Abstract
Conflict of interest: none declared.
Introduction
The incidence of diabetes type 2 (diabetes mellitus type 2 – DM 2) is rapidly increasing worldwide. Physical inactivity and obesity are the major determinants of the disease. Primary prevention of DM 2 entails health monitoring of people at risk category. People with impaired glycemic control are at high risk for development of DM 2 and enter the intensive supervision program for primary and secondary prevention.
Objective of the research
To evaluate the impact of metformin and lifestyle modification on glycemia and obesity in patients with prediabetes.
Patients and Methods
The study was conducted on three groups of 20 patients each (total of 60 patients) aged from 45 to 80, with an abnormal glycoregulation and prediabetes. The study did not include patients who already met the diagnostic criteria for the diagnosis of diabetes. During the study period of 6 months, one group was extensively educated on changing lifestyle (healthy nutrition and increased physical activity), the second group was treated with 500 mg metformin twice a day, while the control group was advised about diet and physical activities but different from the first two groups. At beginning of the study, all patients were measured initial levels of blood glucose, HbA1C, BMI (Body Mass Index), body weight and height and waist size. Also the same measurements were taken at the end of the conducted research, 6 months later. For the assessment of diabetes control was conducted fasting plasma glucose (FPG) test and 2 hours after a glucose load, and HbA1C.
Results
At the beginning of the study the average HbA1C (%) values in three different groups according to the type of intervention (lifestyle changes, metformin, control group) were as follows: (6.4 ± 0.5 mmol / l), (6.5 ± 1.2 mmol / l), (6.7 ± 0.5 mmol / l). At the end of the research, the average HbA1C values were: 6.2 ± 0.3 mmol / l, 6.33 ± 0.5 mmol / l and 6.7 ± 1.4 mmol / l. In the group of patients who received intensive training on changing lifestyle or group that was treated with metformin, the average reduction in blood glucose and HbA1C remained within the reference range and there were no criteria for the diagnosis of diabetes. Unlike the control group, a group that was well educated on changing habits decreased average body weight by 4.25 kg, BMI by 1.3 and waist size by 2.5 cm. Metformin therapy led to a reduction in the average weight of 3.83 kg, BMI of 1.33 and 3.27 for waist size. Changing lifestyle (healthy diet and increased physical activity) has led to a reduction in total body weight in 60% of patients, BMI in 65% of patients, whereas metformin therapy led to a reduction of the total body weight in 50%, BMI in 45% of patients. In the control group, the overall reduction in body weight was observed in 25%, and BMI in 15% of patients.
Conclusion
Modification of lifestyle, such as diet and increased physical activity or use of metformin may improve glycemic regulation, reduce obesity and prevent or delay the onset of developing DM 2.
Keywords: lifestyle changes, metformin, obesity, prediabetes, primary prevention
1. INTRODUCTION
The incidence of type 2 diabetes is increasing rapidly worldwide. Physical inactivity and obesity are the major determinants of disease and with the heritage are the main causes of insulin resistance, which reduces the sensitivity of tissues to insulin and brings in prediabetes condition. Persons with prediabetes are at increased risk for developing type 2 diabetes, and also in an increased risk of developing cardiovascular disease. Prediabetes or disturbed glycoregulation means that blood sugar is above normal, but not so large that they meet the requirement for the diagnosis of diabetes, and there are categories: impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) (1).
Primary prevention refers to intervention before the development of an underlying disorder, and is trying to prevent its occurrence and development. Usually involves attempts to influence the risk factors, in terms of reducing their impact, and strengthen protective factors.
One of the most used strategies for primary prevention is education. Primary prevention of DM 2 entails health monitoring of people at risk categories (2).
Screening asymptomatic patients as well as health monitoring risk categories include the following activities: education about diabetes, education about healthy nutrition and physical activity, prevention and treatment of obesity, measures to protect the pancreas (3) (4).
