Abstract
A clear understanding of the pharmacodynamic properties of antifungal agents is important for the adequate treatment of fungal infections like candidiasis. For certain antifungal agents, the determination of Minimal Fungicidal Concentration (MFC) and time kill curve could be clinically more relevant than the determination of the Minimal Inhibitory Concentration (MIC). In this study, MIC and MFC to fluconazole, amphotericin B and caspofungin against C. albicans isolates and the killing patterns obtained with caspofungin and amphotericin B against susceptible and resistant strains to fluconazole were determined. The results of MICs showed that all C. albicans isolates were highly susceptible to amphotericin B, but two isolates were fluconazole resistant. The comparative analysis between MIC and MFC showed that MFC of fluconazole was fourfold higher than MIC in 41.9% of the C. albicans isolates. Same values of MFC and MIC of amphotericin B and caspofungin were found for 71% of the isolates. Correlation between time kill curves and MFC of amphotericin B and caspofungin against all 4 isolates tested was observed. The caspofungin killing effect was more evident at MFC in 6 hours of incubation than at MIC in this time, suggesting dependence of concentration. The similarity of results of time-kill curve and MFC values indicate that determination of MFC is an alternative for the detection of the fungicidal activity of these drugs.
Keywords: Antifungal susceptibility, Candida albicans, Time kill curves
Candidiasis, the main opportunistic fungal infection has steadily increased over the past 30 years (15,24). Many factors and overuse of broad-spectrum antimicrobials agents improved life-sustaining therapy, aggressive anticancer therapy and the AIDS epidemic contribute to the increase of incidence of this infection (8,33).
Oropharyngeal candidiasis is the most common clinical manifestation in human immunodeficiency virus patients (HIV) (16,24,34). Treatment of this fungal infection presents several problems. Besides the toxicity presented by amphotericin B, the widespread use of antifungal agents has induced to resistance to azoles (1,18,23). Therefore the clear understanding of the pharmacodynamic properties of antifungal agents is important for the improvement of the treatment of oropharyngeal candidiasis (4). Amphotericin B deoxycholate, considered gold standard for therapy of fungal infection due to binding to fungal membrane sterols, has been reported having of fungicidal action (6,18,33). The echinocandin caspofungin, shown be equivalent to amphotericin B for the treatment of candidiasis due to inhibition of 1,3 β D glucan synthase, an enzyme essential for the formation fungal cell wall, has also been described as fungicidal (12,14,30,31). The azoles, such as fluconazole, used in the treatment of superficial and deep-seated candidiasis, are described as fungistatic (19,22,32).
For the adequate treatment of the fungal infections, the determination of minimal fungicidal concentration (MFC) and time kill curve could be clinically more relevant than the minimal inhibitory concentration (MIC) of some antifungal agents. Previous reports have shown that the same MIC of amphotericin B may correspond to different killing activities depending on the strain tested (6). In this study we evaluated the MIC and MFC to fluconazole, amphotericin B and caspofungin against C. albicans strains isolated from HIV+ patients and the killing patterns obtained with caspofungin and amphotericin B against fluconazole susceptible and resistant strains.
MATERIALS AND METHODS
Microorganisms
A total of 31 Candida albicans isolates were used in this study. These isolates, previously identified according to Kurtzman and Fell (21), were obtained of oral mucosa from HIV+ patients. All patients gave written informed consent and the study was approved by the HC Bioethics Committee of Hospital de Doenças Tropicais de Goiás (007/2004) and Hospital das Clinicas da UFG (027/07). All isolates were stored in sterile distilled water at room temperature and subsequently inoculated onto Sabouraud dextrose agar (SDA- DIFCO) for 24 h at 35ºC before testing. C. parapsilosis ATCC 22019 was used as control.
