not be reliably ascertained.9, 26–28 Due to the very short post-shock pauses in this study, only 56 shocks had post-shock pauses that were at least 5 s long, enabling assessment of shock success. We attempted to resolve this issue by developing a metric of the “shock success at next pause.” However, an unadjusted analysis showed no significant difference between the two study groups in terms of this metric (data not shown). In addition, the validity of such a measure has yet to be tested in the clinical setting and the length of elapsed time between shock delivery and the next pause was highly variable. We also attempted to use a previously described compression artifact filtering algorithm to look at shock success in the 5 s following a shock regardless of when chest compressions resumed.29 However, we found that the fidelity of the technique was not sufficient for our analysis.
Our study was also limited in that it was observational in nature and did not represent a randomized controlled trial of charging during compressions. Finally, although it was a multi-center study, these sites may not be representative of hospitals in general since the sites were chosen for inclusion based on their use of CPR-sensing defibrillators, indicating an institutional valuing of CPR quality. In addition, rescuers at all three sites received additional resuscitation education, beyond ACLS certification, with added focus on CPR quality. Although the technique of charging during compressions is emphasized most at site A, all three receive some instruction to do the same. Therefore, it is likely that other institutions lacking the benefit of similar training and emphasis charge during compressions at significantly lower rates, if at all. Furthermore, these other institutions may also have a higher incidence of inappropriate shocks than the roughly 20% reported in our study.
CONCLUSIONS
Charging during compressions is a feasible technique that results in decreased hands- off time with minimal risk to rescuers or patients during in-hospital cardiac arrest. Charging in anticipation of a potentially shockable rhythm may yield even greater benefits. Future work will be needed to assess the impact of these strategies on patient outcomes.
ACKNOWLEDGEMENTS
This work was supported by an unrestricted grant from Philips Healthcare (Andover, MA). We would like to acknowledge the support of the cardiac arrest resuscitation teams at the University of Chicago, University of Pennsylvania, and MacNeal Hospital. Without the hard work and commitment of the residents, interns and medical students at these sites, this study would not have been possible. We would also like to thank Mike Nakagawa for his assistance with compression artifact filtering and Derek Ayeh, Shawn Call, Jefferson Cua, and Neda Laiteerapong, MD, for their help with data collection and analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
Dr. Edelson is supported by a career development award from the National Heart, Lung, and Blood Institute (K23 HL097157-01), has received research support, speaking honoria and consulting fees from Philips Healthcare (Andover, MA), and is on the advisory board of Sotera Wireless (San Diego, CA). Dr. Abella has received research support from Philips Healthcare (Andover, MA) and Cardiac Science Corp (Bothell, WA), and speaking honoraria from Medic First Aid (Eugene, OR), Alsius Corp (Irvine, CA), Laerdal Medical (Wappingers Falls, NY), and Philips Healthcare (Andover, MA). Dr. Eilevstjønn is employed by Laerdal Medical AS.
REFERENCES
- 1.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 2.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 3.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 4.Chang Y-T, Tang W, Russell JK, Ristagno G, Sun S, Weil MH. Exclusion of a patient assessment interval and extension of the CPR interval both mitigate post-resuscitation myocardial dysfunction in a swine model of cardiac arrest. Resuscitation. 2008;76:285–290. doi: 10.1016/j.resuscitation.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eftestol T, Sunde K, Steen PA. Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out-of-hospital cardiac arrest. Circulation. 2002;105:2270–2273. doi: 10.1161/01.cir.0000016362.42586.fe. [DOI] [PubMed] [Google Scholar]
- 7.Gundersen K, Kvaloy JT, Kramer-Johansen J, Steen PA, Eftestol T. Development of the probability of return of spontaneous circulation in intervals without chest compressions during out-of-hospital cardiac arrest: an observational study. BMC Med. 2009;7:6. doi: 10.1186/1741-7015-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rea TD, Helbock M, Perry S, et al. Increasing use of cardiopulmonary resuscitation during out-of-hospital ventricular fibrillation arrest: survival implications of guideline changes.[see comment] Circulation. 2006;114:2760–2765. doi: 10.1161/CIRCULATIONAHA.106.654715. [DOI] [PubMed] [Google Scholar]