Secondary prevention includes measures for the early detection of diabetes by mass examinations of the population and screening examinations with increased surveillance of the risk categories for diabetes (patients with prediabetes, IFG and IGT), and people with diabetes (5).
Recently, it is recommended preventive use of metformin in patients with IFG and IGT that increases glucose utilization and sensitivity of insulin receptors (6). People with impaired glycemic control are at high risk for developing type 2 diabetes and enter in the intensive supervision program for primary and secondary prevention of DM 2. The objective of the study was to examine the effects of various measures of prevention to the glycemia and obesity, by lifestyle modification and metformin treatment in patients with prediabetes.
2. PATIENTS AND METHODS
A prospective study was performed in the Team 1 Family Medicine Health Center Kalesija.
The study was conducted in three groups of 20 patients each (total of 60 patients) aged 45 to 80, with an abnormal glycoregulation and prediabetes. The study did not include patients who already met the diagnostic criteria for the diagnosis of diabetes. During the study period of 6 months, one group was extensively educated on changing lifestyle (healthy nutrition and increased physical activity), the second group was treated with 500 mg metformin twice a day, while the control group was advised about diet and physical activities but different from the first two groups. At beginning of the study, all patients were measured initial levels of blood glucose, HbA1C, BMI, body weight and height and waist size. Also the same measurements were taken at the end of the conducted research, 6 months later. For the assessment of diabetes control was conducted fasting plasma glucose (FPG) test and 2 hours after a glucose load, and HbA1C.
The results are expressed as average values with standard deviation. Comparison between the groups of patients was made using the Student T-test for continuous variables and HI square or Fisher’s test for categorical variables.
3. RESULTS
At the beginning of the study the average HbA1C (%) values in three different groups according to the type of intervention (lifestyle changes, metformin, control group) were as follows: (6.4 ± 0.5 mmol/l), (6.5 ± 1.2 mmol/l), (6.7 ± 0.5 mmol/l). At the end of the research, the average HbA1C values were: 6.2 ± 0.3 mmol/ l, 6.33 ± 0.5 mmol/l and 6.7 ± 1.4 mmol/l (Figure 1).
Figure 1.
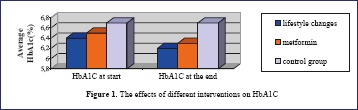
The effects of different interventions on HbA1C
Unlike the control group, in the group of patients who received intensive training on changing lifestyle or group that was treated with metformin, there was a significant reduction in the mean fasting glucose and HbA1C value, they were above the reference range, but were not sufficient for the diagnosis of type 2 diabetes.
Changing lifestyle (healthy nutrition and increased physical activity) led to significant reduction in initial body weight in 60% of patients, BMI in 65% of patients, waist size in 60% of patients, and HbA1C in 55% of patients (Figure 2).
Figure 2.
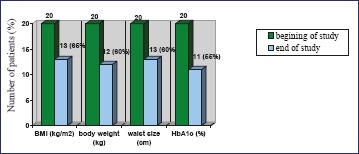
The effects of health education (lifestyle changes end exercise) to reduction of certain parameters
Metformin therapy led to a decrease in the average initial body weight by 3.83 kg, BMI by 1.33, the waist size by 3.27 cm, HbA1C by 0.13% (Figure 3).
Figure 3.
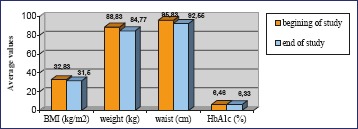
Metformin therapy effects
4. DISCUSSION
Prevention of diabetes type 2 can be achieved with lifestyle changes and the use of some medications. There is evidence that combined diet and exercise, as well as drug therapy (metformin, acarbose), can be effective in people with IGT in order to prevent progression to diabetes (7). Our results showed that, in contrast to the control group, the group with changing lifestyles, and a group treated with metformin, significantly reduced the initial body weight, BMI, waist size and HbA1C. Some studies suggest that weight loss of 5 to 10% of the initial body weight during the six-month period improved overall metabolic and glycemic control in obese patients with type 2 diabetes (8). In our study, reduced levels of fasting glucose and glycosylated hemoglobin were outside of the reference range, but it was not sufficient for the diagnosis of diabetes. Also, the initial decrease in body weight, BMI and waist size in our study was similar to the published results of studies conducted in Finland (9), which was proven to significantly reduce the risk of diabetes associated with lifestyle modifications, as well as studies in which was proven to reduce the risk of diabetes associated with a healthy diet (31%), exercise (46%), and a healthy diet and exercise (42%), by study conducted in China (10).