Antifungal susceptibility testing
Antifungal susceptibility tests for amphotericin B (Bristol-Myers Squibb), fluconazole (Pfizer Pharmaceuticals Group) and caspofungin (Merck Sharpe & Dome) were performed using the broth microdilution method according to CLSI M27A2 (25). The antifungal agents were obtained as standard powders and stock solutions were dissolved in water (caspofungin and fluconazole) or 100% dimethyl sulfoxide (amphotericin B). The final concentrations of the antifungal agents were 0.03 to 16 μg/ ml for caspofungin and amphotericin B and 0.125 to 64 μg/ml for fluconazole. MIC of amphotericin and caspofungin was defined as the concentration resulting in 100% growth inhibition (27) and of fluconazole was defined as the lowest concentration inhibiting at least 50% of the control tube growth (25). Isolates with caspofungin and amphotericin B MICs of > 1 μg/ml and a fluconazole MIC of ≥ 64 μg/ml were considered as resistant (17,25,28).
MFC Determination
Minimal fungicidal concentrations were determined according to Canton et al. (6). Briefly, MFCs were evaluated by transferring 0.1ml from all clear MIC wells (no growth seen in microdilution trays) onto SDA plates. The MFC was the lowest drug concentration that killed ≥ 99.9% of cells.
Time-Kill Curve Procedures
Time kill tests using the methodology of Klepser et al. (20) were conducted for four C. albicans isolates and one Candida parapsilosis ATCC 22019 (control). These strains of C. albicans were selected according to a prior susceptibility testing, including two fluconazole susceptible and two fluconazole resistant isolates. Briefly, three to five colonies of Candida isolates grown for 24 to 48h on SDA were suspended in 5ml of saline, and the fungal suspension was counted using a hemacytometer. An appropriate volume of fungal suspension to yield a starting inoculum of 104 cells/ml was then added to 30 ml of RPMI 1640 medium buffered with MOPS. Caspofungin and amphotericin B were added to individual cultures resulting concentrations equal to 0.5; 1; 2 and 4 times the MICs for the test isolates. Test solutions were placed on a shaker and incubated at 37ºC. At predetermined time points (0, 6, 12 and 24 hours) after the incubation, 100μl volumes were removed from each test suspension, serially diluted in RPMI broth and plated on SDA (100 μl) for colony counting. All time-kill curve studies were conducted in duplicate and average colony counts (log10 CFU/ml) versus time (h) was constructed.
RESULTS
Caspofungin and amphotericin B were highly active against C. albicans isolates. The MIC for all isolates was ≤ 1 μg/ml for these two antifungal agents, with ranges of 0.06 - 1.0 μg/ml for amphotericin B and 0.015 - 1.0 μg/ml for caspofungin. For fluconazole, two isolates were resistant, with MIC ≥ 64 μg/ml. The range of MIC and MFC, MIC50 and MIC90 of these antifungal agents against Candida albicans isolates are shown in Table 1.
Table 1.
In vitro activity of three antifungal agents against 31 C. albicans isolates obtained from oral mucosa of HIV+ patients.
| Antifungal agents | MIC | MFC | ||
|---|---|---|---|---|
| range | 50% | 90% | range | |
| Fluconazole | 0.125 – ≥ 64 | 0.5 | 2 | 0.5 – 256 |
| Amphotericin B | 0.06 – 1 | 0.25 | 1.0 | 0.06 – 2 |
| Caspofungin | 0.015 – 1 | 0.125 | 0.5 | 0.06 – 2 |
The comparative analysis of MIC and MFC indicated that MFC of fluconazole was four times higher than MIC for 13 (41.9%) C. albicans isolates. Same values of MFC and MIC of amphotericin B and caspofungin were found in 22 (71%) isolates (Table 2).
Table 2.