- 9.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Eilevstjonn J, Kramer-Johansen J, Sunde K. Shock outcome is related to prior rhythm and duration of ventricular fibrillation. Resuscitation. 2007;75:60–67. doi: 10.1016/j.resuscitation.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 11.Sato Y, Weil MH, Sun S, et al. Adverse effects of interrupting precordial compression during cardiopulmonary resuscitation. Crit Care Med. 1997;25:733–736. doi: 10.1097/00003246-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Yu T, Weil MH, Tang W, et al. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation. 2002;106:368–372. doi: 10.1161/01.cir.0000021429.22005.2e. [DOI] [PubMed] [Google Scholar]
- 13.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–IV203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 14.2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 8: Interdisciplinary topics. Resuscitation. 2005;67:305–314. doi: 10.1016/j.resuscitation.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 15.Nolan JP, Deakin CD, Soar J, Bottiger BW, Smith G. European Resuscitation Council guidelines for resuscitation 2005. Section 4. Adult advanced life support. Resuscitation. 2005;67(Suppl 1):S39–S86. doi: 10.1016/j.resuscitation.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Perkins GD, Davies RP, Soar J, Thickett DR. The impact of manual defibrillation technique on no-flow time during simulated cardiopulmonary resuscitation. Resuscitation. 2007;73:109–114. doi: 10.1016/j.resuscitation.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–1069. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 18.Steen S, Liao Q, Pierre L, Paskevicius A, Sjoberg T. The critical importance of minimal delay between chest compressions and subsequent defibrillation: a haemodynamic explanation. Resuscitation. 2003;58:249–258. doi: 10.1016/s0300-9572(03)00265-x. [DOI] [PubMed] [Google Scholar]
- 19.Walcott GP, Melnick SB, Walker RG, et al. Effect of timing and duration of a single chest compression pause on short-term survival following prolonged ventricular fibrillation. Resuscitation. 2009;80:458–462. doi: 10.1016/j.resuscitation.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ECC Committee, Subcommittees, and Task Forces of the American Heart Association. 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7.2: management of cardiac arrest. Circulation. 2005;112(supplement):IV-58–IV-66. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 21.Hoke RS, Heinroth K, Trappe HJ, Werdan K. Is external defibrillation an electric threat for bystanders? Resuscitation. 2009;80:395–401. doi: 10.1016/j.resuscitation.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd MS, Heeke B, Walter PF, Langberg JJ. Hands-on defibrillation: an analysis of electrical current flow through rescuers in direct contact with patients during biphasic external defibrillation.[see comment] Circulation. 2008;117:2510–2514. doi: 10.1161/CIRCULATIONAHA.107.763011. [DOI] [PubMed] [Google Scholar]
- 23.Blackburn GE. Ul-1950 - an Iec-950-Based United-States Standard for Information Technology Equipment Including Electrical Business Equipment. Ieee Transactions on Industry Applications. 1992;28:228–232. [Google Scholar]
- 24.Kerber RE. "I'm clear, you're clear, everybody's clear" - A tradition no longer necessary for defibrillation? Circulation. 2008;117:2435–2436. doi: 10.1161/CIRCULATIONAHA.108.773721. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan JL. Letter by Sullivan Regarding Article, "Hands-On Defibrillation: An Analysis of Electrical Current Flow Through Rescuers in Direct Contact With Patients During Biphasic External Defibrillation". Circulation. 2008;118:E712-E. doi: 10.1161/CIRCULATIONAHA.108.803718. [DOI] [PubMed] [Google Scholar]
- 26.Gliner BE, White RD. Electrocardiographic evaluation of defibrillation shocks delivered to out-of-hospital sudden cardiac arrest patients. Resuscitation. 1999;41:133–144. doi: 10.1016/s0300-9572(99)00040-4. [DOI] [PubMed] [Google Scholar]
- 27.Schneider T, Martens PR, Paschen H, et al. Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized Response to Cardiac Arrest (ORCA) Investigators. Circulation. 2000;102:1780–1787. doi: 10.1161/01.cir.102.15.1780. [DOI] [PubMed] [Google Scholar]
- 28.Whitfield R, Colquhoun M, Chamberlain D, Newcombe R, Davies CS, Boyle R. The Department of Health National Defibrillator Programme: analysis of downloads from 250 deployments of public access defibrillators. Resuscitation. 2005;64:269–277. doi: 10.1016/j.resuscitation.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Eilevstjønn J, Eftestol T, Aase SO, Myklebust H, Husoy JH, Steen PA. Feasibility of shock advice analysis during CPR through removal of CPR artifacts from the human ECG. Resuscitation. 2004;61:131–141. doi: 10.1016/j.resuscitation.2003.12.019. [DOI] [PubMed] [Google Scholar]