In DPP (Diabetes Prevention Program) Study the incidence of diabetes was reduced by 58% in the group with changing lifestyle and about 31% in the group treated with metformin, compared to placebo group (11). Insufficience of our study was that the treatment duration of only 6 months was not long enough to lead to a significant loss of body weight, BMI, and to reduce abnormal glucose regulation. Lack of the respondents willing to participate in the study and some other issues made it difficult to conduct research that would last longer. Finally, the benefits will depend on whether the glycemia could be held below those values as diagnostic criteria for prediabetes, and whether maintaining these low values would improve the long-term outcome. Also, this study did not show what are the individual contributions of physical activity and diet for the overall lifestyle change benefits, which could be investigated in the future.
Some studies suggests that prevention of diabetes leads to significant reduction of atherosclerosis, that is the main cause of death in people with type 2 diabetes (12) (13), which could also be investigated in the future.
5. CONCLUSION
Lifestyle modification (diet and increased physical activity) improves glycemic regulation and reduces obesity, can prevent or delay the onset of developing type 2 diabetes. Pharmacological treatment with metformin also reduces the risk, although less dramatically. It is assumed, that the good and ongoing diabetes prevention through education about the benefits of lifestyle change and metformin treatment could lead to a reduction in atherosclerosis and other cardiovascular diseases, which are the main cause of death in people with type 2 diabetes.
REFERENCES
- 1.American Diabetes Association Screening for type 2 diabetes. Diabetes Care. 2004; 27(Suppl. 1): S11–S14 [DOI] [PubMed] [Google Scholar]
- 2.King H, Dowd JE.Primary prevention of type 2 (non-insulindependent) diabetes mellitus. Diabetologia. 1990; 33: 3-8 [DOI] [PubMed] [Google Scholar]
- 3.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346: 393-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344: 1343-1350 [DOI] [PubMed] [Google Scholar]
- 5.[Guideline] American Diabetes Association Standards of medical care in diabetes. Diabetes Care. January2012; 35Suppl 1: S11-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002; 346 (6): 393-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santaguida PL, Balsmanjena tolerancija glukozeon C, Hunt D, et al. 2005. Diagnosis, prognosis, and treatment of impaired glucose tolerance and impaired fasting glucose. Evid Rep Technol Assess (Summ). (128): 1-11 [PMC free article] [PubMed] [Google Scholar]
- 8.Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009; 374 (9702): 1677-1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344: 1343-1350 [DOI] [PubMed] [Google Scholar]
- 10.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 1997; 20: 537-544 [DOI] [PubMed] [Google Scholar]
- 11.The Diabetes Prevention Program Research Group: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346: 393-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillum RF, Mussolino ME, Madans JH.Diabetes mellitus, coronary heart disease incidence, and death from all causes in African American and European American women: the NHANES I epidemiologic follow-up study. J Clin Epidemiol. 2000; 53: 511-518 [DOI] [PubMed] [Google Scholar]
- 13.Kuller LH, Velentgas P, Barzilay J, Beauchamp NJ, O’Leary DH, Savage PJ.Diabetes mellitus: subclinical cardiovascular disease and risk of incident cardiovascular disease and all-cause mortality. Arterioscler Thromb Vasc Biol. 2000; 20: 823-829 [DOI] [PubMed] [Google Scholar]