Relation ship between MFC and MIC for three antifungal agents against Si C. albicans isolates.
| MFC = n X MIC | Number (%) of isolates with MFC n-folds higher than the MIC for | ||
|---|---|---|---|
| Fluconazole | Amphotericin B | Caspofungin | |
| MFC = MIC | 5 (16.1) | 22 (71) | 22 (71) |
| MFC = 2 x MIC | 12 (38.7) | 6 (19.3) | 9 (29) |
| MFC = 4 x MIC | 13 (41.9) | 3(6.4) | 0 |
| MFC = 8 x MIC | 1 (3.2) | 0 | 0 |
The killing patterns of caspofungin and amphotericin B constructed in RPMI 1640 medium buffered with MOPS against Candida isolates were similar to MIC or MFC values. For amphotericin B fungicidal activity, the maximal effect was verified in 6 h of incubation at concentration equal to MIC for three isolates (isolates 2, 3 and 5) and at concentrations equal to MFC for one isolate (isolate 34) and for C. parapsilosis ATCC 22019 (Fig. 1). The maximal effect of caspofungin fungicidal activity occurred in 6 h of incubation at concentration equal to MIC for isolates 34 and for C. parapsilosis ATCC 22019, while for isolates 2, 3 and 5, this activity occurred in 24 h. After 6 h at concentrations equal to MFC the maximal effect was observed for all isolates (Fig. 2).
Figure 1.
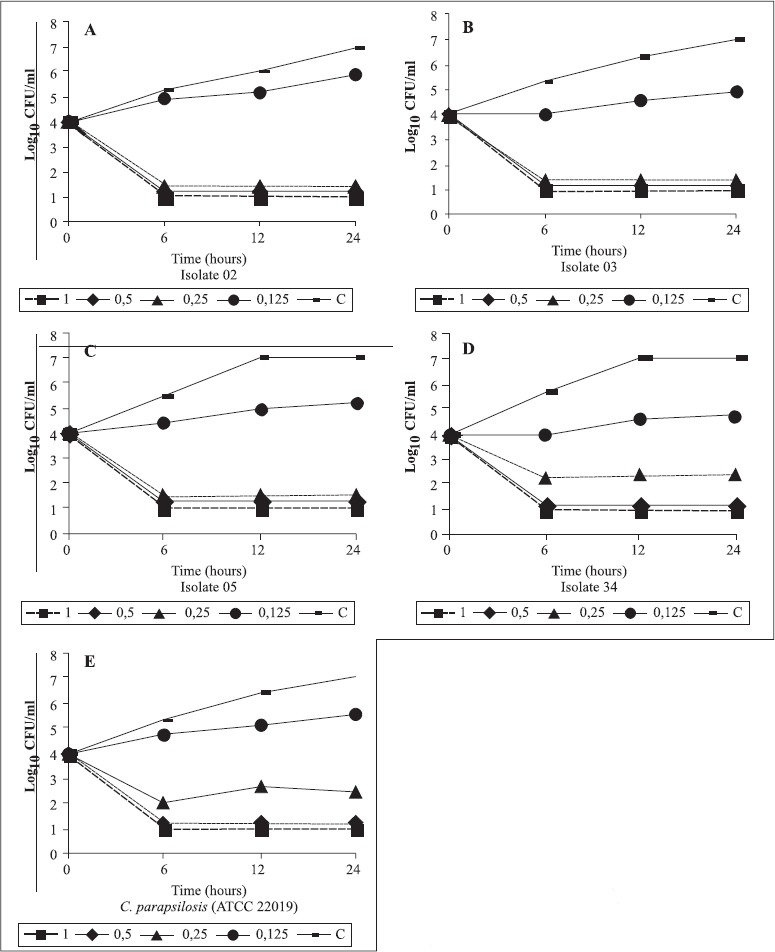
Time-kill curves for amphotericin B against clinical C. albicans isolates. A-isolate 2 (MIC= MFC=0.25 μg/ml); B-isolate 3 (MIC = MFC= 0.125 μg/ml); C-isolate 5 (MIC=MFC= 0.25); Disolate 34 (MIC=0.25; MFC=0.5 μg/ml); E-C. parapsilosis ATCC 22019 (MIC= 0.25, MFC=1)▄ = Growth control; ■ = 4X MIC; ♦ 2X MIC; ▲ = MIC; ● = 1/2 MIC.
Figure 2.
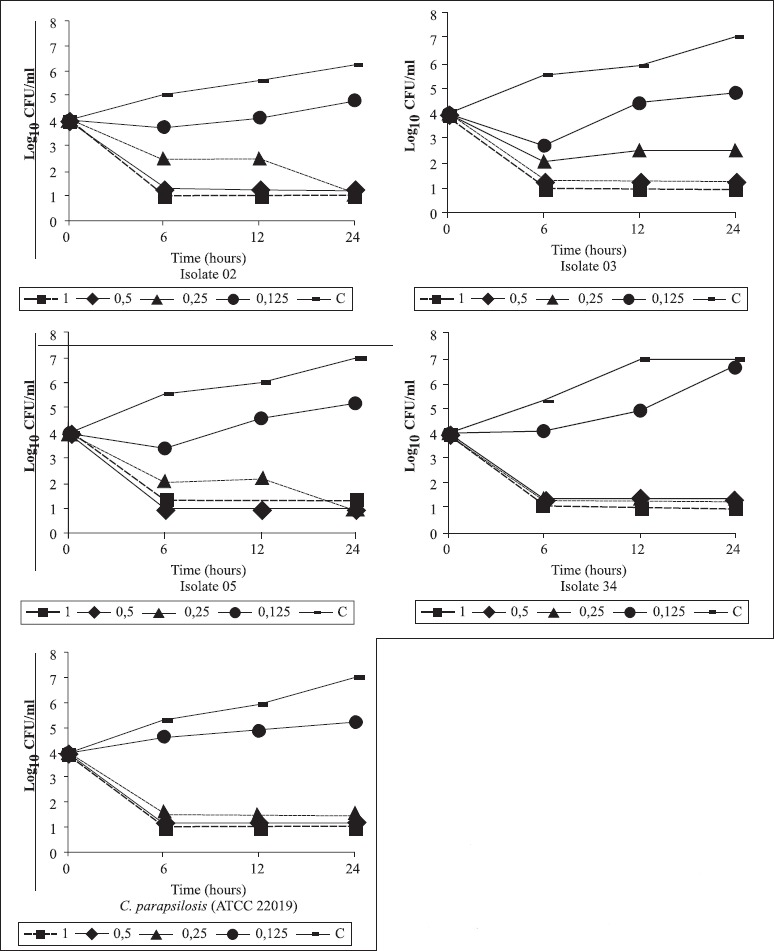
Time-kill curves for caspofungin against clinical C. albicans isolates. A-isolate 2 (MIC= MFC=0.25, MFC=0.5 μg/ml); B,isolate 3 (MIC = MFC= 0.25, MFC= 0.5 μg/ml); C,isolate 5 (MIC=0.25, MFC= 0.5); D, isolate 34 (MIC=0.25; MFC=0.5 μg/ml); E-C. parapsilosis ATCC 22019 (MIC=MFC=0.25)▄ = Growth control; ■ = 4X MIC; ♦ 2X MIC; ▲ = MIC; ● = 1/2 MIC.
DISCUSSION
The antifungal susceptibility results indicated that all Candida albicans isolates obtained from HIV+ patients were highly susceptible to amphotericin B and caspofungin. It is well known that amphotericin B and caspofungin have excellent in vitro activity against C. albicans. MICs of caspofungin ≤ 1 μg/ml were found for 99% of 3959 clinical isolates of Candida studied by Pfaller et al. (29), and a concentration of 0.25 μg/ml was able to inhibit 90% of C. albicans isolates. A antifungal testing performed against 1997 clinical isolates of Candida obtained from BSI (bloodstream infection) showed that amphotericin B was highly active against most isolates with MIC90 of 1 μg/ml for C. albicans (28). In this study, the susceptibility profile exhibited for all C. albicans isolates to these two antifungal agents was ≤ 1 μg/ml, with the MIC90 of caspofungin of 0.5 μg/ml and of amphotericin B of 1.0 μg/ml.
Although used in standard prophylaxis and therapy of candidiasis (22) two isolates were resistant to fluconazole. These resistant isolates were susceptible to amphotericin B and to caspofungin with MICs of 0.125 and 0.25 μg/ml for amphotericin B and of 0.25 and 0.06 μg/ml for caspofungin. In vitro studies have reported fluconazole resistant Candida clinical isolates. Among the 3959 isolates of Candida studied by Pfaller et al. (29) 157 were resistant to fluconazole. Interestingly, these researchers verified that caspofungin was active against the fluconazole resistant Candida isolates. The results of the in Pattern of susceptibility and killing of Candida spp vitro susceptibility tests obtained by Nowika et al (26) also indicated the occurrence of fluconazole resistant C. albicans isolates susceptible to amphotericin B. Treatment failures and recurrence of infection has been seen involving the use of fluconazole (10,30,33).
Several researchers reported the fungicidal activity of caspofungin and amphotericin B (7,9,30). In this study, for 71% of C. albicans isolates the MFC of amphotericin B and caspofungin were equal to MIC (Table 2). For caspofungin, the MFC was 2 x MIC (Table 2) in 29% of the isolates. For amphotericin B MFC was 2 x MIC in 19.3% and 4 x MIC in 6.4% of the isolates (Table 2). Similar results have been observed by Cantón et al. (5) for amphotericin B, who reported differences between MIC and MFC greater than four dilutions for two C. albicans isolates. For caspofungin, MICs comparable the MFCs for C. albicans were reported (2,13).
Little is known about the role of differences between MIC and MFC in treatment failure, and more studies are needed. Cantón et al. (6) have postulated that the use of the time kill curves to provide assessment of fungicidal activity is better than MIC or MFC endpoint.
The in vitro pharmacodynamics findings by time kill curves revealed that amphotericin B fungicidal activity was only exerted at 2x MIC for one isolate resistant to fluconazole and for C. parapsilosis ATCC 22019 (fluconazole susceptible). MFCs for these isolates were also greater than 2 x MIC. For two susceptible and one fluconazole resistant isolates, the fungicidal activity was equal to MIC (Fig. 1). Despite presenting similarity to of Cantón et al. (6) that suggested that the fungicidal activity of amphotericin B against C. albicans is strain dependent results of the present study suggest that the killing effect is concentration dependent as well.
According to Ernst et al. (11), the killing of C. albicans under caspofungin effect is concentration dependent, too. In this study, the caspofungin killing effect was more evident at MFC in 6 h of incubation than at MIC found to this drug in this time (Fig. 2). It is known that the levels of this antifungal agent attainable in the plasma for clinical isolates treated with caspofungin has been seen to be fourfold or more the MIC values detected in vitro (30).
In summary, the time kill curves against C. albicans suggest that amphotericin B is more potent than caspofungin. The maximal fungicidal activity amphotericin B of (Emax) is achieved at 6 h of incubation, while for caspofungin the maximal activity was seen after 24 h. These results were similar to those reported by Bonaventura et al. (3), who verified that EC50 (concentration producing 50% of Emax) for amphotericin B and caspofungin against the Candida isolates were achieved in 0.8 h and 1.3 h, respectively.
The similarity of results of time-kill curve and MFC make the determination of MFC an alternative for the detection of the fungicidal activity of these drugs.
RESUMO
Teste de suscetibilidade de Candida albicans isoladas da mucosa orofaringeana de pacientes HIV+, ao fluconazol, anfotericcina B e caspofungina. Cinética de morte de caspofungina e anfotericina B contra isolados fluconazol resistentes e suscetíveis
Um claro entendimento das propriedades farmacodinâmicas dos agentes antifúngicos é de grande importância para o adequado tratamento das infecções fúngicas como a candidíase. Em alguns casos de escolha do agente antifúngico, a determinação da concentração fungicida minima (CFM) e a curva do tempo de morte podem ser mais clinicamente relevantes do que a concentração inibitória minima (CIM). Nesse estudo, foi avaliado a CIM e a CFM de fluconazol, anfotericina B e caspofungina em Candida albicans e ainda os padrões de morte obtidos com caspofungina e anfotericina B de isolados suscetíveis e resistentes ao fluconazol. Os resultados de CIM mostraram que todos os isolados de Candida albicans foram altamente suscetíveis à anfotericina B, entretanto dois isolados foram fluconazol resistentes. A análise comparativa de CIM e da CFM mostrou que o CFM de fluconazol foi quatro vezes superior à CIM para 41,9% dos isolados de Candida albicans. Valores iguais de CFM e CIM de anfotericina B e caspofungina foram encontrados para 71% dos isolados. Correlação entre a curva do tempo de morte e a CFM de anfotericina B e caspofungina contra quatro isolados testados foi observada. O efeito de morte de caspofungina foi mais evidente na CFM até 6 horas de incubação do que na CIM nesse mesmo tempo, sugerindo a dependência da concentração. A similaridade dos resultados da curva do tempo de morte e os valores de CFM indicam que a determinação da CFM é uma escolha alternativa na detecção da atividade fungicida destes agentes antifúngicos.
Palavras-chave: Suscetibilidade antifúngica, Candida albicans, Curva do tempo de morte
REFERENCES>
- 1.Barchiesi F., Maracci M., Radi B., Arzeni D., Bladassarri I., Giacometti A., Scalise G. Point prevalence, microbiology and fluconazole susceptibility patterns of yeast isolates colonizing the oral cavities of HIV-infected patients in the era of highly active antiretroviral therapy. J. Antimicrob Chemother. 2002;50:999–1002. doi: 10.1093/jac/dkf233. [DOI] [PubMed] [Google Scholar]
- 2.Bartizal K., Gill C.J., Abruzzo G.K., Flattery A.M., Kong L., Scott P.M.J., Smith G., Leighton C.E., Bouffard A., Dropinski J.F., Balkovec J. In vitro preclinical evaluation studies with the echinocandin antifungal MK-0991 (L-743,872). Antimicrob. Agents. Chemother. 1997;41:2326–2332. doi: 10.1128/aac.41.11.2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonaventura G.D.I., Spedicato I., Picciani C., D’Antonio D., Piccolomini R. In vitro pharmacodynamic characteristics of amphotericin B, caspofungin, fluconazole, and voriconazole against bloodstream isolates of infrequent Candida species from patients with hematologic malignancies. Antimicrob. Agents. Chemother. 2004;48:4453–4456. doi: 10.1128/AAC.48.11.4453-4456.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgess D.S., Hastings R.W., Summers K.K., Hardin T.C., Rinaldi M.G. Pharmacodynamics of fluconazole, itraconazole, and amphotericin B against Candida albicans. Diagn Microbiol Infect Dis. 2000;36:13–18. doi: 10.1016/s0732-8893(99)00097-8. [DOI] [PubMed] [Google Scholar]
- 5.Cantón E., Pemán J., Viudes A., Quindós G., Gobernado M., Espinel-Ingroff A. Minimum fungicidal concentrations of amphotericin B for bloodstream Candida species. Diag Microbiol Infect Dis. 2003;45:203–206. doi: 10.1016/s0732-8893(02)00525-4. [DOI] [PubMed] [Google Scholar]
- 6.Cantón E., Pemán J., Gobernado M., Viudes A., Espinel-Ingroff A. Patterns of amphotericin B Killing Kinectics against seven Candida species. Antimicrob. Agents. Chemother. 2004;48:2477–2482. doi: 10.1128/AAC.48.7.2477-2482.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cantón E., Pemán J., Sastre M., Romero M., Espinel-Ingroff A. Killing Kinetics of Caspofungin, Micafungin, and amphotericin B against Candida guilliermondii. Antimicrob. Agents. Chemother. 2006;50:2829–2832. doi: 10.1128/AAC.00524-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chattopadhyay A., Caplan D.J., Slade G.D., Shugars D.C., Tien H.C., Patton L.L. Risk indicators for oral candidiasis and oral hairy leukoplakia in HIV-infected adults. Community. Dent. Oral. Epidemiol. 2005;33:35–44. doi: 10.1111/j.1600-0528.2004.00194.x. [DOI] [PubMed] [Google Scholar]
- 9.Clemons K.V., Espiritu M., Parmar R., Stevens D.A. Assessment of the Paradoxical effect of caspofungin in the therapy of candidiasis. Antimicrob. Agents. Chemother. 2006;50:1293–1297. doi: 10.1128/AAC.50.4.1293-1297.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costa M., Passos X.S., Miranda A.T.B., Araújo R.S.C., Paula C.R., Silva M.R.R. Correlation of in vitro itraconazole and fluconazole susceptibility with clinical outcome for patients with vulvovaginal candidiasis. Mycophatologia. 2004;157:43–47. doi: 10.1023/b:myco.0000012220.09227.25. [DOI] [PubMed] [Google Scholar]
- 11.Ernst E.J., Klepser M.E., Ernst M.E., Messer S.A., Pfaller M.A. In vitro phamacodynamic properties of MK- 0991 determined by time-kill methods. Diag Microbiol. Infect. Dis. 1999;33:75–80. doi: 10.1016/s0732-8893(98)00130-8. [DOI] [PubMed] [Google Scholar]
- 12.Ernst E.J., Klepser M.E., Pfaller M.A. Postantifungal effects of echinocandin, azole and polyene antifungal agents against Candida albicans and Cryptococcus neoformans. Antimicrob. Agents. Chemother. 2000;44:1108–1111. doi: 10.1128/aac.44.4.1108-1111.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Espinel-Ingroff A. Comparison of in vitro activities of the new triazole SCH56592 and the Echinocandins MK-0991 (L743,872) and LY 303366 against opportunistic filamentous and dimorphic fungi and yeasts. J. Clin. Microbiol. 1998;36:2950–2956. doi: 10.1128/jcm.36.10.2950-2956.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garbino J. Caspofungin- a new therapeutic option for oropharyngeal candidiasis. Clin. Microbiol. Infect. 2004;10:187–189. doi: 10.1111/j.1198-743x.2004.00823.x. [DOI] [PubMed] [Google Scholar]
- 15.Ghannoum M.A. Candida: a causative agent of an emerging infection. JID. Symposium. Proceedings. 2001;6:188–196. doi: 10.1046/j.0022-202x.2001.00047.x. [DOI] [PubMed] [Google Scholar]
- 16.Gugnani H.C., Becker K., Fegeler W., Basu S., Chattopadhya D., Baveja U., Satyanarayana S., Kalghatgi T., Murlidhar A. Oropharyngeal carriage of Candida species in HIV-infected patients in India. Mycoses. 2003;46:281–288. doi: 10.1046/j.1439-0507.2003.00896.x. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez S., López-Ribot J.L., Najvar L.K., McCarthy D.I., Bocanegra R., Graybill J.R. Caspofungin Resistance in Candida albicans: Correlating clinical outcome with laboratory susceptibility testing of three isogenic isolates serially obtained from a patient with progressive candida esophagitis. Antimicrob. Agents. Chemother. 2004;48:1382–1383. doi: 10.1128/AAC.48.4.1382-1383.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hossain M.A., Reyes G.H.L., Long A., Mukherjee P.K., Ghannoum M.A. Efficacy of caspofungin combined with amphotericin B against azole-resistant Candida albicans. J. Antimicrob. Chemother. 2003;51:1427–1429. doi: 10.1093/jac/dkg230. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy H.F., Shankland G.S., Bagg J., Chalmers E.A., Gibson B.E.S., Williams C.L. Fluconazole and itraconazole susceptibilities of Candida spp isolated from oropharyngeal specimens and blood cultures of paediatric haematology/ oncology patients. Mycoses. 2006;49:457–462. doi: 10.1111/j.1439-0507.2006.01272.x. [DOI] [PubMed] [Google Scholar]
- 20.Klepser M.E., Ernst E.J., Lewis R.E., Ernst M.E., Pfaller M.A. Influence of test conditions on antifungal time kill curve results: proposal for standardized methods. Antimicrob. Agents. Chemother. 1998;47:1207–1212. doi: 10.1128/aac.42.5.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurtzman C.P., Fell J.W. Fourth edition. Elsevier; 1998. The Yeast, A Taxonomic Study. [Google Scholar]
- 22.Martin M.V. The use of fluconazole and itraconazole in the treatment of Candida albicans infections: a review. J. Antimicrob. Chemother. 1999;44:429–437. doi: 10.1093/jac/44.4.429. [DOI] [PubMed] [Google Scholar]
- 23.Martinez R. An update on the use of antifungal agents. J. Bras. Pneumol. 2006;32:449–460. [PubMed] [Google Scholar]
- 24.Melo N.R., Taguchi H., Jorge J., Pedro R.J., Almeida O.P., Fukushima K., Nishimura K., Miyaji M. Oral Candida flora from Brazilian Human Immunodeficiency Virus-infected patients in the higly active antiretroviral therapy era. Mem. Inst. Oswaldo. Cruz. 2004;99:425–431. doi: 10.1590/s0074-02762004000400014. [DOI] [PubMed] [Google Scholar]
- 25.Vol. 17. Pennsylvania: Document M27-A, NCCLS; 2002. NCCLS- National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeasts; Approved standard. pp. 1–29. [Google Scholar]
- 26.Nowika J., Nawrot U., Juszczack K., Gusin B. Susceptibility to antifungal agents of Candida species isolated from paediatric and adult patients with haematological diseases. Mycoses. 2005;48:385–390. doi: 10.1111/j.1439-0507.2005.01154.x. [DOI] [PubMed] [Google Scholar]
- 27.Pfaller M.A., Messer S.A., Mills K., Bolmström A., Jones R.N. Evaluation of Etest method for determining caspofungin (MK-0991) susceptibilities of 726 clinical isolates of Candida species. J. Clin. Microbiol. 2001;39:4387–4389. doi: 10.1128/JCM.39.12.4387-4389.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfaller M.A., Diekma D.J., Jones R.N., Messer S.A., Hollis R.J. Trends in antifungal susceptibility of Candida spp isolated from pediatric and adult patients with bloodstream infections: SENSTRY antimicrobial surveillance program, 1997 to 2000. J. Clin. Microbiol. 2002;40:852–856. doi: 10.1128/JCM.40.3.852-856.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pfaller M.A., Diekema D.J., Messer S.A., Hollis R.J., Jones R.N. In vitro activities of caspofungin compared with those of fluconazole and itraconazole against 3,959 clinical isolates of Candida spp., including 157 fluconazole-resistant isolates. Antimicrob. Agents. Chemother. 2003;47:1068–1071. doi: 10.1128/AAC.47.3.1068-1071.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pfaller M.A., Messer S.A., Boyken L., Rice C., Tendolkar S., Hollis R.J., Diekema D.J. Caspofungin activity against clinical isolates of fluconazole-resistant Candida. J. Clin. Microbiol. 2003;41:5729–5731. doi: 10.1128/JCM.41.12.5729-5731.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pfaller M.A., Boyken L., Hollis R.J., Messer S.A., Tendolkar S., Diekema D.J. In vitro susceptibilities of Candida spp to caspofungin: four years of global surveillance. J. Clin. Microbiol. 2006;44:760–763. doi: 10.1128/JCM.44.3.760-763.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swinne D., Watelle M., Nolard N. In vitro activities of voriconazole, fluconazole, itraconazole and amphotericin B against non Candida albicans yeast isolates. Rev. Iberoam. Micol. 2005;22:24–28. doi: 10.1016/s1130-1406(05)70002-4. [DOI] [PubMed] [Google Scholar]
- 33.Yang Y.L., Li S.Y., Cheng H.H., Lo H.J. TSARY Hospitals. The trend of susceptibilities to amphotericin B and fluconazole of Candida species from 1999 to 2002 in Taiwan. BMC. Infect. Dis. 2005;5:99. doi: 10.1186/1471-2334-5-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Y.L., Lo H.J., Hung C.C., Li Y. Effect of prolonged HAART on oral colonization with Candida and candidiasis. BMC. Infect. Dis. 2006;6:8. doi: 10.1186/1471-2334-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


